Abstract
Background
Perceptions of pain as unfair are a significant risk factor for poorer physical and psychological outcomes in acute injury and chronic pain. Chief among the negative emotions associated with perceived injustice is anger, arising through frustration of personal goals and unmet expectations regarding others’ behavior. However, despite a theoretical connection with anger, the social mediators of perceived injustice have not been demonstrated in chronic pain.
Purpose
The current study examined 2 socially-based variables and a broader measure of pain interference as mediators of the relationships between perceived injustice and both anger and pain intensity in a sample of 302 patients in a tertiary care pain clinic setting.
Methods
Data from the Collaborative Health Outcomes Information Registry (CHOIR) were analyzed using cross-sectional path modeling analyses to examine social isolation, satisfaction with social roles and activities, and pain-related interference as potential mediators of the relationships between perceived injustice and both anger and pain intensity.
Results
When modeled simultaneously, ratings of social isolation mediated the relationship between perceived injustice and anger, while pain-related interference and social satisfaction did not. Neither social variable was found to mediate the relationship between perceived injustice and pain intensity, however.
Conclusions
The current findings highlight the strongly interpersonal nature of perceived injustice and anger in chronic pain, though these effects do not appear to extend to the intensity of pain itself. Nevertheless, the results highlight the need for interventions that ameliorate both maladaptive cognitive appraisal of pain and pain-related disruptions in social relationships.
Keywords: Chronic pain, perceived injustice, anger, social function, CHOIR
In the past decade, there has been a proliferation of research examining the role of justice beliefs in the context of chronic pain adaptation and treatment. Perceptions of injustice, defined broadly as blame assigned to others and feelings of irreparability of loss (1), have been identified as a significant barrier to effective recovery after acute injury and predict myriad poor outcomes in both acute pain and chronic pain populations. Individuals who view their pain as highly unjust tend to report more intense pain (2, 3), show greater susceptibility to maladaptive pain behaviors (4–7), greater pain catastrophizing (1, 3, 7), and increased rates of disability (3, 8, 9). Notably, perceived injustice is also a salient predictor of negative emotions, demonstrating strong relationships with depression (10–12), post-traumatic stress disorder symptoms after an acute injury (11, 13), and anger (3, 14–16).
Of the negative emotions connected to perceived injustice, anger is the negative emotion that shows perhaps the most robust empirical and theoretical relationship with this construct. Perceived injustice has been found to influence both pain intensity and depressive symptoms through increased feelings of anger (3). However, there is also a strong theoretical indication that perceived injustice may have consequences for social relationships, as feelings of blame, often directed towards others, are a key component of the construct of perceived injustice (1). Similarly, it is pain-related impairments in social relationships, rather than overall pain-related physical dysfunction, that appear to be more salient predictors of anger states in individuals with chronic pain (17). Conversely, supportive or meaningful social relationships appear to have protective effects for mood and function in individuals with chronic pain (18–20). Taken together, prior findings suggest that the social environment may amplify either the positive or negative aspects of everyday life for people with pain. Although some prior studies have suggested that perceived injustice may impact specific social relationships, perhaps by increasing conflict with medical providers or friends or family due to feelings of increased anger or feeling misunderstood by others (14, 15, 21), the social context of perceived injustice and its implication for anger has not been explicitly tested.
Consequently, we sought to examine the potential social underpinnings of perceived injustice in the current study by examining 3 potential mediators of the relationship between perceived injustice and anger: 2 indicators of social functioning (satisfaction with social roles and activities and social isolation), and a more general measure of perceived interference in daily life due to pain. Lower levels of satisfaction with one’s social relationships have previously been identified as a salient contributor to mood dysregulation in chronic pain (17). To date, there have been no studies examining perceived injustice and social isolation; this variable was included in the current study in order to more fully represent the construct of social disruption in chronic pain. Unlike social satisfaction, which may be affected by a variety of factors, such as the availability of social relationships, interpersonal conflict or by pain-relevant physical dysfunction (17), inclusion of social isolation was expected to better encapsulate feelings of social disconnection and loneliness that might not be assessed specifically in a measure of social satisfaction. In addition to these social mediators, we also opted to test whether pain-related interference, a construct that measures perceptions of pain as a barrier in multiple domains of everyday life that is not specifically focused on social functioning, might serve as a mediator of the relationship between perceived injustice and anger. In this way, we sought to clarify the specific social contributions of perceived injustice to anger, above and beyond general perceptions of pain as a barrier of meaningful function. As the broader literature concerning perceptions of injustice in chronic pain has regularly examined pain intensity as an outcome, we also opted to test the socially-based mediators in examining the relationship between perceived injustice and pain intensity as an exploratory analysis. These relationships were examined in a sample of 302 patients with chronic pain, presenting to an initial visit to a tertiary care pain clinic. Study data were gathered using the Collaborative Health Outcomes Information Registry (CHOIR), an open-source data registry developed by Stanford University (22).
Methods
Study procedures, which involved exclusively retrospective review of clinical data, were approved by the Institutional Review Board at the Stanford University School of Medicine.
Participants
Data were collected from the initial visits of 302 patients at the Stanford Pain Management Center, a large, tertiary care pain clinic, between April 2015 and July 2015. The sample was 62.6% female (N = 189). Patient age in the current sample ranged from 18 to 87 years (M = 47.6, SD = 14.6). In the current sample, the median education level was a completed Associate’s Degree. The majority of the sample (52.3%) reported being married at the time of data collection. Two binary variables were used to describe the work status of patients in our sample: one that indicated whether patients were currently working (“yes/no”) and one that indicated whether patients were currently on disability (“yes/no”). 46.0% of the sample (N = 139) reported being currently employed at the time of data collection, and 27.2% (N = 82) of the sample reported being their status as “disabled.” The average duration of pain in the current sample was 8.67 years (SD = 10.13; range = 90 days–33 years). In terms of pain disorders, patients self-reported their pain complaints according to several broad categories (e.g., due to nerve, muscle, disk, or bone problems, or due to specific problems like cancer). In the current sample, patients most commonly identified their pain as being due to a nerve problem (N = 139, 46.0%), followed by muscle pain (N = 82, 27.2%), disk problems (N = 66, 21.9%), bone problems (N = 33, 10.9%), infections (N = 14, 4.6%), and cancer (N = 8, 2.6%). Notably, 72 patients (23.8%) reported a belief that their pain was at least partially caused by an undiagnosed process, and 95 patients (31.5%) reported an unknown cause of their pain. Patients could endorse more than one category regarding the cause of their pain; 99 endorsed only one underlying cause of their pain, 93 endorsed 2 different pain categories, 35 endorsed 3 different categories, 18 endorsed 4 different categories, 7 endorsed 5 different categories, and 2 patients endorsed 6 different categories. Forty-eight patients did not endorse any of the provided pain categories.
Procedures
Patients were asked to complete an initial set of questionnaires through the CHOIR system, which could be completed on a day prior to their first visit to the clinic or using a tablet computer immediately before their first medical appointment at the clinic. The CHOIR system (http://choir.stanford.edu) is an open-source, open platform health outcomes registry and learning health system. CHOIR assesses several domains of physical, psychological and social functioning using Patient-Reported Outcomes Measurement Information Systems (PROMIS) item banks developed by the National Institutes of Health, as well as legacy instruments to supplement PROMIS assessments. PROMIS item banks are obtained from Northwestern University Assessment Center, including item content and item parameters. Computerized adaptive testing (CAT) is administered by CHOIR-CAT, a local implementation of the Northwestern University algorithm (23). Use of CHOIR-CAT reduces participant burden by administering a select subset of items from each item bank until the resulting measurement meets pre-set criteria for standard errors; this approach typically requires fewer items than traditional forms of assessment, which utilize a set list of items for all respondents (23–25). Data from CHOIR have been used in prior empirical work (17, 26); of note, however, the majority of the current sample is distinct from these prior studies, which utilized only data collected prior to 2015.
Measures
Perceived Injustice
Perceived injustice was assessed using the Injustice Experience Questionnaire (IEQ) (1). The construct of perceived injustice encompasses 2 related domains: irreparability of loss and self-blame (1). The IEQ consists of 12 items, scored from 0 (“Never”) to 4 (“All the time”); IEQ scores are computed as a sum score with a range from 0 to 48, with higher scores representing a greater degree of perceived injustice. The IEQ has demonstrated adequate psychometric properties (1) and been validated for use in both acute injury samples (1, 11) and chronic pain samples (8, 27). In the current sample, the internal consistency of the IEQ was high (Cronbach’s α = .918).
PROMIS Pain Intensity
Pain intensity was assessed on a numerical rating scale (NRS) using a modified PROMIS Pain Intensity scale (28). Respondents were asked to rate their average pain intensity over the previous 7 days on a scale of 0–10. Assessment of pain intensity using an NRS has been supported in prior studies (29).
PROMIS Instruments
Item banks for Satisfaction with Social Roles and Activities, Social Isolation, Pain Interference, and Anger from PROMIS (30) using the CHOIR-CAT algorithm. Although all descriptions of PROMIS item banks are available online (http://www.nihpromis.org/measures/domainframework1), their general content will be summarized here. PROMIS Satisfaction with Social Roles and Activities assess levels of satisfaction with engagement in one’s typical social roles and activities, such as engagement with one’s family, work, and leisure activities, while PROMIS Social Isolation items assess feelings of exclusion and disconnection from others. PROMIS Anger items assess the occurrence of angry moods, negative beliefs about others, verbal aggression, and attempts to control anger. PROMIS instruments utilize an Item Response Theory structure that does not yield mean scores, but rather yields t-scores (mean = 50, standard deviation = 10) (31, 32); t-scores for PROMIS instruments are normed on a large sample of the US population (30). As noted in previous CHOIR studies, CAT-based assessments demonstrate some advantages over traditional, static forms of assessment due to a smaller number of items required to reach reliable assessment of a construct, while maintaining other preferable aspects of psychometric assessment, such as lower standard errors of measurement (33). Higher scores on average pain intensity, anger, and social isolation signified greater severity of these symptoms, while higher scores on PROMIS Satisfaction with Social Roles and Activities reflect a greater degree of satisfaction with social roles and activities. Items from PROMIS Anger, Pain Interference, and Pain Intensity assess these constructs over the previous 7 days, while PROMIS Satisfaction with Social Roles and Activities and Social Isolation are assessed in a more general fashion and are not confined to a specific period of time.
Analytic Plan
Mplus software (34) was used to estimate structural path models in the current study; this analytic approach has been used in prior CHOIR publications (17, 26). In the current study, several steps were taken in analysis. First, bivariate correlations were estimated between all study variables. Second, the direct relationships between perceived injustice and both anger and pain intensity were estimated (the c path). Third, a series of mediated effects were estimated in the relationship between perceived injustice and both outcome variables. Three variables were tested as potential mediators of these relationships: pain interference, social isolation, and satisfaction with social roles and activities. Mediation models were first constructed estimating these mediated effects independently (e.g., testing the mediating effect of social isolation in the relationship between perceived injustice and each outcome variable, without any other potential mediators in the model). Finally, a fully-estimated model was tested, in which all mediators were tested simultaneously in predicting anger. As it was deemed theoretically unlikely that pain interference would act as a mediator of the relationship between perceived injustice and pain intensity, these mediated effects were not estimated. Average pain intensity over the previous 7 days was included as a covariate in all models in which anger was an outcome. Marital status and a binary variable representing current disability status were also modeled as covariates in all models, as these variables were deemed to be relevant to the social variables represented in the model.
All mediated effects were estimated using a 1000-draw bootstrap-estimated product of coefficients approach. The product of coefficients approach tests the product of the path coefficients from the predictor to the mediator (the a path) and from the mediator to the outcome (the b path). This approach has been deemed preferable in mediation analysis due to a decreased susceptibility to Type-I error and a greater ability to detect mediated effects (i.e., greater power) (35). All direct paths and mediated effects are represented using standardized path coefficients, which allows for comparison of the relative sizes of each path. However, as Mplus does not provide significance values for standardized path coefficient models, significance values are reported from identical unstandardized path coefficient models. Given that there were significant correlations between each of the examined mediators, they were freed to co-vary in the final estimated model, as we expected a significant degree of conceptual and statistical overlap between these constructs. As this final model was fully saturated, no model fit indices will be reported.
Results
Descriptive statistics can be found in Table 1, bivariate correlations between study variables can be found in Table 2, and the total proportion of variance accounted for in each endogenous variable (satisfaction with social roles and activities, social isolation, pain interference, and anger) by the full set of predictors in each model can be found in Tables 3 and 4. Patients endorsing higher levels of perceived injustice reported significantly higher levels of anger, social isolation, and pain-related interference, as well as lower levels of social satisfaction; all of these relationships were statistically significant, above and beyond the effects of pain intensity, marital status, and disability status. Patients reporting higher levels of perceived injustice also reported significantly higher levels of average pain, above and beyond the effects of marital status and disability status.
Table 1.
Means and Standard Deviations of Study Variables.
| Study Variable | Mean (SD) |
|---|---|
| NRS Average Pain Intensity | 5.66 (2.25) |
| Perceived Injustice | 17.92 (11.40) |
| PROMIS Anger | 51.00 (10.20) |
| PROMIS Pain Interference | 64.39 (7.76) |
| PROMIS Satisfaction with Social Roles and Activities | 42.09 (9.89) |
| PROMIS Social Isolation | 48.94 (9.72) |
Note: PROMIS assessments are based on a mean of 50 with a standard deviation of 10.
Note: NRS scores were assessed on an 11-point scale from 0–10.
Note: Scores are based on data from 391 individuals with chronic pain.
Table 2.
Correlations Between Study Variables
| Perceived Injustice | Social Isolation | Social Satisfaction | Pain Interference | Anger | Pain Intensity | |
|---|---|---|---|---|---|---|
| Perceived Injustice | 1 | .540 | −.480 | .482 | .543 | .347 |
| Social Isolation | 1 | −.523 | .343 | .522 | .180 | |
| Social Satisfaction | 1 | −.544 | −.453 | −.264 | ||
| Pain Interference | 1 | .428 | .551 | |||
| Anger | 1 | .312 | ||||
| Pain Intensity | 1 |
Scores are based on data from 302 individuals with chronic pain.
Note: All correlations significant at p < .01.
Table 3.
Proportion of anger variance accounted for - Perceived injustice as sole predictor, single-mediator and 3-mediator models
| Perceived Injustice Only | Social Isolation as Mediator | Social Satisfaction as Mediator | Pain Interference as Mediator | Fully Specified Model | |
|---|---|---|---|---|---|
|
| |||||
| Outcome Variable | R2 Variance | R2 Variance | R2 Variance | R2 Variance | R2 Variance |
| Anger | .293 .293 |
.408 .318 |
.362 N/A |
.342 N/A |
.428 .318 |
| Social Isolation | |||||
| Social Satisfaction | .231 .236 |
N/A N/A |
.248 N/A |
N/A .406 |
.248 .406 |
| Pain Interference | |||||
Table 4.
Proportion of pain intensity variance accounted for - Perceived injustice as sole predictor and single-mediator models
| Perceived Injustice Only | Social Isolation as Mediator | Social Satisfaction as Mediator | |
|---|---|---|---|
|
| |||
| Outcome Variable | R2 Variance | R2 Variance | R2 Variance |
| Pain Intensity | .125 | .149 | .156 |
| Social Isolation | .293 | .317 | N/A |
| Social Satisfaction | .231 | N/A | .240 |
Notably, patients who reported being currently disabled also reported significantly higher levels of pain intensity (t(163.9) = 2.56, p = .011), pain interference (t(183.0) = 3.68, p < .001), social isolation (t(150.2) = 3.30, p = .001), perceived injustice (t(136.3) = 3.26, p = .001), and anger (t(145.7) = 2.13, p = .035), and also reported significantly lower levels of social satisfaction (t(164.0) = −2.80, p = .006). Marital status was found to be a significant predictor of 3 study variables: social isolation (F(5, 296) = 2.96, p = .013), pain interference (F(5, 296) = 2.31, p = .044), and pain intensity (F(5, 296) = 2.74, p = .020). Post-hoc analyses using a Bonferroni adjustment for multiple comparisons, however, suggested fewer differences: pain intensity was significantly lower in married patients than in patients living together with a romantic partner but were not married (p = .047), and social isolation was found to be significantly lower in married patients compared to patients who were widowed (p = .049). No other post-hoc comparisons reached significance for any other study variable.
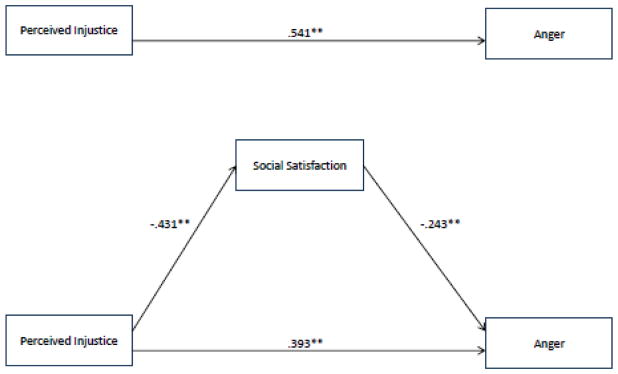
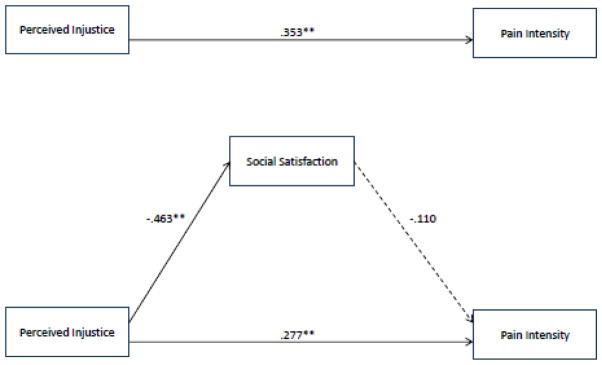
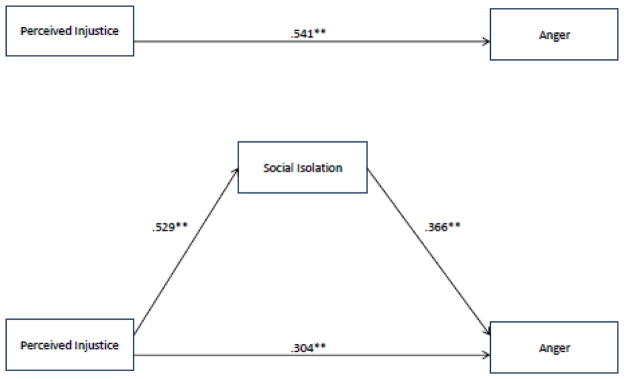
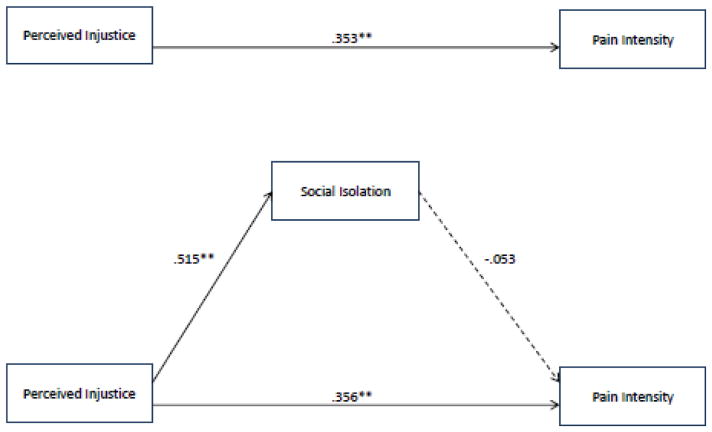
Single Mediator Models
First, single-mediator models were estimated, testing the mediating effects of social satisfaction on anger (Figure 1) and pain intensity (Figure 2), social isolation on anger (Figure 3) and pain intensity (Figure 4), and pain-related interference on anger (Figure 5). All three mediators were found to be significant predictors of anger, above and beyond the effects of pain intensity, disability status, and marital status. Similarly, social isolation, social satisfaction and pain interference were found to be significant mediators of the relationship between perceived injustice and anger, when these mediators were modeled separately. Of note, social isolation appeared to be the strongest mediator (i.e., demonstrated the largest coefficient as a mediator and accounted for the greatest proportion of the relationship) between perceived injustice and anger, whereas pain interference appeared to account for the smallest proportion of this relationship when modeled as the sole mediator.
Figure 1.
Social satisfaction as a mediator of the relationship between perceived injustice and anger.
Note: ** = p < .01, * = p < .05
Note: Mediated effect of social satisfaction was significant (ab = .110, p < .001).
Figure 2.
Social satisfaction as a mediator of the relationship between perceived injustice and pain intensity.
Note: ** = p < .01, * = p < .05
Note: Mediated effect of social isolation was significant (ab = .210, p < .001).
Figure 3.
Social isolation as a mediator of the relationship between perceived injustice and anger.
Note: ** = p < .01, * = p < .05
Note: Mediated effect of social isolation was significant (ab = .210, p < .001).
Figure 4.
Social isolation as a mediator of the relationship between perceived injustice and pain intensity.
Note: ** = p < .01, * = p < .05
Note: Mediated effect of social satisfaction was significant (ab = −.033, p = .28).
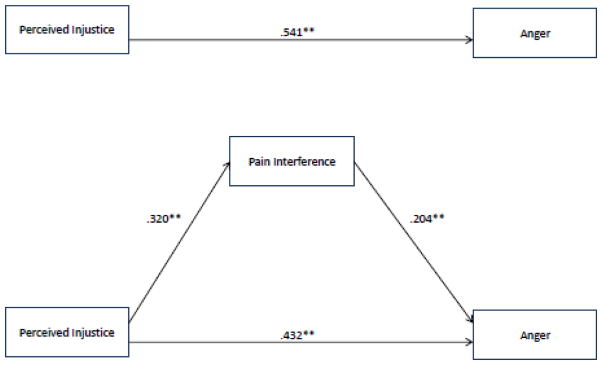
Figure 5.
Pain interference as a mediator of the relationship between perceived injustice and anger.
Note: ** = p < .01, * = p < .05
Note: Mediated effect of pain interference was significant (ab = .046, p = .010).
Neither social isolation nor social satisfaction was a significant predictor of pain intensity ratings when perceived injustice, disability status, and marital status were also included as predictors in the models. Accordingly, neither social variable mediated the relationship between perceived injustice and pain intensity.
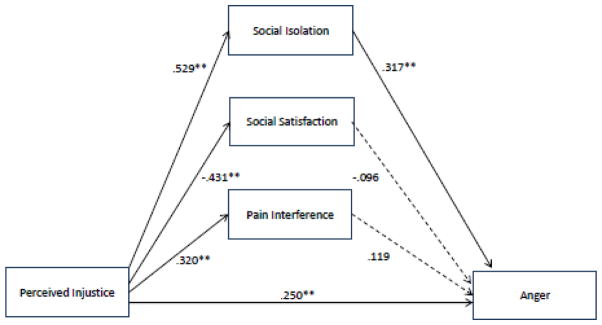
Fully-Estimated Model
Figure 6 depicts an estimated model in which all three potential mediators (social isolation, social satisfaction, and pain interference) were modeled simultaneously in the relationship between perceived injustice and anger. Of note, when these mediators were modeled simultaneously, social isolation remained the strongest predictor of anger, while social satisfaction and pain interference did not significantly predict anger, above and beyond the effects of other predictors in the model. Similarly, social isolation, but not pain interference or social satisfaction, was found to significantly mediate the relationships between perceived injustice and anger. As neither social isolation nor social satisfaction were found to be mediators in the single-mediator models predicting pain intensity, a fully-estimated model in which both mediators were tested concurrently was deemed to be unnecessary. As an exploratory step, a 3-mediator model was estimated in which both pain intensity and anger were modeled as outcomes; in this model, there was a modest but statistically significant relationship between pain intensity and anger (r = .172, p = .004), above and beyond the effects of each mediator and covariate.
Figure 6.
Pain interference, social isolation, and social satisfaction as mediators of the relationship between perceived injustice and anger.
Note: Mediated effects of social satisfaction (ab = .053, p = .047) and social isolation (ab = .178, p < .001) were significant, but pain interference was not a significant mediator (ab = .018, p = .28).
Discussion
Perceived injustice, defined as feelings of blame and the irreparability of loss related to an acute injury or chronic pain condition, has significant implications for negative emotional states in individuals with chronic pain. However, despite some theoretical ties between perceived injustice and disrupted social relationships, the interpersonal mediators of the relationship between perceived injustice and anger have not been previously explored. In our sample of 302 individuals with chronic pain, perceived injustice was found to significantly impact ratings of anger through feelings of social isolation, but not through general perceptions of pain-related interference. To our knowledge, the current study is the first to demonstrate the notable degree to which interpersonal factors connect perceived injustice to anger. However, results suggested that social variables did not mediate the relationship between perceived injustice and pain intensity, and anger showed only a modest correlation with pain intensity, above and beyond the effects of other variables in the model. These results suggest that the aspects of social functioning affected by perceived injustice have clearer implications for affective states of a person with pain, but do not appear to show a strong direct relationship with the experience of pain itself.
The results of this study are informative in several ways. First, they clearly highlight the interpersonal implications of perceived injustice, which have not been demonstrated in prior empirical studies. The relationship between perceived injustice and social disruption is not surprising; as noted previously, one of the key constructs contributing to feelings of perceived injustice is a sense of blame and unfairness (1). These constructs are inextricably tied to the social world, as feelings of blame necessitate identification of a person or situation responsible for one’s current troubles. Similarly, feelings of unfairness related to pain are likely to involve a degree of social comparison; it is only by viewing the situations of comparable others that one might infer whether a situation is unfair (36, 37). Further, prior evidence suggests that feelings of injustice are directed towards external figures, including others who may be responsible for pain-related difficulties (as in the case of acute injuries due to the negligence of others), those responsible for treating pain (such as medical providers), and society as a whole, from which an individual with chronic pain may feel alienated or stigmatized (15).
The current findings also contribute to the relatively small literature examining psychosocial processes underlying anger in chronic pain. A recent publication using CHOIR data, which used a largely non-overlapping study sample from the same population of tertiary care pain clinic patients, highlighted the relative importance of social factors in anger states in individuals with chronic pain (17). The current study findings differ somewhat from this prior publication, in that social satisfaction was not found to be a key mediator in the fully-specified model; however, it may be that the negatively-valenced social isolation domain is a better conceptual fit in representing the negative social and emotional consequences of perceived injustice. Nevertheless, the current study expands upon prior findings by highlighting that social contributors to anger rely primarily on perceptions of inequity or irreversibility of pain and pain-related consequences. It is notable that pain interference, although a significant mediator of the relationship between perceived injustice and anger in a single-mediator model, was not a significant mediator in the fully-specified model. This finding was unexpected, as prior research has suggested that anger may originate from frustration of personal goals, and pain interference might be construed as a broad measure of the degree to which an individual views his or her pain as a barrier in everyday life (38). As the broad construct of pain interference is not bereft of social factors (items in the PROMIS Pain interference item bank assess pain-related interference in social domains), this finding may suggest that the extent to which pain interference connected perceived injustice and anger in the single-mediator model may have been due to interference specifically in social function due to pain, and not necessarily in other domains of function.
Our findings may also have implications for future treatment. Of note, it has been recently suggested that stronger beliefs related to perceived injustice reflect a greater degree of psychological inflexibility, which underlies a great deal of maladaptive cognitive and behavioral reactions to pain (39). The model of psychological flexibility emphasizes that optimal responses to pain or challenge are best defined in a context of one’s goals and the broader environment (40, 41). Individuals who view their pain-related difficulties as containing a high degree of injustice may thus be at higher risk of inflexible responses to pain, reducing their ability to act in ways consistent with their personal values and with appropriate regard to the social context (39). This phenomenon may manifest noticeably in the context of pain treatment, where patients who dwell on the unfairness of their pain and the likelihood that they will not return to a previous, higher state of function, may be prone to less effective utilization of medical and psychological resources that may otherwise bolster recovery (15). Consequently, treatment approaches designed to increase psychological flexibility, such as contextual cognitive-behavioral therapy or acceptance and commitment therapy, may ameliorate some of the negative consequences of perceived injustice (39). Further, treatments that ameliorate feelings of isolation, disconnection, and disengagement from social support may be useful in addressing the problems caused by perceived injustice. One nascent treatment approach in this area concerns social intelligence interventions, which are designed to ameliorate interpersonal difficulties through the promotion of cognitive patterns that facilitate healthier and more rewarding social relationships (42, 43).
Limitations
The current study includes some limitations that warrant mention. First, the study sample was comprised solely of patients in a tertiary care pain clinic. The tertiary care nature of the sample suggests that many of the individuals had been seeking treatment for many years, often with limited success; indeed, the current sample demonstrated high levels of pain-related interference, a high rate of disability, and an average pain duration of more than 8 years. The chronic and refractory nature of the pain complaints for many patients in the current sample may thus complicate generalization of the effects of our examined study variables in acute or more treatment-responsive pain conditions. Further, the long-term nature of chronic pain in the current sample may suggest that perceptions of injustice may have developed and been maintained differently than in samples of individuals facing acute trauma, where elements of blame and irreparability of loss may be more recent or salient due to the nature of injury and the suddenness of loss.
Additionally, causal inferences in terms of the directionality of examined effects cannot be made due to the cross-sectional nature of the data. Although several of the PROMIS measures are designed to measure symptoms in a fairly circumscribed window of time (e.g., over the previous 7 days), we cannot state definitively that perceptions of injustice cause social disruption or anger. Indeed, there is a reasonable argument to be made that, during states of increased anger or feelings of increased social isolation, pain and pain-related difficulties may be viewed as more irreparable and more unjust. At a conceptual level, however, the temporal precedence of effects may be somewhat less important in the current model than in some cross-sectional models. Our results connect perceived injustice to anger using factors in one domain (social isolation) while demonstrating that other key aspects of pain experience (namely, the perception of pain as a barrier) do not factor significantly in this relationship. Given that the base of research examining predictors or correlates of anger in chronic pain populations is relatively sparse, we propose that the statistical models in the current paper remain valuable despite these limitations, even if they are interpreted simply as a network of associations between variables with no implicit assumption of causality.
Given the limitations of cross-sectional analysis, however, we nevertheless urge greater attention to these factors in future longitudinal studies, where the stability of constructs can be better measured, as well as using daily diary or experience sampling method (ESM) approaches, which yield time-series data that may be used to more clearly demonstrate temporal precedence of an effect. It is similarly noteworthy that recent experimental studies have highlighted the vulnerability of maladaptive responses to pain after a violation of beliefs related to justice (6); use of experimental methodologies may allow for greater causal inference than can be drawn by cross-sectional, self-report studies. Additionally, greater causal evidence may be gleaned from clinical intervention studies designed to improve social relationships; if reductions in feelings of social isolation are found to occur without corresponding changes in perceived injustice beliefs, this may provide a degree of specificity in the causal ordering of these effects (i.e., that social benefits may be a downstream consequence of reduced perceptions of injustice). Similarly, if an intervention designed specifically to reduce perceived injustice is found to predict concurrent improvements in social functioning, it may provide additional evidence of the temporal precedence of the effects of perceived injustice on interpersonal relationships.
Directions for Future Research
Although our findings suggest that perceived injustice may overlap with anger largely because of disrupted social relationships, it would be worthwhile to validate these effects in specific interpersonal domains. For example, it may be worthwhile to determine if individuals who report higher levels of perceived injustice from their pain also view themselves as having a poorer alliance with their treatment providers. Prior evidence suggests that the cognitive appraisals of both medical providers and patients affect perceptions and behaviors within existing treatment relationships (44, 45). Given that many patients report feeling misunderstood and stigmatized by the “invisible” nature of their pain and consequently may show less willingness to engage in treatment, it would be worthwhile to determine whether there may be a similar effect in individuals who view their pain as a permanent and unjust entity.
Further, perceived injustice may have implications for the behavior of other people close to an individual with pain. More specifically, assessing perceptions of injustice in others who are close to the pain sufferer (whether or not significant others, for example, believe that the pain experienced by their loved ones is unfair) may yield highly useful information about how perceived injustice might affect function, relationships, or treatment response. It may be, for example, that asynchrony between these perceptions (e.g., if one’s partner does not view the pain of the sufferer as highly unjust while perceived injustice beliefs are high in the person with pain) contributes to a heightened degree of distress. Alternatively, if both members of a romantic relationship view this pain as unfair, it may further exacerbate maladaptive coping attempts by reinforcing beliefs that pain is unchangeable and cannot be understood by others.
Finally, prior social experiences warrant inclusion in future models of perceived injustice. For example, individuals who have experienced previous traumas, particularly those suffered at the hands of others (as in the case of abuse or neglect), might be predisposed to identify and ruminate upon the inequity of pain experiences. This phenomenon may also generalize to broader, societal forms of inequity; prior studies have suggested that beliefs about justice and fairness are dependent on the personal needs of the pain sufferer, as well as aspects of socioeconomic status and social class (46).
Conclusions
The current study expanded upon the extant literature demonstrating the deleterious consequences of perceived injustice in chronic pain. Our results suggest that perceived injustice contributes to greater anger, a significant risk factor for poorer pain-related outcomes, primarily by increasing feelings of isolation and disconnection from others. This social dysregulation appears to be the most salient feature of the relationship between perceived injustice and anger, though these social variables did not appear to be significantly related to the intensity of pain itself. Our results highlight the importance of social context in understanding the plight of individuals facing a chronic pain condition. Consequently, treatment for chronic pain may be improved through implementation of approaches that increase psychological flexibility and ameliorate ongoing forms of social isolation, conflict, and disconnection that may manifest as a result of pain and perceived injustice.
Acknowledgments
The authors wish to acknowledge funding from the National Institutes of Health (NIH HHSN 271201200728P, NIH K24 DA029262, NIH P01 AT006651, and NIH/NIDA 3T32DA035165-02S1), as well as the Redlich Pain Endowment.
Footnotes
The authors have no other financial conflicts to disclose.
References
- 1.Sullivan MJ, Adams H, Horan S, et al. The role of perceived injustice in the experience of chronic pain and disability: scale development and validation. Journal of occupational rehabilitation. 2008;18:249–261. doi: 10.1007/s10926-008-9140-5. [DOI] [PubMed] [Google Scholar]
- 2.Ferrari R. Perceived injustice in fibromyalgia and rheumatoid arthritis. Clinical Rheumatology. 2014;33:1501–1507. doi: 10.1007/s10067-014-2552-z. [DOI] [PubMed] [Google Scholar]
- 3.Scott W, Trost Z, Bernier E, Sullivan MJ. Anger differentially mediates the relationship between perceived injustice and chronic pain outcomes. Pain. 2013;154:1691–1698. doi: 10.1016/j.pain.2013.05.015. [DOI] [PubMed] [Google Scholar]
- 4.Sullivan MJ, Davidson N, Garfinkel B, Siriapaipant N, Scott W. Perceived injustice is associated with heightened pain behavior and disability in individuals with whiplash injuries. Psychological Injury and Law. 2009;2:238–247. [Google Scholar]
- 5.Sullivan MJ, Adams H, Martel M-O, Scott W, Wideman T. Catastrophizing and perceived injustice: risk factors for the transition to chronicity after whiplash injury. Spine. 2011;36:S244–S249. doi: 10.1097/BRS.0b013e3182387fed. [DOI] [PubMed] [Google Scholar]
- 6.Trost Z, Scott W, Lange J, et al. An experimental investigation of the effect of a justice violation on pain experience and expression among individuals with high and low just world beliefs. Eur J Pain. 2014;18:415–423. doi: 10.1002/j.1532-2149.2013.00375.x. [DOI] [PubMed] [Google Scholar]
- 7.Yakobov E, Scott W, Stanish W, et al. The role of perceived injustice in the prediction of pain and function after total knee arthroplasty. PAIN®. 2014;155:2040–2046. doi: 10.1016/j.pain.2014.07.007. [DOI] [PubMed] [Google Scholar]
- 8.Scott W, Trost Z, Milioto M, Sullivan MJ. Further validation of a measure of injury-related injustice perceptions to identify risk for occupational disability: a prospective study of individuals with whiplash injury. Journal of occupational rehabilitation. 2013;23:557–565. doi: 10.1007/s10926-013-9417-1. [DOI] [PubMed] [Google Scholar]
- 9.Scott W, Trost Z, Milioto M, Sullivan MJ. Barriers to Change in Depressive Symptoms After Multidisciplinary Rehabilitation for Whiplash: The Role of Perceived Injustice. Clin J Pain. 2015;31:145–151. doi: 10.1097/AJP.0000000000000095. [DOI] [PubMed] [Google Scholar]
- 10.Scott W, Sullivan M. Perceived injustice moderates the relationship between pain and depressive symptoms among individuals with persistent musculoskeletal pain. Pain Research & Management: The Journal of the Canadian Pain Society. 2012;17:335. doi: 10.1155/2012/501260. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Trost Z, Agtarap S, Scott W, et al. Perceived injustice after traumatic injury: Associations with pain, psychological distress, and quality of life outcomes 12 months after injury. Rehabilitation Psychology. 2015;60:213. doi: 10.1037/rep0000043. [DOI] [PubMed] [Google Scholar]
- 12.Yakobov E, Scott W, Tanzer M, et al. Validation of the Injustice Experiences Questionnaire adapted for use with patients with severe osteoarthritis of the knee. Journal of Arthritis. 2014;3:130–136. [Google Scholar]
- 13.Sullivan MJ, Thibault P, Simmonds MJ, et al. Pain, perceived injustice and the persistence of post-traumatic stress symptoms during the course of rehabilitation for whiplash injuries. Pain. 2009;145:325–331. doi: 10.1016/j.pain.2009.06.031. [DOI] [PubMed] [Google Scholar]
- 14.Trost Z, Vangronsveld K, Linton SJ, Quartana PJ, Sullivan MJ. Cognitive dimensions of anger in chronic pain. Pain. 2012;153:515–517. doi: 10.1016/j.pain.2011.10.023. [DOI] [PubMed] [Google Scholar]
- 15.McParland JL, Eccleston C. “It’s Not Fair” Social Justice Appraisals in the Context of Chronic Pain. Curr Dir Psychol Sci. 2013;22:484–489. [Google Scholar]
- 16.Sullivan MJ, Scott W, Trost Z. Perceived injustice: a risk factor for problematic pain outcomes. Clin J Pain. 2012;28:484–488. doi: 10.1097/AJP.0b013e3182527d13. [DOI] [PubMed] [Google Scholar]
- 17.Sturgeon JA, Dixon EA, Darnall BD, Mackey SC. Contributions of Physical Function and Satisfaction with Social Roles to Emotional Distress in Chronic Pain: A Collaborative Health Outcomes Information Registry (CHOIR) Study. Pain. 2015 doi: 10.1097/j.pain.0000000000000313. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Evers AWM, Kraaimaat FW, Geenen R, Jacobs JWG, Bijlsma JWJ. Pain coping and social support as predictors of long-term functional disability and pain in early rheumatoid arthritis. Behaviour Research and Therapy. 2003;41:1295–1310. doi: 10.1016/s0005-7967(03)00036-6. [DOI] [PubMed] [Google Scholar]
- 19.Ferreira VM, Sherman AM. The relationship of optimism, pain and social support to well-being in older adults with osteoarthritis. Aging Ment Health. 2007;11:89–98. doi: 10.1080/13607860600736166. [DOI] [PubMed] [Google Scholar]
- 20.Onoda K, Okamoto Y, Nakashima K, et al. Decreased ventral anterior cingulate cortex activity is associated with reduced social pain during emotional support. Soc Neurosci. 2009;4:443–454. doi: 10.1080/17470910902955884. [DOI] [PubMed] [Google Scholar]
- 21.Sullivan MJ, Yakobov E, Scott W, Tait R. Perceived injustice and adverse recovery outcomes. Psychological Injury and Law. 2014;7:325–334. [Google Scholar]
- 22.Collaborative Health Outcomes Information Registry (CHOIR) from http://choir.stanford.edu.
- 23.Gershon R, Rothrock NE, Hanrahan RT, et al. The development of a clinical outcomes survey research application: Assessment CenterSM. Quality of Life Research. 2010;19:677–685. doi: 10.1007/s11136-010-9634-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Kao MCJ, Cook K, Olson G, Pacht T, Darnall BD, Weber SC, Mackey SC. SNAPL-CAT: Catalyzing the rate-limiting step of big data psychometrics with item-response theory and advanced computerized adaptive testing (poster presentation). American Medical Informatics Associations (AMIA) 2014 Joint Summits on Translational Science; San Francisco, CA. 2014. [Google Scholar]
- 25.Cella D, Gershon R, Lai J-S, Choi S. The future of outcomes measurement: item banking, tailored short-forms, and computerized adaptive assessment. Quality of Life Research. 2007;16:133–141. doi: 10.1007/s11136-007-9204-6. [DOI] [PubMed] [Google Scholar]
- 26.Sturgeon JA, Darnall BD, Kao M-CJ, Mackey SC. Physical and Psychological Correlates of Fatigue and Physical Function: A Collaborative Health Outcomes Information Registry (CHOIR) Study. The Journal of Pain. 2014;16:291–298. e291. doi: 10.1016/j.jpain.2014.12.004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Rodero B, Luciano JV, Montero-Marín J, et al. Perceived injustice in fibromyalgia: Psychometric characteristics of the Injustice Experience Questionnaire and relationship with pain catastrophising and pain acceptance. Journal of Psychosomatic Research. 2012;73:86–91. doi: 10.1016/j.jpsychores.2012.05.011. [DOI] [PubMed] [Google Scholar]
- 28.Farrar JT, Young JP, Jr, LaMoreaux L, Werth JL, Poole RM. Clinical importance of changes in chronic pain intensity measured on an 11-point numerical pain rating scale. Pain. 2001;94:149–158. doi: 10.1016/S0304-3959(01)00349-9. [DOI] [PubMed] [Google Scholar]
- 29.Cook KF, Dunn W, Griffith JW, et al. Pain assessment using the NIH Toolbox. Neurology. 2013;80:S49–S53. doi: 10.1212/WNL.0b013e3182872e80. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Cella D, Yount S, Rothrock N, et al. The Patient-Reported Outcomes Measurement Information System (PROMIS): progress of an NIH Roadmap cooperative group during its first two years. Med Care. 2007;45:S3–S11. doi: 10.1097/01.mlr.0000258615.42478.55. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Amtmann D, Cook KF, Jensen MP, et al. Development of a PROMIS item bank to measure pain interference. Pain. 2010;150:173–182. doi: 10.1016/j.pain.2010.04.025. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Hays RD, Bjorner JB, Revicki DA, Spritzer KL, Cella D. Development of physical and mental health summary scores from the patient-reported outcomes measurement information system (PROMIS) global items. Qual Life Res. 2009;18:873–880. doi: 10.1007/s11136-009-9496-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Fries JF, Cella D, Rose M, Krishnan E, Bruce B. Progress in assessing physical function in arthritis: PROMIS short forms and computerized adaptive testing. J Rheumatol. 2009;36:2061–2066. doi: 10.3899/jrheum.090358. [DOI] [PubMed] [Google Scholar]
- 34.Muthén LK, Muthén BO. Mplus: Statistical Analysis with Latent Variables; User’s Guide;[Version 5] Muthén & Muthén; 2007. [Google Scholar]
- 35.MacKinnon DP, Lockwood CM, Williams J. Confidence limits for the indirect effect: Distribution of the product and resampling methods. Multivariate Behavioral Research. 2004;39:99–128. doi: 10.1207/s15327906mbr3901_4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Smith RH, Parrott WG, Ozer D, Moniz A. Subjective injustice and inferiority as predictors of hostile and depressive feelings in envy. Personality and Social Psychology Bulletin. 1994;20:705–711. [Google Scholar]
- 37.Kawakami K, Dion KL. Social Identity and Affect as Determinants of Collective Action Toward an Integration of Relative Deprivation and Social Identity Theories. Theory & Psychology. 1995;5:551–577. [Google Scholar]
- 38.Fernandez E, Turk DC. The scope and significance of anger in the experience of chronic pain. Pain. 1995;61:165–175. doi: 10.1016/0304-3959(95)00192-U. [DOI] [PubMed] [Google Scholar]
- 39.Scott W, McCracken LM, Trost Z. A psychological flexibility conceptualisation of the experience of injustice among individuals with chronic pain. British Journal of Pain. 2013 doi: 10.1177/2049463713514736. 2049463713514736. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.McCracken LM, Morley S. The psychological flexibility model: a basis for integration and progress in psychological approaches to chronic pain management. J Pain. 2014;15:221–234. doi: 10.1016/j.jpain.2013.10.014. [DOI] [PubMed] [Google Scholar]
- 41.McCracken LM, Vowles KE. Acceptance and commitment therapy and mindfulness for chronic pain: Model, process, and progress. American psychologist. 2014;69:178. doi: 10.1037/a0035623. [DOI] [PubMed] [Google Scholar]
- 42.Zautra AJIF, Zautra E, Gallardo C, Velasco L. The humanization of social relations: Nourishment for resilience in mid-life. In: Ong A, Löckenhoff C, editors. New Developments in Emotional Aging. Washington, DC: American Psychological Association; In press. [Google Scholar]
- 43.Zautra AJ. Advancing Pain Care through Behavior Change Science & Mobile Health Technologies Conference: The Translational Research Institute on Pain in Later Life (TRIPLL) Cornell Medical School; New York City, New York: 2015. Fostering Resilience to Chronic Pain through the Humanization of Social Relations. [Google Scholar]
- 44.De Ruddere L, Goubert L, Stevens MAL, et al. Health care professionals’ reactions to patient pain: impact of knowledge about medical evidence and psychosocial influences. The Journal of Pain. 2014;15:262–270. doi: 10.1016/j.jpain.2013.11.002. [DOI] [PubMed] [Google Scholar]
- 45.Newton BJ, Southall JL, Raphael JH, Ashford RL, LeMarchand K. A narrative review of the impact of disbelief in chronic pain. Pain Manag Nurs. 2013;14:161–171. doi: 10.1016/j.pmn.2010.09.001. [DOI] [PubMed] [Google Scholar]
- 46.McParland JL, Eccleston C, Osborn M, Hezseltine L. It’s not fair: an interpretative phenomenological analysis of discourses of justice and fairness in chronic pain. Health. 2011;15:459–474. doi: 10.1177/1363459310383593. [DOI] [PubMed] [Google Scholar]