Abstract
Background
Limited access to resources can significantly impact health behaviors. Previous research on food insecurity and HIV has focused on establishing the relationship between lacking access to nutritious food and antiretroviral (ARV) medication non-adherence in a variety of social contexts.
Purpose
This study aims to determine if several aspects of food insecurity co-occur with missed doses of medication on a daily basis among a sample of people living with HIV who have recently experienced hunger.
Methods
The current study utilized a prospective, observational design to test the daily relationship between food insecurity and medication non-adherence. Participants were followed for 45 days and completed daily assessments of food insecurity and alcohol use via interactive text message surveys and electronic medication adherence monitoring using the Wisepill.
Results
Fifty-nine men and women living with HIV contributed a total of 2,655 days of data. Results showed that severe food insecurity (i.e. hunger), but not less severe food insecurity (i.e. worrying about having food), significantly predicted missed doses of medication on a daily level. Daily alcohol use moderated this relationship in an unexpected way; when individuals were hungry and drank alcohol on a given day they were less likely to miss a dose of medication.
Conclusions
Among people living with HIV with recent experiences of hunger, this study demonstrates that there is a daily relationship between hunger and nonadherence to antiretroviral therapy. Future research is needed to test interventions designed to directly address the daily relationship between food insecurity and medication non-adherence.
Keywords: Food insecurity, HIV/AIDS, adherence, alcohol use, multi-level modeling
HIV infections are largely concentrated among those with low socioeconomic status (SES) [1, 2]. Individuals living in poverty face a myriad of social disadvantages, including overcrowding, restricted access to nutritious food, and violence, all of which have direct implications for health and well-being [3–5]. People living in poverty with HIV have limited access to the resources necessary to “survive and thrive” [6]. For optimal adherence to medications, people living with HIV require tangible resources including food, shelter, money to purchase their medications, and transportation. Additionally, individuals must also have cognitive resources to cope with their disease and adequately carry out the necessary tasks associated with medication adherence There are also competing demands for these resources. For example, a person living with co-morbid HIV infection and a substance use disorder will have only limited funds and must decide between buying food and substances [7].
Food insecurity can be construed as a marker of socioeconomic marginalization. Food insecurity is “the limited availability of nutritionally adequate or safe food, or the inability to procure food in socially acceptable ways” [8]. Among people living with HIV, food insecurity is particularly detrimental because it can lead to malnutrition, which exacerbates the adverse health outcomes of immune suppression resulting from HIV infection. Both malnutrition and HIV impact immune system functioning and when these two conditions co-occur the impact on the immune system is compounded and synergistic [9]. In addition to the detrimental impacts that food insecurity has on the physical health of people living with HIV, food insecurity has also been associated with worse health behaviors, such as lower antiretroviral (ARV) medication adherence and higher levels of sexual risk behavior [10, 11].
In a systematic review of studies reporting on the relationship between food insecurity and ARV medication adherence, nine out of thirteen studies that adjusted for other markers of poverty found statistically significant relationships such that greater food insecurity predicted lower ARV adherence [11]. In one of the few longitudinal studies in this literature, Weiser, Yuan et al., (2013) followed 284 unstably housed participants for a median of 22 months in San Francisco, CA. Weiser, et al. [12] found that food insecurity was associated with higher odds of medication non-adherence, having incomplete HIV RNA viral suppression, and having a CD4 T-cell count of less than 200. From their review, Singer, Weiser and McCoy [11] concluded that across multiple settings in resource poor and resource rich countries, food insecurity is an important barrier to ARV adherence. Several explanations for this relationship have been offered including purposeful non-adherence due to prescriptions with food requirements, side effects, competing resource demands, and the exacerbation of hunger during the initiation phase of ARVs [13, 14].
Food insecurity is fairly common among substance users, however, it is unknown if there is an interaction between alcohol use and food insecurity. Among alcohol users in Atlanta, Kalichman et al. [15] found that 43% of participants experienced food insecurity. Alcohol use has been related to medication adherence among food insecure populations. In South Africa, Morojele, Kekvaletswe, & Nkosi [16] found that alcohol use was independently associated with ARV adherence when controlling for socioeconomic status, having a stable living situation and food insecurity. Alcohol use, particularly alcohol addiction, and food insecurity, are competing demands for limited resources that can have direct implications on ARV adherence. Alcohol use is an important factor to consider when observing the daily relationship between aspects of food insecurity and medication adherence.
The relationship between food insecurity and ARV non-adherence is robust in the literature and previous studies have extensively controlled for other indicators of SES. Previous work has also established the causal relationship between food insecurity and ARV non-adherence [17,18]. However, it is unknown if days when a person lacks food are the same days when they miss their medications. The temporal relationship between food insecurity and non-adherence is assumed in interventions that provide food to improve adherence [19], but whether or not these two events occur on the same day is unknown. A true test of whether medication non-adherence occurs on days with limited access to food requires data collection of both food insecurity and ARV adherence at the day level in a prospective study design.
The purpose of the current study was to test the daily relationship between several aspects of food insecurity and medication non-adherence among people living with HIV with recent experiences of hunger. Additionally, to better understand the interaction between alcohol use and food insecurity on medication adherence, daily alcohol use was tested as a moderator of the relationship between food insecurity and medication adherence, using alcohol use dichotomously (did not drink vs. drank alcohol) to determine if simply drinking alcohol on a given day interacts with aspects of food insecurity and continuously to determine if quantity of alcohol consumed interacts with food insecurity.
Methods
The current study employed an observational cohort design that included 45-days of daily text message surveys and daily electronic medication monitoring. Participants also completed a computer-assisted interview and provided their CD4 T-cell count and HIV RNA viral load retrieved from their medical records. Participants were compensated for all completed study activities and the University Institutional Review Board approved the study protocol.
Population and Screening
Study participants consisted of men and women living with HIV/AIDS in and around Atlanta, GA, an area with a substantial HIV epidemic [20]. Atlanta has the seventh highest number of new HIV diagnoses for large metropolitan areas [21]. Notices announcing the study were posted in infectious disease clinics and interested persons called the study site and were screened for the study. Eligibility criteria included (a) being 18 or older, (b) name-matching proof of positive HIV status and photo identification, (c) currently taking antiretroviral medications (ARVs), (d) self-reported missing at least one dose of medication in the past month, (e) self-reported being hungry in the past month but unable to eat because he/she could not afford food, (f) self-reported consumption of at least one alcoholic beverage within the past month, and (g) willingness to use a Wisepill device for medication management. If the participant was deemed eligible, the screener gave the participant an enrollment appointment.
Enrollment Session
Participants were consented into the study and then completed an audio-computer assisted self-interview (ACASI) to gather basic demographic information including gender, race/ethnicity, education, and age. After the participants completed the ACASI, the assessor instructed them on how to complete the daily text message surveys and each participant completed a practice survey in the office. A project cell phone was provided to each participant. Finally, the assessor explained electronic medication monitoring (see below). The participants were instructed to use an electronic device to hold their ARV medication for the entirety of the study and to refill it themselves as needed.
Daily Data Collection
We provided participants with a study cell phone to deliver daily interactive text-message assessments. Participants received the same text message survey every day for 45 days and the questions referred to the previous day’s activities. This type of daily measurement has been used to assess a wide variety of health behaviors and cognitions including sexual risk behaviors, depression, coping skills, and alcohol consumption [22–25]. In addition, we monitored daily ARV adherence using electronic devises for assessing adherence contemporaneous with food insecurity at the day level. A time frame of 45 days was chosen for two reasons. In order to estimate the association of day-level events, the number of assessments (days) within the individual had to be large rather than focusing on a large individual sample size. Additionally, individuals living in poverty who often rely on government or state assistance financial resources (i.e. food stamps, Social Security benefits), receive these payments only once or twice a month. It is possible that severity of food insecurity differ on the days leading up to payments versus days directly following payments. In order to capture these potential fluctuations, the time period in which participants were observed had to be greater than one month.
Daily aspects of food insecurity
We assessed several aspects of food insecurity on a daily basis. Participants answered three questions adapted from the USDA Household Food Security Scale [26]. These items are answered with a yes or a no response and are as follows: “I worried about my food running out yesterday,” “I ate less than I needed to yesterday,” and “I was hungry, but could not eat because I couldn’t afford food yesterday.” Responses were dichotomous, 1=Yes, 0=No. These particular aspects were selected because we felt they might have the highest variability on a daily basis, however, they do not capture other important aspects of food insecurity, such as quality of food.
Daily alcohol use
To assess alcohol, participants were asked “How many alcohol drinks did you have yesterday? If you did not drink say 0.” These responses were used in two ways: 1) dichotomously to indicate 0 = ‘Did not drink’ or 1 = ‘Drank alcohol’ to determine whether or not drinking on a given day impacts adherence and 2) continuously to capture whether or not quantity of alcohol matters.
Medication adherence
Daily medication adherence data was collected using the Wisepill device [27–29]. This device functions as a medication pillbox with sensors for opening and closing. When a participant opens the Wisepill device to take their medication, a date and time stamp is created which is then sent to a central server via general packet radio service (GPRS). This information is then accessible via a secure, internet-based interface. These data were downloaded from the website and compared to each participant’s dosing schedule. For the individual level analyses this information was used to calculate an aggregate adherence percentage for the 45-day period. For the day level analyses this information was coded dichotomously for missed doses. For example, if a participant opened their Wisepill device on a day only once for a medication that is prescribed twice daily the medication was coded as a missed day. Wisepill signal lapses of 48 hours or greater were investigated by a phone call to the participant to determine whether the lapse was due to a technical failure (battery failure, loss of cellular signal) or if it was due to a behavioral cause (pocket dose, missed dose) [27]. An adjusted adherence that factored in reported pocket doses was calculated [28].
Chart Abstracted HIV RNA Viral Load and CD4 T Cell Count
During the study, participants were asked to obtain a copy of their latest HIV RNA viral load and CD4 T cell counts from their health care provider and these records could be no older than 3 months. These records had to be marked with a clinic stamp to verify its authenticity. For consistency across viral load chart values, we defined undetectable viral load as <50 copies/mL.
Financial Assessment
Following the 45-day observation period, participants completed a financial assessment with a trained staff member. Participants were asked about where the source of any received financial resources, the amount of money or money equivalent (i.e. food stamps) received, and when they received that payment for the past 45 days. Participants were also asked about any jobs (full time/part time/side work), short-term disability, Social Security, unemployment assistance, food stamps, and any other types of monetary assistance that they received.
Statistical Analyses
To characterize the sample, means and rates were calculated using demographic information collected in the ACASI, the chart abstracted lab reports, and the financial assessment. Rates were also calculated for the day-level behaviors from the text message surveys and the Wisepill device. To analyze the relationship between aspects of food insecurity and medication adherence, two-levels of analysis were used. At the individual level, behaviors were collapsed across the 45-day period. Bivariate and multivariate regressions were conducted to determine if there was a relationship between aspects of food insecurity and medication adherence. Next, multilevel modeling was conducted using event records as a statistical unit of analysis (or “level 1 unit”), nested within participants (or “level 2 unit). All of these analyses were conducted using R version 3.1.3. [30] and the library “lme4: Linear mixed-effects models using Eigen and S4” (version 1.7) [31]. Prior to testing the daily relationship between aspects of food insecurity and missed doses of medication, the impact of time was examined to determine whether there was any indication of reactivity to the daily measurement. If habituation or sensitization effects occur over the course of the study, we would expect to observe a significant upward or downward linear trend in the rates at which missed doses of medication and aspects of food insecurity occurred.
To test the daily relationships between aspects of food insecurity, alcohol use, and missed doses of medication, the data was restructured. Because the food insecurity and alcohol use questions refer to the prior days’ experiences whereas the Wisepill data is reported for the current day, the data was restructured so that all of the data for the aspects of food insecurity, alcohol use and adherence referred to the same day. Fixed and random effects were used such that the intercepts and slopes of the models were modeled first as random effects in logistic regressions. If the residual variances for the slopes are determined to not vary across level 2 units, they were converted to fixed effects [32], with the exception of time variables in order to retain the growth model component of the model and the nested nature of the data. B estimates and standard errors are reported for model estimates.
Missing data days were included in these analyses and we assume them to be missing at random (MAR). Missing data were handled using multiple imputation by chained equations using all variables in the dataset to estimate missing data using the R package “mice: Multivariate Imputation by Chained Equations” version 2.22 [33, 34]. Predictive mean matching, a semi-parametric imputation method, was used in order to preserve any non-linear relationships present in the data [33].
Results
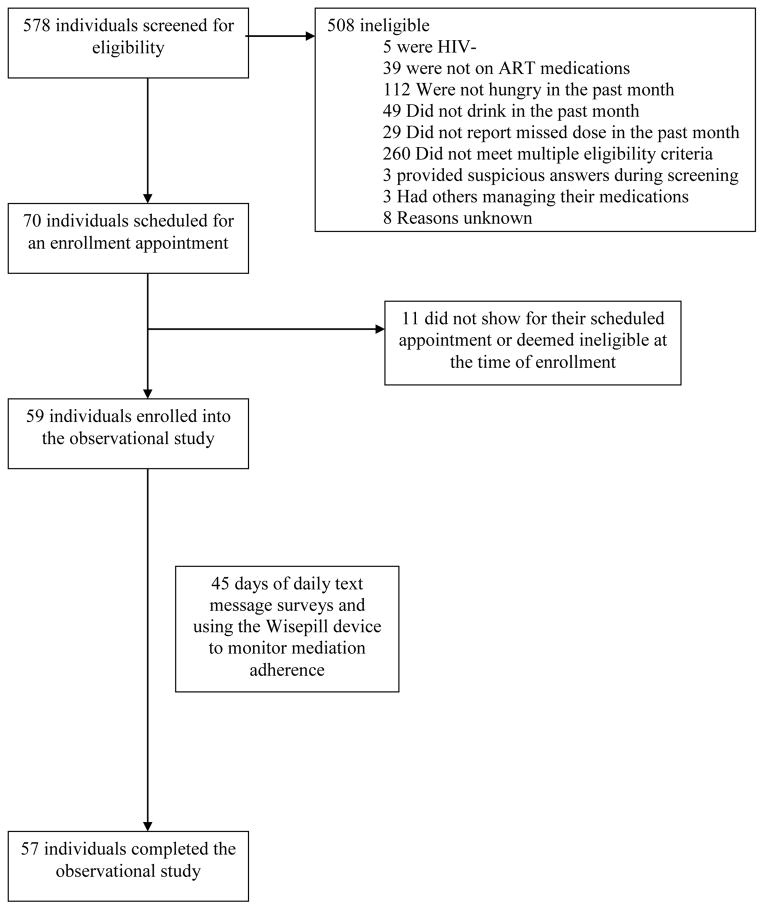
For the current study, 578 individuals were screened for eligibility and a total of 508 were deemed not eligible for the study (See Figure 1). The majority of participants (N=260) screened out because they did not meet multiple eligibility criteria. Of the three major criteria for entry into the study, 112 individuals did not report severe food insecurity in the previous month (i.e. hunger and unable to buy more food), 49 individuals did not report drinking alcohol in the past month, and 39 individuals were not currently taking antiretroviral medications at the time of screening. There were 70 individuals who met all eligibility criteria for study entry and were scheduled for an in-office enrollment appointment. Of these individuals, a total of 59 individuals attended their appointment and enrolled into the study; 57 individuals completed follow-up assessments.
Figure 1.
Screening and enrollment into the 45-day observational study
Demographic Characteristics
The majority of the 59 participants enrolled in the current study were male (N=40; 67.8%; See Table 1), identified as African American/Black (96.6%), and were middle-aged (M= 48, SD = 6.6). In terms of education, 35.6% of participants completed high school or their GED and an additional 44.1% completed some education after high school. On average, participants had an income of $1,472.66 for the 45 days. Most (76.3%) received a type of disability payment. Additionally, 61% of participants received food stamps during the course of the study. More than half (61%) of participants were on ARV regimens that required taking their prescriptions with food.
Table 1.
Demographic characteristics of participants enrolled in current study (N=59)
| N | % | |
|---|---|---|
| Gender | ||
| Male | 40 | 67.8 |
| Female | 12 | 20.3 |
| Transgender | 7 | 11.9 |
| Race/Ethnicity | ||
| White | 1 | 1.7 |
| African American/Black | 57 | 96.6 |
| Hispanic/Latino | 1 | 1.7 |
| Education | ||
| Less than High School | 12 | 20.3 |
| High school/GED | 21 | 35.6 |
| More than High School | 26 | 44.1 |
| Types of Income Received Over 45 days | ||
| Job (Part Time/Full Time) | 9 | 15.3 |
| Any Disability (Short-time/SSDI) | 45 | 76.3 |
| Unemployment | 1 | 1.7 |
| Food Stamps | 36 | 61.0 |
| Other | 5 | 8.5 |
| Medication Food Requirement | ||
| Regimen Requires Food | 36 | 61 |
| Regimen Does Not Require Food | 23 | 39 |
| Viral Loada | ||
| Detectable | 10 | 18.9 |
| Undetectable | 43 | 81.1 |
| CD4 (T-Cell) Counta | ||
| 200 or less | 6 | 11.5 |
| Greater than 200 | 46 | 88.5 |
|
| ||
| M | SD | |
|
| ||
| Income Over 45 Days | $1,472.66 | 1323.93 |
| Age Range (30–59) | 48 | 6.62 |
| Baseline Visual Analog Scale | 84.54 | 18.62 |
Note: There was missing viral load data from 6 participants and missing CD4 data from 7 participants
The sample was fairly healthy; the majority of participants had undetectable HIV RNA viral loads (81.1%). Participants also had relatively high CD4 T-cell counts, with only six having a CD4 T-cell count of 200 or less, the cut-off for an AIDS diagnosis.
Day-Level Behavior
Of the 2,655 days of collected data, there were 530 days (20.0%) where doses of medication were missed. Participants reported one or more aspects of food insecurity on 718 days (27.0%). Of these days, worrying about food running out occurred on 597 days (22.5%), eating less than needed because there wasn’t enough food occurred on 533 days (20.1%), and being hungry but not able to afford more food occurred on 298 days (11.2%). Participants reported drinking alcohol on 566 days (21.3%) with an average of 2.27 drinks (SD = 1.29) when they were drinking. The quantity of alcohol drinks was skewed (skewness = 2.7, SE = 0.050) with responses ranging from 0 to 12 drinks consumed in a day. However, given the meaningfulness of the minimum score (i.e. 0), this variable was not transformed [33].
Aspects of food insecurity and missed doses of medication occurred on at least one day for a large percentage of participants. Over the course of the study, 74.6% of participants reported at least one day of any of the three food insecurity indicators. Nearly all participants had at least one day where they missed a dose of medication (91.5%). A large proportion of participants had at least one day where they drank alcohol (83.1%). Of the 2655 days of text message surveys, 170 days were missing due to uncompleted surveys (6.4%). Additionally, 16 surveys were partially completed (0.6%).
Aspects of Food Insecurity and Medication Adherence Across the 45 Days
To replicate past findings, analyses were first conducted across the 45-day observational period using the individual as the case; medication adherence and aspects of food insecurity were collapsed across days. On average, participants were 83.2% adherent to the medication in their Wisepill device (SD =13.62; Range 50% – 100%). In a bivariate regression, all aspects of food insecurity combined predicted medication adherence such that greater food insecurity was associated with poorer medication adherence (β = −0.312, p = 0.016; Table 2). This relationship remained significant even after controlling for education and income over the 45 days (β = −0.345, p = 0.011).
Table 2.
Bivariate and multivariate regressions predicting ART medication adherence across the 45-day observational period
| Predictors | Bivariate Regression
|
Multivariate Regression
|
||||
|---|---|---|---|---|---|---|
| B | SE | Beta | B | SE | Beta | |
|
|
|
|||||
| Any Food Indicator | −4.25 | 1.714 | −0.312* | −4.698 | 1.786 | −0.345* |
| Worry | −4.211 | 1.716 | −0.309* | |||
| Ate Less | −2.573 | 1.772 | −0.189 | |||
| Hungry | −2.943 | 1.762 | −0.216^ | |||
| Income over 45 days | −1.293 | 1.841 | −0.095 | −2.178 | 1.82 | −0.16 |
| Education | 0.398 | 1.804 | 0.029 | 1.781 | 1.789 | 0.133 |
p<0.10,
p<0.05
Bivariate regressions were also conducted using each individual indicator of food insecurity. Worrying about running out of food predicted medication adherence, such that greater worry predicted lower medication adherence (β = −0.309, p = 0.017). Eating less because there was not enough food and being hungry did not predict medication adherence in individual bivariate regressions (β = −0.189, p = 0.152, β = −0.216, p = 0.100, respectively).
Aspects of Food Insecurity and Medication Adherence on a Daily Level
Test of reactivity to the daily measurement
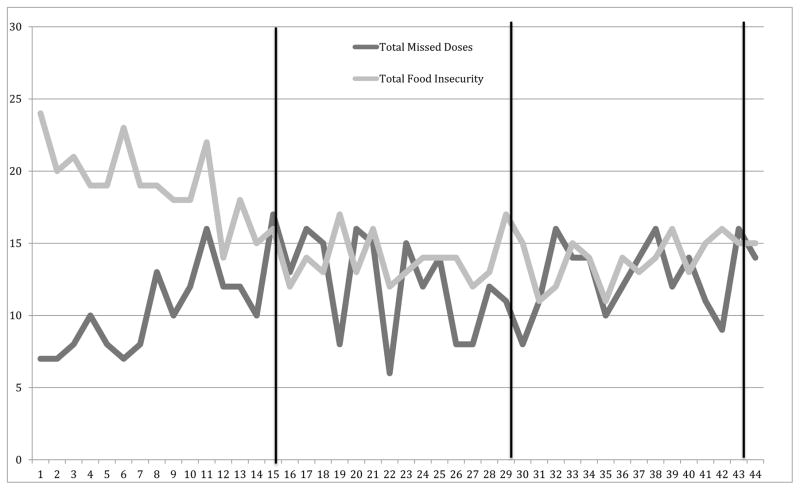
Day in the study predicted missed doses such that the longer participants were in the study, the more likely they were on a given day to miss doses of medication (B = 0.017, SE = 0.006, p = 0.008). The same model was also run with all aspects of food insecurity combined. Day in the study predicted food insecurity such that the longer participants were in the study, the less likely they were to report at least one of the aspects of food insecurity on any given day (B = −0.029, SE = 0.010, p = 0.004). This analysis was also replicated for each indicator of food insecurity; “worried about not having enough to eat” and “eating less because there was not enough food” both showed significant time trends. However, day in the study did not significantly predict the question about hunger. All subsequent analyses control for the effect of day. Figure 2 shows the time trends of missed doses of medication and food insecurity. In addition, days that participants received financial payments and income did not impact adherence.
Figure 2.
Time Trends of Daily Day with Study Payments Marked (Days 15, 29, 43)
Note: Each line represents the total number of events that occurred each day across participants
Daily relationship between aspects of food insecurity and missed medication doses
A multilevel model was constructed to test the daily relationship between the aspects of food insecurity measured in this study combined and missed doses of medication. Results showed that all the aspects of food insecurity as a composite did not predict missed doses of medication on a day-to-day basis (B = −0.053, SE = 0.236, p=0.82). After controlling for income over the 45 days and education, this relationship was still non-significant (B = −0.090, SE = 0.245, p=0.71).
Multilevel models were also conducted using each individual indicator of food insecurity. Worrying about food running out and eating less because there wasn’t enough food were not significant predictors of daily missed doses (worry: B = −0.198, SE = 0.321, p=0.54; ate less: B = 0.019, SE = 0.242, p=0.94). However, severe food insecurity as indexed by the hunger item did significantly predict daily missed doses of medication such that daily reported hunger was associated with a greater likelihood of missing medications on a daily level (B = 0.519, SE = 0.254, p=0.046; See Model 1 in Table 3). This relationship held even after controlling for income over the 45 days and education (B = 0.570, SE = 0.285, p = 0.050; See Model 2 in Table 3).
Table 3.
Fixed effects and random effects estimates for multilevel model of daily hunger predicting daily missed doses of medication with imputed data
| Model 1 | Model 2 | |||
|---|---|---|---|---|
|
| ||||
| Fixed Effects | ||||
|
| ||||
| Parameter | B | SE | B | SE |
| Intercept | −2.312*** | 0.257 | −2.442*** | 0.265 |
| Level 1 (Daily Level Data) | ||||
| Day | 0.016* | 0.006 | 0.017** | 0.007 |
| Hunger | 0.519* | 0.254 | 0.54* | 0.274 |
| Level 2 (Individual Level Data) | ||||
| Income Over 45 days | 0.138 | 0.207 | ||
| Education | −0.168 | 0.198 | ||
|
| ||||
| Random Effects | ||||
|
| ||||
| Intercept (σ^2) | 2.238 | 1.510 | 2.195 | 1.481 |
| Level 1 (Daily Level Data) | ||||
| Day | 0.0004 | 0.021 | 0.0004 | 0.020 |
| Day* Hungry | 0.0002 | 0.016 | 0.0002 | 0.015 |
p<0.05,
p<0.01,
p<0.001
Alcohol use as a moderator
Whether or not a participant was drinking on a given day was tested as a moderator of the daily relationship between hunger and missing a dose of medication (See Table 4). There were 85 days in which participants drank and were hungry and 18 participants contributed at least one of those days. Among the entire sample, drinking on a given day predicted missing a dose of medication on a daily level (B = 0.731, SE = 0.319, p = 0.022). When accounting for daily alcohol use, hunger was no longer a significant predictor of missing a dose of medication (B = 0.673, SE = 0.474, p = 0.156). There was a significant interaction between drinking and experiencing hunger (B = −1.919, SE = 0.575, p<0.001). This interaction, however, was in an unexpected direction; those who drank alcohol and experienced hunger on a given day had the lowest likelihood of missing a dose on that day. Those that did not drink alcohol but did experience hunger on a given day were the most likely to miss a dose of medication on that day. This analysis was also conducted using the alcohol measure continuously to test whether quantity of alcohol use on a given day would interact with hunger, however, this interaction was not significant (B = 0.100, SE = 0.706, p = 0.887).
Table 4.
Fixed effects and random effects estimates for multilevel model with drinking (Yes/No) as a moderator
| Fixed Effects | ||
|---|---|---|
|
| ||
| Parameter | B | SE |
| Intercept | −2.627*** | 0.288 |
| Level 1 (Daily Level Data) | ||
| Day | 0.19* | 0.008 |
| Hunger | 0.673 | 0.474 |
| Drinking (Yes/No) | 0.731* | 0.319 |
| Drinking* Hunger | −1.919*** | 0.575 |
| Day* Hunger | 0.010 | 0.016 |
| Day* Drinking | −0.003 | 0.012 |
| Level 2 (Individual Level Data) | ||
| Income Over 45 days | 0.137 | 0.197 |
| Education | −0.165 | 0.194 |
|
| ||
| Random Effects | ||
|
| ||
| Intercept (σ^2) | 2.274 | 1.508 |
| Level 1 (Daily Level Data) | ||
| Day | 0.001 | 0.025 |
| Drinking* Hunger | 0.298 | 0.546 |
p<0.05,
p<0.001
Discussion
The current study replicates findings from both resource poor and resource rich settings that demonstrate that food insecurity is related to medication adherence, even when controlling for other markers of socioeconomic status, such as income and education. Additionally, this study extends the literature by looking at this relationship on a daily level. Although worrying about not having enough to eat and eating less did not predict adherence, hunger was directly related to missing medication on a daily basis. This day-level finding supports a direct temporal relationship between food and medication adherence, such that having tangible resources impacts health behaviors [8]. This also lends credence to the potential explanations for the relationship between food insecurity and ARV adherence. Food requirements of prescriptions and avoiding side effects associated with taking medications on an empty stomach are potential explanations of the link between day level food insecurity and day level medication non-adherence. Although these explanations were not specifically tested in this study, the current findings support future research to tease apart these mechanisms.
The results of this study support the assumption that hunger and medication adherence are directly related, due to circumstances that occur at the daily level. However, worrying about having enough to eat and eating less were not associated with non-adherence on a daily basis but was associated with non-adherence across time. Less severe food insecurity may, therefore, serve as a marker for social disadvantage that predicts non-adherence in general with severe food insecurity predicting non-adherence on the same day. Additionally, worrying about having enough food to eat taps into the psychological consequences of the stress of poverty. Worrying about having enough to eat may impact medication adherence in a cumulative way rather than on a day-by-day basis. Future research should replicate these findings in other locations, including rural areas of both resource rich and resource poor countries to confirm this daily relationship.
There was potential reactivity to the daily measurement both for missed doses of medication and food insecurity defined as indicating yes to any of the three daily food insecurity questions. Participants were more likely to miss doses of medications the longer that they were in the study. A possible explanation for this finding is that using the Wisepill device may have served as a reminder for participants to take their medications at the beginning of the study, but as the study progressed, the Wisepill device became less of a reminder. Reactivity to using the Wisepill has also been found in other studies with HIV positive adults in China and Uganda [27, 28]. Future research may take these factors into account and perhaps lag the time between starting to use the Wisepill device and starting the daily food insecurity measurement to reduce the potential effect of reactivity on adherence.
There was also an interaction between hunger and drinking alcohol, but in a direction opposite of what was predicted. Those who drank alcohol and were hungry on a given day were the least likely to miss a dose of medication on that day. This interaction was not observed for quantity of alcohol use. One possible explanation for the direction of the interaction observed is that participants who were hungry but still drinking may have had less severe hunger than those that were not drinking. Differences in hunger severity may have masked the expected relationship, where greater alcohol use and food insecurity would predict non-adherence. Also possible is the role of alcohol use in coping with extreme poverty. Although maladaptive, drinking may reduce the stress of poverty, even if diverting resources away from food. Thus, stress reduction could account for the paradoxically better adherence among drinkers experiencing food insecurity. Finally, we cannot dismiss the possibility that the interaction between drinking and hunger could have been a statistical artifact in the data particularly because the interaction disappears when using the drinking variable continuously. Thus, our study should be replicated with more sensitive measurements for hunger before concluding that this counterintuitive interaction is reliable.
There were limitations to this study that should be taken into account. First, the eligibility criteria was specifically chosen so that there would be enough events of each variable of interest (i.e. aspects of food insecurity, alcohol use, and non-adherence) within the daily study, however, this may have limited the generalizability of these findings because only 10% of individuals screened were enrolled into the study. Individuals screened out may have been using alcohol and experiencing hunger but reported being adherent to their medications. It would be important to understand the facilitators for these individuals to maintain their adherence during economic hardships and while using substances, such as high resiliency, greater social support, or lower levels of depression, however, this study was limited in its design to elucidate this. Additionally, days of hunger and non-adherence may both be impacted by a third, confounding variable, such as daily housing instability. This type of severe disruption to daily life should be measured and incorporated into future daily analyses.
Another factor to take into consideration in the interpretation of these results is the skew of the quantity of alcohol consumed variable. The decision not to transform these data was due to the meaningful nature of “0” in this variable. To transform a variable a constant must be added to minimum value of the variable changing the interpretation of the results [35]. However, this has implications for the possible results of the interaction. The skew of the data may have contributed to the non-significance of this interaction. The reactivity seen in the daily data may have also contributed to the non-significance.
Another limitation of the study is that it was conducted in one large southeastern U.S. city. It is possible that the results do not generalize to other cities within the U.S. or suburban or rural areas of the U.S. or elsewhere. Additionally, almost the entire sample for this study identified as African-American (96%). There may be racial factors that play a role in the relationship between aspects of food insecurity and medication adherence such as race-based medical mistrust [36], racial prejudice/discrimination [37], and racial stigma [38, 39]. Finally, only 3 aspects of food insecurity were used to explore its daily relationship with medication non-adherence. This limited number of items was used to reduce the burden of answering these questions on a daily basis and these particular items were chosen because we felt that they would change the most over time. These items, however, do not address quality of food or the procurement of food in socially unacceptable ways. Although eliminating these aspects led to a less nuanced picture of daily food insecurity, the items that were used in the daily assessment provide range of food insecurity, albeit a smaller one than if the full assessment was used.
In order to improve medication adherence among people living with HIV, interventions on multiple levels are required. Structural changes are necessary to make food more available to those living in poverty. Subsidized grocery stores, expansion of food stamp programs, and increasing the availability of quality food in food deserts are all needed steps to increase access to food. Providers can also screen for food insecurity prior to prescribing medications that require food to collaboratively decide on appropriate regimens with their patients. Behavioral and psycho-education based interventions can address individual decision-making around medication adherence and also skills-building for how to navigate the social services system as well as how to seek out potential resources such as food pantries.
Acknowledgments
This research was supported by the National Institute of Alcohol Abuse and Alcoholism grant R01 AA021471 (PI: Seth Kalichman), and the National Institute of Mental Health grants T32 MH074387 (PI: Seth Kalichman) and T32 MH078788 (PI: Larry Brown). This manuscript contains content submitted in partial fulfillment of the requirements for the degree of Doctor of Philosophy for Jennifer Pellowski to the University of Connecticut. The authors thank Dr. Tania B. Huedo-Medina for her statistical assistance.
Footnotes
Authors’ Statement of Conflict of Interest and Adherence to Ethical Standards
Authors Pellowski, Kalichman, S. Cherry, Conway-Washington, C. Cherry, Grebler, and Krug declare that they have no conflicts of interest. All participants were treated according to the APA guidelines for treatment of human participants and with the Helsinki Declaration of 1975.
References
- 1.Centers for Disease Control and Prevention. Characteristics associated with HIV infection among heterosexuals in urban areas with high AIDS prevalence – 24 cities, United States, 2006–2007. MMWR Morb Mortal Wkly Rep. 2011;60:1045–1049. [PubMed] [Google Scholar]
- 2.Pellowski JA, Kalichman SC, Matthews KA, Adler N. A pandemic of the poor: social disadvantage and the U.S. HIV epidemic. Am Psychol. 2013;68:197–209. doi: 10.1037/a0032694. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Lynch JW, Smith GD, Kaplan GA, House JS. Income inequality and mortality: importance to health of individual income, psychosocial environment, or material conditions. BMJ. 2000;320:1200–1204. doi: 10.1136/bmj.320.7243.1200. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Reif S, Whetten K, Lowe K, Ostermann J. Association of unmet needs for support services with medication use and adherence among HIV-infected individuals in the southeastern United States. AIDS Care. 2006;18:277–283. doi: 10.1080/09540120500161868. [DOI] [PubMed] [Google Scholar]
- 5.Young AS, Sullivan G, Bogart LM, Koegel P, Kanouse DE. Needs for services reported by adults with severe mental illness and HIV. Psychiatr Serv. 2005;56:99–101. doi: 10.1176/appi.ps.56.1.99. [DOI] [PubMed] [Google Scholar]
- 6.Johnson BT, Redding CA, DiClemente RJ, et al. A network-individual-resource model for HIV prevention. AIDS Behav. 2010;14:204–221. doi: 10.1007/s10461-010-9803-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Hobfoll SE. Conservation of resources: a new attempt at conceptualizing stress. Am Psychol. 1989;44:513–524. doi: 10.1037//0003-066x.44.3.513. [DOI] [PubMed] [Google Scholar]
- 8.Weiser SD, Hatcher A, Frongillo EA, et al. Food insecurity is associated with greater acute care utilization among HIV-infected homeless and marginally housed individuals in San Francisco. J Gen Intern Med. 2013;28:91–98. doi: 10.1007/s11606-012-2176-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Anabwani G, Navario P. Nutrition and HIV/AIDS in sub-Saharan Africa: An overview. Nutrition. 2005;21:96–99. doi: 10.1016/j.nut.2004.09.013. [DOI] [PubMed] [Google Scholar]
- 10.Anema A, Vogenthaler N, Frongillo EA, Kadiyala S, Weiser SD. Food insecurity and HIV/AIDS: current knowledge gaps, and research priorities. Curr HIV/AIDS Rep. 2009;6:224–231. doi: 10.1007/s11904-009-0030-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Singer AW, Weiser SD, McCoy SI. Does food insecurity undermine adherence to antiretroviral therapy? A systematic review. AIDS Behav. 2015;19:1510–1526. doi: 10.1007/s10461-014-0873-1. [DOI] [PubMed] [Google Scholar]
- 12.Weiser SD, Yuan C, Guzman D, et al. Food insecurity and HIV clinical outcomes in a longitudinal study of urban homeless and marginally housed HIV-infected individuals. AIDS. 2013;27:2953–2958. doi: 10.1097/01.aids.0000432538.70088.a3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Kalichman SC, Washington C, Grebler T, et al. Medication adherence and health outcomes of people living with HIV who are food insecure and prescribed antiretrovirals that should be taken with food. Infect Dis Ther. 2015;4:79–91. doi: 10.1007/s40121-015-0057-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Young S, Wheeler AC, McCoy SI, Weiser SD. A review of the role of food insecurity in adherence to care and treatment among adult and pediatric populations living with HIV and AIDS. AIDS Behav. 2014;18(Suppl 5):S505–515. doi: 10.1007/s10461-013-0547-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Kalichman SC, Grebler T, Amaral CM, et al. Food insecurity and antiretroviral adherence among HIV positive adults who drink alcohol. J Behav Med. 2014;37:1009–1018. doi: 10.1007/s10865-013-9536-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Morojele NK, Kekwaletswe CT, Nkosi S. Associations between alcohol use, other psychosocial factors, structural factors and antiretroviral therapy (ART) adherence among South African ART recipients. AIDS Behav. 2014;18:519–524. doi: 10.1007/s10461-013-0583-0. [DOI] [PubMed] [Google Scholar]
- 17.Cantrell RA, Sinkala M, Megazinni K, et al. A pilot study of food supplementation to improve adherence to antiretroviral therapy among food insecure adults in Lusaka, Zambia. J Acquir Immune Defic Syndr. 2008;49(2):190–5. doi: 10.1097/QAI.0b013e31818455d2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Tirivayi N, Koethe JR, Groot W. Clinic-based food assistance is associated with increased medication adherence among HIV-infected adults on long-term antiretroviral therapy in Zambia. J AIDS Clin Res. 2012;3:171. doi: 10.4172/2155-6113.1000171. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.de Pee S, Grede N, Mehra D, Bloem MW. The enabling effect of food assistance in improving adherence and/or treatment completion for antiretroviral therapy and tuberculosis treatment: a literature review. AIDS Behav. 2014;18(Suppl 5):S531–41. doi: 10.1007/s10461-014-0730-2. [DOI] [PubMed] [Google Scholar]
- 20.Georgia Department of Public Health. HIV/AIDS Surveillance. Georgia: 2012. [Accessibility verified August 17, 2015]. Available at: https://dph.georgia.gov/data-fact-sheet-summaries. [Google Scholar]
- 21.Centers for Disease Control and Prevention. [Accessibility verified August 17, 2015];Diagnoses of HIV infection in the United States and dependent areas. 2013 Available at: http://www.cdc.gov/hiv/library/reports/surveillance/2013/surveillance_Report_vol_25.html.
- 22.Affleck G, Zautra A, Tennen H, Armeli S. Multilevel daily process designs for consulting and clinical psychology: a preface for the perplexed. J Consult Clin Psychol. 1999;67:746–754. doi: 10.1037//0022-006x.67.5.746. [DOI] [PubMed] [Google Scholar]
- 23.Barta WD, Portnoy DB, Kiene SM, Tennen H, Abu-Hasaballah K, Ferrer R. A daily process investigation of alcohol-involved sexual risk behavior among economically disadvantaged problem drinkers living with HIV/AIDS. AIDS Behav. 2008;12:729–740. doi: 10.1007/s10461-007-9342-4. [DOI] [PubMed] [Google Scholar]
- 24.Parsons JT, Rosof E, Mustanski B. The temporal relationship between alcohol consumption and HIV-medication adherence: a multilevel model of direct and moderating effects. Health Psychol. 2008;27:628–637. doi: 10.1037/a0012664. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Tennen H, Affleck G, Armeli S, Carney MA. A daily process approach to coping: linking theory, research, and practice. Am Psychol. 2000;55:626–636. doi: 10.1037//0003-066x.55.6.626. [DOI] [PubMed] [Google Scholar]
- 26.Bickel D, Nord M, Price C, Hamilton W, Cook J. [Accessibility verified March 25, 2016];United States Department of Agriculture (USDA) Guide to measuring household food security. Available at: http://www.fns.usda.gov/sites/default/files/FSGuide_0.pdf.
- 27.Bachman DeSilva M, Gifford AL, Keyi X, et al. Feasibility and acceptability of a real-time adherence device among HIV-positive IDU patients in China. AIDS Res Treat. 2013:957862. doi: 10.1155/2013/957862. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Haberer JE, Kahane J, Kigozi I, et al. Real-time adherence monitoring for HIV antiretroviral therapy. AIDS Behav. 2010;14:1340–1346. doi: 10.1007/s10461-010-9799-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Pellowski JA, Kalichman SC, White D, Amaral CM, Hoyt G, Kalichman MO. Real-time medication adherence monitoring intervention: test of concept in people living with HIV infection. J Assoc Nurses AIDS Care. 2014;25:646–651. doi: 10.1016/j.jana.2014.06.002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.R Core Team. R: A language and environment for statistical computing. R Foundation for Statistical Computing; Vienna, Austria: [Accessibility verified August 17, 2015]. Available at: http://www.r-project.org. [Google Scholar]
- 31.Bates D, Maechler M, Bolker B, et al. [Accessibility verified August 17, 2015];Package ‘lme4: Linear mixed-effects models using Eigen and S4’. available through the Comprehensive R Archive Network. http://cran.r-project.org/web/packages/lme4/index.html.
- 32.Snijders T, Bosker R. Multilevel analysis: An introduction to basic and advanced multilevel modeling. London, England: Sage; 1999. [Google Scholar]
- 33.van Buuren S, Groothuis-Oudshoorn K. mice: Multivariate Imputation by Chained Equations in R. J Stat Softw. 2011;45:1–67. [Google Scholar]
- 34.van Buuren S, Groothuis-Oudshoorn K. [Accessibility verified August 17, 2015];mice: Multivariate Imputation by Chained Equations. available through the Comprehensive R Archive Network. http://cran.r-project.org/web/packages/mice/index.html.
- 35.Osborne J. Notes on the use of data transformations. Practical Assessment, Research, & Evaluation. 2002;8(6):1. Retrieved from http://PAREonline.net/getvn.asp?v=8&n=6. [Google Scholar]
- 36.Eaton LA, Driffin DD, Kegler C, et al. The role of stigma and medical mistrust in the routine health care engagement of black men who have sex with men. Am J Public Health. 2015;105:e75–e82. doi: 10.2105/AJPH.2014.302322. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Bogart LM, Wagner GJ, Galvan FH, Klein DJ. Longitudinal relationships between antiretroviral treatment adherence and discrimination due to HIV-serostatus, race, and sexual orientation among African-American men with HIV. Ann Behav Med. 2010;40:184–190. doi: 10.1007/s12160-010-9200-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Earnshaw VA, Bogart LM, Dovidio JF, Williams DR. Stigma and racial/ethnic HIV disparities: moving toward resilience. Am Psychol. 2013;68:225–236. doi: 10.1037/a0032705. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Earnshaw VA, Smith LR, Chaudoir SR, Amico KR, Copenhaver MM. HIV stigma mechanisms and well-being among PLWH: a test of the HIV stigma framework. AIDS Behav. 2013;17:1785–1795. doi: 10.1007/s10461-013-0437-9. [DOI] [PMC free article] [PubMed] [Google Scholar]