Abstract
Case series
Patients: Female, 19 • Female, 18
Final Diagnosis: Solid pseudopapillary tumor of pancreas
Symptoms: Abdominal discomfort
Medication: —
Clinical Procedure: Surgery
Specialty: Oncology
Objective:
Unusual setting of medical care
Background:
Solid pseudopapillary tumor of the pancreas (Frantz tumor) is a rare, low-grade malignant neoplasm. Laparoscopic pancreatoduodenectomy is a good approach for tumors located in the pancreatic head. We present two successful cases in young women.
Case Report:
A 19-year-old woman was admitted to Department of Digestive Surgery due to epigastric pain, nausea, and vomiting. Computed tomography scan of the abdomen was performed, and a 3.0×2.2 cm solid tumor localized in the head of the pancreas was observed. After the diagnosis of Frantz tumor of the pancreas, the patient underwent laparoscopic pancreatoduodenectomy. Histopathology confirmed solid and cystic pseudopapillary tumor. The postoperative course was uneventful, and after 8 months the patient remained disease-free. An 18-year-old woman was admitted at the emergency room with abdominal pain, vomiting, and diarrhea. Computed tomography scans revealed a mass of 4.1×3.3 cm in size in the head of the pancreas consistent with a solid pseudopapillary tumor. Laparoscopic pancreatoduodenectomy was performed by two expert surgeons who divided the work: one did resection and the other did reconstruction. The patient was discharged at postoperative day 6 without complications, and during five months of follow-up the patient has been well and without disease.
Conclusions:
Laparoscopic pancreatoduodenectomy can be performed safely in patients with Frantz tumor by surgeons with expertise in laparoscopic surgery, technical skill, and adequate equipment.
MeSH Keywords: Laparoscopy; Pancreatic Neoplasms; Pancreaticoduodenectomy; Surgical Procedures, Minimally Invasive
Background
Solid pseudopapillary tumor of the pancreas, known as Frantz tumor, is a rare clinical pathologic condition and occurs predominantly in women. Degenerative cystic changes are commonly observed and capsule is common. First described by Virginia K. Frantz, it is a tumor defined as a low-grade malignant neoplasm of the exocrine pancreas. The majority of patients are young females, and the tumor is located in the body and tail (67%) and head (32%) of the pancreas. Most of the tumors are asymptomatic until they become large. The diagnosis can be made by computed tomography and magnetic resonance imaging. Surgical resection is the treatment for all cystic tumors of the pancreas, and the approach is most dependent on location of the tumor. For tumors located in the pancreatic head, the surgery is pancreatoduodenectomy [1–3].
Laparoscopic pancreatoduodenectomy is classified as a complicated surgical procedure and is only performed in some specialized centers. However, it has been demonstrated to be a safe and feasible surgery. Some factors are responsible for a safe pancreatoduodenectomy [4,5]. These factors are the careful selection of the patient, skill in laparoscopic surgical technique, laparoscopic equipment and instruments, and experience with open pancreatoduodenectomy [4,6]. The aim of this study is to present two selected cases of laparoscopic pancreatoduodenectomy in patients with Frantz tumor of the pancreas.
Case Report
Case 1
A 19-year-old woman, body mass index (BMI) 20 kg/m2, was admitted to Department of Digestive Surgery due to back pain, epigastric pain, nausea, vomiting, and weight loss (8 kg in 9 months). An abdominal computed tomography scan showed a 3×2.2 cm solid tumor localized into the head of the pancreas, near the inferior vena cava. A magnetic resonance image confirmed a solid and cystic tumor in the uncinate process and the diagnosis of solid pseudopapillary tumor of the pancreas (Figure 1). On examination, the patient had no jaundice, and no abdominal mass was palpable. Tumor markers like CA19-9, carcinoembryonic antigen (CEA), Beta-HCG, and alpha-fetoprotein (AFP) were normal. Laboratory tests were normal except for hemoglobin 11 g/dL. Cardiovascular evaluation was normal, and the patient underwent laparoscopic pancreatoduodenectomy.
Figure 1.

Solid pseudopapillary tumor in the head of the pancreas.
The patient was placed in a supine position with a reverse Trendelenburg and the surgeon positioned between the legs of the patient. Six trocars were placed under direct vision and pneumoperitoneum was maintained with CO2 at 13 mm Hg. The pancreatoduodenectomy was performed with division of the pancreas at the neck, bile duct divided above the cystic duct, and stomach resected near the pylorus using a linear stapler, without pylorus preservation (Figure 2). The reconstruction was carried out with two-layer invagination pancreatojejunostomy with a tube inside the pancreatic duct, running suture hepatico-jejunostomy, and stapled gastrojejunostomy. Two silicone drains were placed, and the specimen was removed through a small incision in the pelvis. The operative time was 6 hours and no blood transfusion was given.
Figure 2.

Specimen with tumor in the head of the pancreas.
Histopathology confirmed a 3.5×2.5 cm pancreatic solid and cystic pseudopapillary tumor, hemorrhagic areas, and clear resection margins (Figure 3).
Figure 3.
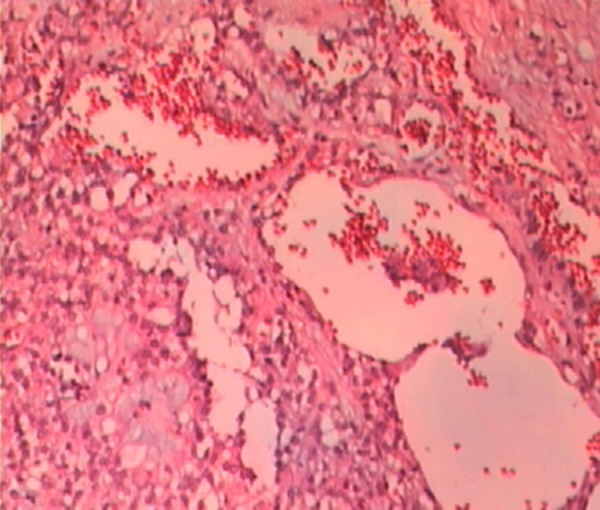
Histopathology with pseudopapillary pattern, cystic degeneration, and hemorrhage (HE 100×).
The postoperative course was uneventful and the patient was discharged 8 days after the first procedure. After 8 months of follow-up, the patient remained well and disease-free.
Case 2
An 18-year-old woman, BMI 19 kg/m2, was admitted at the emergency room with complaints of abdominal pain, nausea, vomiting, and diarrhea. Her past medical history was unremarkable. On physical examination some discomfort and upper abdominal pain were observed. The rest of the examination was normal. Laboratory evaluation was normal. Upper abdominal ultrasonography and computed tomography scans revealed a solid mass of 4.1×3.3 cm in size in the head and uncinate process of the pancreas, and the diagnosis of solid pseudopapillary tumor of the pancreas was made (Figure 4). There was no biliary or pancreatic duct dilation. The tumor markers (α-fetoprotein, CA19-9, carcinoembryonic antigen, and human chorionic gonadotropin) were normal. The preoperative evaluation was normal, and the patient underwent laparoscopic pancreatoduodenectomy.
Figure 4.
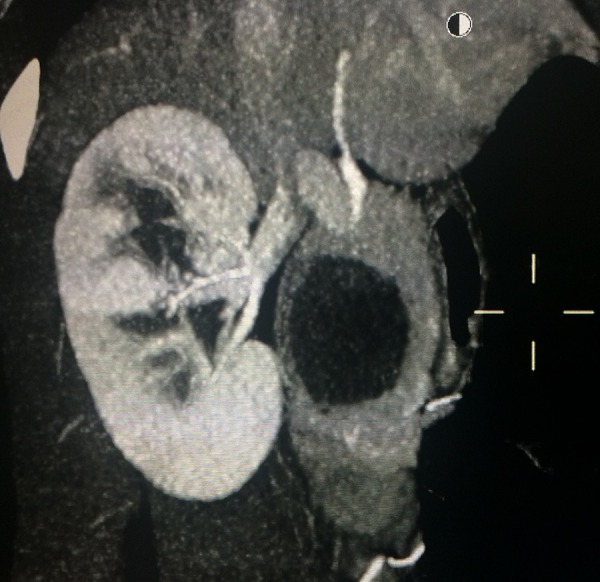
Cystic and solid pseudopapillary tumor in the head of the pancreas.
Laparoscopic pancreatoduodenectomy was performed by two expert surgeons who divided the work: one did resection and the other did reconstruction. After the patient was placed in a supine position with reverse Trendelenburg, six trocars were placed under direct vision. The gastrocolic omentum was dissected to access the lesser sac. The superior mesenteric vein and portal vein were dissected to isolate the pancreas, which was divided (Figure 5). The Kocher maneuver was carried out and the duodenum was transected using a linear stapler without pylorus preservation. The biliary tract was dissected and transected above the cystic duct. Complete lymphadenectomy was carried out.
Figure 5.
Dissection of superior mesenteric vein and portal vein.
The reconstruction was carried out in a classic single loop with the pancreas (invagination), with a tube inside the pancreatic duct to facilitate the anastomosis, followed by the bile duct (duct-to-mucosa) and stomach using a linear stapler. Two silicone drains were placed, and a small incision in the pelvic region was made to remove the specimen (Figure 6). The operative time was 10 hours and no blood transfusion was given.
Figure 6.

Specimen with tumor in the head of the pancreas.
The pathological examination of the specimen revealed a pancreatic solid and cystic pseudopapillary tumor of 3.9×3.2 cm in size, with negative margins (Figure 7) and no evidence of metastases in the lymph nodes.
Figure 7.
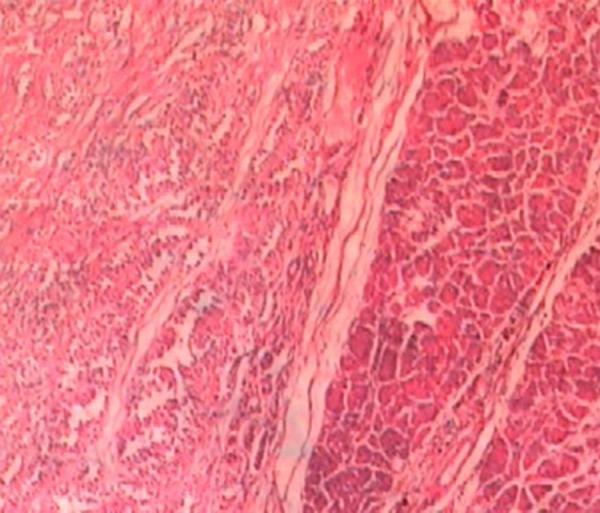
Histopathology-confirmed surgical margin, well delimited (HE 100×).
The patient was discharged at postoperative day 6 without complications, and during five months of follow-up she has been well, without disease, and the final appearance of the abdomen was good (Figure 8).
Figure 8.

Final aspect of the abdomen five months after the procedure.
Discussion
Solid pseudopapillary tumor of pancreas is a rare condition and represents 0.2–2.7% of malignant tumors of the pancreas. Histologically the tumor contains proportions of pseudo-papillary, solid, and cystic components. The tumor is encapsulated and well circumscribed with degenerative cystic cavities and hemorrhages [1–3].
Gagner and Pomp performed the first laparoscopic pancreatoduodenectomy in 1994 [4]. After more than 20 years this procedure is only performed in some specialized centers [5,6]. Acceptance is still slow due to inherent technical limitations and the need for skills in advanced laparoscopic surgery, which is not always possible for hepato-pancreatobiliary surgeons. However, this procedure is safe and feasible. The selection of the patients, experience in open pancreatoduodenectomy, and skill in laparoscopic surgery are important factors for the success of this procedure [7,8]. In the present study, we reviewed two successful laparoscopic pancreatoduodenectomies due to solid pseudopapillary tumor of the pancreas in young women.
The selection of the patients is extremely important. The ideal candidates for laparoscopic pancreatoduodenectomy include patients with low-grade tumors, without vascular invasion, without obesity, without previous surgery, and not affected by comorbidities [5–7]. In these cases the patients were young, had excellent general health, had no history of previous surgery, had no invasion of mesenteric vein, portal vein, or surrounding tissues, and had no lymph nodes metastases. Surgeons who want to perform the procedure should have the motivation and capacity to pursue innovation and accept challenge. Moreover, laparoscopic instruments and equipment like the ultrasonic knife, bipolar cautery, and stapler are necessary to perform the procedure properly. Each of these instruments has a different utility [6,9,10].
Surgical expertise in conventional pancreatoduodenectomy and knowledge about vascular anatomy, both normal and variations, are necessary. The laparoscopic technique includes dissection and reconstruction. During the resection, the possibility of bleeding during the dissection with an ultrasonic device is low. Correct evaluation of the vascular anatomy before the operation is important to reduce major injuries and the need for blood transfusion and conversion. For reconstruction, the surgeon needs the ability to perform laparoscopic suturing and surgical knots [6–8]. Pancreatojejunostomy can be performed with duct-mucosa technique or invagination. Duct-mucosa anastomosis is suitable in patients with a pancreatic duct of 3 mm or more in diameter. The laparoscopic visualization of the pancreatic duct is better than in open surgery [7,8]. In these cases we performed invagination of the pancreas with a tube inside the pancreatic duct, and we did not observe a pancreatic leak. Bile duct anastomosis is possible even in a small duct. In this situation running suturing is not indicated due to the risk of biliary stenosis. Finally, for gastrojejunostomy, the linear stapler makes the procedure feasible, fast, and safe. The risk of fistula after stapled gastroenteric anastomosis is low. To minimize complications, the procedure should be performed by two expert surgeons who divide the work: one doing resection and the other doing reconstruction. [7–10].
An important difficulty related to laparoscopic pancreatoduodenectomy is vascular dissection. In case of vascular invasion, the procedure is more complex laparoscopically [11]. In the present study there was no vascular involvement, the tumor had a low grade of malignancy, the lymph nodes were clear, and resection was possible in both cases.
Laparoscopic pancreatoduodenectomy is associated with rapid recovery and shorter hospitalization. Moreover, the mortality rate is similar to that of open pancreatoduodenectomy [5–7,9]. Another advantage of laparoscopic pancreatoduodenectomy that should be taken into consideration in these cases is the cosmetic results. The present cases, two young women with low-grade malignant tumors of the pancreas and no previous operations, certainly had good outcomes.
Conclusions
Laparoscopic pancreatoduodenectomy is an effective and safe procedure, can achieve perioperative outcomes similar to those of open surgery, and can be performed safely in selected patients as in these cases, particularly by surgeons experienced in advanced laparoscopy. This procedure does require laparoscopic technical skill and adequate equipment.
Footnotes
Conflict of interest statement
The authors declare that they have no conflict of interest.
Ethical standards
Ethical approval was not required, and patient identifying knowledge was not presented in this report.
References:
- 1.Frantz VK. Atlas of tumor pathology, 7th section, 27–28th fascicles. Washington, DC: US Armed Forces Institute of Pathology; 1959. Tumors of the pancreas; pp. 32–33. [Google Scholar]
- 2.Parelkar SV, Oak SN, Kapadnis SP, et al. Solid pseudo papillary tumor of the pancreas: an unusual tumor in children. J Indian Assoc Pediatr Surg. 2013;18:38–40. doi: 10.4103/0971-9261.107019. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Bacelar-Junior EA, Gomes MAP, et al. Frantz’s tumor of the pancreas. Arq Bras Cir Dig. 2010;23:212–13. [Google Scholar]
- 4.Gagner M, Pomp A. Laparoscopic pylorus-preserving pancreatoduodenectomy. Surg Endosc. 1994;8:408–10. doi: 10.1007/BF00642443. [DOI] [PubMed] [Google Scholar]
- 5.Asbun HJ, Stauffer JA. Laparoscopic vs. open pancreaticoduodenectomy: Overall outcomes and severity of complications using the Accordion Severity Grading System. J Am Coll Surg. 2012;215:810–19. doi: 10.1016/j.jamcollsurg.2012.08.006. [DOI] [PubMed] [Google Scholar]
- 6.Kendrick ML, Cusati D. Total laparoscopic pancreaticoduodenectomy: Feasibility and outcome in an early experience. Arch Surg. 2010;145:19–23. doi: 10.1001/archsurg.2009.243. [DOI] [PubMed] [Google Scholar]
- 7.Palanivelu C, Rajan PS, Rangarajan M, et al. Evolution in techniques of laparoscopic pancreaticoduodenectomy: A decade long experience from a tertiary center. J Hepatobiliary Pancreat Surg. 2009;16:731–40. doi: 10.1007/s00534-009-0157-8. [DOI] [PubMed] [Google Scholar]
- 8.Shrikhande SV, Sivasanker M. Laparoscopic pancreatoduodenectomy: How far have we come and where are we headed? World J Gastrointest Surg. 2015;7:128–32. doi: 10.4240/wjgs.v7.i8.128. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Boggi U, Amorese G, Vistoli F, et al. Laparoscopic pancreaticoduodenectomy: A systematic literature review. Surg Endosc. 2015;29:9–23. doi: 10.1007/s00464-014-3670-z. [DOI] [PubMed] [Google Scholar]
- 10.Palanivelu C, Jani K, Senthilnathan P, et al. Laparoscopic pancreaticoduodenectomy: technique and outcomes. J Am Coll Surg. 2007;205:222–30. doi: 10.1016/j.jamcollsurg.2007.04.004. [DOI] [PubMed] [Google Scholar]
- 11.Croome KP, Farnell MB, Que FG, et al. Pancreaticoduodenectomy with major vascular resection: A comparison of laparoscopic versus open approaches. J Gastrointest Surg. 2015;19:189–94. doi: 10.1007/s11605-014-2644-8. [DOI] [PubMed] [Google Scholar]



