Abstract
Background:
Chronic obstructive pulmonary disease (COPD) is a common disease with important healthcare, social, and economic consequences. The aim of this study was to analyze the costs of hospitalizing patients with COPD.
Materials and Methods:
In this state-level cross-sectional study, data from 165 COPD patients who had presented to our hospital between April 1, 2011 and March 31, 2013 were reviewed retrospectively. Patients were eligible for inclusion if they had a diagnosis of COPD [international classification of diseases-10 (ICD-10) code J44]. Costs of COPD patients were calculated by multiplying the amount of services used by the unit cost. Finally, we used multivariate regression analysis to determine predictors of hospital costs.
Results:
Mean (SD) age of the patients was 68.6 ± 12 years and 65.5% of them were ≥ 65. The mean (SD) and median length of stay (LOS) for patients were 8.5 ± 11.5 and five days [IQR 3; 9], respectively. All hospital cost drivers had significant relationships with LOS, and the mean cost per patient was higher in patients with hospital LOS longer than nine days. Prolonged LOS (LOS > 9 days) involved 830 bed/days. Therefore, the mean cost per each extra day of hospital stay was estimated to be US $115.80. The mean costs per patient with and without hypertension were US $1,422.5 and US $627.4, respectively (P=0.017).
Conclusion:
Hospitalization and medication costs were the two major cost drivers for patients hospitalized with COPD exacerbation. Duration of hospital stay, history of hypertension, and the number of clinical consultations other were significant predictors associated with hospital cost in patients with COPD.
Keywords: Hospital Costs, Chronic Obstructive Pulmonary Disease, Length of Stay
INTRODUCTION
Chronic obstructive pulmonary disease (COPD) is a common and preventable chronic disease with considerable health related and economic consequences (1–3). COPD is one of the leading causes of morbidity and mortality in the world (4, 5). The prevalence of COPD is continually rising and by 2020 COPD is predicted to be the third leading cause of death in the worldwide (4, 6). It is the third major cause of death in the United States and 70% of the 24 million patients with COPD are < 65 (7). Mathers et al. reported that by 2030 COPD will be the fifth and tenth leading causes of disability adjusted life years (DALY) in middle-income and high-income countries, respectively (8). A study reported that the prevalence of COPD in Iran and some other countries was approximately the same (9). COPD death rate and DALY in Iran were estimated to be 26.3 and 395/100,000, respectively, which were nearly 5.9-, and 3.2 times higher than those in Japan (10).
Chronic obstructive pulmonary disease has a major effect on healthcare costs, particularly direct medical costs (11). Most studies of costs associated with COPD have shown significant associations between disease severity and economic burden of COPD exacerbation and diseases severity (3). In 2010, COPD was responsible for $49.9 billion in direct and indirect costs in the United States (12). A study from the United States showed that the total cost of hospitalized patients with COPD was approximately $6,000.00 higher than that of hospitalized patients without COPD (13). A study from Iran reported that the mean duration of hospital stay, which was the main driver of direct cost, was 11.82 days for patients with COPD exacerbation (14). Hilleman et al. showed that the cost of hospital stay accounted for 40.4% and 62.6% of total costs for patients with mild and severe COPD, respectively (15). Another study showed that hospitalization costs represented 70% of all COPD-related medical care costs (16). Predicting the cost of caring for patients with common chronic diseases is important for prioritizing health care utilization and policy making (17). Very few studies have estimated the costs associated with COPD in Iran. The aim of this study was to analyze factors influencing costs of caring for patients hospitalized with acute exacerbation of COPD.
MATERIALS AND METHODS
Patients and study setting
The study sample consisted of 165 patients with diagnosis of COPD who were admitted to a referral public university hospital (Imam Khomeini hospital), which is affiliated with Ahvaz Jundishapur University of Medical Sciences, for severe acute exacerbation of COPD. The hospital was refunded by public insurances such as social security medical insurance, Iranian health insurance, military forces medical insurance, and the rural health insurance, which cover 80–90% of the fees for hospitalized patients. Approximately 10–20% of the hospitalization costs are paid out of pocket by the patients
Data collection
Data were collected retrospectively by reviewing billing data from April 1, 2011 to March 31, 2013. Patients were eligible for inclusion if they had been diagnosed with COPD (ICD-10 code J44). We studied consecutive patients who were hospitalized for the first time with COPD exacerbation. We extracted data from the computerized medical records of the hospital. The following variables were included based on a literature review: patient’s age, sex, marital status, place of living (urban vs. rural), medical insurance source (public vs. private), length of hospital stay, the number of clinical consultations obtained, and other comorbidities.
Cost calculation
Patient-level costs of COPD were calculated by multiplying the amount of resources utilized, including medications, imaging services, medical consults, nursing care, cost of hospital room, and laboratory services by the unit cost. Costs in Iranian currency (Rial) were subsequently converted into American dollar values (US$), using the official price list of the Iranian Central Bank, where US $1 was equal to 11,000 Rials in 2011, 12,300 Rials in 2012, and 17,000 Rials in 2013, on average. We considered inflation over the three year period when calculating costs to patients. We used the following equation to calculate costs of care:
Statistical analysis
Continuous data were reported as mean ± standard deviation or median [interquartile range (IQR)], while categorical data were reported as percentages. Since hospitalization costs and LOS data were skewed, we used non-parametric statistical tests such as the Mann-Whitney U test, Kruskal Wallis test, and Spearman’s coefficient for univariate analysis. In this study, the residuals of dependent variable, which are differences between the observed value of the dependent variable (y) and the predicted value (ŷ), were normally distributed. Therefore, we used multivariate regression analysis to determine predictors of hospitalization costs and LOS over nine days (corresponding to > 75th percentile) (18, 19). The multivariate analysis initially included variables from the univariate analysis with P < 0.05. Stepwise approach was used to model independents variables. We considered P < 0.05 as statistically significant. We used SPSS version 20 (IBM Corporation, Armonk, NY, USA) for data analysis. Given the retrospective nature of our study, informed consent was not required.
RESULTS
We reviewed the records of 165 patients, 72.7% of which were men. Mean (SD) age of the patients was 68.6 ± 12 years and 65.5% of them were ≥ 65 years old. Furthermore, 91.5% of the patients lived in urban areas. The patients were covered by medical insurance funds including social security (41.8%), Iranian Health insurance (10.9%), armed forces Insurance (2.4%) and rural insurance (23%). About 12.1% of the patients were uninsured and more than half of the patients (58.2%) were active smokers. The most frequently present comorbidity in our study population was hypertension, which was present in 40.6% of patients. Twenty eight percent of the patients had diabetes mellitus, 15.2% suffered from orthopnea, and 11.5% of the patients suffered from asthma. Furthermore, our results showed a significant relationship between hospital costs per patient and past medical history of hypertension (P=0.017) and family history of COPD (P=0.036). The mean cost per patient was US $1,422.5 for patients with hypertension, compared to US $627.4 for those without it. The cost per patient for patients with a family history of COPD was 1.3 times higher than that for patients without a family history of COPD (US $1,253 vs. US $932.8). The mean hospital cost per patient for patients over 65 years of age was 1.3 times higher compared to that for younger patients (Table 1). Also, according to Spearman’s rank correlation coefficient, there were significant relationships between patients’ age and LOS with the mean of hospital costs (P=0.022; coefficient of correlation 0.178, P=0.001; coefficient correlation 0.658).
Table 1.
Demographic and clinical characteristics of patients by mean hospital costs
| Variable | N (%) | Mean cost (US$) | Std. deviation | Median | CI (95%) for mean | P-value |
|---|---|---|---|---|---|---|
| Age | ||||||
| <65 | 57(34.5) | 791 | 1744 | 290 | [329; 1254] | 0.118 |
| >65 | 108(65.5) | 1033 | 1614 | 474 | [725; 1341] | |
| Female | 45(27.3) | 1251 | 2287 | 378 | [564 ; 1939] | 0.863 |
| Male | 120(72.7) | 837 | 1345 | 386 | [594; 1080] | |
| Urban | 151(91.5) | 941 | 1662 | 386 | [674; 1209] | 0.472 |
| Rural | 14(8.5) | 1043 | 1678 | 275 | [74; 2012] | |
| Type of medical insurance | ||||||
| uninsured | 20(12.1) | 1613 | 2762 | 278 | [320 ; 2906] | |
| Social security insurance | 69(41.8) | 929 | 1722 | 396 | [515 ; 1343] | |
| Iranian health insurance | 18(10.9) | 1155 | 1599 | 658 | [360 ; 1951] | |
| Rural health insurance | 38(23) | 648 | 946 | 336 | [337 ; 959] | 0.137 |
| Military medical insurance | 4(2.4) | 1497 | 1027 | 1258 | [−136; 3132] | |
| Others | 16(9.7) | 559 | 733 | 236 | [168 ; 950] | |
| Family History | 9(5.5) | 1253 | 1121 | 921 | [391 ; 2114] | 0.036 |
| Disease history | 21(12.7) | 716 | 810 | 535 | [347 ; 1085] | 0.488 |
| Hypertension | 67(40.6) | 1422 | 2342 | 448 | [851 ; 1993] | 0.017 |
| Diabetes | 46(27.9) | 928 | 1833 | 339 | [384 ; 1473] | 0.366 |
| Hyperlipidemia | 6(3.6) | 1332 | 2491 | 357 | [−1282; 3947] | 0.734 |
| Myocardial Infraction | 4(2.4) | 946 | 1253 | 334 | [−1048; 2941] | 0.695 |
| Smoking | 96(58.2) | 964 | 1615 | 361 | [636 ; 1291] | 0.692 |
| Orthopnea | 25(15.2) | 1447 | 1886 | 386 | [668 ; 2225] | 0.177 |
| Asthma | 19(11.5) | 854 | 1222 | 386 | [265 ; 1443] | 0.980 |
| Cerebra Vascular Attack | 7(4.2) | 1114 | 1891 | 216 | [−635; 2864] | 0.588 |
CI: Confidence Interval
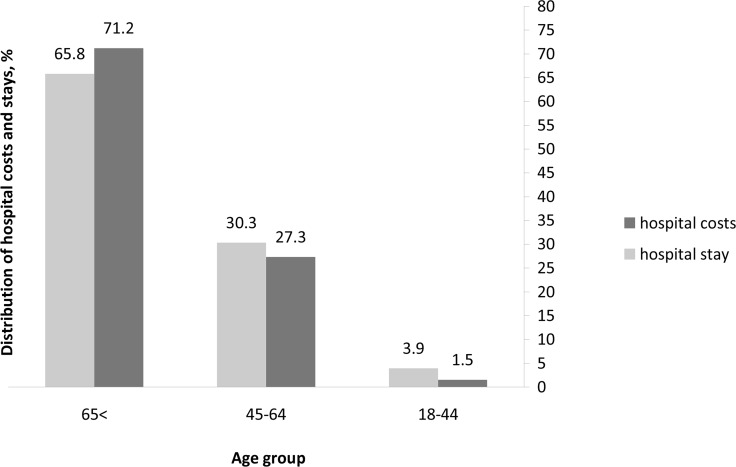
According to figure 1, adults under the age of 65 accounted for nearly two-thirds of the aggregate hospital costs and hospital stays between 2011–2013. Adults between 45–64 years of age and those over 65 also had the highest mean hospital costs (US $1,034 and US $825.2, respectively).
Figure 1.
Distribution of mean costs and hospital stays based on patient’s age groups
According to Table 2, all cost drivers for LOS > nine days were higher significantly (P<0.05). The mean (SD) and median LOS for patients were 8.5 ± 11.5 and five days [IQR 3; 9], respectively. In this study, LOS less than, or equal to nine days was determined as the cut off point for prolonged LOS. Mean cost per patient was US $2,465.4 for patients with LOS ≥ nine days compared to $481.3 for patients with LOS < nine days. Hospitalization cost (cost per hospital day) and medication costs were the major drivers of cost in the two patient groups. Prolonged LOS (LOS ≥ 9 days) accounted for 830 bed/days. Therefore, mean cost per each extra day of hospitalization was estimated to be US $115.8 (US $496,152.5/830 days).
Table 2.
Mean cost (US$) per COPD patient based on length of stay (day)
| Services | Mean cost for patients with LOS ≤ 9 days (n=126) [95% CI] | Mean cost for patients with LOS > 9 days (n=39) [95% CI] | P-value | ||||
|---|---|---|---|---|---|---|---|
| Mean | Median | SD | Mean | Median | SD | ||
| Nursing services | 18 [9;27] | 7 | 49 | 93 [51; 135] | 55 | 128 | 0.001 |
| Laboratory | 54 [41; 67] | 34 | 73 | 175 [123;226] | 140 | 158 | <0.001 |
| Radiology | 5 [3;7] | 2 | 12 | 17 [10;23] | 10 | 20 | <0.001 |
| Medicines | 134 [85;183] | 69 | 279 | 579 [352;806] | 334 | 699 | 0.001 |
| Hospitalization | 231 [171;290] | 119 | 336 | 1481 [901;2061] | 971 | 1788 | <0.001 |
| Consultation | 22 [15; 29] | 10 | 38 | 86 [56; 116] | 74 | 93 | 0.001 |
| Other services | 15 [12; 18] | 10 | 16 | 31 [22; 40] | 29 | 27 | <0.001 |
| Total mean cost | 481 [371;591] | 283 | 623 | 2465 [1576;3354] | 1788 | 2741 | 0.001 |
CI: confidence interval.
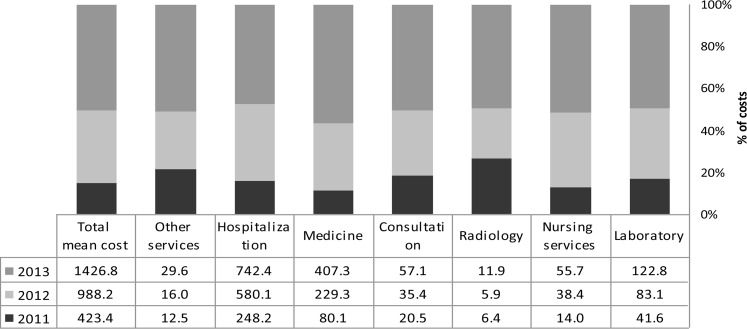
Figure 2 depicts mean hospital costs from 2011 to 2013 based on cost drivers. Our results showed that the mean cost per patient was US $423.3 in 2011, US $988.2 in 2012, and US $1,426.8 in 2013. Therefore, in 2013, mean cost per patient was 1.4 times higher than that in 2012.
Figure 2.
Distribution of The mean hospital cost (US$) of patients (2011–2013)
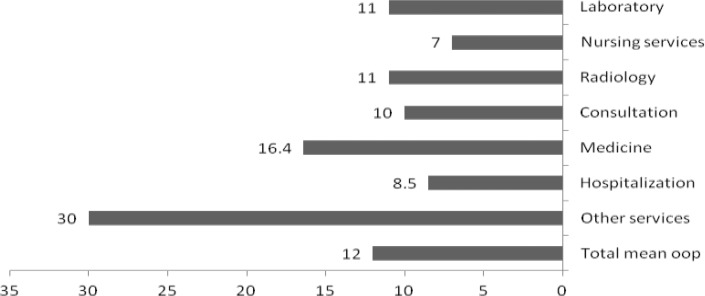
According to figure 3, the major determinants of out of pocket costs were para-clinical services (30%) and medications (16.4%), respectively. On average out of pocket cost per hospitalized patient accounted for 12% of the total cost of hospitalization.
Figure 3.
The mean of out of pocket costs by hospital services
According to multivariate regression analysis, the number of clinical consultations, LOS in days, and past medical history of hypertension were significant predictors of the total cost. Presence of hypertension increased mean hospital cost by US $346. Also, each extra day in hospital increased the mean cost by US $53.3 o (Table 3). The results of the multivariate regression model were presented by the following equation:
Y (cost) = −162.6+ the number of clinical consultation (161.3) + hospital stay (53.3) + hypertension (346)
Table 3.
Multivariate analysis of factors associated with hospitalization costs
| Variables | B | SE | T | p-value | 95% CI |
|---|---|---|---|---|---|
| (Constant) | −162.6 | 111.6 | −1.456 | 0.147 | [−383.2 ; 58] |
| No of medical consultations | 161.3 | 24.41 | 6.608 | <0.001 | [113.1 ; 209.6] |
| Duration of stay in days | 53.3 | 10.02 | 5.349 | <0.001 | [33.8 ; 73.3] |
| Hypertension | 346 | 111.7 | 2.165 | 0.032 | [113.1 ; 209.5] |
CI: Confidence interval; SE: Standard error
DISCUSSION
This cost analysis study was performed to evaluate the hospital costs associated with COPD over a three-year period (20). Hospitalization cost is the main source of direct medical cost for patients with COPD (21–23). Although only 10%–15% of patients with COPD will require hospitalization, hospitalization accounts for > 70% of all COPD-related medical costs (18). Hospitalization cost is mainly due to medication costs, clinical consultations, surgical services, intensive care unit (ICU) services, hospital beds, nursing services, and diagnostic tests. Our results show that the mean of hospitalization cost increased over the three-year period from US$ 423.3 in 2011 to US$ 2,436.2 in 2013. A similar study from the US showed that the mean hospital cost per patient in 2013 was 5.7 times higher than that in 2011. Other studies have also reported that the costs of caring for patients with COPD have been increasing in other countries as well (24). Stanford et al. showed that average annual percentage change in aggregate costs for COPD was 3.1% between 1997–2010 (25). According to Pfuntner et al, the mean actual cost per episode of severe COPD exacerbation was €1,711, €621 of which was reimbursed by the national social security funds (26). It should be noted that there are differences in COPD cost estimates between different countries. These differences are secondary to the use of different research hypotheses and methodologies, different sample sizes, data sources, the organizational structure of the health systems, and the sources of financing. Main variations are observed in costs of treatment and hospital stay between different countries (20). For example, in 2000 the annual direct cost of treatment and hospitalization for patients with COPD was $522 in France, $1,258 in Canada, $3,196 in Spain, and $4,119 in the US (27). In the current study, mean (SD) age of the patients was 68.6 ± 12 years and 65.5% of the patients were older than 65. According to our findings, older patients with COPD had higher hospital costs, which is consistent with prior reports (24–27). Elderly patients have more comorbidity, therefore they may require longer duration of intubation, longer ICU stays, and longer hospital stays (28). According to multivariate analysis, each extra day of hospital stay increased mean cost by $53.6. The length of hospital stay is the main driver of health care cost in patients with COPD. Geitona et al. reported that the length of hospital stay for severe COPD exacerbation was the major determinant of cost. Price discrepancies are observed between the actual and the nominal cost per patient in all stages of COPD. Reducing length of stay could result in substantial cost savings (20). Agency for Healthcare Research and Quality reported that hospital cost per stay for COPD patients was $6,400 in 1997 and $7,400 in 2010 (26). Also, this study showed that increasing the number of clinical consultations led to increased costs. Patients who required a higher number of specialty consultations also had longer LOS. Yoon et al. reported that specialty consultation was associated with prolonged hospital stay, and there was a significant difference between services consulted (29). Therefore, reducing inappropriate clinical consultations can reduce the LOS and hospital costs. It should be noted that analyzing the resource consumption is a useful technique to regulate the behavior of health care consumers and providers. The current study had some limitations; in this cost analysis, there were no data available regarding indirect costs, or costs related to ICU admissions. The studied hospitals did not provide any ICU data. Estimation of indirect costs is a difficult part of cost of illness studies and only a few studies have previously attempted to do so.
CONCLUSION
Our results showed that the costs of hospitalization for patients with COPD are increasing.. Similarly, our results showed that length of hospital stay and medication costs were the two major determinants of cost of care. Length of hospital stay, history of hypertension, and the number of specialty consultations were significant factors associated with hospitalization cost. Therefore, hospital managers and providers can reduce hospitalization costs of COPD patients by reducing excessive length of stay, managing the hospital bed, optimizing the number of medical consultations, implementing clinical guidelines, and better discharge planning. It should be noted that cost analysis studies are an important tool to improve hospital resource Utilization.
Acknowledgments
This study was part of a research project, which was granted (No. CDCRC-9410) and financially supported by the deputy vice chancellor for research affairs of Ahvaz Jundishapur University of Medical Sciences and chronic disease care research center. The authors would like to thank the deputy vice chancellor for research affairs of Ahvaz Jundishapur University of Medical Sciences and chronic disease care research center.
Footnotes
- Cost of illness and health economic are important tools for hospital resource utilization.
- Optimizing hospital resources utilization can lead to reduced costs for patients and healthcare systems.
Authors’ contributions
Dr. Torabipour designed the study and was responsible for the writing the original manuscript. Ashrafalsadat Hakim contributed to writing the manuscript. Marzieh Dolatshah and Maryam Yusufzadeh contributed to gathering data. Dr. Ahmadi Angali contributed to writing the statistical analysis.
Conflict of interest
Authors declare no conflict of interest.
Funding
This study was funded by Chronic Disease Care Research Center, Ahvaz Jundishapur University of Medical Sciences Ahvaz, Iran.
REFERENCES
- 1.Ferrari R, Caram LM, Faganello MM, Sanchez FF, Tanni SE, Godoy I. Relation between systemic inflammatory markers, peripheral muscle mass, and strength in limb muscles in stable COPD patients. Int J Chron Obstruct Pulmon Dis 2015;10:1553–8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Burns DK, Wilson EC, Browne P, Olive S, Clark A, Galey P, et al. The Cost Effectiveness of Maintenance Schedules Following Pulmonary Rehabilitation in Patients with Chronic Obstructive Pulmonary Disease: An Economic Evaluation Alongside a Randomised Controlled Trial. Appl Health Econ Health Policy 2016;14(1):105–15. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Blasi F, Cesana G, Conti S, Chiodini V, Aliberti S, Fornari C, et al. The clinical and economic impact of exacerbations of chronic obstructive pulmonary disease: a cohort of hospitalized patients. PLoS One 2014;9(6):e101228. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Tawara Y, Senjyu H, Tanaka K, Tanaka T, Asai M, Kozu R, et al. Value of systematic intervention for chronic obstructive pulmonary disease in a regional Japanese city based on case detection rate and medical cost. Int J Chron Obstruct Pulmon Dis 2015;10:1531–42. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Halbert RJ, Natoli JL, Gano A, Badamgarav E, Buist AS, Mannino DM. Global burden of COPD: systematic review and meta-analysis. Eur Respir J 2006;28(3):523–32. [DOI] [PubMed] [Google Scholar]
- 6.Lee AL, Goldstein RS. Gastroesophageal reflux disease in COPD: links and risks. Int J Chron Obstruct Pulmon Dis 2015;10:1935–49. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Lethbridge-Çejku M, Rose D, Vickerie J. Summary health statistics for u.s. Adults: national health interview survey, 2004. Vital Health Stat 10 2006;(228):1–164. [PubMed] [Google Scholar]
- 8.Mathers CD, Loncar D. Projections of global mortality and burden of disease from 2002 to 2030. PLoS Med 2006;3(11):e442. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Golshan M, Amra B, Welte T. Sample survey of chronic obstructive pulmonary disease and associated risk factors in Isfahan, Iran. Tanaffos 2011;10(3):32–6. [PMC free article] [PubMed] [Google Scholar]
- 10.Mannino DM, Buist AS. Global burden of COPD: risk factors, prevalence, and future trends. Lancet 2007;370(9589):765–73. [DOI] [PubMed] [Google Scholar]
- 11.Kim J, Lee TJ, Kim S, Lee E. The economic burden of chronic obstructive pulmonary disease from 2004 to 2013. J Med Econ 2016;19(2):103–10. [DOI] [PubMed] [Google Scholar]
- 12.Morbidity & Mortality: Chart Book on Cardiovascular, Lung. National Institutes of Health: 2012. [Google Scholar]
- 13.Foster TS, Miller JD, Marton JP, Caloyeras JP, Russell MW, Menzin J. Assessment of the economic burden of COPD in the U.S.: a review and synthesis of the literature. COPD 2006;3(4):211–8. [DOI] [PubMed] [Google Scholar]
- 14.Mousavi SA, Fereshtehnejad SM, Khalili N, Naghavi M, Yahyazadeh H. Determination of the factors affecting duration of hospitalization inpatients with chronic obstructive pulmonary disease (COPD) in Iran. Medical Journal of The Islamic Republic of Iran (MJIRI) 2008;22(1):29–36. [Google Scholar]
- 15.Hilleman DE, Dewan N, Malesker M, Friedman M. Pharmacoeconomic evaluation of COPD. Chest 2000;118(5):1278–85. [DOI] [PubMed] [Google Scholar]
- 16.Sullivan SD, Ramsey SD, Lee TA. The economic burden of COPD. Chest 2000;117(2 Suppl):5S–9S. [DOI] [PubMed] [Google Scholar]
- 17.Scarborough P, Bhatnagar P, Wickramasinghe KK, Allender S, Foster C, Rayner M. The economic burden of ill health due to diet, physical inactivity, smoking, alcohol and obesity in the UK: an update to 2006–07 NHS costs. J Public Health (Oxf) 2011;33(4):527–35. [DOI] [PubMed] [Google Scholar]
- 18.Wang Y, Stavem K, Dahl FA, Humerfelt S, Haugen T. Factors associated with a prolonged length of stay after acute exacerbation of chronic obstructive pulmonary disease (AECOPD). Int J Chron Obstruct Pulmon Dis 2014;9:99–105. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Harries TH, Thornton HV, Crichton S, Schofield P, Gilkes A, White PT. Length of stay of COPD hospital admissions between 2006 and 2010: a retrospective longitudinal study. Int J Chron Obstruct Pulmon Dis 2015;10:603–11. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Geitona M, Hatzikou M, Steiropoulos P, Alexopoulos EC, Bouros D. The cost of COPD exacerbations: a university hospital--based study in Greece. Respir Med 2011;105(3):402–9. [DOI] [PubMed] [Google Scholar]
- 21.Mittmann N, Kuramoto L, Seung SJ, Haddon JM, Bradley-Kennedy C, Fitzgerald JM. The cost of moderate and severe COPD exacerbations to the Canadian healthcare system. Respir Med 2008;102(3):413–21. [DOI] [PubMed] [Google Scholar]
- 22.Halpern MT, Stanford RH, Borker R. The burden of COPD in the U.S.A.: results from the Confronting COPD survey. Respir Med 2003;97 Suppl C:S81–9. [DOI] [PubMed] [Google Scholar]
- 23.Andersson F, Borg S, Jansson SA, Jonsson AC, Ericsson A, Prütz C, Rönmark E, Lundbäck B. The costs of exacerbations in chronic obstructive pulmonary disease (COPD). Respir Med 2002;96(9):700–8. [DOI] [PubMed] [Google Scholar]
- 24.Ford ES, Murphy LB, Khavjou O, Giles WH, Holt JB, Croft JB. Total and state-specific medical and absenteeism costs of COPD among adults aged ≥ 18 years in the United States for 2010 and projections through 2020. Chest 2015;147(1):31–45. [DOI] [PubMed] [Google Scholar]
- 25.Stanford RH, Shen Y, McLaughlin T. Cost of Chronic Obstructive Pulmonary Disease in the Emergency Department and Hospital: An Analysis of Administrative Data from 218 US Hospitals. Treat Respir Med 2006;5(5):343–9. [DOI] [PubMed] [Google Scholar]
- 26.Pfuntner A., Wier LM. (Truven Health Analytics)Steiner C. (AHRQ). Costs for Hospital Stays in the United States, 2010. HCUP Statistical Brief# 146. January 2013. Agency for Healthcare Research and Quality, Rockville, MD: Available at http://www.hcup-us.ahrq.gov/reports/statbriefs/sb146.pdf. [PubMed] [Google Scholar]
- 27.Wouters EF. Economic analysis of the Confronting COPD survey: an overview of results. Respir Med 2003;97 Suppl C:S3–14. [DOI] [PubMed] [Google Scholar]
- 28.Hirose H, Amano A, Yoshida S, Takahashi A, Nagano N, Kohmoto T. Coronary artery bypass grafting in the elderly. Chest 2000;117(5):1262–70. [DOI] [PubMed] [Google Scholar]
- 29.Yoon P, Steiner I, Reinhardt G. Analysis of factors influencing length of stay in the emergency department. CJEM 2003;5(3):155–61. [DOI] [PubMed] [Google Scholar]