Abstract
Introduction
Arthroscopy procedures are the gold standard for the management of tibial spine avulsion. This review evaluates and compares different arthroscopic treatment options for tibial spine fractures.
Source of data
PubMed, Medline, Ovid, Google Scholar and Embase databases were systematically searched with no limit regarding the year of publication.
Areas of agreement
An arthroscopic approach compared with arthrotomy reduces complications such as soft-tissue lesions, post-operative pain and length of hospitalization.
Areas of controversy
The use of suture techniques, compared to cannulated screw technique, avoids a second surgery for removal of the screws, but requires longer immobilization and partial weight bearing.
Growing points
Clinical outcomes and radiographic results do not seem to differ in relation to the chosen method of fixation.
Areas timely for developing research
Further studies are needed to produce clear guidelines to define the best choice in terms of clinical outcomes, function and complications.
Keywords: arthroscopic treatment, avulsion, fracture, tibial eminence, tibial spine
Introduction
Avulsion fractures of the tibial spine, first described by Poncet in 1875,1 are a major intra-articular injury in the paediatric knee2 and considered equivalent to tears of the anterior cruciate ligament (ACL) in adults.3
The most common mechanism of trauma, which leads to a disruption of the not completely ossified tibial spine rather than to failure of the ACL,4,5 is a trauma forcing the knee in hyperextension combined with valgus-external rotation.6 At times, these lesions can occur in adults; in this instance, the main cause is high-energy trauma, such as road accidents.7–9 This specific etiology explains the higher incidence of associated lesions to the menisci or capsulo-ligamentous structures in adults.1,10,11
The most common classification for these fractures was developed by Meyers and Mc Keever,12 and it is reliable for decision-making in diagnosis and treatment. Type I lesions are undisplaced or minimally displaced fractures involving the anterior margin of the spine; Type II fractures present a superior displacement of the anterior part of the fragment, with the posterior portion still attached to the rest of the proximal tibia (‘bird's beak’ pattern); in Type III lesions the fragment is completetly detached. Type III fractures can be further divided into Type IIIA, in which only the ACL insertion is involved, and Type IIIB, in which the whole tibial eminence is involved. Other authors described a Type IV, including comminuted fractures.13
The literature supports conservative management with a knee cast or splint in extension or mild flexion (20°–30°) for 6–12 weeks for Type I undisplaced tibial spine fractures14,15 and surgical treatment for Type II, if reduction is not anatomical,14,16 and Type III and IV fractures.17,18 Open surgical techniques have several disadvantages and more complications (soft-tissue damage, higher post-operative pain, longer hospital stay, and delay in rehabilitation). For this reason, arthroscopic techniques are considered the gold standard for the treatment of these lesions: they allow direct visualization of intra-articular injuries, simplified diagnosis, accurate reduction of fracture fragments, treatment of associated soft-tissue injuries and removal of loose fragments.9,19,20
The present study reviews different arthroscopic techniques and methods of fixation of these fractures reported in current literature, describing the state of art for the treatment of this pathology.
Methods
Search strategy
In September 2015, a systematic search was conducted in the online PubMed, Google Scholar, CINAHL, Cochrane Central and Embase Biomedical databases using the isolated or combined keyword ‘arthroscopic treatment and tibial eminence’, ‘arthroscopic treatment and tibial spine’, ‘tibial eminence avulsion’, ‘tibial spine fracture’; with no limits regarding the year of publication. Articles were included if they reported data on clinical and functional outcomes, complications and radiographic evaluation in series of patients who had undergone arthroscopic treatment for tibial spine avulsion. Two authors (Matteo Buda and Francesco Soldati) screened the selected articles for title, abstract and full text in accordance with predefined inclusion and exclusion criteria. The articles were accurately analysed focusing on objective rating scores, clinical and radiographic assessment and complications reported.
Criteria for consideration
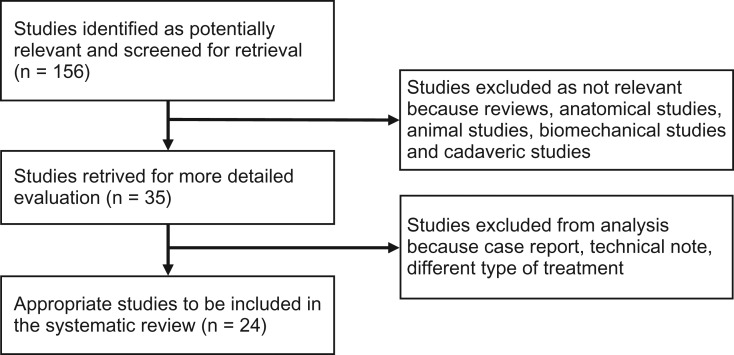
Given our language capabilities, we considered publications in Italian and English. Two authors (M.B. and S.F.) independently reviewed the content of each abstract. Once an article was identified as likely to be included, full-text versions were obtained to evaluate the exact content of the study. The reference lists of the selected articles were then examined by hand to identify articles not identified at the electronic search. All journals were considered and all relevant articles were retrieved. Studies focusing on clinical outcomes of patients who had undergone arthroscopic treatment of tibial eminences with any device were selected. Biomechanical reports, studies on animals, cadavers, in vitro studies, case reports, literature reviews, technical notes, letters to editors, instructional course and studies focusing only on complications were excluded. A final article analysis was made by all the authors, and a fully trained orthopaedic surgeon with a special interest in knee surgery and sports medicine (L.O.) made the final decision in cases of doubt (Fig. 1).
Fig. 1.
Study flow chart.
Results
Literature review
At the first electronic search, we identified 156 relevant publications. After application of the inclusion criteria, 35 studies remained. Of these, 11 studies were excluded because they were case report, technical notes, and described different types of treatment. Twenty-four studies ultimately met the inclusion criteria, 13 were retrospective20–32 and 11 prospective.7,33–42 Each study described a different arthroscopic treatment of tibial eminence fracture, reporting also post-operative protocol (Table 1).
Table 1.
Type of management, rehabilitation protocol and study population
| Author | Study | Technique | Inclusion criteria | Exclusion criteria | Post-operative treatment | Rehabilitation | Post-operative evaluation | Patients, Age; M/F | Type of lesion |
|---|---|---|---|---|---|---|---|---|---|
| Sommerfeldt, 200821 | Retrospective | Arthroscopic reduction and internal fixation (ARIF) with K-wires or cannulated screws | Type II, III and IV | ACL tears and tibial plateau growth plate fracture | Full W-B. in 20° of knee flexion with knee brace | Passive and active ext-flexion without W-B at 3–4 w (week), full W-B and stairs at 6–8 w | Rx, ROM and Lachman test | 9 pts (patients), 10,2 y(7–14) | 4 Type II, 4 pt Type III, 1 pt Type IV |
| Wouters, 201133 | Prospective | Meniscus Arrows(11) and ACL-aiming device(1) | Type II and III skelet immature patients | None | 5 w plaster | Progressive W-B, closed-chain exercise and proprioception | Rx, ROM, Lachman test, ADS and KT-1000 | 11 pts, 12 y(6–15); 4/7 | Not indicated |
| Ahn, 200522 | Retrospective | Pull-out suture | Type III and IV acute and cronic (nonunion) fractures | None | 2 w long leg splint and partial W-B until union | Limited motion brace gradually increased ROM | Rx, ROM, Lachman test, ADS, KT-2000, Lysholm knee scores, and Hospital for Surgery scores(HSS) | 14 pts, 29.7 y(6–47); 3/7 | 4 Type IIIA, 3 Type IIIB, 3 Type IV; 4 nonunion |
| Huang, 20087 | Prospective | Pull-out suture | Type II or higher, Lachman and ADS 2+, and acute fractures | None | 1 w full-ext brace | Full W-B, isom. ex., 2–4 w ROM 0–60, at 8 w ROM 0–120, 10–12 w cycling, at 6 m sports | Rx, ROM, Lachman, ADS, KT-1000, Lysholm score, Tegner Activity Level, and IKDC | 36 pts, 37 y(17–73); 14/22 | 6 Type II, 16 Type III and 14 Type IV |
| Vega, 200834 | Prospective | Fixation with suture-anchor | Type III and IV, skelet immature patient (open physes), and acute (<12 days after trauma) | Follow-up < 6 months | Full-ext brace for 2–3 w, partial W-B | Gradual flexion of the knee | Rx, ROM, Lachman, KT-1000, IKDC and Lysholm | 7 pts, 11,8 y(7–20); 5/2 | 5 Type III, and 2 Type IV |
| Reynders, 200223 | Retrospective | Cannulated screw fixation with spiked washer (screw removal within 6 m) | Type II and III, and acute fractures | Type I | Knee plaster cast for 1 w, WB at 6 w | Not indicated | Rx, ROM, Lachman, ADS, Pivot-shift and Lysholm | 26 pts, Type II: 15 y(13–17); 11/5; Type III: 17 y(16–18); 5/5 | 16 Type II, 10 Type III |
| Kocher, 200320 | Retrospective | Cannulated screw fixation (screw removal after 8–12 m) | Type III skelet immature patient | Skeletal mature patient (4 cases) and other methods (15 pt) | Long-leg cast flexed 30° and touch-down W-B for 4 w | Not indicated | Rx, ROM, Lachman and Pivot-shift, IKDC, KT-1000, Lysholm, Tegner, and Marshall knee score | 6 pts, 12.0 y (7,9–16,1); 4/2 | 6 Type III |
| Osti, 200035 | Prospective | Reduction and fixation with metallic suture; removal after union | Type III | None | Partial W-B, hinged brace locked 0° for 1 months | 0–30days: CPM, isom. ex, stretching; 30–60 d: full W-B; 60–90 d: swim and cycling; 120 d: return to sports | Rx at 6/8 w, ROM, Lachman, ADS, Pivot shift, KT-1000, quadriceps atrophy and swelling | 10 pts, 26.7 y (17–41); 7/3 | All Type III |
| May, 201124 | Retrospective | Screws (15 pt:68%)/sutures (7 pt:32%) ARIF (18 pt:82%)/ORIF (4 pt:18%) |
Type II and III, acute fractures | Ipsilat. lower limb fractures, multiligam.inj., non-op.treat. | Immob. in brace for 5.5 w (72%) or cast for 4 w (28%) | ROM initiated immediately in 11 pts (50%) and beyond the second w in 11 pts (50%). W-B initially toe-touch or not WB in 19 patients (86%) and W-B as tolerated in 3 pts (14%). | Rx, ROM, Lachman, ADS, Pivot-shift, Biodex testing, Lysholm, IKDC and Tegner | 22 pts, 17 y (7–39); 12/10 14 pt (64%) skelt imm | 12 Type II (55%) and 10 Type III (45%) |
| Liljeros, 200936 | Prospective | Bioabsorbable nails | Type II and III, skelet immature patient, and acute fractures (<72 h) | None | Cast in slight flex for 5 w and full W-B with crutches | FKT for 2 months | Rx, ROM, Lachman-KT-1000, Lysholm knee scoring scale and activity | 13(16) pts: 11 y(7–15); 8/8; 3 pt no follow-up | 2 Type II and 14 Type III |
| In Y, 200837 | Prospective | Fixation of the fragment using bioabsorbable suture anchors | None | None | Limitated-motion brace in full-ext. and no W-B for 2 w | After 2 w ROM exercises and partial W-B, at 6 w brace removal | Rx, ROM, Lachman and Pivot-shift IKDC, and KT-2000 | 5 pts: 4 adults (28–48 y) 1 child (8 y); 4/1 | 2 Type II, 2 Type III and 1 Type IV |
| Abdelkafy, 201438 | Prospective | FiberWire® or Orthocord® suture fixation | Type III, skeletally immature patients and fracture untreated for >6 w | Multiligamentous injury, chondral or osteochondral injury, skeletal maturity and Type I and II | Long-leg, hinged knee brace | Muscle contractions, straight-leg raises, passive ROM using a continuous passive motion (CPM) machine limited to 90° for one min and the gradually increased, toe-touch W-B with crutches immediately postoperatively. Progression to full W-B began 6 w after surgery. | Rx, IKDC, modified Lysholm knee score, VAS pain and patient satisfaction. | 13 pts, 10 y (7–14); 9/4 | Type III |
| Verdano, 201339 | Prospective | Absorbable suture fixation | Type II, III and IV | None | Not indicated | Not indicated | Rx, Lysholm knee scoring and Marshall scoring system | 21 pts, 28 y (9–60) | 9 Type II, 8 Type III and 5 Type IV |
| Wiegand, 201340 | Prospective | Herbert-screw fixation | Type II and III skelet immature patient | None | Long plaster splint was applied in the position of a 20°flexion until wound healing | Active and passive exercises 2–3 times a week and partial W-B after 4 w. Full W-B after the 6 w. | Rx, Lysholm functional scale, anterior drawer, Lachmann and Pivot shift | 8 pts, 12,5 y; 6/2 | 3 Type II and 5 Type III |
| Kluemper, 201325 | Retrospective | RCG device/suture or the RCG device/T-Fix (Acufex) methods | Type II, III and IV | Screw fixation, damage to the ACL exceeding 50% of substance, previous knee surgery and concomitant injuries | Brace locked in extension for weight bearing. | Physical therapy and quadriceps activation at 2 w, with flex limited to 90° for the first 6 w. Then full ROM and W-B with the brace. At 3 m (if anatomic fracture healing) brace was discontinued and return to sports at 4 m. | ROM, Lachman stability, varus/valgus stress test, pain, anterior and posterior drawer tests, resumption of preinjury activity levels and integrity of the ACL. | 17 pts, 16.8 y (13–37 y); 16/1 | 15 (88%) Type III, 1 Type II fracture and 1 patient Type IV. |
| Faivre, 201426 | Retrospective | Tightrope fixation | Type II or III acute fractures | Tibial plateau fracture, nerve or vessel damage, multiligament injury or knee dislocation | Brace for the first month | Knee motion exercises to prevent flexion deformity were started immediately without any limitation, W-B as tolerated. | Rx, post-operative knee laxity measured by Rolimeter® and IKDC scores, the kneemobility, and the Lachman test | 8 pts, 34.2 y( ± 12.5); 2/6 | 5 Type II, 2 Type IIIa and 1 Type IIIb |
| Pan, 201227 | Retrospective | Cannulated screws (SF) or Ethibond sutures (ES) | Type II, III and IV fractures and skeletally mature | None | Brace for 8 w | Isometric quadriceps strengthening exercises in a full-extension knee brace. Total W-B permitted. ROM 0°–90° for 3–4 w, then 0°–120° for 5–6 w. Cycling, swimming and removal of brace at 8 w followed by running and a progressive return to athletic activities at 16 w. | Rx, pivot shift test and side-to-side difference in laxity measured by the KT-1000 arthrometer, ROM, IKDC and Lysholm score | 48 pts: 25 SF (18–52 y); 4/11; 23 ES (17–50 y); 16/7 | SF: 9 Type II, 15 Type III and 1 Type IV fracture. EF: 8 Type II, 14 Type III and 1 Type IV |
| Ochiai, 201141 | Prospective | Meniscal Viper Repair System (Arthrex, Naples and FL) |
Type II, III and IV fractures | None | Cast for 2 w. | Brace and ROM training from 2 w. Partial W-B from 5 and full W-B from 8 w after surgery | Rx, ROM, side-to-side differences measured by Telos SE and Lysholm scores | 5 pts, 28.8 y (7–55); 4/1 | 1 Type II, 3 Type III and 1 Type IV |
| Tudisco, 201028 | Retrospective | Conservative managment (4 Type I, 2 Type II and 1 Type III), ORIF(1 Type III) and ARIF with suture (1 Type II and 5 Type III) | Type I, II, III and IV fractures | None | Long-leg brace for 6 w unlocked for 6–10 h a day for 3 w | Physical therapy with flex limited to 90° for the first 2 w. Full ROM by 6 w. | Rx, pain, ROM, clinical test, KT-1000 and IKDC | 14 pts, 12.3 y (7–16); 12/2 | 4 Type 1, 3 Type II and 7 Type III |
| Matthews, 199442 | Prospective | Suture fixation and 1 conservative management (Type II) | Type II and III | None | Knee immobilizer for 3 w in full extension | ROM, quadriceps strenghtening started at 3 w and W-B at 6 w | Rx, ROM, lachman and pivot shift test | 6 pts, 24 (16–36); 5/1 | 5 Type III and 1 Type II |
| Wagih, 201529 | Retrospective | Transosseous suture | Type III | None | Extension for 4–6 w | Partial W-B for the first 2–4 w with ROM exercises and active hamstring flexion exercises. Active open chain quadriceps contractions are not allowed for 6 w. Full W-B at 4–6 w. | Rx, ROM, lachman test and IKDC | 11 pts, 8 (6–11); 8/3 | Type III |
| Edmonds, 201430 | Retrospective | Suture fixation: ARIF 28 pts ORIF 29 pts Conservative management 19 pts (CM) |
Type II and III | Type I and no post-operative Xray | Immob. in brace: ARIF: 5.1 w ORIF: 4.4 w CM: 5.4 w |
Not indicated | Rx, Pain, Lysholm score and treatment satisfaction | 76 pts, ARIF: 12.4 ± 2 y; 64%/36% ORIF: 12.2 ± 3 y; 83%/17% CM: 12.4 ± 4 y; 79%/21% |
Not indicated |
| Watts, 201531 | Retrospective | ARIF: 18 pts (suture: 9, screw: 8 and both: 1) ORIF: 13 pts (suture: 2, screw: 9 and both: 2) |
Type II and III | None | Immobilization: ARIF: 16.6d (2–36) ORIF: 21.8d (7–44) |
Not indicated | Not indicated | 31 pts, ARIF: 12.9 ± 2.7; 11/7 ORIF: 11.5 ± 2.6; 7/6 |
Type II: ARIF: 13, ORIF: 9 Type III: ARIF: 5, ORIF: 4 |
| Memisoglu, 201532 | Retrospective | Intra-articular button | Not indicated | Not indicated | Brace (0°–30°) for 3 w and increased 10°–20° per week. Full weightbearing with a locking knee brace in 0° extension. | Patellar mobilizations, quadriceps isometric strengthening exercises and ROM exercises using a CPM machine | Rx, objective and subjective IKDC score, Lysholm knee score, KT-1000 arthrometer, ROM, Anterior drawer, Lachman and pivot-shift tests | 11 pts, 12.2(10–16);11/0 | 9 Type IIIA, 1 Type IIIB, 1 Type IV |
Surgical technique
Different arthroscopic surgical techniques were used in the articles analysed. Arthroscopic reduction and internal fixation (ARIF) with Kirschner wires,21 cannulated screws,20,21,23,24,27,31 a Meniscus Arrow device,33 pull-out sutures,7,22 suture with anchores,34,37 metallic suture,35 transosseous sutures,24,27–31,38,39,42 intra-articular button,32 bioabsorbable nail,36 Herbert screw,40 Tight-rope fixation,26 rotator cuff guide (RCG) device/suture or the RCG device/T-Fix (Acufex) methods,25 and Meniscal Viper Repair System (Arthrex, Naples, FL)41 were used.
Outcome measures
The criteria used for the evaluation of the outcomes were bone union of the fracture on standard AP and lateral views, range of motion (ROM), and specific tests for instability such as the Lachman, pivot shift and drawer test measured by KT-1000 Arthrometer or similar devices. Outcome scores used were Lysholm Knee Score (LKS),7,20,22–24,27,30,32,34,36,38–41 the Hospital for Special Surgery (HSS) knee score,22 the International Knee Documentation Committee (IKDC),7,24,26,27,29,32,34,37,38 Marshal,20,39 Tegner7,20,24,27 and VAS scores.38
Rehabilitation protocol
Different rehabilitation protocols were used (Table 2). The length of immobilization and weight-bearing was different in each of the reviewed studies. In summary, rehabilitation depends on the type of fracture, the quality of fixation and patient compliance. Stiffness after surgical procedure is considerably increased compared with conservative treatment, thus early mobilization was recommended. Isometric exercises are usually performed to improve the strength of the quadriceps during the period of immobilization to reduce muscular atrophy.
Table 2.
Outcomes and complications
| Author | Results | Follow-up | Complications | |||
|---|---|---|---|---|---|---|
| ROM | TEST | RX | SCORE | |||
| Sommerfeldt, 200821 | Normal (100%) | Lachmann+ in 3 pts without subjective instability | Slight dislocation without impingement | Not indicated | 12 m | 10 converted in mini-arthrotomy (6 Type IV) |
| Wouters, 201133 | Normal (100%) at 9 w | Mild laxity in 2 pts: KT-1000 < = 3 mm (diff. both sides) | 100% union | Not indicated | 4 y(3–10) | 1 refracture: retreated and healed |
| Ahn, 200522 | Normal (100%) | 13pts (Lachman-, ADS- and KT-2000 < 3 mm), 1 pt F (Lachman and ADS 2+, KT-2000 5 mm) | Acute cases: union 10.8 w (8–12) and nonunion 15 w (12–16) | LKS 95.6 (92–100), HSS 96.4 (91–100); no preop (pre-operative) | 51 m (30–80); acute 53 m | Limb leg discrepancy 1 cm (affected longer) in 2 pts |
| Huang, 20087 | 16 pts (44,4%) normal ROM; 2 pts (5.5%) abnormal flex (16–25°) (1 Type I and 1 Rype IV) |
Lachman and ADS -(100%), KT-1000 <3 mm (100%) | 100% union after 3 m, 2 pts (10%) Stage I degen. sec. Ahlback | LKS: preop 38, postop 98. TEL: preop 3 postop 7.3. IKDC: preop light to sedentary activity level, postop 94,5% strenous-to-moderate activity level (= preinjury level). |
34.4 m (24–91) | None |
| Vega, 200834 | 4 normal, 3 nearly n. | KT-1000 2 mm(1–3); Lachman and ADS and Pivot shift – (100%) | 100% union | Lysholm: preop 29 postop 94 IKDC: post 92 (86–98) |
6–24 m | Not reported |
| Reynders, 200223 | 22 normal, 4 ext nearly n. | Type II: 3 pt no laxity, 13 pt Lach. + without giving way; Type III: 100% ADS + in 4 pt, ++ in 4 pt, +++ in 2 pt. | 4 pts with Type III: improper reduction | Lysholm: Type II 95.25 and Type III 89.70 | 2–8 y | Ledging (shelf-like projection of bone due to improper reduction) in 4 pts (1 second-look for impingenment) and ACL insufficiency in 2 pts with Type III |
| Kocher, 200320 | Normal (100%) | Lachman: 1 pt normal, 3 nearly normal, 2 abnormal Pivot-shift: 4 normal, 2 n.normal. KT-1000 >3 mm in 4/6 pts. |
No malunion | Lysholm: 99.5 (98–100) Marshall: 49.0 (47–50) Tegner: 8.7 (7–9) |
3.2 y (2–6.3) | Not noted |
| Osti, 200035 | Full ext. /flex. 125–135° | Lachman and Pivot-shift—and KT-1000<3 mm (80%), Lachman + and KT-1000>3 mm (20%) | 100% union after 6–8 w | No patients complain residual pain/instability | 1 year (13–74 m) | Recurrent swelling after sport in 1 pt |
| May, 201124 | Mean knee extension: −1° (−7°/−10°) and mean knee flexion: 133°(90°/150°) | Lachman- (80%), 1+ (15%) and 2+ (5%). All + had Type III. | 17 pts (72%) 100% union; 5 pts (28%) gap 2–5 mm (2 ARIF + suture, 2 ARIF + screw, and 1 ORIF + screw) | LKS: pre 43 post 93 IKDC: pre 45 post 91 Tegner: preop 6.6 postop 6.4. Age has negative impact on LKS (-7 x ogni decade increse), IKDC (−7) and Tegner (−1) |
7 y (2–15) | 6 pts (27%): 4 pts (57%) screw fixation required symptomatic hardware removal. 2 pts (13%) with suture fixation: 1 manipulation and 1 arthroscopic scar tissue debridement. |
| Liljeros, 200 936 | 3 pts 5–10° flex.def.; 4 pts 5° ext.def. |
1 pt con KT-1000 = 3 mm, 100% normal at single-leg hop test, and 1 pt abnormal side-hop test | 100% union (3 pts 2 mm frag. elevation) | Lysholm score: 11 pts excellent, 1 pt good and 1 pt poor. | 3, 9 y (2–5) | 1 conversion to OPEN for technical problems |
| In Y, 200837 | Full ROM | Lachmann & Pivot-shift -, KT-2000 <3 mm | 100% union | IKDC: normal in 2 pts, nearly normal in 3 pts. | 1 y | None |
| Abdelkafy, 201438 | Full ROM | 11 pts Lachman, anterior drawer and pivot shift tests -. 2 pts Lachman test +, anterior drawer and pivot shift tests -. All pts return to their preinjury level of activity and recreational sports |
Few mm of superior displacement of the anterior end of the fracture fragment | IKDC: 12 A and 1 B Lysholm score: 91.2 Subjective IKDC: 80.5 VAS pain: 0.4 VAS operation satisfaction: 9.6 |
10.8 m (SD 6.8; 4–24) | One case of superficial wound infection (successfully treated with antibiotics) |
| Verdano, 201339 | Not indicated | Not indicated | 100% union at 8 w (6–10) | Lysholm knee score: 60% good results and 40% very good results Marshall scoring system: 20% good results and 80% very good results |
24 m (12–33) | None |
| Wiegand, 201340 | Full ROM | No instability in any pts. Lachman and anterior drawer + in one case | 100% union | Lysholm functional scale: 94.97 in Type II and 94.20 in Type III | 1 y | Incipient arthritis 5 years after primary treatment. |
| Kluemper, 201325 | 2 pts lost 3° of ext, and 1 pt lost more than 10° of flex (On average lost 5.5°) | All pts Lachman-, good stability, anterior and posterior drawer tests -,varus/valgus stress test-, and resumed their preop level of activity | 100% union | 9 (53%) pts no pain and 8 pts mild intermittent pain associated with strenuous activity. | 25.3 m (2 m–13 y) | None |
| Faivre, 201426 | 3 pts severe difficulties regaining motion | One significant anterior laxity with a side-to-side Rolimeter difference of 4 mm and Lachman test+, | 100% union | 3 pts IKDC A, 2 B, 1 C and 1 D | 10 m | 3 pts motion complications and 2 required an arthroscopic arthrolysis. |
| Pan, 201227 | Extension deficit > 2° in 3 SF (12%) and in 6 ES (27%). Flexion deficit > 5° in 2 SF (8%) and in 5 ES (22%). |
KT-1000 side-to-side difference > 5 mm in 2 pts (8%) in SF group and in 3 pts (13%) in the ES group. SF: 2 (8%) pt pivot shift + and 2 (8%) 2 pivot shift ++. ES: 5 (22%) pivot shift +, 3 (13%) pivot shift ++ and 1 (9%) pivot shift +++ |
100% union | SF group: Lysholm: 95, IKDC subjective: 93, Tegner activity: 8, and IKDC objective evaluation (%): 23 A (92%), 2 B (8%), and C0 (0%) ES group: Lysholm: 90, IKDC subjective: 90, Tegner activity: 7, and IKDC objective evaluation (%): 16 A (70%), 4B (17%), and 3 C (13%) |
SF: 58 m (24–100) ES: 47 m (24–93) |
One joint stiffness approximately 3 months after surgery (EF group) |
| Ochiai, 201141 | ROM side-to-side difference(°): ext: 2.0 (0–8) and flx: 0.8 (0–4) | Telos SE/the side-to-side difference (mm): 3.6 (2.4–3.9) | 100% union | Lysholm score: 90.7 (90–100) | 16 m (8–24) | None |
| Tudisco, 201028 | Complete | 13 pt: returned to the same sport activity level 4 pt: Lachman + and KT-1000 difference >5 mm but not subjective instability |
Good reduction in five cases and sufficient in two cases | Seven treated nonoperatively: normal reults in six cases and abnormal in one (Type III). ORIF: nearly normal results ARIF: 2 normal (1 Type II e 1 Type III) and 4 nearly normal (Type III) |
29 y (12–42) end of skeletal growt (mean age: 41 y) | Degenerative arthrosis in 2 pts |
| Matthews, 199442 | 2–135° (range 0–140°) | No instability in any of the pts. Lachman and pivot shift - | 100% union | None | 1 y | None |
| Wagih, 201529 | 1 pt: 5° extension deficit | 1 pt: Lachman 1+ | 100% union | IKDC: 9A and 2 B | 16.3 (11–21) m | None |
| Edmonds, 201430 | Not indicated | Not indicated | 100% union | Pain: ARIF: 0.2, ORIF: 0.7 and C.m.: 2.7 Lysholm: ARIF: 95, ORIF: 97.4 and CM: 86 Treatment satisfaction: ARIF: 9.6, ORIF: 9.9 and CM: 9 |
5 ARIF: 5.6 ± 2 y 7 ORIF: 6.8 ± 2 y 6 CM: 5.8 ± 2 y |
Arthrofibrosis: ARIF:12% and ORIF: 11.1% CM: 16.7% subsequent operation |
| Watts, 201531 | Not indicated | None | Not indicated | Not indicated | ARIF: 13.9 ± 10.5 m ORIF: 12.7 ± 14.3 m |
Arthrofibrosis: ARIF: 7 pts (38.9%) and ORIF: 1 pt (14.3%) |
| Memisoglu, 201532 | Active extension: −1.8°± 3.4 (−10° to 0°) Active flexion: 135.5°± 6.1° (125°– 145°) |
Anterior drawer, Lachman and pivot-shift tests - | 100% union | Lysholm score: 95.7 ± 6.6 (84–100) IKDC subjective score: 94.3 (85–100). Global IKDC scores: 7 normal (A) and 4 nearly normal (B) |
69 m (60–84) | None |
Study population
The total number of patients was 384 (235 males and 142 females). Two studies21,39 did not report gender. Fifteen studies20,21,23–25,28–34,36,38,40 had an average age of less than 18 years (skeletally immature patients) while 9 studies7,22,26,27,35,37,39,41,42 reported data about adult patients.
Using Meyers and McKeever classification, 104 Type II, 202 Type III and 31 Type IV lesions were reported. One study33 did not describe the types of lesion.
Clinical outcomes
The clinical results overall were excellent. Regarding ROM, 263 patients achieved complete ROM (100%), and 7 patients achieved a nearly normal ROM.23,34 Eighteen patients exhibited a flexion deficit (5–10°),7,25,27,36,41 and an extension deficit was found in 21 patients.25,27,29,36,41 Three patients had severe difficulties regaining complete ROM.26
Clinical evaluation was based on the Lachman test, pivot shift test and anterior drawer sign (ADS), in some studies the KT-1000 or similar was used. A Lachman + was found in 36 patients,20–24,26,28,29,33,35,36,38,40 a Lachman 2+ in 3 patients.20,24 Anterior knee laxity measured with ADS and KT-1000 was found in 31 patients.20,22,23,26–28,33,35,36,40 Pivot shift test when used as a rotational instability test was found + in 4 patients.20,27 Details from the included articles are provided in Table 2.
Radiographic evaluation
In 16 publications7,24–27,29,30,32–35,37,39–42 there was a 100% bone union, an acceptable reduction was achieved in two patients (2/7) treated with ARIF in one study,28 and a mild superior displacement of the anterior end of the fracture fragment was found in patients treated with FiberWire® or Orthocord® suture fixation38 and in three (3/16) patients treated with bioabsorbable nails.36 In four patients with a Type III lesion treated with cannulated screw an improper reduction was achieved.23 One study used Kirschner wires or cannulated screws; it evidenced a slight dislocation without impingment21 in five patients (28%) treated with different techniques, and a 2–5 mm gap.24
Complications
Different complications occurred: 1 patient refractured,33 a limb leg discrepancy of 1 cm (with the affected leg longer) was reported in 2 patients,22 ledging (shelf-like projection of bone due to improper reduction) in 4 patients,23 partial ACL lesion in 3 patients, recurrent swelling after sport in 1 patients,35 and arthrofibrosis in 19 patients.24,26,29,30 In one patient, conversion to open surgery was necessary for technical problem36; there was one case of superficial wound infection,38 an incipient arthritis 5 years after primary treatment,40 one joint stiffness at 3 months after surgery,27 and degenerative arthrosis in two patients.28
Discussion
Surgical treatment is indicated for Type II fractures, when attempt at the reduction has failed, and for Type III and IV fractures.8,9,22–24,33,34,37
Different surgical options have been proposed, including open reduction and internal fixation (ORIF),14,17,43 arthroscopic reduction and immobilization, and ARIF.8,9,22–24,33,34,37 Open surgical techniques have several disadvantages and more complications, including soft-tissue damage during arthrotomy, higher postoperative pain causing delay in physical therapy and a longer hospital stay. On the other hand, arthroscopic techniques are considered the gold standard for these lesions since they allow to better visualize intra-articular injuries, simplify the diagnosis, reduce accurately the fracture, remove loose fragments and manage associated soft-tissue injuries.9,19,20 Among associated injuries, tears to the anterior root of both menisci and interstitial tears of the ACL may frequently occur.9,19,20 Meniscal tears may be repaired arthroscopically after reduction and fixation of the fracture; the interstitial tears of the ACL may not be diagnosed and, after surgery, cause ACL laxity, which is often not relevant from a clinical view point.9,19,20
Arthroscopic management consists first in the debridement of the bony bed of the avulsion fragment and the removal of the soft tissue interposed, which might prevent anatomical reduction. Each part of meniscus or intermeniscal ligament entrapped in the fracture site must be carefully removed without damaging these structures or altering their function.44
Methods of arthroscopic fixation of these fractures include Kirschner wires,21,44 staples,45 absorbable nails,33,36 metallic screws,21,23,45 fixation with non-absorbable sutures1,9,22,24,46 or metallic wire,35 reinsertion of the fragment with a metallic34 or absorbable37 anchor-screw. Screws and suture fixation are currently the most used and reliable surgical techniques reported in the literature.1,9,21–24,45,46
Fracture fixation can be achieved with either anterograde or retrograde screw insertion. Cannulated screws are often used to optimize the entry point of the screw in the fragment and to insert it in a more accurate direction. Antegrade screw insertion is performed inserting an aiming guide through the superior anteromedial portal and the direction of the screw is from superoanterior to inferoposterior, keeping the knee at 90 degrees of flexion. In the retrograde fashion, the screw is inserted from the anterior cortex of the proximal tibia through the tibial eminence fracture.47
The screw technique is therefore simple and reproducible, allows early mobilization and weight-bearing, but has some contraindications and disadvantages. Removal of the screw can be necessary in case of persistent discomfort at the site of fixation after fracture healing. Thus, some authors reported good results and high patients satisfaction with this further procedure. Nevertheless, incorrect position of the screw can also cause impingement and cartilage damage.48 Growth disturbance and leg-length discrepancy might occur in patients with open physis, but the screw can be inserted with a physeal-sparing technique providing excellent radiographic and clinical outcomes.3 Screw fixation is controindicated in case of small size or comminution of the fragment, and thus its insertion can lead to further displacement.5,12,22
Different devices, such as Tightrope,26 meniscal viper repair system,41 RCG,25 Meniscus arrows or ACL–aiming device33 or simple sutures, can be used to achieve the same clinical and radiographic results. One of the advantages of these techniques is the possibility to use it to treat fractures with small or comminuted fragments, providing a stable fixation with no need for further intervention to remove those devices. On the other hand, the passage of the bone tunnels through growth plates could cause bone growth disorders.13 Matthews and Geisseler42 developed a technique of arthroscopic reduction and fixation using sutures with multiple PDS wires in five patients with tibial eminence fractures. No patients complained of subjective instability at 1 year, and only one patient had a deficit of 2° to full extension at latest follow-up.
Huang et al. 7 reported 36 patients (average age: 37, range 17–73) with Type II, III and IV fractures treated with multiple sutures and pull-out (No. 5 Ethibond wires). This method provided good functional results (LKS, Tegner Activity Level, IKDC): only one patient had residual pain during moderate-intense exercise, and two patients (one Type III and one Type IV) showed a significant flexion deficit of 16–25°.
Ahn and Yoo22 used a similar technique of fixation with multiple sutures and pull-out (No. 0 PDS) to treat 10 acute fractures (Type III and IV) and 4 non-unions, reporting excellent functional results with fracture healing after a mean of 12.3 months and full ROM in all patients, and only one patient with laxity at Lachman and drawer tests and instrumental tests (KT-2000 arthrometer >5 mm of difference with contralateral knee) without subjective instability. The authors reported two patients who experienced growth disturbance with the affected limb 1 cm longer than the contralateral, and a genu recurvatum in one of the two patients; they suggest, in patients with open growth plates, to use alternative methods or to prevent the passage of tunnels for the pull-out through the anterior side of cartilage growth.
Osti et al. 35 reported a series of 10 adult patients (mean age 26.7 years) with a Type III fracture treated arthroscopically with metallic suture removed after complete fragment union: all patients showed radiographic healing in 6–8 weeks with full ROM and stability (two patients had a KT-1000 > 3 mm, without symptomatic instability).
Using absorbable suture fixation, Verdano et al. 39 also showed good and very good results in 21 patients with complete union of the avulsed fragment at 2 years of follow-up without complications and similar results were reported by Pan et al. 27 However, ARIF with sutures requires a longer immobilization and partial weight-bearing, resulting in a higher risk of joint stiffness and arthrofibrosis.35
Conclusions
Arthroscopy provides a less invasive method to approach these lesions, reducing the risks related to open technique such as soft-tissue damage, post-operative pain, infection and longer period of hospital stay. Furthermore, arthroscopic reduction and suture fixation do not require further surgery to remove fixation devices, but longer period of immobilization and partial weight-bearing. Nevertheless, clinical and radiographic results do not differ in relation to the chosen method of fixation. We suggest that the choice of the fixation technique should rely mainly on the experience of the surgeon.
Conflict of Interest statement
The authors have no potential conflicts of interest.
References
- 1.Kendall NS, Hsu SY, Chan KM. Fracture of the tibial spine in adults and children. A review of 31 cases. J Bone Joint Surg Br 1992;74:848–52. [DOI] [PubMed] [Google Scholar]
- 2.Andersen JW, Mejdahl S. Bilateral fracture of the tibial spine. Acta Orthop Belg 1993;59:394–7. [PubMed] [Google Scholar]
- 3.Kocher MS, Micheli LJ. The pediatric knee: Evaluation and treatment In: Insall JN, Scott WN (eds). Surgery of the Knee, 3rd ed New York: Churchill-Livingstone, 2001, 1356–97. [Google Scholar]
- 4.Reynders P, Reynders K, Broos P. Pediatric and adolescent tibial eminence fractures: arthroscopic cannulated screw fixation. J Trauma 2002;53:49–54. [DOI] [PubMed] [Google Scholar]
- 5.Woo SL, Hollis JM, Adams DJ, et al. Tensile properties of the human femur-anterior cruciate ligament-tibia complex. The effects of specimen age and orientation. Am J Sports Med 1991;19:217–25. [DOI] [PubMed] [Google Scholar]
- 6.Rockwood CA, Green DP. Fractures in Adults. Philadelphia, etc: JB Lippincott Co, 1984. [Google Scholar]
- 7.Huang TW, Hsu KY, Cheng CY, et al. Arthroscopic suture fixation of tibial eminence avulsion fractures. Arthroscopy 2008;24:1232–8. [DOI] [PubMed] [Google Scholar]
- 8.Shelbourne KD, Urch SE, Freeman H. Outcomes after arthroscopic excision of the bony prominence in the treatment of tibial spine avulsion fractures. Arthroscopy 2011;27:784–91. [DOI] [PubMed] [Google Scholar]
- 9.Vargas B, Lutz N, Dutoit M, Zambelli PY. Nonunion after fracture of the anterior tibial spine: case report and review of the literature. J Pediatr Orthop B 2009;18:90–2. [DOI] [PubMed] [Google Scholar]
- 10.Liljedahl S-O, Lindvall N, Wetterfors J. Early diagnosis and treatment of acute ruptures of the anterior cruciate ligament: a clinical and arthrographic study of forty-eight cases. J Bone Joint Surg [Am] 1965;47-A:l503–13. [PubMed] [Google Scholar]
- 11.Falstie-Jensen S, Sondergard Petersen PE. Incarceration of the meniscus in fractures of the intercondylar eminence of the tibia in children. Injury 1984;15:236–8. [DOI] [PubMed] [Google Scholar]
- 12.Meyers MH, McKeever FM. Fracture of the intercondylar eminence of the tibia. J Bone Joint Surg Am 1959;41:209–22. [PubMed] [Google Scholar]
- 13.Zaricznyj B. Avulsion fracture of the tibial eminence: treatment by open reduction and pinning. J Bone Joint Surg Am 1977;59:1111–4. [PubMed] [Google Scholar]
- 14.Kocher MS. Lesioni intra-articolari del ginocchio. Rockwood e Wilkins – Traumatologia Pediatrica In: Beaty JH, Kasser JR (eds). 6° Edizione Verduci Editore. Vol. 2 2008, 987–97. [Google Scholar]
- 15.Meyers MH, McKeever FM. Follow-up notes: fracture of the intercondylar eminence of the tibia. J Bone Joint Surg Am 1970;52:1677–83. [PubMed] [Google Scholar]
- 16.Bakalim G, Wilppula E. Closed treatment of fracture of the tibial spines. Injury 1973;5:210–212. [DOI] [PubMed] [Google Scholar]
- 17.Molander ML, Wallin G, Wikstad I. Fracture of the intercondylar eminence of the tibia: a review of 35 patients. J Bone Joint Surg Br 1981;63-B:89–91. [DOI] [PubMed] [Google Scholar]
- 18.Bakalim G, Wilppula E. Closed treatment of fracture of the tibial spines. Injury 1974;5:210–2. [DOI] [PubMed] [Google Scholar]
- 19.Lubowitz JH, Elson WS, Guttmann D. Part II: Arthroscopic treatment of tibial plateau fractures. Arthroscopy 2005;21: 86–92. [DOI] [PubMed] [Google Scholar]
- 20.Kocher MS, Foreman ES, Micheli LJ. Laxity and functional outcome after arthroscopic reduction and internal fixation of displaced tibial spine fractures in children. Arthroscopy 2003;19:1085–90. [DOI] [PubMed] [Google Scholar]
- 21.Sommerfeldt DW. Arthroscopically assisted internal fixation of avulsion fractures of the anterior cruciate ligament during childhood and adolescence. Oper Orthop Traumatol 2008;20:310–20. [DOI] [PubMed] [Google Scholar]
- 22.Ahn JH, Yoo JC. Clinical outcome of arthroscopic reduction and suture for displaced acute and chronic tibial spine fractures. Knee Surg Sports Traumatol Arthrosc 2005;13:116–21. [DOI] [PubMed] [Google Scholar]
- 23.Reynders P, Reynders K, Broos P. Pediatric and adolescent tibial eminence fractures: arthroscopic cannulated screw fixation. J Trauma 2002;53:49–54. [DOI] [PubMed] [Google Scholar]
- 24.May JH, Levy BA, Guse D, et al. ACL tibial spine avulsion: mid-term outcomes and rehabilitation. Orthopedics 2011;34:89. [DOI] [PubMed] [Google Scholar]
- 25.Kluemper CT, Snyder GM, Coats AC, et al. Arthroscopic suture fixation of tibial eminence fractures. Orthopedics 2013;36:e1401–6. [DOI] [PubMed] [Google Scholar]
- 26.Faivre B, Benea H, Klouche S, et al. An original arthroscopic fixation of adult's tibial eminence fractures using the Tightrope® device: a report of 8 cases and review of literature. Knee 2014;21:833–9. [DOI] [PubMed] [Google Scholar]
- 27.Pan RY, Yang JJ, Chang JH, et al. Clinical outcome of arthroscopic fixation of anterior tibial eminence avulsion fractures in skeletally mature patients: a comparison of suture and screw fixation technique. J Trauma Acute Care Surg 2012;72:E88–93. [DOI] [PubMed] [Google Scholar]
- 28.Tudisco C, Giovarruscio R, Febo A, et al. Intercondylar eminence avulsion fracture in children: long-term follow-up of 14 cases at the end of skeletal growth. J Pediatr Orthop B 2010;19:403–8. [DOI] [PubMed] [Google Scholar]
- 29.Wagih AM. Arthroscopic treatment of avulsed tibial spine fractures using a transosseous sutures technique. Acta Orthop Belg 2015;81:141–6. [PubMed] [Google Scholar]
- 30.Edmonds EW, Fornari ED, Dashe J, et al. Results of displaced pediatric tibial spine fractures: a comparison between open, arthroscopic, and closed management. J Pediatr Orthop 2015;35:651–6. [DOI] [PubMed] [Google Scholar]
- 31.Watts CD, Larson AN, Milbrandt TA.. Open versus arthroscopic reduction for tibial eminence fracture fixation in children. J Pediatr Orthop 2015. [Epub ahead of print] [DOI] [PubMed] [Google Scholar]
- 32.Memisoglu K, Muezzinoglu US, Atmaca H, et al. Arthroscopic fixation with intra-articular button for tibial intercondylar eminence fractures in skeletally immature patients. J Pediatr Orthop B 2016;25:31–6. [DOI] [PubMed] [Google Scholar]
- 33.Wouters DB, de Graaf JS, Hemmer PH, et al. The arthroscopic treatment of displaced tibial spine fractures in children and adolescents using Meniscus Arrows. Knee Surg Sports Traumatol Arthrosc 2011;19:736–9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Vega JR, Irribarra LA, Baar AK, et al. Arthroscopic fixation of displaced tibial eminence fractures: a new growth plate–sparing method. Arthroscopy 2008;24:1239–43. [DOI] [PubMed] [Google Scholar]
- 35.Osti L, Merlo F, Liu H, Bocchi L. A Simple modified arthroscopic procedure for fixation of displaced tibia1 eminence fractures. Arthroscopy 2000;16:379–82. [DOI] [PubMed] [Google Scholar]
- 36.Liljeros K RPT, Werner S RPT, Janarv P-M. Arthroscopic fixation of anterior tibial spine fractures with bioabsorbable nails in skeletally immature patients. Am J Sports Med 2009;37:923–8. [DOI] [PubMed] [Google Scholar]
- 37.In Y, Kim JM, Woo YK, et al. Arthroscopic fixation of anterior cruciate ligament tibial avulsion fractures using bioabsorbable suture anchors. Knee Surg Sports Traumatol Arthrosc 2008;16:286–9. [DOI] [PubMed] [Google Scholar]
- 38.Abdelkafy A, Said HG.. Neglected ununited tibial eminence fractures in the skeletally immature: arthroscopic management. Int Orthop 2014. [DOI] [PubMed] [Google Scholar]
- 39.Verdano MA, Pellegrini A, Lunini E, et al. Arthroscopic absorbable suture fixation for tibial spine fractures. Arthrosc Tech. 2013;3:e45–8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Wiegand N, Naumov I, Vámhidy L, Nöt LG. Arthroscopic treatment of tibial spine fracture in children with a cannulated Herbert screw. Knee 2014;21:481–5. [DOI] [PubMed] [Google Scholar]
- 41.Ochiai S, Hagino T, Watanabe Y, et al. One strategy for arthroscopic suture fixation of tibial intercondylar eminence fractures using the Meniscal Viper Repair System. Sports Med Arthrosc Rehabil Ther Technol. 2011;3:17. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Matthews DE, Geissler WB. Arthroscopic suture fixation of displaced tibial eminence fractures. Arthroscopy 1994;10:418–23. [DOI] [PubMed] [Google Scholar]
- 43.Oostvogel HJ, Klasen HJ, Reddingius RE. Fractures of the intercondylar eminence in children and adolescents. Arch Orthop Trauma Surg 1988;107:242–7. [DOI] [PubMed] [Google Scholar]
- 44.Lowe J, Chaimsky G, Freedman A, et al. The anatomy of tibial eminence fractures: Arthroscopic observations following failed closed reduction. J Bone Joint Surg Am 2002; 84:1933–38. [PubMed] [Google Scholar]
- 45.Kobaysashi S, Terayama K. Arthroscopic reduction and fixation of a completely displaced fracture of the intercondylar eminence of the tibia. Arthroscopy 1994;10:231–35. [DOI] [PubMed] [Google Scholar]
- 46.Lehman RA Jr, Murphy KP, Machen MS, Kuklo TR. Modified arthroscopic suture fixation of a displaced tibial eminence fracture. Arthroscopy 2003;19:E6. [DOI] [PubMed] [Google Scholar]
- 47.Ando T, Nishihara K. Arthroscopic internal fixation of fractures of the intercondylar eminence of the tibia. Arthroscopy 2003; 19:54–61. [DOI] [PubMed] [Google Scholar]
- 48.Senekovic V, Veselko M. Anterograde arthroscopic fixation ofavulsion fractures of the tibial eminence with a cannulated screw: five-year results. Arthroscopy 2003;19:54–61. [DOI] [PubMed] [Google Scholar]