Abstract
Background
Treatment of cellulite using a 1440-nm YAG wavelength laser with side-firing fiber has proven safe and effective, lasting at least 6 months.
Objectives
The authors evaluate the safety and efficacy of a single, subdermal procedure to treat the underlying structure of cellulite for at least 1 year.
Methods
Fifty-seven patients underwent a 3-step cellulite treatment with a 1440-nm Nd:YAG laser with a side-firing fiber and temperature-sensing cannula. Efficacy was measured by the blinded evaluators to distinguish baseline photos from those taken at 12 months posttreatment, with results on a 5-point, 2-category ordinal photonumeric scale when comparing baseline photos to 12 months posttreatment. Subject and physician satisfaction was assessed based on completion of a satisfaction survey. Adverse events (AE) were recorded throughout the study. Twelve month data were analyzed and compared to 6 month data.
Results
Evaluators chose baseline photographs 97% on average from 6 (−1, +2) months and 91% from the 12 (−3, +2) months posttreatment photographs. At 6 (−1, +2) months, the average improvement score was 1.7 for dimples and 1.1 for contour irregularities. At 12 (−3, +2) months, the average improvement score was 1.4 for dimples and 1.0 for contour irregularities. The average satisfaction score for the physician was 5.6 and the patient was 5.3 on a 6-point scale.
Conclusions
A single, 3-step, minimally invasive laser treatment using a 1440-nm Nd:YAG laser, side-firing fiber, and temperature-sensing cannula to treat the underlying structure of cellulite proved to be safe and maintained effectiveness at least 1 year post treatment.
Level of Evidence: 2
 Therapeutic
Therapeutic
The underlying structure of cellulite has been studied and explained by histology and magnetic resonance imaging (MRI).1 In normal skin, the hypodermal fat layer is divided into chambers by septae. The fibrous tissue strands extend from the dermal layer, through the hypodermal fat layer, and connect to the underlying muscle layer. However, in women with cellulite, the septae sclerose contract, holding the skin at an inflexible length, while hypodermal fat lobules extend upward into the dermis. These structural changes cause a heterogeneous effect on the skin surface which affects at least 85% of post-pubertal women.2 With age, the integrity of the dermis is further compromised as skin thickness and elasticity decreases.3 Treating any or all of the anatomical features of cellulite restores the skin to a more homogenous state, reducing the appearance of cellulite.
Many treatment methods are available to treat cellulite such as massage,4 low-level light energy therapy from laser light,5 intense pulse light, radiofrequency,6 diode laser, infrared light, and ultrasound with and without mechanical massage as well as injectables and topicals7-15 and subcision, both mechanical and thermal.16-17 The results of these studies have reported mild and temporary improvement.
In 2008, the first use of a laser procedure to treat cellulite subdermally was reported.1 In that study, the authors reported 84.6% of patients rated the results from treatment as either good or excellent. In 2011, a report was published of 10 patients treated with a 1440-nm Nd:YAG laser and a newly developed fiber with a precise delivery capability (SideLight 3D; Cynosure, Westford, MA) enclosed in a thermal-sensing cannula (ThermaGuide; Cynosure).2 This new fiber technology provided a highly targeted means of delivering laser energy into the targeted anatomical structures underlying the cellulite. The thermal-sensing cannula is integrated with the laser delivery system to provide a safe and even distribution of energy to the treatment site. At one year, study findings showed mean skin thickness and skin elasticity increased significantly. Subjective physician and subject evaluation indicated improvement, high subject satisfaction, and minimal adverse events.
METHODS
An IRB (Independent Investigation Review Board INC, Plantation, FL, ), FDA-approved multicenter studied was conducted beginning in November 2010 and 6 month data were published.18 The same group of patients were provided an optional 1 year follow-up to assess longer term results which are reported in this study and evaluated from the period of November 2011 through April 2012.
Pretreatment
A total of 57 female patients at five study centers for this IRB-approved clinical trial were enrolled and treated. Prospective patients were excluded from participation in the trial if any of the following were present: surgical/nonsurgical treatment for cellulite in past 6 months; history of thrombophlebitis, acute infections, heart failure or keloid formation; recent antiplatelet, anticoagulant, thrombolytic, vitamin E or anti-inflammatory therapy; intolerance to anesthesia or medications which produce a photosensitizing effect; pregnant, breast feeding or planning a pregnancy, or unable to maintain a diet and exercise routine during the study period.
Patients who met the inclusion/exclusion criteria were consented. Basic chemistry panel was taken typical to standard practice for surgery, and patients were given antibiotics to be taken the evening prior to treatment and continued 7 days posttreatment. Weight was recorded and photographs were taken pretreatment and at all follow-up visits.
Treatment
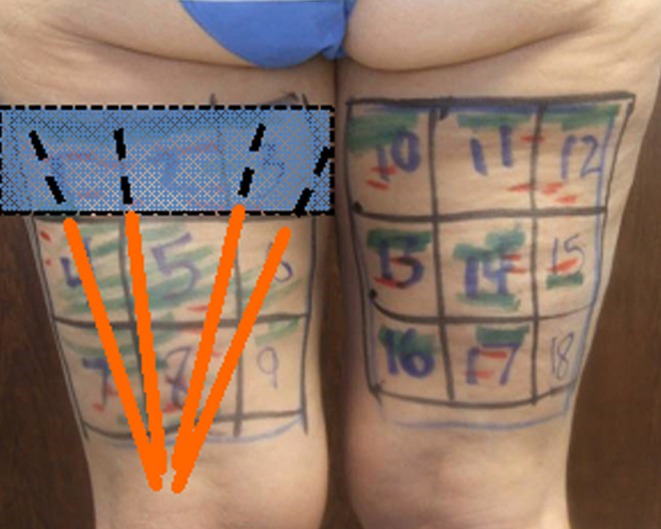
With the patient in a standing position, a treatment grid of 5 cm × 5 cm squares (sector) was marked over the treatment area. Lumps at least 3 cm × 3 cm square were marked in green, and dimples at least 1 cm long were marked in red (Figure 1).
Figure 1.
The total treatment dosage in joules is based upon the size of the area, the evaluation of the skin, and the grade of cellulite. The average amount of joules used in this study was 1000 J per 5×5 cm2. Generally in step 1, 300 joules are allocated for mounds 3 cm and 600 joules for mounds 5 cm. In step 2, 100 joules are allocated for dimples 1 cm, 300 joules for dimples 3 cm and 5cm dimples received 600 joules. In step 3, the remaining joules are applied to the skin subdermally, up to approximately 1000 joules. Deposition of up to an additional 300 to 500 joules/square was allowed in addition to 1000 joules at the investigator's discretion for more complex presentations, such as thicker fibrous bands and larger fat mounds.
With the patient positioned either in the lateral decubitus or prone position, the skin was prepared with povidone-iodine antiseptic. A small amount of lidocaine was injected at chosen injection sites. Using a small blade, 1 mm incisions were made. Distal incision points at the lower border of the marked grid were preferred for proper drainage posttreatment. Proximal incisions at the upper border of the marked grid were made as necessary. Each defined sector was infused with up to 60 mL of tumescent anesthesia mixture (50 mL of 0.5% lidocaine, 1 mg epinephrine per liter of warm saline, and 20 mL of 8.4% sodium bicarbonate).
Patients underwent a single procedure with the 1440-nm laser in the bilateral thighs and/or buttocks. The cannula with side-firing fiber tip was passed through the incisions, delivering energy at 8 to 10 Watts and 25 Hz. The temperature-sensing cannula was set to monitor subdermal temperatures, and would sound at a minimum of 47°C and a maximum of 52°C.
Four to six squares were treated at one time. A 3-step procedure was used.2,18 In step 1, the laser cannula-fiber is placed in the down position 1 to 2 cm below the dermis within the selected 5 × 5 cm squares and passed in a fan-shaped manner to treat the excess hypodermal fat; step 2, the cannula-fiber is moved sideways in a fanning pattern perpendicular to the marked depressions 3 to 5 mm below the dermis to subsize taut septal bands and release dimples; step 3, the fiber is placed in the superficial position 1 to 3 mm below the dermis to heat the entire skin in the 5 cm × 5 cm square to increase skin collagen and elastin for tissue tightening and dermal thickening (Figures 2-4).2
Figure 3.
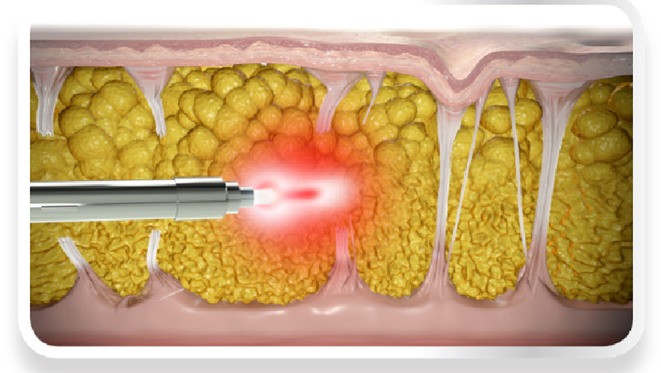
Illustration of bidirectional fiber performing laterally directed thermal subcision for the disruption of depressed vertical septae. Reprinted with permission from Cynosure (Westford, Massachusetts).
Figure 2.
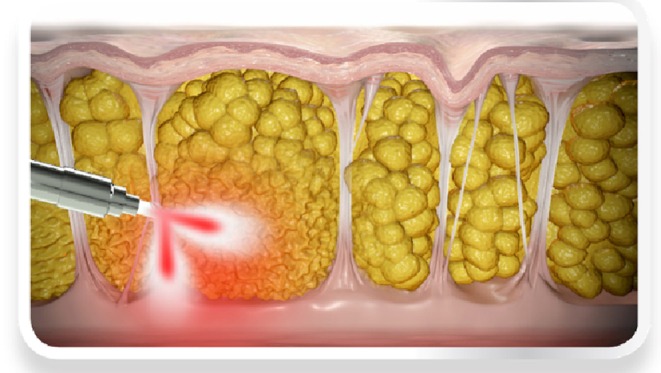
Illustration of bidirectional fiber performing disruption of the deeper fat to lessen the height of the raised mounds. Reprinted with permission from Cynosure (Westford, Massachusetts).
Figure 4.
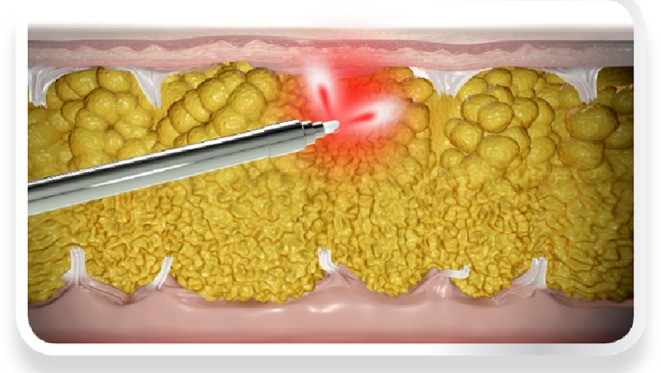
Illustration of bidirectional fiber performing delivery of superficial energy to the dermis. Reprinted with permission from Cynosure (Westford, Massachusetts).
Following laser treatment, aspirate generated by the cellulite treatment is removed through soft tissue massage and milking, to allow an effluent of the tumescent fluid and some small amounts of the liquefied fat, serum, and blood to be drained through the access incisions. A rolled-up towel or medical roller was sometimes used to facilitate the process. Standard pressure dressings were applied to the treated areas, and patients were instructed to wear a compression garment for the next 2 to 3 weeks. Standard practice postoperative instructions were given. Patients were informed of common side effects such as bruising, swelling, pain, numbness, and itching that may occur.
A camera system (Canfield Scientific, Fairfield, NJ) was set-up in each of five clinical centers. Dedicated photography rooms were used and a mat was used to repeat positioning. A lumen meter was used to record the exact amount of light falling on the patient. The photographs of thighs and buttocks were taken in a standardized manner; in the same room, with the same camera fixed at the same location by the same person hired for reproducibility.
RESULTS
Demographics
Of 57 subjects treated at baseline, 47 (82%) were present for the 6 (−1, +2) months evaluation representing 5 study centers and 30 (53%) patients returned for the 12 (−3, +2) months visit representing 4 study centers (Table 1). The original 57 patients had an average age of 43.3 years (range, 21-55 years), and body mass index (BMI) of 25.1 (range, 20-33). The 47 patients with a six month follow-up had an average age of 42.8 years (range, 21-55 years) and BMI of 25.0 (range, 20-33). The 30 patients with a one year follow-up had an average age of 41.8 years (range, 21-55 years) and BMI of 25.1 (range, 21-31). The majority of patients were of Caucasian and Hispanic descent with Fitzpatrick Skin Types of mostly type II and III (Table 2).
Table 1.
Number of Patients per Clinical Center
| Months | Center |
|||||
|---|---|---|---|---|---|---|
| 1 | 2 | 3 | 4 | 5 | Total | |
| 0 (Baseline) | 10 | 7 | 12 | 13 | 15 | 57 |
| 6 (−1,+2) Months | 5 | 5 | 11 | 12 | 14 | 47 |
| 12(−1,+2) Months | 0 | 3 | 8 | 8 | 11 | 30 |
Table 2.
Patient Demographics
| Baseline (N = 57) | 6 (−1, +2) Months (N = 47) | 12 (−3, +2) Months (N = 30) | |
|---|---|---|---|
| Age [SD (Min-Max)] | 43.3 [8.7 (21-55)] | 42.8 [8.9 (21-55)] | 41.8 [9.3 (21-55)] |
| BMI [SD (Min-Max)] | 25.1 [3.0 (20-33)] | 25.0 [3.1 (20-33)] | 25.1 [2.9 (21-31)] |
| Fitzpatrick Score | |||
| I | 8 | 8 | 4 |
| II | 21 | 17 | 12 |
| III | 23 | 18 | 11 |
| IV | 3 | 3 | 2 |
| V | 1 | 1 | 1 |
| Race | |||
| African American | 2 | 2 | 2 |
| Caucasian | 43 | 35 | 22 |
| Hispanic | 12 | 10 | 6 |
Identifying Treatment Time points
Evaluators were asked to identify the pretreatment (baseline) photographs from the 6 (−1, +2) month and 12 (−3, +2) month posttreatment photographs.
Six Month (−1, +2) Evaluation
Each of the 47 subjects had 2 treatment sites (thighs or buttocks) to be assessed, totaling 94 photographs. However, only 62 sites were evaluable because 32 photographs were of inadequate quality. Therefore 62 pairs of treatment area photographs were analyzed in paired analysis (62 baseline, 62 six months posttreatment photographs). For the 62 paired photographs, 97% (average) of the baseline photographs were correctly chosen by the evaluators (Table 3).
Table 3.
Percentage of Correct Selection of Baseline Photographs
| Evaluator | 6 (−1, +2) Months (n = 62) | 12 (−3, +2) Months (n = 52) | P Valuea |
|---|---|---|---|
| 1 | 60 (97) | 48 (92) | <.001 |
| 2 | 59 (95) | 47 (91) | <.001 |
| 3 | 61 (98) | 47 (91) | <.001 |
| Average % evaluators | 97 | 91 |
For the 47 subjects at 6 months there were 94 treatment sites, of which 62 (66%) were suitable for photographic evaluation. For the 30 subjects at 12 months there were 60 treatment sites, of which 52 (87%) were suitable for photographic evaluation. aThe P value is based on a chi-square test. P values < .001 shows statistical significance that the selection of baseline photographs is not based on random selection.
Twelve Month (−3, +2) Evaluation
Each of the 30 subjects had 2 treatment sites to be assessed totaling 60 photographs. However, only 52 sites were evaluable because 8 photographs were of inadequate quality. Therefore 52 treatment area photographs were analyzed in paired analysis (52 baseline, 52 twelve months posttreatment photographs). For the 52 paired photographs, 91% (average) of the baseline photographs were correctly chosen by the evaluators (Table 3).
Level of Improvement
A validated scale was designed that presented two main clinical morphologic features of cellulite (categories): (A) number of evident dimples (Figure 5); and (B) severity of linear undulations (contour irregularities) (Figure 6). The severity of each category was graded on a 5-point scale (0-4).18 Responder rates were then calculated. A responder is defined as a treatment site having a baseline score greater than zero with an improvement score equal to or greater than one. Inter-rater reliability was determined by comparing paired evaluator scores and expressed as a weighted Kappa value. Kappa values above 0.50 were recognized as demonstrating reasonable agreement.
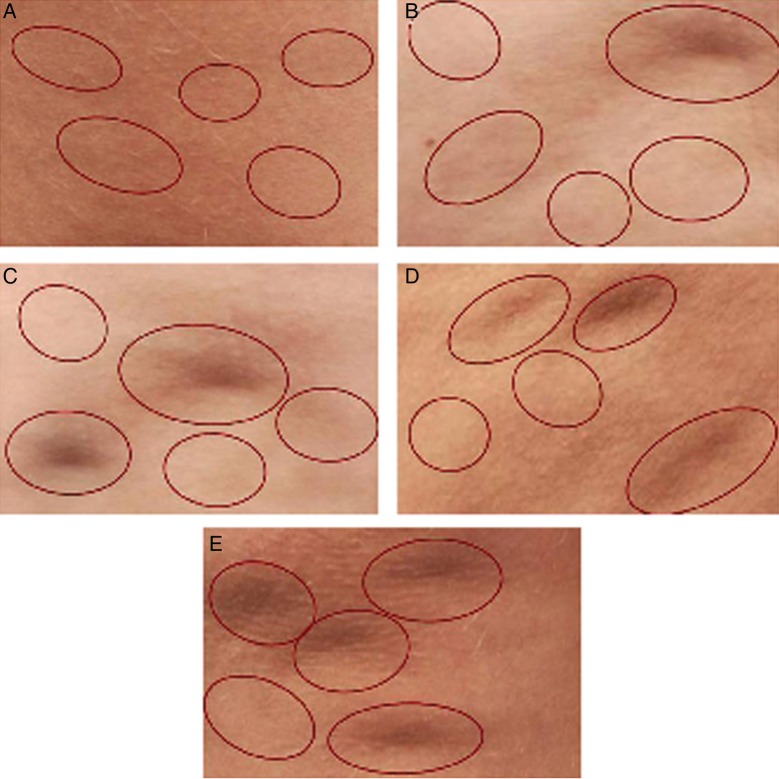
Figure 5.
Scale for evaluating cellulite dimples, in which a dimple is an isolated circular or oval-shaped depression on the surface of the skin. Each photo represents a number of dimples. Five circles are placed in each photo for evaluation purposes. The circle may or may not contain a dimple. This is done so the evaluator is not confused by nondimpling irregularities, but not biased by being told exactly where the dimples are located. (A) Score 0 (no dimples); (B) score 1 (1 dimple); (C) score 2 (2 dimples); (D) score 3 (3 dimples); (E) score 4 (4 or more dimples). From DiBernardo et al18 reprinted with permission from Oxford University Press.
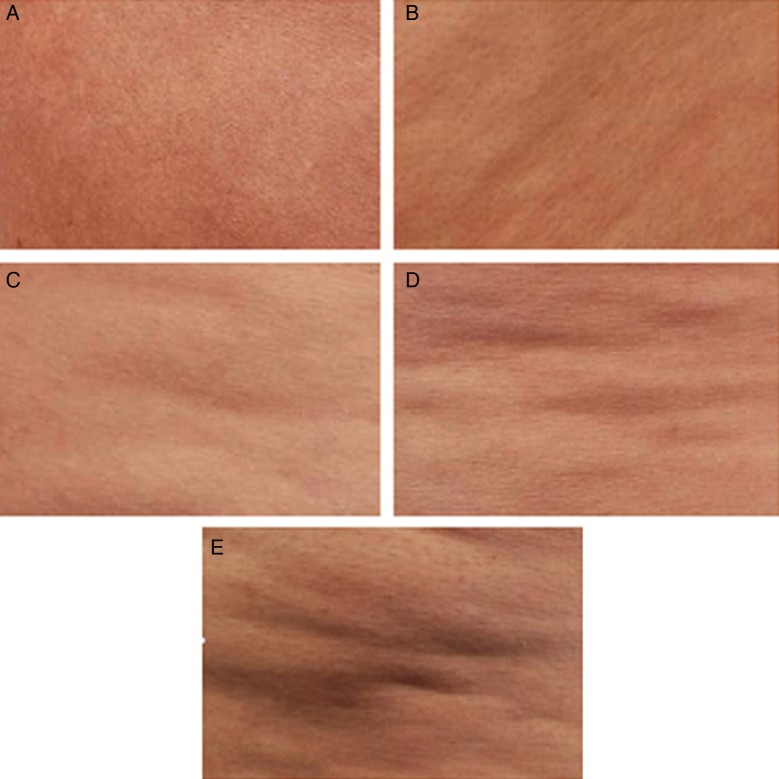
Figure 6.
Scale for evaluating contour irregularities. The irregularities become more severe as more concavity and convexity occur in the linear undulations. (A) Score 0 (none—no depressions or raised areas); (B) score 1 (superficial: generalized, small depressions with no protuberances; (C) score 2 (mild: pattern of mild linear undulations with alternating areas of protuberances and depressions); (D) score 3 (moderate: pattern of moderate linear undulations with alternating areas of protuberances and depressions); (E) score 4 (severe: severe generalized linear undulations with alternating areas of protuberances and depressions). From DiBernardo et al18 reprinted with permission from Oxford University Press.
Six Month (−1, +2) Evaluation
One of the 62 treatment sites evaluated at 6 months did not have dimples at baseline. Fifty-eight of 61 (95%) of dimpled treatment sites and 61 of 62 (98%) contour irregularity sites had at least a ≥1 score improvement (Table 4). The average improvement score was 1.7 for dimples and 1.0 for contour irregularities (Table 4).
Table 4.
Responder Improvement Scores
| Responder (Treatment Sites) With ≥1 Score Improvement per Category | ||||
|---|---|---|---|---|
| 6 (−1, +2) Months |
12 (−3, +2) Months |
|||
| Dimples | Contour | Dimples | Contour | |
| Baseline score > 0 | 61 | 62 | 51 | 51 |
| Improvement score ≥ 1 | 58 | 61 | 46 | 46 |
| % Improvement | 95 | 98 | 90 | 90 |
Twelve Month (−3, +2) Evaluation
One photograph of the 52 treatment sites at 12 months (−3, +2) did not have dimples and one site did not have contour irregularities at baseline. Forty-six of 51 (90%) treatment sites with dimples and contour irregularities had at least a ≥1 score improvement. The average improvement score was 1.4 for dimples and 1.0 for contour irregularities (Table 4).
Satisfaction
Physician and subject satisfaction was assessed by a questionnaire based on a 6-point Likert Scale: 6 = extremely satisfied, 5 = satisfied, 4 = slightly satisfied, 3 = slightly dissatisfied, 2 = dissatisfied, and 1 = extremely dissatisfied.
Patients were provided a satisfaction survey with the patient ID on the survey and asked to respond to the questionnaire at the physician's office immediately prior to meeting with the physician. The physician segment was completed by the physician after the follow-up visit.
At the 6 month visit, 45 subjects had completed questionnaires and the average score for the physician was 5.4 and the subject was 5.0.
At the 12 month visit, 11 subjects had completed questionnaires and the average score for the physician was 5.6 and the subject was 5.3 (Table 5).
Table 5.
Physician and Patient Satisfaction
| 6 (−1, +2) Months | 6 (−1, +2) Months | 12 (−3, +2) Months | 12 (−3, +2) Months | |
|---|---|---|---|---|
| Physician N = 45 | Patient N = 45 | Physician N = 11 | Patient N = 11 | |
| Average Scorea | 5.4 | 5.0 | 5.6 | 5.3 |
| Mode | 6 | 5 | 6 | 6 |
aLikert 6-point scale: 6 = extremely satisfied, 5 = satisfied, 4 = slightly satisfied, 3 = slightly dissatisfied, 2 = dissatisfied, 1 = extremely dissatisfied.
Safety
The laser treatment continues to demonstrate an excellent safety profile. No adverse events reported at 12 months. Two representative cases are presented in Figures 7 and 8.
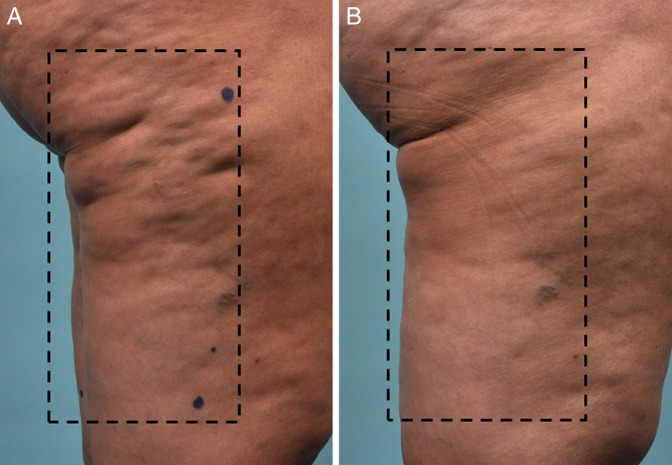
Figure 7.
(A) This 39-year-old woman presented with moderate-severe cellulite. (B) One year after a single treatment with the 1440-nm Nd:YAG laser. The dotted line encloses the treatment area.
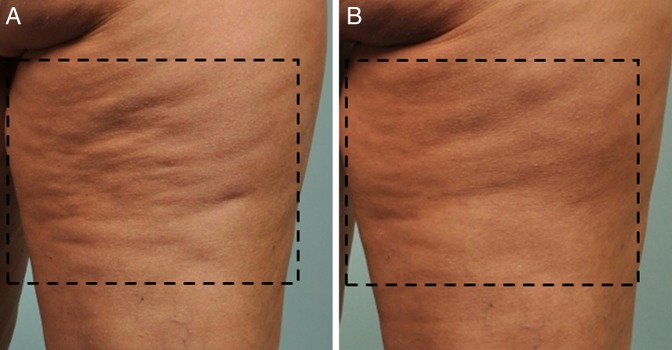
Figure 8.
(A) This 39 year-old woman presented with moderate cellulite. (B) One year after a single treatment with the 1440-nm Nd:YAG laser. The dotted line encloses the treatment area.
DISCUSSION
This multicenter study showed sustained improvement in the appearance of cellulite and continued safety following a single, 3-step cellulite treatment with the 1440-nm Nd:YAG side-firing laser through 12 months.
Since the 12 month visit was optional, the 12 month population consisted of 30 subjects (53%) compared to 47 subjects (82%) at 6 months (Table 1).
Data were analyzed separately per time point for each sub population. To show sustained efficacy over a 1 year period, the data were tested using a sub population of subjects that presented at the two time points of 6 and 12 months.
A chi-square test was used to statistically confirm that evaluators identifying pretreatment photographs exceeded the chance of random selection. The evaluators chose the baseline photographs 97% on average from 6 (−1/+2) months, and 91% from 12 (−3/ +2) photographs. The P value comparing 6 month and 12 month data was >0.05, confirming that there was no significant difference in efficacy between the 6 (−1/+2) month and 12 (−3/+2) month visits, and proving sustainability at 1 year (Table 3).
A paired t test was used to assess improvement scores based on the validated scale. At 6 (−1, +2) months, the average improvement score was 1.7 for dimples and 1.1 for contour irregularities. At 12 (−3, +2) months, the average improvement score was 1.4 for dimples and 1.0 for contour irregularities. The P value was >0.05 when comparing scores at 6 months vs 12 months, confirming no significant difference in improvement scores between the 6 (−1/+2) month and 12 (−3/+2) month time points (Table 6).
Table 6.
Average Improvement Scores Compared to Baseline Score
| 6 (−1, +2) Months | 12 (−3, +2) Months | |
|---|---|---|
| Total sites evaluated | 62 | 52 |
| Baseline Dimple Score | 2.2 | 2.3 |
| Follow up Dimple Score | 0.6 (P < .001) | 0.9 (P < .001) |
| Dimple Improvement Score | 1.7 | 1.4 |
| Baseline Contour Irregularity Score | 2.1 | 2.1 |
| Follow up Contour Irregularity Score | 1.0 (P < .001) | 1.1 (P < .001) |
| Contour Irregularity Improvement | 1.1 | 1.0 |
Data were consistent across clinical centers (Table 7). When improvement scores were analyzed relative to weight change, there was no correlation. Throughout the study, patient and physician satisfaction was high. Incidence of adverse events were recorded throughout the course of the study. No events were reported between 6 months and 12 months.
Table 7.
Responder Rates Per Clinical Center
| Centera | 6 (−1, +2) Months |
12 (−3, +2) Months |
||
|---|---|---|---|---|
| Treatment Sites Evaluated | Respondersb N (%) | Treatment Sites Evaluated | Respondersb N (%) | |
| 1a | 10 | 10 (100%) | NA | NA |
| 2 | 9 | 9 (100%) | 6 | 4 (67%) |
| 3 | 19 | 19 (100%) | 16 | 16 (100%) |
| 4 | 18 | 17 (94%) | 14 | 13 (93%) |
| 5 | 5 | 5 (100%) | 16 | 14 (88%) |
| Totals | 61 | 60 (97%) | 52 | 47 (90%) |
aCenter 1 had zero patients for the 12 month evaluation. bNumber and percentage of treatment sites with a ≥1 improvement response rate.
Potential limitations in a multicenter study such as this can be inconsistencies of measurements and photography from center to center. These effects are magnified with a condition such as cellulite due to the exact lighting that is required consistently and reproducible measurements for the ultrasound. To overcome these obstacles, third party photography was performed in each center (Canfield Scientific, Fairfield, NJ) and well as third party evaluation of the photographs. In addition, the same ultrasonographer was used on all patients, at all centers, and at all time points
CONCLUSION
The Cellulaze laser system provides a sustainable improvement in the appearance of cellulite for at least 1 year, as seen in this study. Other publications have shown results maintaining at least 3 years. Data to date have shown this single laser procedure to have an outstanding safety profile with a high satisfaction rate for both physicians and subjects.
Disclosures
All authors are paid research consultants for Cynosure, Inc., the manufacturer of the product discussed in this article.
Funding
The authors received financial support for the research study from Cynosure, Inc., the manufacturer of the product discussed in this article, which included equipment, writing assistance, and procedure costs for each patient.
REFERENCES
- 1.Goldman A, Gotkin RH, Sarnoff DS, Prati C, Rossato F. Cellulite: a new treatment approach combining subdermal Nd: YAG laser lipolysis and autologous fat transplantation. Aesthet Surg J. 2008;286:656-662. [DOI] [PubMed] [Google Scholar]
- 2.DiBernardo BE. Treatment of cellulite using a 1440-nm pulsed laser with one-year follow-up. Aesthet Surg J. 2011;313:328-341. [DOI] [PubMed] [Google Scholar]
- 3.Escoffier C, de Rigal J, Rochefort A, Vasselet R, Lévêque JL, Agache PG. Age-related mechanical properties of human skin: an in vivo study. J Invest Dermatol. 1989;933:353-357. [PubMed] [Google Scholar]
- 4.Güleç AT. Treatment of cellulite with LPG endermologie. Int J Dermatol. 2009;483:265-270. [DOI] [PubMed] [Google Scholar]
- 5.Sasaki GH. Scientific basis for the use of low level light energy on the treatment of cellulite. In: Cellulite. 2nd ed London, UK: Informa Healthcare; 2010:118-123. [Google Scholar]
- 6.Goldberg DJ, Fazeli A, Berlin AL. Clinical, laboratory, and MRI analysis of cellulite treatment with a unipolar radiofrequency device. Dermatol Surg. 2008;342:204-209. [DOI] [PubMed] [Google Scholar]
- 7.Alexiades-Armenakas M, Dover JS, Arndt KA. Unipolar radiofrequency treatment to improve the appearance of cellulite. J Cosmet Laser Ther. 2008;103:148-153. [DOI] [PubMed] [Google Scholar]
- 8.Alster TS, Tanzi EL. Cellulite treatment using a novel combination radiofrequency, infrared light, and mechanical tissue manipulation device. J Cosmet Laser Ther. 2005;72:81-85. [DOI] [PubMed] [Google Scholar]
- 9.Gold MH, Khatri KA, Hails K, Weiss RA, Fournier N. Reduction in thigh circumference and improvement in the appearance of cellulite with dual-wavelength, low-level laser energy and massage. J Cosmet Laser Ther. 2011;131:13-20. [DOI] [PubMed] [Google Scholar]
- 10.Lach E. Reduction of subcutaneous fat and improvement in cellulite appearance by dual-wavelength, low-level laser energy combined with vacuum and massage. J Cosmet Laser Ther. 2008;104:202-209. [DOI] [PubMed] [Google Scholar]
- 11.Nootheti PK, Magpantay A, Yosowitz G, Calderon S, Goldman MP. A single center, randomized, comparative, prospective clinical study to determine the efficacy of the VelaSmooth system versus the Triactive system for the treatment of cellulite. Lasers Surg Med. 2006;3810:908-912. [DOI] [PubMed] [Google Scholar]
- 12.Sadick NS, Mulholland RS. A prospective clinical study to evaluate the efficacy and safety of cellulite treatment using the combination of optical and RF energies for subcutaneous tissue heating. J Cosmet Laser Ther. 2004;64:187-190. [DOI] [PubMed] [Google Scholar]
- 13.Trelles MA, Mordon SR. Adipocyte membrane lysis observed after cellulite treatment is performed with radiofrequency. Aesthetic Plast Surg. 2009;331:125-128. [DOI] [PubMed] [Google Scholar]
- 14.Trelles MA, van der Lugt C, Mordon S, Ribé A, Al-Zarouni M. Histological findings in adipocytes when cellulite is treated with a variable-emission radiofrequency system. Lasers Med Sci. 2010;252:191-195. [DOI] [PubMed] [Google Scholar]
- 15.Wanner M, Avram M. An evidence-based assessment of treatments for cellulite. J Drugs Dermatol. 2008;74:341-345. [PubMed] [Google Scholar]
- 16.Orentreich DS, Orentreich N. Subcutaneous incisionless (subcision) surgery for the correction of depressed scars and wrinkles. Dermatol Surg. 1995;216:543-549. [DOI] [PubMed] [Google Scholar]
- 17.Hexsel DM, Mazzuco R. Subcision: a treatment for cellulite. Int J Dermatol. 2000;397:539-544. [DOI] [PubMed] [Google Scholar]
- 18.DiBernardo B, Sasaki G, Katz BE, Hunstad JP, Petti C, Burns AJ. A multicenter study for a single, three-step laser treatment for cellulite using a 1440-nm Nd:YAG laser, a novel side-firing fiber, and a temperature-sensing cannula. Aesthet Surg J. 2013;334:576-584. [DOI] [PubMed] [Google Scholar]