Abstract
Fractures of the second cervical vertebra (C2, axis) are common in adult spine surgery. Those fractures occurring in younger adult patients are often associated with high-energy mechanism trauma, resulting in a “Hangman’s Fracture.” Management of these fractures is often successful with nonoperative means, though surgery may be needed in those fractures with greater displacement and injury to the C2-C3 disc. Older patients are more likely to sustain fractures of the odontoid process. The evidence supporting surgical management of these fractures is evolving, as there may be a mortality benefit to surgery. Regardless of treatment, longer-term mortality rates are high in this patient population, which should be discussed with the patient and family at the time of injury. Pediatric patients may suffer fractures of the axis, though differentiation of normal and pathologic findings is necessary and more difficult with the skeletally immature spine.
Keywords: Fracture, C2, Axis, Odontoid, Hangman’s, Spondylolisthesis
Introduction
Fractures of the second cervical vertebra (C2, axis) comprise approximately one-third of cervical spine fractures [1]. The mechanisms for these fractures may occur from high-energy mechanisms in younger patients, but can commonly occur with low-energy trauma in the geriatric population. The anatomy of the second cervical vertebra varies greatly from subaxial levels, with the odontoid process and an elongated pars interarticularis between the atlantoaxial joint and the C2-C3 joint. Treatment of C2 fractures varies according to fracture morphology and patient demographics. Here, we offer an introduction to the evaluation and management of fractures of the axis.
Pediatric fractures of the atlas
High cervical injuries are uncommon in the pediatric population and are commonly associated with high-energy mechanisms, such as motor vehicle accidents and pedestrians struck by automobiles [2–4]. Fractures of C2 are more likely to happen in younger children (age <8). Historically, neurological deficits were reportedly uncommon, although one study reported a 66 % prevalence of neurological deficits with pediatric cervical injuries [3]. As these injuries are uncommon, missed injuries and misdiagnoses are not uncommon. Identification of cervical injuries in children is essential, as misdiagnosis has been associated with high rates of neurological deficits at the time the correct diagnosis is made [5]. Young (age <8) children may be the population most susceptible to incorrect diagnoses, as a result of the immature spine and difficulty with examination, and the upper cervical spine is the most common region for incorrect diagnoses. These facts emphasize the need for an organized method for evaluation of the upper cervical spine in the pediatric population. While several studies have attempted to provide a “perfect” decision algorithm, the consensus seems to be that application of the National Emergency X-Radiography Utilization Study (NEXUS) to children older than 9 years old is appropriate, while any concerning sign or symptom in a younger child should elicit a radiographic evaluation of the cervical spine [4, 6].
Skeletally immature children are at risk of misdiagnosis because of incomplete fusion of their ossifying C2 vertebra [7]. Development of C2 involves ossification of four separate ossification centers consisting of the vertebral body, the odontoid, and right and left facet/pars/lamina. The odontoid process fuses to the vertebral body between 3 and 6 years of age. A secondary ossification center develops at the apex of the odontoid process, fusing by 12 years of age. The facet/pars/lamina centers fuse to the vertebral body also between the ages of three and six. These separate centers may not be completely fused until young adolescence, and as a result, normal areas of incomplete fusion may be mistaken for fractures. In addition, variance in the process of ossification can lead to areas susceptible to fracture as well.
Fractures of the odontoid may occur through the odontoid-body synchondrosis. These fractures often heal when treated with halo or Minerva immobilization as the synchondrosis is well vascularlized [8]. In some cases, the fragment may retract, forming an os odontoideum. This radiographic finding may be a normal anatomical variant as well, so care to distinguish the two is essential. Magnetic resonance imaging may be useful for this purpose. Older pediatric patients are more likely to sustain a traumatic spondylolisthesis, similar to adults. The majority of these cases are treated with rigid halo or Minerva immobilization. C1-C2 arthrodesis is indicated in cases of neglected odontoid process fractures that have gone on to develop an os odontoideum with C1-C2 instability.
Odontoid fractures
Classification
The Anderson and D’Alonso system is commonly used in classification of odontoid fractures [9]. Type I fractures involve avulsion of the tip of the odontoid by the alar ligament. These are generally treated effectively in a hard cervical collar, as they are stable injuries. Type II fractures (Fig. 1) occur at the base of the odontoid process, at the odontoid-body junction. These are common fractures in the geriatric population, and significant debate exists regarding appropriate management of this injury as many will go on to a nonunion. Type III fractures extend into the body of C2 and have good healing potential. Computed tomography scanning is essential to characterize C2 fractures, as inter-rater reliability is variable, and this may affect management options [10].
Fig. 1.
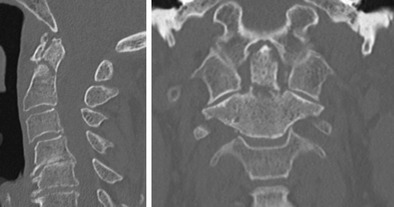
Type II odontoid fracture in a 74-year-old woman after a fall from standing
Geriatric injuries
The incidence of odontoid fractures is increasing, with a 135 % increase from 2000 to 2011 in the Medicare population [11••]. This increase may be due to a combination of an increasingly active older population and improved diagnostic accuracy with modern imaging techniques [12]. The rate of surgical management of C2 fractures in the elderly seems to be relatively constant, near 15 % [11••]. The appropriate management of odontoid fractures in this population remains a matter of debate, as the immediate risks of surgery are weighed against the long-term risks of odontoid nonunion.
Chapman et al. reviewed 322 patients with type II odontoid fractures [13•]. The average age of patients in this study was 81.8 (range 65–101.5). Fourteen percent of patients expired within 30 days of their fracture diagnosis, and 44 % had died at an average of 2-year follow-up. Nonoperative management was associated with a higher 30-day mortality risk (hazard ratio = 3) when adjusting for age, gender, and comorbid conditions. This association was lost when looking at longer-term follow-up, however, underscoring the poor prognosis for patients sustaining these fracture and emphasizing the need for appropriate discussion with the patient and family. The AOSpine North America multi-centre prospective geriatric odontoid fracture study (GOF) followed 159 patients 65 years of age or older with type II odontoid fractures [14••]. The majority of patients enrolled in the study were treated with surgery (63.5 % surgery and 36.5 % nonoperative). Approximately half (54.1 %) of the enrolled patients were considered to have failed treatment, which was defined by death, decline of Neck Disability Index (NDI) by more than 9.5 points, or any major complication attributed to the treatment. Analysis of their results found increasing age, nonoperative treatment (OR = 3.09), male gender (OR = 4.33), and neurological comorbidity (OR = 4.13) to be associated with treatment failures. This study, however, was not a randomized trial, and superiority cannot be claimed for surgical intervention. These findings support the conclusion that surgical treatment of a type II odontoid fracture should be considered if the patient is physically fit for surgery. This is supported by Pearson, who found lower mortality in the surgical group both at 30 days (8.3 versus 16.2 %) and at 1 year after surgery (21.7 versus 32.3 %) [11••].
Nonoperative management
Nonoperative management of type II odontoid fractures may be with a soft cervical collar for comfort or immobilization with a hard cervical collar or a halo-vest. Halo-vest orthoses are associated with high rates of complications, and the risk of mortality in the geriatric population is elevated [15–17]. Complications associated with halo-vest treatment are often mild and most frequently pin-site infections. In most cases, these infections can be treated with local wound care and antibiotics [15]. In some rare cases, surgical debridement of the infection site may be needed. Nonunions persist in the halo-vest, and this is a cause for delayed surgical intervention. Nonunion rates may be as high as 50 %, which may be considered a high failure rate when the risks of halo-vest immobilization are considered [18]. The most concerning risk is mortality associated with the halo-vest, which may be as high as 20 % in the geriatric population [17]. In younger patients, halo-vest orthoses are considered to be safer [16]. In the geriatric population, halo-vest immobilization is frequently associated with high mortality rates. Pneumonia, cardiac arrest, and respiratory arrest have been associated with mortality in geriatric patients treated with halo-vests, and this method of nonoperative treatment has been termed “a last resort.” [17] Hard cervical collar may be a more appropriate treatment option, as lower rates of respiratory complications have been reported [19]. Polin et al. and Patel et al. have reviewed their single-center experiences comparing halo-vest with rigid cervical collar for immobilization of both type II and III odontoid fractures [18, 20]. Halo-vest was not found superior to hard cervical collar immobilization for these fracture types, leading them to recommend hard collars, which do not carry the risks associated with halo-vests. These results are supported by the GOF study, where nonunions were more common following halo-vest treatment than hard collar treatment. Patel et al. and others have noted that a solid union is not necessary to achieve good outcomes with type II odontoid fractures and that a fibrous nonunion can offer good outcomes [20, 21]. Nonunions are a concern with nonoperative management of type II odontoid fractures, however, as pain and instability can lead to delayed surgical management [22••]. Instability at C1-C2 is an uncommon cause of myelopathy, but it remains a cited reason for recommending surgery. Myelopathy due to an odontoid nonunion is rare and frequently presents as a result of a chronic nonunion [23, 24]. It may be associated with gross instability or with a hypertrophic nonunion causing central stenosis. Patients with a hypertrophic nonunion frequently exhibit C2 radiculopathy as well, and this may serve as an early warning for a developing myelopathy secondary to the nonunion [25]. As with other causes of cervical myelopathy, prompt management upon diagnosis can yield meaningful improvements in neurological function [25].
Delayed surgery for odontoid fractures treated nonoperatively has been reported at rates as high as 20–30 % [22••]. Smith et al. reported a 22 % nonunion rate in the GOF study, with over half (63 %) of these nonunions requiring surgery. In addition to the confirmed nonunions requiring surgery, this cohort found that a radiographic union did not preclude delayed surgical intervention. Ten percent of patients underwent surgery for “delayed fracture displacement.” In combination with primary nonunions, 22 % of patients treated nonoperatively in the GOF study underwent delayed surgical intervention. This delay in “definitive” treatment did not adversely affect patient-reported outcomes measured by the Neck Disability Index (NDI) and short form-36 instruments. All patients suffered declines in HRQOL from their pre-injury state, regardless of union status, emphasizing the need for informed patient counseling at the time of the injury.
Techniques for operative management
Anterior odontoid screws are used in the management of geriatric odontoid fractures [26, 27]. Nonunion rates are higher in older patients (greater than 65 years of age) [27]. This may be due to factors such as poor bone stock, which prevents appropriate lag screw technique in the odontoid process. Placement of the odontoid screw requires access to the C2-C3 disc level. In older patients, this is associated with a higher risk of postoperative dysphagia, which may require gastrostomy tube placement.
Posterior instrumentation and fusion is more commonly performed for the management of these fractures [13•, 28]. Modern instrumentation makes the Harms-Goel a commonly accepted fixation strategy, with C1 lateral mass screws and C2 pars/pedicle screws. Wright has described the C2 intralaminar screw as another fixation option for C2, providing adequate biomechanical stability [29, 30]. Intralaminar screws may also help limit distal dissection and are useful when vertebral artery anatomy precludes pedicle or pars fixation (Fig. 2). Transarticular screws may be used when the vertebral artery anatomy allows and may be useful when subaxial surgery is performed as well (Fig. 3). Atlantoaxial fusion has been reported to have high union rates in this patient population.
Fig. 2.
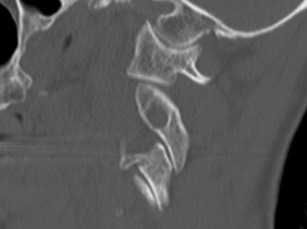
Foramen transversarium residing within the pars interarticularis, precluding safe pedicle or pars screw fixation
Fig. 3.

Transarticular screws fixing a type II odontoid fracture in a patient with falls due to subaxial spondylotic myelopathy. Surgery consisted of C1-C2 transarticular screws with posterior element wiring (using the C3 lamina) and C4, C5, and C6 laminoplasty
There may be a benefit to mortality with operative intervention. This finding is not consistent, however, and should be interpreted with caution. The retrospective GOF study found a benefit, as did an analysis of Medicare beneficiaries [11••, 13•]. These findings have been inconsistent across smaller, single-center studies. Schoenfeld et al. reported high overall mortality rates regardless of intervention, but did suggest there is a mortality benefit for patients aged 65 to 74 years old [31]. Similarly, Woods et al. found a lower 30-day mortality rate in patient treated with surgery [32•]. This benefit was not observed at 1 and 5 years after the injury, further reinforcing the overall poor prognosis for patients sustaining type II odontoid fractures.
While there may be benefit to long-term mortality, there are likely higher complication rates with surgical management in the near term [19]. Tracheostomy (25 %) and feeding tube placement (19 %) were the two most common complications associated with surgery, which may carry their own morbidity in an older patient population. Surgery has also been associated with longer hospital stays, increased ventilator requirements, and higher rates of venous thromboembolic events [33].
Spondylolisthesis of the axis
Commonly referred to as “Hangman’s fracture,” traumatic spondylolisthesis of the axis is more common in younger patients and often associated with higher-energy mechanisms of injury [1]. These fractures are often classified by the system proposed by Effendi and modified by Levine and Edwards [34, 35]. Type I fractures are the result of axial loading and hyperextension, with minimally displaced (<3 mm) fractures through both pars interarticularis and a competent C2-C3 disc. Type II fractures are the result of hyperextension, with rebound flexion causing displacement of the fractures, disruption of the C2-C3 disc, and flexion of the vertebral body fragment. Type IIa fractures (Fig. 4) are distinct as they are associated with severe flexion of the body fragment, with minimal displacement of the fractures. A variant of type I and type II fractures, termed “atypical Hangman’s,” exist, which carry a higher risk of neurological deficit for type II fractures [36]. These atypical fractures are characterized by an oblique fracture through one pars, leaving the contralateral pars intact with a posterior vertebral body fragment (Fig. 5). Ventral displacement of the odontoid results in spinal canal stenosis from the residual body and the ventral C1 ring. Type III fractures are the result of flexion/rebound extension with unilateral or bilateral facet joint dislocations and are the least common injury type [37] (Fig. 6). Knowledge of this classification system is essential to management of these fractures, as the fracture type will often dictate management and understanding the mechanism of injury will assist with reduction of the C2 injury.
Fig. 4.
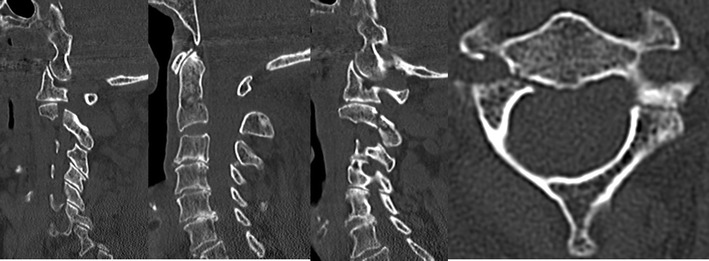
Effendi-Levine type 2a spondylolisthesis of the axis. Notice the angulation of the odontoid fragment with the relative absence of translation
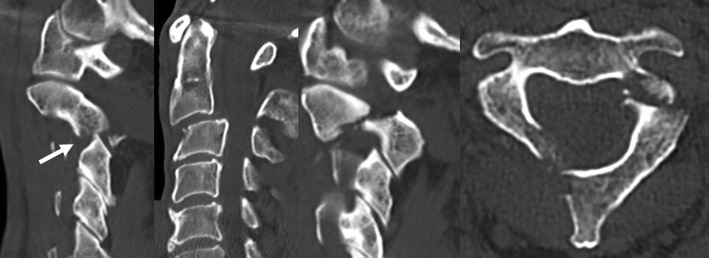
Fig. 5.
“Atypical” Hangman’s fracture with an oblique fracture line leaving a portion of the posterior vertebral body wall (arrow) attached to the dorsal fragment
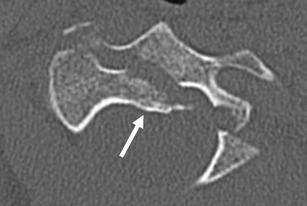
Fig. 6.
Effendi-Levine type 3 spondylolisthesis with dislocation of the right C2-C3 joint (arrow). Notice the large pedicle on the left, without fracture involvement of the foramen transversarium
Type I fractures
These injuries, characterized by minimally displaced fractures with a competent C2-C3 disc, are often effectively treated with a halo-vest orthosis or a hard cervical collar, with reported union rates approaching 100 % [38–40]. This is not unexpected, given the stability of the fracture in concert with a large surface area of apposed cancellous bone at the fracture site. There remains debate regarding the most appropriate immobilization technique, hard collar versus halo. Coric et al. presented a consecutive series of 64 patients, all treated with Philadelphia collars and all achieving union [38]. While halo-vests are generally safe, they are associated with minor complications such as pin-site infections and avoidance of a halo may be best when possible. Surgical treatment of type I injuries has been reported, with lag screw fixation; though given the effectiveness of nonoperative treatment, one must consider the costs and risks of surgery for these injury types.
Type II fractures
These injuries are characterized by displacement of the fracture site as well as angulation of the C2-body fragment. The C2-C3 disc is incompetent, and the anterior longitudinal ligament is disrupted. Nonoperative and operative treatments have been recommended for these injuries. Proponents of surgical treatment note the instability of the fracture fragments, as the disc and all are disrupted. As surgical management of a subaxial fracture would often be recommended in such a situation, so should the rule be at C2-C3 [41]. However, nonoperative management with rigid external immobilization with a halo has been described in numerous series. Vaccaro et al. described early halo immobilization after a brief period of traction (average 2 days) with Gardner-Wells tongs [42]. Seventy-eight percent (21/27) of these patients went on to union, without displacement of the fracture fragment. Those that displaced the fracture were treated with a second episode of traction, followed by rigid immobilization. Greater degree of fracture angulation (>11.5°) at presentation was associated with a higher risk of fracture displacement. Successful healing of this fracture may result in ossification through the C2-C3 disc, rather than through the fracture fragments. Surgical management often consists of C2-C3 arthrodesis, either through an anterior approach (C2-C3 anterior cervical discectomy and fusion (ACDF)) or posterior approach. In the rare instance of a traumatic disc herniation at C2-C3 with the spondylolisthesis, an anterior approach would be preferred, as this offers direct access to ventral canal for decompression. Anterior and posterior fixation techniques are, in general, similarly stable [43, 44]. In cases with severe comminution or a vertebral artery course that preclude safe C2 instrumentation, then a posterior technique will require fusion of more than one cervical segment. Temporary immobilization with a C1-C3 construct, followed by removal of the C1 implants after C2-C3 arthrodesis, has been described as a method to encourage motion preservation [45]. Lag screw fixation through the fracture fragments has also been described for type II injuries. This technique neglects the C2-C3 discoligamentous injury, however, and significant displacement through the C2-C3 disc may preclude lag screw management [46]. Muller et al. emphasized the importance of the C2-C3 disc integrity, noting that nonoperative management was most likely to fail in these patients, with nearly half of those patients undergoing a delayed surgery [37].
Type IIa
Type IIa fractures are a result of a flexion-distraction mechanism. As a result, there is flexion of the odontoid fragment without translation. This results in gapping at the fracture site and widening of the posterior aspect of the disc space. Identification of these fractures is necessary, as reduction of the fracture requires extension without traction. Traction may cause further displacement of the fracture fragments (Fig. 7). As with type II fractures, these have been treated successfully with rigid halo immobilization. However, surgical treatment through an anterior or posterior approach is reasonable as these fractures may displace within the halo and the C2-C3 disc is disrupted. As noted by Vaccaro, fracture angulation more than 11.5° was associated with redisplacement within the halo, and surgical treatment of those injuries with greater angulation should be considered [42, 47].
Fig. 7.

Traction applied to the patient in Fig. 4. Notice the worsening of fracture displacement. The patient was reduced and immobilized for surgery using a Mayfield positioner
Type III
These injuries, characterized by a C2-C3 facet subluxation/dislocation, are often treated with an open posterior surgery. As with posterior surgeries for type II injuries, the fracture or vertebral artery course may preclude safe C2 screw placement. In these cases, C1-C3 arthrodesis or C1-C3 stabilization followed by implant removal at C1-C2 may be performed. A posterior approach is required to reduce the C2-C3 facet injury (Fig. 8). As the anterior fragment is not attached to the posterior fragment, ACDF will not allow for reduction of the facet joints. Similar to type II fractures, nonoperative management can still be successful [47]. Initial fracture displacement and angulation are associated with treatment failure and delayed surgery. An informed discussion with the patient is necessary to determine optimum treatment, understanding the risks and benefits of operative and nonoperative interventions.
Fig. 8.

Postoperative radiographs of Fig. 6. A C2 lag screw was placed on the left to fix the fracture and the segment, sparing a fusion level
C2 vertebral body fractures
Fractures of the vertebral body of C2 are uncommon, though a number of case series have been presented. These fractures are generally stable and successfully treated with nonoperative management and external immobilization. Though rarely reported, burst fractures of C2 may be an exception, and posterior cervical fusion has been reported. Application of the concepts of the load-sharing classification may help guide indications for surgery in C2 burst fractures, with fracture comminution and kyphosis driving the decision to operate [48]. One must be aware of the possibility of vertebral artery injury in these fractures. Comminution of the vertebral body and involvement of the foramen transversarium have been associated with vertebral artery injuries [49, 50•]. Thus, some form of angiography may be indicated in C2 body fractures with gross comminution or fracture fragments within the foramen transversarium.
Conclusion
Fractures of the atlas are common, with traumatic spondylolisthesis (Hangman’s fracture) occurring in younger patients while fractures of the odontoid process are more common in elderly patients. Children are at risk as well, with children younger than 8 more likely to sustain a C2 fracture than a subaxial fracture. Knowledge of normal, developing anatomy is necessary to minimize the rate of misdiagnosis and missed diagnosis in pediatric patients. Delayed diagnosis has been associated with neurological deficits. Traumatic spondylolisthesis is often successfully managed with external immobilization, in the form of a hard cervical collar or a halo-vest orthosis. Greater amounts of displacement and fracture angulation are associated with failure of nonoperative management, and surgery, anterior or posterior, should be considered for type II, IIa, and III fractures.
Odontoid fractures pose an interesting and important fracture subtype, as their incidence is increasing with the aging population. While there is no level I data to support surgery in geriatric fractures, there is evidence supporting early surgical intervention for patients that are deemed surgical candidates. Regardless of initial management, mortality rates at 1 year and beyond are high and similar for geriatric patients sustaining odontoid fractures. A careful history and physical examination in combination with a discussion with patient and family will help guide decision making for these fractures.
Treatment of fractures of the atlas requires an understanding of anatomy and fracture mechanisms. This will aid in classification of fracture types, which may aid in decision making with respect to surgery. Attention to possible concomitant subaxial injuries and injuries to the vertebral arteries must be paid. Good outcomes can be expected for most fractures of the atlas, provided that the risk factors for failure of nonoperative management are identified and surgical intervention is used judiciously.
Compliance with ethical standards
Conflict of interest
Megan E. Gornet declares that she has no conflict of interest.
Michael P. Kelly reports grants paid directly to his institution from the Cervical Spine Research Society, AO Spine, Barnes Jewish Foundation, Fox Family Foundation, Orthopedic Research Education Foundation, Cerapedics, and PCORI, outside the submitted work.
Human and animal rights and informed consent
This article does not contain any studies with human or animal subjects performed by any of the authors.
Footnotes
This article is part of the Topical Collection on Cervical Injuries and Treatment
References
Papers of particular interest, published recently, have been highlighted as: • Of importance •• Of major importance
- 1.Ryan MD, Henderson JJ. The epidemiology of fractures and fracture-dislocations of the cervical spine. Injury. 1992;23:38–40. [DOI] [PubMed]
- 2.Lui TN, Lee ST, Wong CW, et al. C1-C2 fracture-dislocations in children and adolescents. J Trauma. 1996;40:408–11. [DOI] [PubMed]
- 3.Platzer P, Jaindl M, Thalhammer G, et al. Cervical spine injuries in pediatric patients. J Trauma. 2007;62:389–96. discussion 94-6. [DOI] [PubMed]
- 4.Viccellio P, Simon H, Pressman BD, et al. A prospective multicenter study of cervical spine injury in children. Pediatrics. 2001;108, E20. [DOI] [PubMed]
- 5.Avellino AM, Mann FA, Grady MS, et al. The misdiagnosis of acute cervical spine injuries and fractures in infants and children: the 12-year experience of a level I pediatric and adult trauma center. Childs Nerv Syst. 2005;21:122–7. [DOI] [PubMed]
- 6.Pieretti-Vanmarcke R, Velmahos GC, Nance ML, et al. Clinical clearance of the cervical spine in blunt trauma patients younger than 3 years: a multi-center study of the American Association for the Surgery of Trauma. J Trauma. 2009;67:543–9. discussion 9-50. [DOI] [PubMed]
- 7.Lustrin ES, Karakas SP, Ortiz AO, et al. Pediatric cervical spine: normal anatomy, variants, and trauma. Radiographics. 2003;23:539–60. [DOI] [PubMed]
- 8.Sherk HH, Nicholson JT, Chung SM. Fractures of the odontoid process in young children. J Bone Joint Surg Am. 1978;60:921–4. [PubMed]
- 9.Anderson LD, D’Alonzo RT. Fractures of the odontoid process of the axis. J Bone Joint Surg Am. 1974;56:1663–74. [PubMed]
- 10.Barker L, Anderson J, Chesnut R, Nesbit G, Tjauw T, Hart R. Reliability and reproducibility of dens fracture classification with use of plain radiography and reformatted computer-aided tomography. J Bone Joint Surg Am. 2006;88:106–12. [DOI] [PubMed]
- 11.••.Pearson AM, Martin BI, Lindsey M, Mirza SK. C2 vertebral fractures in the medicare population: incidence, outcomes, and costs. J Bone Joint Surg Am. 2016;98:449–56. C2 Fracture incidence is rising, though rate of surgery remains steady. There may be a mortality benefit to surgery in the Medicare population. [DOI] [PubMed]
- 12.Smith HE, Kerr SM, Fehlings MG, et al. Trends in epidemiology and management of type II odontoid fractures: 20-year experience at a model system spine injury tertiary referral center. J Spinal Disord Tech. 2010;23:501–5. [DOI] [PubMed]
- 13.•.Chapman J, Smith JS, Kopjar B, et al. The AOSpine North America Geriatric Odontoid Fracture Mortality Study: a retrospective review of mortality outcomes for operative versus nonoperative treatment of 322 patients with long-term follow-up. Spine (Phila Pa 1976). 2013;38:1098–104. A retrospective cohort study examining mortality after geriatric odontoid fractures. At maximum follow-up, there is some evidence to support a mortality benefit to surgery over nonoperative treatment. [DOI] [PMC free article] [PubMed]
- 14.••.Fehlings MG, Arun R, Vaccaro AR, Arnold PM, Chapman JR, Kopjar B. Predictors of treatment outcomes in geriatric patients with odontoid fractures: AOSpine North America multi-centre prospective GOF study. Spine (Phila Pa 1976). 2013;38:881–6. A prospective study of geriatric odontoid fractures found improved patient reported outcomes for younger patients and those treated with surgery at their initial hospitalization. [DOI] [PMC free article] [PubMed]
- 15.Bransford RJ, Stevens DW, Uyeji S, Bellabarba C, Chapman JR. Halo vest treatment of cervical spine injuries: a success and survivorship analysis. Spine (Phila Pa 1976). 2009;34:1561–6. [DOI] [PubMed]
- 16.Longo UG, Denaro L, Campi S, Maffulli N, Denaro V. Upper cervical spine injuries: indications and limits of the conservative management in Halo vest. A systematic review of efficacy and safety. Injury. 2010;41:1127–35. [DOI] [PubMed]
- 17.Majercik S, Tashjian RZ, Biffl WL, Harrington DT, Cioffi WG. Halo vest immobilization in the elderly: a death sentence? J Trauma. 2005;59:350–6. discussion 6-8. [DOI] [PubMed]
- 18.Polin RS, Szabo T, Bogaev CA, Replogle RE, Jane JA. Nonoperative management of Types II and III odontoid fractures: the Philadelphia collar versus the halo vest. Neurosurgery. 1996;38:450–6. discussion 6-7. [DOI] [PubMed]
- 19.Smith HE, Kerr SM, Maltenfort M, et al. Early complications of surgical versus conservative treatment of isolated type II odontoid fractures in octogenarians: a retrospective cohort study. J Spinal Disord Tech. 2008;21:535–9. [DOI] [PubMed]
- 20.Patel A, Zakaria R, Al-Mahfoudh R, et al. Conservative management of type II and III odontoid fractures in the elderly at a regional spine centre: a prospective and retrospective cohort study. Br J Neurosurg. 2015;29:249–53. [DOI] [PubMed]
- 21.Koech F, Ackland HM, Varma DK, Williamson OD, Malham GM. Nonoperative management of type II odontoid fractures in the elderly. Spine (Phila Pa 1976). 2008;33:2881–6. [DOI] [PubMed]
- 22.••.Smith JS, Kepler CK, Kopjar B, et al. Effect of type II odontoid fracture nonunion on outcome among elderly patients treated without surgery: based on the AOSpine North America geriatric odontoid fracture study. Spine (Phila Pa 1976). 2013;38:2240–6. Odontoid nonunions may be treated effectively, without an adverse effect on patient reported outcomes. However, the majority of patients sustaining a nonunion underwent delayed surgery. [DOI] [PubMed]
- 23.Bachs A, Barraquer-Bordas L, Barraquer-Ferre L, Canadell JM, Modolell A. Delayed myelopathy following atlanto-axial dislocation by separated odontoid process. Brain. 1955;78:537–53. [DOI] [PubMed]
- 24.Kirankumar MV, Behari S, Salunke P, Banerji D, Chhabra DK, Jain VK. Surgical management of remote, isolated type II odontoid fractures with atlantoaxial dislocation causing cervical compressive myelopathy. Neurosurgery. 2005;56:1004–12. discussion -12. [PubMed]
- 25.Shamji MF, Alotaibi N, Ghare A, Fehlings MG. Chronic hypertrophic nonunion of the Type II odontoid fracture causing cervical myelopathy: case report and review of literature. Surg Neurol Int. 2016;7:S53–6. [DOI] [PMC free article] [PubMed]
- 26.Apfelbaum RI, Lonser RR, Veres R, Casey A. Direct anterior screw fixation for recent and remote odontoid fractures. J Neurosurg. 2000;93:227–36. [DOI] [PubMed]
- 27.Platzer P, Thalhammer G, Ostermann R, Wieland T, Vecsei V, Gaebler C. Anterior screw fixation of odontoid fractures comparing younger and elderly patients. Spine (Phila Pa 1976). 2007;32:1714–20. [DOI] [PubMed]
- 28.Joaquim AF, Patel AA. Surgical treatment of Type II odontoid fractures: anterior odontoid screw fixation or posterior cervical instrumented fusion? Neurosurg Focus. 2015;38, E11. [DOI] [PubMed]
- 29.Wright NM. Translaminar rigid screw fixation of the axis. Technical note. J Neurosurg Spine. 2005;3:409–14. [DOI] [PubMed]
- 30.Claybrooks R, Kayanja M, Milks R, Benzel E. Atlantoaxial fusion: a biomechanical analysis of two C1-C2 fusion techniques. Spine J. 2007;7:682–8. [DOI] [PubMed]
- 31.Schoenfeld AJ, Bono CM, Reichmann WM, et al. Type II odontoid fractures of the cervical spine: do treatment type and medical comorbidities affect mortality in elderly patients? Spine (Phila Pa 1976). 2011;36:879–85. [DOI] [PMC free article] [PubMed]
- 32.•.Woods BI, Hohl JB, Braly B, Donaldson 3rd W, Kang J, Lee JY. Mortality in elderly patients following operative and nonoperative management of odontoid fractures. J Spinal Disord Tech. 2014;27:321–6. Geriatric patients sustaining an odontoid fracture have 1- and 5-year mortality, regardless of surgical or nonoperative management. [DOI] [PubMed]
- 33.Fagin AM, Cipolle MD, Barraco RD, et al. Odontoid fractures in the elderly: should we operate? J Trauma. 2010;68:583–6. [DOI] [PubMed]
- 34.Effendi B, Roy D, Cornish B, Dussault RG, Laurin CA. Fractures of the ring of the axis. A classification based on the analysis of 131 cases. J Bone Joint Surg (Br). 1981;63-B:319–27. [DOI] [PubMed]
- 35.Levine AM, Edwards CC. The management of traumatic spondylolisthesis of the axis. J Bone Joint Surg Am. 1985;67:217–26. [PubMed]
- 36.Starr JK, Eismont FJ. Atypical Hangman’s fractures. Spine (Phila Pa 1976). 1993;18:1954–7. [DOI] [PubMed]
- 37.Muller EJ, Wick M, Muhr G. Traumatic spondylolisthesis of the axis: treatment rationale based on the stability of the different fracture types. Eur Spine J. 2000;9:123–8. [DOI] [PMC free article] [PubMed]
- 38.Coric D, Wilson JA, Kelly Jr DL. Treatment of traumatic spondylolisthesis of the axis with nonrigid immobilization: a review of 64 cases. J Neurosurg. 1996;85:550–4. [DOI] [PubMed]
- 39.Govender S, Charles RW. Traumatic spondylolisthesis of the axis. Injury. 1987;18:333–5. [DOI] [PubMed]
- 40.Grady MS, Howard MA, Jane JA, Persing JA. Use of the Philadelphia collar as an alternative to the halo vest in patients with C-2, C-3 fractures. Neurosurgery. 1986;18:151–6. [DOI] [PubMed]
- 41.Suchomel P, Hradil J, Barsa P, et al. [Surgical treatment of fracture of the ring of axis—“hangman’s fracture”]. Acta Chir Orthop Traumatol Cech. 2006;73:321–8. [PubMed]
- 42.Vaccaro AR, Madigan L, Bauerle WB, Blescia A, Cotler JM. Early halo immobilization of displaced traumatic spondylolisthesis of the axis. Spine (Phila Pa 1976). 2002;27:2229–33. [DOI] [PubMed]
- 43.Chittiboina P, Wylen E, Ogden A, Mukherjee DP, Vannemreddy P, Nanda A. Traumatic spondylolisthesis of the axis: a biomechanical comparison of clinically relevant anterior and posterior fusion techniques. J Neurosurg Spine. 2009;11:379–87. [DOI] [PubMed]
- 44.Duggal N, Chamberlain RH, Perez-Garza LE, Espinoza-Larios A, Sonntag VK, Crawford NR. Hangman’s fracture: a biomechanical comparison of stabilization techniques. Spine (Phila Pa 1976). 2007;32:182–7. [DOI] [PubMed]
- 45.Schleicher P, Scholz M, Pingel A, Kandziora F. Traumatic spondylolisthesis of the axis vertebra in adults. Global Spine J. 2015;5:346–58. [DOI] [PMC free article] [PubMed]
- 46.Buchholz AL, Morgan SL, Robinson LC, Frankel BM. Minimally invasive percutaneous screw fixation of traumatic spondylolisthesis of the axis. J Neurosurg Spine. 2015;22:459–65. [DOI] [PubMed]
- 47.Ryken TC, Hadley MN, Aarabi B, et al. Management of isolated fractures of the axis in adults. Neurosurgery. 2013;72 Suppl 2:132–50. [DOI] [PubMed]
- 48.McCormack T, Karaikovic E, Gaines RW. The load sharing classification of spine fractures. Spine (Phila Pa 1976). 1994;19:1741–4. [DOI] [PubMed]
- 49.Ding T, Maltenfort M, Yang H, et al. Correlation of C2 fractures and vertebral artery injury. Spine (Phila Pa 1976). 2010;35:E520–4. [DOI] [PubMed]
- 50.•.Durand D, Wu X, Kalra VB, Abbed KM, Malhotra A. Predictors of vertebral artery injury in isolated C2 fractures based on fracture morphology using CT angiography. Spine (Phila Pa 1976). 2015;40:E713–8. Fracture communition and involvement of the foramen transversarium are associated with vertebral artery injuries at the level of C2. Angiography may be indicated in patients with these fracture findings on plain computed tomography. [DOI] [PubMed]


