Abstract
Objective
To examine how history of criminal justice involvement (CJI) is related to HIV care continuum metrics among young Black men who have sex with men (YBMSM) 16–29 years of age.
Design
Population-based survey
Methods
From 2013–2014 a representative sample of YBMSM was generated using Respondent Driven Sampling (RDS) in Chicago (n=618). HIV antibody/Ag and RNA testing were performed using dry blood spots. Factors assessed in the care continuum included HIV testing, HIV diagnosis, linkage-to-care within 6 months, retention-in-care, adherence to antiretrovirals, and viral suppression. RDS-weighted regression models examined the associations between history of CJI, including frequency of CJI and durations of stay and each of the continuum metrics.
Results
A final analytic sample of 618 participants was generated through RDS chains of up to 13 waves in length and with a mean of 2.1 recruits per participant. At enrollment, 40.8% had prior history of CJI and 34.6% were HIV seropositive. Of persons reporting HIV seropositive status, 58.4% were linked to care, 40.2% retained in care, 32.2% adherent to antiretrovirals and 24.3% virally suppressed. Any CJI history was associated with the overall care continuum (aOR, 2.35; 95% CI 1.13–4.88) and was most associated with increased retention-in-care (aOR 3.72 (1.77–7.84)). Having one CJI experience and detention for only one day was associated with better retention-in-care compared to no or more frequent CJI.
Conclusions
Those with a previous history of CJI were more successful in achieving most HIV care continuum metrics. Frequent and cycling CJI, however, was detrimental to HIV care.
Introduction
HIV care continuum research that includes Black MSM has primarily utilized a disparities framework which compares Black MSM to a White MSM reference group [1, 2]. While this approach may suggest broad differences between these two populations, such analyses are unable to account for the marked heterogeneity within Black MSM communities [3–5]. In addition, existing studies have not adequately explored the role of criminal justice involvement (CJI), which is higher among Black versus White MSM. Such CJI might be related to the HIV care continuum [6]. Therefore, next generation analyses that move beyond a disparities framework can begin to illuminate factors and processes that are most amenable to intervention among Black MSM. Such an approach recognizes BMSM as a diverse group, and in particular younger Black MSM where prevention interventions are largely absent [7]. More specifically, in the context of CJI, studies [8, 9] have demonstrated high rates of HIV transmission among criminal justice involved Black MSM. However, there is little understanding of how CJI might be related to the HIV care continuum among YBMSM. Whether CJI might benefit or detract from HIV care engagement is an important question that can have significant primary and secondary HIV intervention implications within this population, who are disproportionately burdened by staggering rates of CJI and HIV incidence [8, 10].
In order to examine the relationship between CJI and the HIV care continuum we use recent data from the uConnect cohort, a population-based sample of younger Black MSM 16–29 years of age. Because drivers of the HIV care continuum are poorly characterized among YBMSM, [11, 12] a population-based sample helps avoid some of the biases associated with samples of YBMSM based in clinics or jails, or other convenience samples, that would impact our understanding of factors most associated with the entire breadth of the HIV care continuum.
Methods
Sample Generation
Respondent Driven Sampling (RDS) was used to generate the uConnect cohort and estimation of population parameters from the data. Additional information regarding justification for RDS, population parameter estimates, weights computation of finite population correction, sensitivity analyses, implementation of RDS sampling and sourcing of seeds has been previously described [13, 14] and is available in Supplementary Materials 1.0 – 3.0.
Data Collection: Eligibility Criteria
Using an RDS approach, a baseline sample of eligible YBMSM was recruited in South Chicago and adjacent South suburbs between June 2013 and July 2014 [13]. This geographic area was sampled because it represents the largest region of highest HIV incidence in Chicago [15] and, as the most populous contiguous majority Black community area in the United States [16], provides the opportunity to generate a large sample with limited variation in environmental exposures [17]. Study respondents were eligible to be interviewed if they: 1) self-identified as African American or Black, 2) were born male, 3) were between 16 and 29 years of age (inclusive), 4) reported oral or anal sex with a male within the past 24 months, 5) resided in South Chicago or the adjacent South suburbs, and 6) were willing and able to provide informed consent at the time of the study visit.
HIV Care Continuum Measures
HIV care continuum measures included HIV infected unaware, linkage to care, retention in care, adherence to antiretrovirals and viral suppression. HIV infection was determined by three assays applied to samples eluted from dry blood spot samples: ARCHITECT HIV Ag/Ab Combo, Multispot HIV-1/HIV-2 Bio-Rad, and Realtime HIV-1 RNA (Abbot). HIV-infected but unaware individuals were identified as clients who reported HIV negative status (or never tested), and who were found to be HIV seropositive. All clients found to be HIV-infected-but-unaware were reviewed and confirmed by a trained social worker following the study visit and corroboration with Department of Public Health surveillance records. Linkage to care, retention in care and adherence to antiretrovirals were based upon self-report. Multiple definitions of linkage to care exist [18–26]. In the uConnect cohort, linkage was defined as reporting at least one HIV medical care visit within 6 months after diagnosis. Retention in care was defined as reporting two or more appointments 90 days apart in the previous 12 months [27]. Viral load frequency measures of retention collected from Chicago Department of Public Health laboratory surveillance data was used to verify self-report, and was correlated (data not shown). Adherence to antiretrovirals was defined as self-report of missing HIV medications on fewer than 4 days in the previous month to be consistent with >85% adherence. Viral suppression was defined as having an HIV RNA <2000 nucleic acid (NA) copies/mL in whole blood (RealTime, Abbott).
Independent Variable Measures
The variables selected for this study were informed by prior empirical considerations suggesting that racial disparities associated with HIV care continuum metrics were associated with sociodemographic, risk behavior, health, and social factors [28–32]. Additional information on these variables and CJI definitions can be found in Supplementary materials 1.0–4.0.
Statistical Analysis
First, we assessed the bivariate relationships between each of the independent variables with our primary HIV care continuum outcomes using simple logistic regressions, giving us unadjusted bivariate odds ratios for each of the independent/outcome variable pairings. Next, we accounted for sociodemographic characteristics and preexisting situations that may affect one’s place on the continuum in each of the logistic regressions to produce adjusted bivariate odds ratios. Our final comprehensive models included each HIV care continuum variable against the entire set of independent variables and controls. Significant associations between independent variables and HIV care continuum variables were assessed via the odds ratios in those final six multivariate logistic regression models (α=0.05). Joint p-values for the effect of each independent variable across the span of the HIV care continuum were calculated using techniques to adjust for overall effects in seemingly unrelated regressions [33].
Finally, to more clearly understand the association between the HIV care continuum and CJI, we substituted in total time served, average time served per detainment (days) and total number of separate detainments for the original dichotomous CJI variable in the final multivariate logistic regression models. All regression analyses were conducted using Stata 14 software [34].
Results
A final analytic sample of 622 eligible participants was generated through RDS chains of up to 13 waves in length and with a mean of 2.1 recruits per participant. At enrollment, 71.1% of the sample was 24 years of age and under, 40.8% had prior history of CJI, 54.4% had health care coverage and 34.6% were HIV seropositive. Of those HIV seropositive, 58.4% had been linked to care within 6 months of diagnosis, 40.2% were retained in care, 32.2% were adherent to antiretrovirals and 24.3% were virally suppressed. uConnect cohort descriptives can be found in Supplementary Materials.
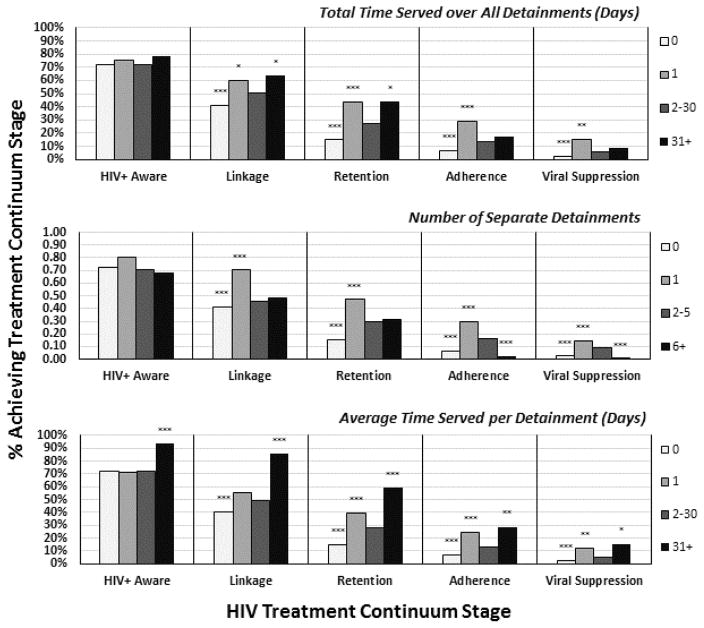
In adjusted analyses, CJI was associated with the overall HIV care continuum (aOR 2.35; 95% CI 1.13–4.88) including viral suppression (aOR 3.00; 95% CI 1.15–7.79). In addition several covariates were associated with each step in the HIV care continuum as demonstrated in Table 1. Length and frequency of CJI was also associated with care continuum metrics albeit in a more nuanced way (Figure 1).
Table 1.
Multivariable logistic regression models of potential HIV Care Continuum drivers among a population-based sample of younger black MSM, uConnect 2013–2014
| HIV Care Continuum Drivers Odds Ratio (95% CI) |
Serostatus N=618 |
HIV+ Aware N=214 |
Linked to Care N=214 |
Retained in Care N=214 |
Adherence to ARVs N=214 |
Viral Suppress N=214 |
|---|---|---|---|---|---|---|
| Social Factors | ||||||
| Criminal justice involvement | 2.24 (1.28–3.94)** | 1.57 (0.63–3.87) | 3.20 (1.10–9.36)* | 3.72 (1.77–7.84)** | 2.52 (1.30–4.89)** | 3.00 (1.15–7.79 |
| Have a mother/mother figure | 0.58 (0.24–1.36) | 4.33 (1.24–15.13)* | 1.16 (0.50–2.72) | 1.28 (0.42–3.88) | 0.98 (0.34–2.87) | 2.31 (0.71–7.4 |
| Open about sexual identity | 0.79 (0.41–1.55) | 3.52 (1.07–11.57)* | 1.85 (0.55–6.28) | 1.90 (0.51–7.16) | 1.18 (0.32–4.31) | 1.36 (0.31–5.9 |
| House/Ball or gay family member | 1.51 (0.94–2.45)† | 1.22 (0.53–2.81) | 0.79 (0.43–1.44) | 1.35 (0.51–3.55) | 1.34 (0.49–3.66) | 0.83 (0.25–2.8 |
| Closeness to Black community | 0.82 (0.46–1.46) | 0.75 (0.18–3.03) | 2.58 (0.59–11.33) | 0.63 (0.19–2.09) | 0.53 (0.14–1.95) | 0.52 (0.15–1.7 |
| Ever witness to violent assault(s) | 0.68 (0.36–1.30) | 0.52 (0.18–1.52) | 1.09 (0.44–2.69) | 0.95 (0.44–2.10) | 0.54 (0.28–1.05)† | 1.50 (0.76–2.9 |
|
| ||||||
| Sociodemographics | ||||||
| Age (Years) | ||||||
| 16–18 | 0.12 (0.02–0.57)** | 7.08 (1.84–27.24)** | 0.33 (0.08–1.48) | 0.40 (0.07–2.23) | 0.14 (0.01–1.67) | 0.16 (0.01–2.1 |
| 19–20 | 0.19 (0.09–0.42)*** | 2.18 (0.43–11.00) | 6.33 (1.23–32.61)* | 0.93 (0.30–2.90) | 0.98 (0.30–3.23) | 0.34 (0.11–1.05 |
| 21–24 | 0.43 (0.25–0.75)** | 1.29 (0.50–3.34) | 1.13 (0.40–3.16) | 0.82 (0.43–1.55) | 0.53 (0.20–1.42) | 0.42 (0.14–1.2 |
| 25+ | 1.00 | 1.00 | 1.00 | 1.00 | 1.00 | 1.00 |
| Education | ||||||
| Less than high school | 0.94 (0.51–1.75) | 1.47 (0.39–5.61) | 1.32 (0.55–3.15) | 1.72 (0.50–5.91) | 1.94 (0.49–7.61) | 4.45 (1.03–19.2 |
| High school or equivalent | 1.00 | 1.00 | 1.00 | 1.00 | 1.00 | 1.00 |
| Some college or higher | 1.07 (0.68–1.68) | 2.17 (0.86–5.44)† | 1.17 (0.53–2.55) | 0.89 (0.41–1.93) | 0.73 (0.32–1.63) | 0.71 (0.26–1.9 |
| Identifies as gay | 3.10 (1.34–7.19)** | 1.89 (0.48–7.41) | 1.99 (0.74–5.36) | 0.98 (0.47–2.03) | 0.82 (0.37–1.84) | 0.64 (0.23–1.8 |
| Current employment | ||||||
| Unemployed | 1.00 | 1.00 | 1.00 | 1.00 | 1.00 | 1.00 |
| Full time | 0.63 (0.36–1.10) | 2.01 (0.64–6.29) | 0.80 (0.33–1.93) | 1.12 (0.32–3.86) | 0.62 (0.17–2.25) | 0.53 (0.17–1.6 |
| Part time | 0.85 (0.43–1.68) | 1.02 (0.42–2.51) | 0.60 (0.26–1.36) | 1.32 (0.62–2.82) | 1.59 (0.72–3.49) | 1.63 (0.66–4.0 |
| Housing instability in past year | 1.08 (0.64–1.80) | 1.27 (0.45–3.59) | 0.33 (0.12–0.89)* | 0.70 (0.28–1.77) | 0.95 (0.33–2.70) | 1.09 (0.42–2.7 |
| Behavior & Health | ||||||
| Drug use in past year | 1.64 (1.03–2.60)* | 2.12 (0.80–5.64) | 1.21 (0.49–3.02) | 1.72 (0.80–3.68) | 0.98 (0.37–2.59) | 1.09 (0.37–3.2 |
| Health care coverage | 1.46 (0.96–2.21)† | 9.86 (4.19–23.22)*** | 10.00 (3.97–25.19)*** | 5.24 (2.27–12.05)*** | 6.60 (3.02–14.39)*** | 6.14 (2.59–14.55 |
| Psychological distress | 0.93 (0.53–1.63) | 4.10 (0.55–30.49) | 2.92 (1.02–8.35)* | 0.91 (0.26–3.19) | 0.66 (0.14–3.18) | 0.46 (0.07–2.9 |
| Years since HIV diagnosis | Excludedb | Excludedb | 1.14 (0.98–1.32)† | 1.09 (0.99–1.20)† | 1.07 (0.97–1.18) | 1.06 (0.96–1.1 |
p<0.10;
p<0.05;
p<0.01;
p<0.001
ARVs, antiretrovirals; CI, confidence interval; MSM, men who have sex with men; TasP, treatment as prevention.
Ordinal variable giving the highest stage each respondent reached in the HIV Care Continuum.
Excluded from model due to dependence on the outcome variable
Figure 1.
Adjusted estimates of HIV Treatment Continuum success by length and frequency of criminal justice detention, uConnect 2013–2014 (n=214)
*p<0.05; **p<0.01; ***p<0.001
Discussion
There are several new and important findings from these analyses. First, we documented that CJI YBMSM versus those with no such histories are more likely to be successfully engaged in the HIV care continuum. These findings were robust across a variety of HIV care continuum stag. A critical caveat to these findings is that there are competing forces between total days spent per detention and frequency of detention episodes. Repeated episodes of CJI resulted in worse HIV care engagement across a number of measures, yet longer stays were associated with better HIV care engagement across all HIV care continuum measures. Frequent and recurrent cycling within the criminal justice system has also been reported by others as a risk factor for ongoing HIV risk and transmission [35, 36]. It is unclear from our analysis whether frequent cycling of YBMSM in and out of CJI is a symptom of other social factors that limit HIV care engagement, or whether repeated CJI is disruptive to maintaining engagement with HIV care.
Our finding of the association between longer CJI stays and improved HIV care engagement substantiates those of prior studies which have documented that CJI is associated with improved HIV care continuum metrics. A recent systematic review suggests that HIV care continuum measures such as achievement of viral suppression were highest during the incarcerated period [37]. The review also highlights that following incarceration, criminal justice involved populations are less likely to engage in the HIV Care Continuum and at slightly lower rates to those engaged prior to incarceration. Our findings extend those of earlier studies by characterizing the nuance of HIV care engagement based upon the frequency of exposure and duration of CJI. Some of the differences in our study may be due to several factors including that the majority of studies in the systematic review were focused on prison populations that included both men and women sexual identity was rarely reported, and race/ethnicity was not assessed. Clearly, the association between duration of CJI and HIV care engagement is of concern and may reflect the poor HIV care engagement infrastructure outside of jails in communities of color.
The current study also finds that having a “mother figure” is an important factor related to improved care continuum metrics. It may be that having important kin relationships is associated with better care outcomes, although having a mother figure did not modify the findings when added to the model. Previous work has shown that family in the lives of YBMSM matters with respect to HIV testing and other HIV related risk behaviors [38, 39]. Relatedly, network interventions have been found to be effective including group-level interventions [40], which may hold promise for improving the HIV care continuum [41].
In summary, this analysis of the YBMSM care continuum highlights the nuanced nature of CJI’s possible impacts on the HIV care continuum. Understanding these nuances was possible because we moved away from an examination of disparities that compares White to Black MSM, and instead focused on the heterogeneity within YBMSM communities. While CJI systems may be good for HIV care retention, its overall social role is likely very negative, especially considering outcomes that go beyond public health (police brutality, disruption of community lives, lack of opportunity upon release, etc). In addition, while limiting criminalization of YBMSM may reduce risk of HIV, the criminal justice system is structured to implement many steps of the HIV continuum, including testing and treatment which may engage some in care even post-release. However, frequent and cycling CJI was associated with less care engagement and may reflect disruptions in HIV care engagement or represents other structural factors that would limit care engagement. Consequently, forming more coordinated joint partnerships with criminal justice systems, departments of public health and other community based initiatives are needed to improve the HIV continuum for YBMSM.
Supplementary Material
Acknowledgments
We would like to thank the uConnect study participants and Ishida Robinson, Eve Zurawski, Billy Davis, Rebecca Duvoisin and the NORC field team for generating the data for analysis. We would like to thank Michelle Taylor and Iman Little for providing linkage services for all participants. We would also like to thank the National Institutes of Health (R01 DA039934, R01 DA033875) for funding the study and analysis.
Footnotes
Competing interests: We have no competing interests to declare.
Presented in part: Conference on Retroviruses and Opportunistic Infections (CROI) February 2015.
References
- 1.Rosenberg ES, Millett GA, Sullivan PS, Del Rio C, Curran JW. Understanding the HIV disparities between black and white men who have sex with men in the USA using the HIV care continuum: a modeling study. Lancet HIV. 2014;1:e112–e118. doi: 10.1016/S2352-3018(14)00011-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Millett GA, Peterson JL, Flores SA, Hart TA, Jeffries WLt, Wilson PA, et al. Comparisons of disparities and risks of HIV infection in black and other men who have sex with men in Canada, UK, and USA: a meta-analysis. Lancet. 2012;380:341–348. doi: 10.1016/S0140-6736(12)60899-X. [DOI] [PubMed] [Google Scholar]
- 3.Mays VM, Cochran SD, Zamudio A. HIV Prevention Research: Are We Meeting the Needs of African American Men Who Have Sex With Men? J Black Psychol. 2004;30:78–105. doi: 10.1177/0095798403260265. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Peterson JL, Jones KT. HIV prevention for black men who have sex with men in the United States. Am J Public Health. 2009;99:976–980. doi: 10.2105/AJPH.2008.143214. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Malebranche DJ, Arriola KJ, Jenkins TR, Dauria E, Patel SN. Exploring the “bisexual bridge”: a qualitative study of risk behavior and disclosure of same-sex behavior among black bisexual men. Am J Public Health. 2010;100:159–164. doi: 10.2105/AJPH.2008.158725. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Iroh PA, Mayo H, Nijhawan AE. The HIV Care Cascade Before, During, and After Incarceration: A Systematic Review and Data Synthesis. Am J Public Health. 2015;105:e5–16. doi: 10.2105/AJPH.2015.302635. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Hemmige V, McFadden R, Cook S, Tang H, Schneider JA. HIV prevention interventions to reduce racial disparities in the United States: a systematic review. J Gen Intern Med. 2012;27:1047–1067. doi: 10.1007/s11606-012-2036-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Brewer RA, Magnus M, Kuo I, Wang L, Liu TY, Mayer KH. The High Prevalence of Incarceration History Among Black Men Who Have Sex With Men in the United States: Associations and Implications. American Journal of Public Health. 2014;104:448–454. doi: 10.2105/AJPH.2013.301786. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Brewer RA, Magnus M, Kuo I, Wang L, Liu TY, Mayer KH. Exploring the Relationship Between Incarceration and HIV Among Black Men Who Have Sex With Men in the United States. Jaids-Journal of Acquired Immune Deficiency Syndromes. 2014;65:218–225. doi: 10.1097/01.qai.0000434953.65620.3d. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Brewer RA, Magnus M, Kuo I, Wang L, Liu TY, Mayer KH. Exploring the relationship between incarceration and HIV among black men who have sex with men in the United States. J Acquir Immune Defic Syndr. 2014;65:218–225. doi: 10.1097/01.qai.0000434953.65620.3d. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Singh S, Bradley H, Hu X, Skarbinski J, Hall HI, Lansky A, et al. Men living with diagnosed HIV who have sex with men: progress along the continuum of HIV care--United States, 2010. MMWR Morb Mortal Wkly Rep. 2014;63:829–833. [PMC free article] [PubMed] [Google Scholar]
- 12.Whiteside YO, Cohen SM, Bradley H, Skarbinski J, Hall HI, Lansky A, et al. Progress along the continuum of HIV care among blacks with diagnosed HIV- United States, 2010. MMWR Morb Mortal Wkly Rep. 2014;63:85–89. [PMC free article] [PubMed] [Google Scholar]
- 13.Khanna AS, Michaels S, Skaathun B, Morgan E, Green K, Young L, et al. Preexposure Prophylaxis Awareness and Use in a Population-Based Sample of Young Black Men Who Have Sex With Men. JAMA Intern Med. 2015:1–3. doi: 10.1001/jamainternmed.2015.6536. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Placeholder for Ann Epidemiol paper. Ann Epidemiol [Google Scholar]
- 15.Chicago Department of Public Health. HIV/STI Surveillance Report, 2015. Chicago, IL: City of Chicago; 2015. [Google Scholar]
- 16.U.S. Census Bureau. State and County Quick Facts. Data derived from population estimates, American community survey, census of population and housing, county business patterns, economic census, survey of business owners, building permits, consolidated federal funds report, census of governments [Google Scholar]
- 17.Heckathorn DD. Respondent-driven sampling: a new approach to the study of hidden populations. SOCIAL PROBLEMS-NEW YORK. 1997 [Google Scholar]
- 18.Hightow-Weidman LB, Jones K, Wohl AR, Futterman D, Outlaw A, Phillips G, 2nd, et al. Early linkage and retention in care: findings from the outreach, linkage, and retention in care initiative among young men of color who have sex with men. AIDS Patient Care STDS. 2011;25(Suppl 1):S31–38. doi: 10.1089/apc.2011.9878. [DOI] [PubMed] [Google Scholar]
- 19.Reed JB, Hanson D, McNaghten AD, Bertolli J, Teshale E, Gardner L, et al. HIV testing factors associated with delayed entry into HIV medical care among HIV-infected persons from eighteen states, United States, 2000–2004. AIDS Patient Care STDS. 2009;23:765–773. doi: 10.1089/apc.2008.0213. [DOI] [PubMed] [Google Scholar]
- 20.Craw J, Gardner L, Rossman A, Gruber D, Noreen O, Jordan D, et al. Structural factors and best practices in implementing a linkage to HIV care program using the ARTAS model. BMC Health Serv Res. 2010;10:246. doi: 10.1186/1472-6963-10-246. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Ikard K, Janney J, Hsu LC, Isenberg DJ, Scalco MB, Schwarcz S, et al. Estimation of unmet need for HIV primary medical care: a framework and three case studies. AIDS Educ Prev. 2005;17:26–38. doi: 10.1521/aeap.2005.17.Supplement_B.26. [DOI] [PubMed] [Google Scholar]
- 22.Bamford LP, Ehrenkranz PD, Eberhart MG, Shpaner M, Brady KA. Factors associated with delayed entry into primary HIV medical care after HIV diagnosis. AIDS. 2010;24:928–930. doi: 10.1097/QAD.0b013e328337b116. [DOI] [PubMed] [Google Scholar]
- 23.Keller S, Jones J, Erbelding E. Choice of Rapid HIV testing and entrance into care in Baltimore City sexually transmitted infections clinics. AIDS Patient Care STDS. 2011;25:237–243. doi: 10.1089/apc.2010.0298. [DOI] [PubMed] [Google Scholar]
- 24.Holtgrave DR. On the epidemiologic and economic importance of the National AIDS Strategy for the United States. J Acquir Immune Defic Syndr. 2010;55:139–142. doi: 10.1097/QAI.0b013e3181f4107a. [DOI] [PubMed] [Google Scholar]
- 25.Rothman RE, Kelen GD, Harvey L, Shahan JB, Hairston H, Burah A, et al. Factors associated with no or delayed linkage to care in newly diagnosed human immunodeficiency virus (HIV)-1-infected patients identified by emergency department-based rapid HIV screening programs in two urban EDs. Acad Emerg Med. 2012;19:497–503. doi: 10.1111/j.1553-2712.2012.01351.x. [DOI] [PubMed] [Google Scholar]
- 26.Bertolli J, Shouse RL, Beer L, Valverde E, Fagan J, Jenness SM, et al. Using HIV surveillance data to monitor missed opportunities for linkage and engagement in HIV medical care. Open AIDS J. 2012;6:131–141. doi: 10.2174/1874613601206010131. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Mugavero MJ, Davila JA, Nevin CR, Giordano TP. From access to engagement: measuring retention in outpatient HIV clinical care. AIDS Patient Care STDS. 2010;24:607–613. doi: 10.1089/apc.2010.0086. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Sullivan PS, Rosenberg ES, Sanchez TH, Kelley CF, Luisi N, Cooper HL, et al. Explaining racial disparities in HIV incidence in black and white men who have sex with men in Atlanta, GA: a prospective observational cohort study. Ann Epidemiol. 2015;25:445–454. doi: 10.1016/j.annepidem.2015.03.006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Maulsby C, Millett G, Lindsey K, Kelley R, Johnson K, Montoya D, et al. HIV among Black men who have sex with men (MSM) in the United States: a review of the literature. AIDS Behav. 2014;18:10–25. doi: 10.1007/s10461-013-0476-2. [DOI] [PubMed] [Google Scholar]
- 30.Mayer KH, Wang L, Koblin B, Mannheimer S, Magnus M, del Rio C, et al. Concomitant socioeconomic, behavioral, and biological factors associated with the disproportionate HIV infection burden among Black men who have sex with men in 6 U.S. cities. PLoS One. 2014;9:e87298. doi: 10.1371/journal.pone.0087298. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Christopoulos KA, Das M, Colfax GN. Linkage and retention in HIV care among men who have sex with men in the United States. Clin Infect Dis. 2011;52(Suppl 2):S214–222. doi: 10.1093/cid/ciq045. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Giordano TP, Gifford AL, White AC, Jr, Suarez-Almazor ME, Rabeneck L, Hartman C, et al. Retention in care: a challenge to survival with HIV infection. Clin Infect Dis. 2007;44:1493–1499. doi: 10.1086/516778. [DOI] [PubMed] [Google Scholar]
- 33.AZ An Efficient Method of Estimating Seemingly Unrelated Regressions and Tests for Aggregation Bias. Journal of the American Statistical Association. 1962;57:348–368. [Google Scholar]
- 34.Stata Corp. Stata Statistical Software: Release 14. College Station, TX: StataCorp LP; 2015. [Google Scholar]
- 35.Khan MR, Miller WC, Schoenbach VJ, Weir SS, Kaufman JS, Wohl DA, et al. Timing and duration of incarceration and high-risk sexual partnerships among African Americans in North Carolina. Ann Epidemiol. 2008;18:403–410. doi: 10.1016/j.annepidem.2007.12.003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Khan MR, Rosen DL, Epperson MW, Goldweber A, Hemberg JL, Richardson J, et al. Adolescent criminal justice involvement and adulthood sexually transmitted infection in a nationally representative US sample. J Urban Health. 2013;90:717–728. doi: 10.1007/s11524-012-9742-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Iroh PA, Mayo H, Nijhawan AE. The HIV Care Cascade Before, During, and After Incarceration: A Systematic Review and Data Synthesis. Am J Public Health. 2015;105:e5–e16. doi: 10.2105/AJPH.2015.302635. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Bouris A, Hill BJ, Fisher K, Erickson G, Schneider JA. Mother-Son Communication About Sex and Routine Human Immunodeficiency Virus Testing Among Younger Men of Color Who Have Sex With Men. J Adolesc Health. 2015;57:515–522. doi: 10.1016/j.jadohealth.2015.07.007. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Schneider J, Michaels S, Bouris A. Family network proportion and HIV risk among black men who have sex with men. J Acquir Immune Defic Syndr. 2012;61:627–635. doi: 10.1097/QAI.0b013e318270d3cb. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Valente TW. Network interventions. Science. 2012;337:49–53. doi: 10.1126/science.1217330. [DOI] [PubMed] [Google Scholar]
- 41.Bouris A, Voisin D, Pilloton M, Flatt N, Eavou R, Hampton K, et al. Project nGage: Network Supported HIV Care Engagement for Younger Black Men Who Have Sex with Men and Transgender Persons. J AIDS Clin Res. 2013:4. doi: 10.4172/2155-6113.1000236. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.