Abstract
Work-related musculoskeletal injuries and disorders (WMSD) are a significant issue in the health care sector. Allied Health professionals (AHP) in this sector are exposed to physical and psychosocial factors associated with increased risk of developing a WMSD. Clarification of relevant hazard and risk factors for AHP is needed to improve understanding and inform WMSD risk management. A systematic analysis of the literature was undertaken to determine prevalence and risk factors for WMSD in AHP. Databases of Ovid MEDLINE, CINAHL (EBSCO), EMBASE and the Cochrane Database of Systematic Reviews were reviewed. This quality of articles was low. Outcome measures were varied, with prevalence rates of WMSD reported from 28% to 96% over a one-year time period. The lower back was the most commonly affected body part. Relevant factors identified with the development of WMSD included inexperience in the role and area of employment. Future research needs to focus on undertaking high quality prospective studies to determine the factors associated with WMSD development in AHP.
Keywords: allied health, risk factors, work-related musculoskeletal disorders
1. Introduction
Work-related musculoskeletal injuries and disorders (WMSDs) are a significant issue in the health care sector [1]. Within this sector, allied health professionals (AHPs) are important providers of services for individuals who are sick or injured, or have a disability. AHPs comprise occupational groups that have similar job roles, levels of job satisfaction, and issues concerning work life balance and staff retention [2], [3], [4], [5], [6], [7], [8]. The allied health professions include those of physiotherapists, occupational therapists, speech pathologists, prosthetists and orthotists, dieticians, sonographers, social workers, osteopaths, audiologists, radiologists, exercise physiologists, perfusionists, and, under some definitions, chiropractors [9]. AHPs undertake a variety of work activities and are exposed to a range of hazards and risks associated with a higher chance of WMSD development [10], [11]. Despite the large body of evidence that supports the role of physical and psychosocial factors in the development of WMSDs [12], the literature on allied health has largely focused on the former [13], [14], [15], [16], [17], [18]. To date, a comprehensive examination of the literature relating to this professional group has not been undertaken in relation to WMSDs, a gap this review aims to address. The health care literature provides a useful lens to examine the relationship between work environment and development of WMSDs in AHPs.
A substantial overlap exists between a range of work activities undertaken by health care workers, such as nurses and AHPs. Both roles involve physically demanding work and exposure to a range of psychosocial hazards [10], [11], [19], [20] such as high workloads, time pressure, or limited job control. However, strategies designed to prevent WMSDs in the health care sector have largely focused on minimizing physical hazards and risks, such as lifting or transferring of patients [19], [21]. This mismatch between potential WMSD causal factors and risk management strategies may, in part, explain the high numbers of WMSDs reported in the health care sector, despite extensive efforts to reduce their prevalence.
The multifactorial nature of WMSD development requires identification of a range of causal factors relevant to the population group, in this instance AHPs. This information can then be used to guide the development of effective strategies to reduce hazards and risks for WMSD. The current focus on physical aspects of work necessarily limits the development of a multifactorial prevention approach. In the first instance, improved understanding of what are the key issues is needed to inform prevention strategies.
An additional factor, not restricted to the health care sector, is the over-reliance on compensation data to inform risk management strategies [22]. In health care, previous research [11], [23], [24] has reported that health care workers are reluctant to report injuries, and as such compensation data are likely to under-represent actual injury rates. Furthermore, the complex and cumulative nature of WMSD development means that attribution of causation is challenging, and compensation data do not capture this information accurately [22].
To improve the understanding of key issues for AHPs in relation to the development of WMSDs, a systematic review of the available literature is needed. This systematic review has two aims: first, to determine the prevalence of WMSDs, and second, to identify hazard and risk factors associated with the development of WMSDs.
2. Materials and methods
2.1. Quality assessment
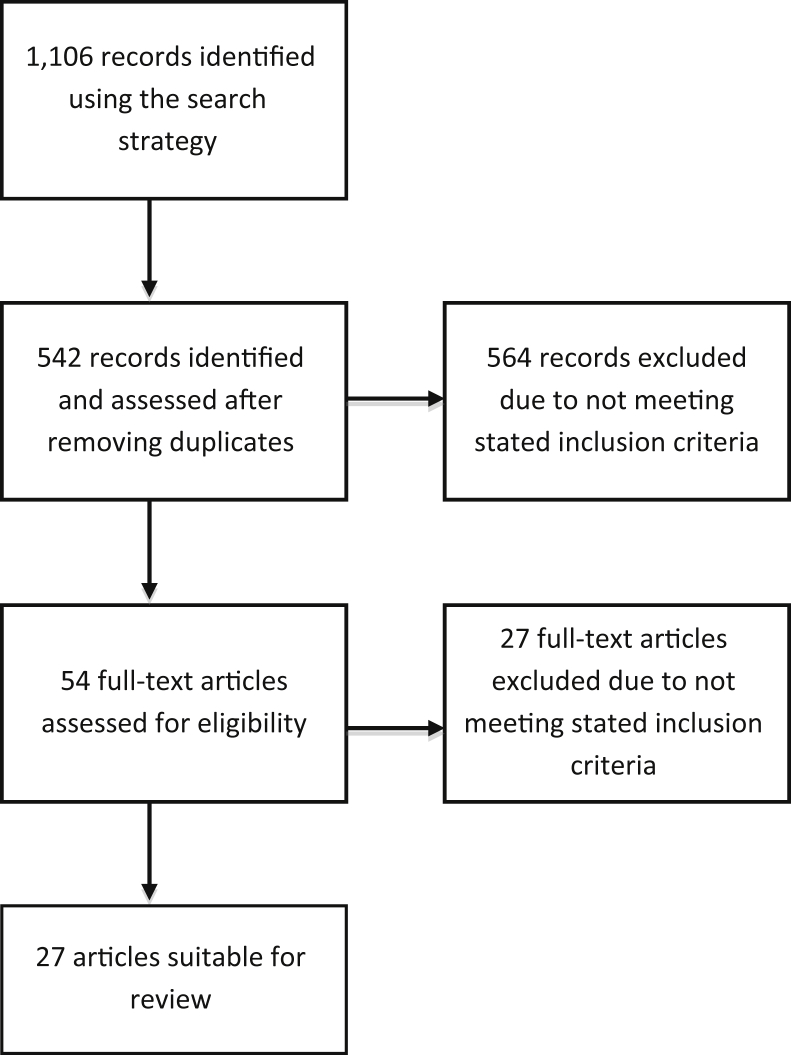
The Preferred Reporting Items for Systematic reviews and Meta-Analyses (PRISMA) checklist and diagram (see Fig. 1) were used to conduct the systematic review to ensure complete, transparent, and unbiased reporting. Quality assessments were undertaken using one of the following tools, depending on the study design: the Critical Review Form for Quantitative Studies [25], the Critical Review Form for Qualitative Studies [26] from McMaster University, and, for systematic reviews, the Critical Appraisal Skills Programme [27]. These quality checklists were used to assess the risk of bias, research design, and rigor of the included studies.
Fig. 1.
Flow chart.
2.2. Data extraction
One reviewer (S.A.) assessed the title and abstract of each study to determine if it met the inclusion criteria. All excluded abstracts were then assessed by a second reviewer to ensure no accidental exclusion of relevant articles. Full papers were then reviewed and those that did not satisfy the inclusion criteria were excluded (Fig. 1).
The following characteristics of included studies were extracted and described: study design, occupation, location, sample detail, outcome measure, prevalence measure, risk factors identified, body area affected, and the consequence of injury for the individual.
2.3. Search strategy
Following the PRISMA guidelines, a search protocol was developed, identifying analysis and inclusion/exclusion criteria. A search of the literature was conducted in March 2016, using Ovid MEDLINE (1948–March 2016), CINAHL (EBSCO) (1937–March 2016), EMBASE (Ovid) (1947–March 2016), and the Cochrane Database of Systematic Reviews (1991–March 2016). Databases were searched from inception to March 2016, for articles in English language. Reference lists from identified papers were hand searched to ensure that all relevant papers were identified.
A search using Medical Subject Headings (MeSH) terms (exploded) and free text words was performed, including appropriate acronyms and synonyms, relevant truncations, and wildcard symbols, to ensure that all spellings and variations of root words were taken into account. The search terms used are listed in Table 1. Allied health titles were selected using definitions from the AHP Australia [9] (Table 1).
Table 1.
Key search terms and search strategy
| Subject heading | (1) Exp. occupational health (2) Exp. occupational disease (3) Exp. occupational accident |
| Keywords | (4) Workplace or occupational injur* or occupational disease* or occupational health |
| Combine | (5) 1 or 2 or 3 or 4 |
| Subject heading | (6) Exp. musculoskeletal disease (7) Exp. musculoskeletal injury |
| Keywords | (8) Musculoskeletal disease* or musculoskeletal disorder* or musculoskeletal injur* or MSI or MSD |
| Combine | (9) 6 or 7 or 8 |
| Subject heading | (10) Exp. paramedical profession (11) Exp. physiotherapy (12) Exp. occupational therapy |
| Keywords | (13) “Allied health” or physiotherap* “physical therap*” or “occupational therap*” or podiatr* or “speech patholog*” or osteopath* or audiolog* or chiropractor* or dietic* or psychologist or “exercise physiology*” or prosthet* or orthot* or perfusionist* or “social worker*” or songograph* or “genetic counselor*” or “music therapist*” |
| Combine | (14) 10 or 11 or 12 or 13 |
| Limit | (15) English language |
| Combine | (16) 5 and 9 and 14 and 15 |
Exp, exploded; MSD, musculoskeletal disorder; MSI, musculoskeletal injury.
* Truncation that allows a literature search to include multiple forms of a word including singular, plural and variable spellings.
2.4. Inclusion criteria
For inclusion in the current review, studies required a focus on AHPs, to have reported WMSD prevalence rates or measured hazard and risk factors related to the development of WMSDs across all body sites. Only articles from peer-reviewed journals were included. Letters to the editor, guidelines, case reports, and editorials were excluded. Study designs included experimental, observational, and qualitative studies and systematic reviews. Gray literature was examined to inform the research but excluded from the systematic review.
Four articles were excluded from the current review, as they focused on specific joints such as the hand or upper limb and did not meet the inclusion criteria of WMSDs across all body sites [28], [29], [30], [31].
3. Results
Twenty-seven articles (Table 2) met the inclusion criteria for the current study: 22 retrospective observational cross-sectional design articles, one prospective cohort studies with 1-year follow up, two reviews, and two qualitative articles. No relevant randomized control trials or meta-analysis papers were identified.
Table 2.
Study characteristics
| Authors | Study design | Occupation | Place of study | Sample details | Outcome measure |
|---|---|---|---|---|---|
| Adegoke et al 2008 [32] | ORCSD | PT | Nigeria | n = 126, F = 46, M = 80 | Survey based on Cromie et al [33] and West and Gardner [34] |
| Alnaser 2007 [35] | Systematic review | OT | NA | ||
| Alrowayeh et al 2010 [36] | ORCSD | PT | State of Kuwait | n = 212, F = 99, M = 113 | Self-designed three-part survey; Part 3 based on Kuorinka et al [37] |
| Bork et al 1996 [13] | ORCSD | PT | USA | n = 928, F = 483, M = 445 | Self-designed survey aspects based on Kuorinka et al [37] |
| Campo et al 2008 [38] | Observational prospective cohort 1 y follow-up | PT | USA | n = 881, F = 627, M = 254 | Self-designed survey based on Blair [63] and Kuorinka et al [37] |
| Campo et al 2009 [14] | ORCSD | OT | USA | n = 881, F = 627, M = 254 | Self-designed survey based on Blair [63] and Kuorinka et al [37] |
| Cromie et al 2000 [33] | ORCSD | OT | Australia | n = 536, F = 418, M = 118 | Self-designed survey WMSD aspect based on Kuorinka et al [37] |
| Cromie et al 2002 [39] | In-depth interviews | OT | Australia | n = 18, F = 15, M = 8 | |
| Darragh et al 2009 [40] | ORCSD | OT & PT | Australia |
n = 1,158, F = 997, M = 161 OT477 PT = 681 |
Self-reported injuries based on Holder and Clark [64], Campo et al [38] used to identify WMSD |
| Dyrkacz et al 2012 [41] | ORCSD | OT | Canada | n = 600, F = 571, M = 29 | Self-designed |
| Glover et al 2005 [42] | ORCSD | OT | UK | n = 2,688, F = 2,150, M = 538 | Based on Cromie et al [33], West and Gardner [34], and Kuorinka et al [37] |
| Grooten et al 2011 [43] | ORCSD | PT | Sweden | n = 133, all females | |
| Hill et al 2009 [44] | ORCSD | Sonographers | USA | n = 26, all females | Self-designed, four parts: (1) demographics; (2) based on Kuorinka et al [37]; (3) work habits; (4) job demand |
| Islam et al 2015 [45] | ORCSD | OT & PT | Bangladesh | n = 101, F = 47, M = 53 | Self-designed, two parts: (1) sociodemographic details & (2) discomfort survey by Workplace Safety and Prevention Services |
| Kumar et al 2004 [46] | ORCSD | X-ray technologist | Italy | n = 20, F = 18, M = 2 | Self-designed based on Kumar (unpublished survey) |
| Lorusso et al 2007 [47] | ORCSD | X-ray technologist | Italy | n = 203, F = 45, M = 158 | Self-designed based on Kumar (unpublished survey), Kuorinka et al [37], and the Karasek [65] model of demand/control |
| Losa et al 2010 [48] | ORCSD | Podiatrists | Spain | n = 421, F = 274, M = 147 | Self-designed, three parts:(1) based on Kuorinka et al [37]; (2) sociodemographic variables; (3) pain on the Borg CR-10 scale |
| Nordin et al 2011 [49] | ORCSD | PT | Malaysia | n = 81, F = 63, M = 18 | Based on Kuorinka et al [37] |
| Passier and McPhail 2011 [50] | ORCSD | OT | Australia |
n = 46 All female |
Based on Cromie, Robertson [33] |
| Passier and McPhail 2011 [51] | Quality survey & focus groups | OT & PT | Australia |
n = 112, F = 94, M = 18 OT = 46, PT = 66 |
Self-designed |
| Rozenfeld et al 2010 [16] | ORCSD | PT | Israel | n = 112, F = 82, M = 41 | Based on Cromie et al [33] |
| Rugelj 2003 [52] | ORCSD | PT | Republic of Slovenia | n = 133, F = 127, M = 6 | Self-designed |
| Salik and Ozcan 2004 [53] | ORCSD | PT | Turkey | n = 120, F = 92, M = 28 | Based on Cromie et al [33] |
| Sharan and Ajeesh 2012 [17] | Systematic review | PT | |||
| Sin Ho et al 2013 [54] | ORCSD | PT | Korea | n = 157, F = 74, M = 83 | Based on Adegoke et al [32] |
| Vieira et al 2016 [18] | ORCSD | PT | USA | n = 121, F = 82, M = 39 | Based on Cromie et al [33] |
| West and Gardner 2001 [34] | ORCSD | PT | Australia | n = 217, F = 178, M = 39 | Self-designed |
F, female; M, male; ORCSD, observational retrospective cross sectional design; OT, occupational therapy; PT, physiotherapy; WMSD, work-related musculoskeletal injury and disorder.
Two reviews [17], [35] were examined using the Critical Appraisal Skills Programme tool [27], were found to lack rigor in research design, and did not report conclusive findings. Both reviews lacked a clear methodology and did not have well-documented search protocol or assessment of risk of bias. As such, evidence from these reviews was not included in the current review.
The majority of articles using cross-sectional surveys, appraised using the critical appraisal tool for quantitative research [25], were of high quality and addressed the issues of bias within the papers. However, as these papers were observational and retrospective, a risk of selection and recall bias [55] is possible within the research process.
A number of studies [16], [33], [34], [42], [50] examined both career and 1-year prevalence to address the risk of recall bias (Table 3). The similarity in the findings between the two prevalence measures and associated likelihood of recall bias is discussed further within the findings. Inclusion of whole cohort groups within all these studies goes some way to addressing the issues of bias in the selection of participants.
Table 3.
Prevalence rates and reported area of injury
| Authors | Career prevalence (%) | 1 y prevalence (%) | Area of body affected (%) |
||
|---|---|---|---|---|---|
| Back | Arms | Legs | |||
| Adegoke et al 2008 [32] | 91.3 | Lower back 69.8% Neck 31.1% Upper back 14.3% |
Shoulder 22.2% Forearm 5.6% Wrist & hand 20.6% Thumb 11.1%, |
Hip & thigh 6.3% Knee 15.9% Ankle & foot 9.5% |
|
| Alrowayeh et al 2010 [36] | 47.6 | Lower back 32% Neck 21% Upper back 19% |
Shoulder 13% Elbow 4%, Hand & wrist 11% |
Hip & thigh 3% Knee 11% Ankle & foot 6% |
|
| Bork et al 1996 [13] | 61 | Lower back 45% Upper back 28.7% Neck 24.7%. |
Wrist & hand 29.6% | ||
| Campo et al 2008 [38] | 28 | Lower back 6.6% Neck 4.9% Upper back 2.4% |
Shoulder 3.2% Elbow 1.4% Hand & wrist 5.3% |
Hip & thigh 2.3% Knee 2.1% Ankle & foot 2.2% |
|
| Campo et al 2009 [14] | 33 | Lower back 15.7% Neck 10.2% Upper back 7.1% |
Shoulder 7.3% Wrist & hand 13% Elbow 3.7% |
Knee 4.3% Hip & thigh 3.1% Ankle 2.8% |
|
| Cromie et al 2000 [33] | 91 | 82.8 | Lower back 62.5% Neck 47.6% Upper back 41% |
Shoulder 22.9% Elbow 13.2% Wrist & hand 21.8% Thumb 33.6% |
Hip 7.3% Knee 11.2% Ankle 7.1% |
| Dyrkacz et al 2012 [41] | 55.7 | Neck, spine, & torso 41.8% Head & face 6.7% |
Upper extremities 33.4% | Lower extremities 18.1% | |
| Glover et al 2005 [42] | 68 | 58 | |||
| Grooten et al 2011 [43] | 53.5 | Lower back 56.5% Neck 39.6% |
Shoulder 43.4% Wrist & hand 58.5% |
||
| Hill et al 2009 [44] | 96 | Lower back 69% Neck 50% Upper back 15% |
Shoulder 73% Elbow 27% Wrist & hand 54% |
Knee 23% Hip 19% Ankle & foot 8% |
|
| Islam et al 2015 [45] | 95 | Neck 65% Upper back 70% Lower back 83% |
Shoulder 54% Elbow 18% Forearm 23% Wrist/hand 62% |
Hip 20% Thigh 22% Knee 47% Lower leg 45% Ankles/Feet 42% |
|
| Lorusso et al 2007 [47] | 67 | Lower back 59.6% Shoulder 21.2% Neck 19.7% |
|||
| Losa et al 2010 [48] | 56.53 | Lower back 21.38% Upper back 13.06% Neck 13.54% |
Shoulder 0.95% Wrist/hand 1.19% |
Knee 3.09% Ankle/foot 3.33% |
|
| Nordin et al 2011 [49] | 71.6 | Lower back 51.7% Neck 46.5% Thoracic 44.8% |
|||
| Passier and McPhail 2011 [50] | 80.4 | 63 | Lower back 50% Neck 33% Shoulder 17% |
||
| Rozenfeld et al 2010 [16] | 80 | 83 | Lower back 59.8% Neck 45.5% Upper back 41.1% |
Wrist 35.7% | |
| Rugelj 2003 [52] | 47.4 | Lower back examined specifically, 73.7% lifetime prevalence | |||
| Salik and Ozcan 2004 [53] | 85 | Lower back 26% Neck 12% |
Wrist & hand 18% Shoulder 14% |
||
| Sin Ho et al 2013 [54] | 92.4 | Lower back 53.5% | Shoulder 45.2% | ||
| Vieira et al 2016 [18] | 96 | Neck 61% Upper back 35% Lower back 66% |
Shoulder 42% Elbow 15% Wrist/hand/finger 36% |
Hip/thigh pain 23% Knee 36% Ankle/foot 25% |
|
| West and Gardner 2001 [34] | 40 | 55 | Lower back 35% Neck 24% |
Hand 25% | |
Cohorts within this review were state, region, and country based, and were most commonly restricted to the registered professional groups, for example, the Australian Physiotherapy Association [33]. These observational cohort studies scored poorly in the area of research rigor, primarily due to nonreporting of statistical significance. However, the outcome measure of prevalence rates is not impacted by statistical significance. All studies were observational, and as such evaluation of interventions was not relevant. Two qualitative articles were appraised for the review; one article used one-on-one interviews [39] and the other an open-ended survey with follow-up focus groups [51]. Both articles were assessed using the critical tool for qualitative research [26]; no significant methodological flaws were identified in the studies. Conclusions drawn from the findings of these two studies were limited due to the small sample sizes.
Sample sizes ranged from 18 [39] to 2,688 [42] (Table 2). Sixteen professions [9] were included in the initial literature search; however, only five professional groups were represented in the articles reviewed for this study. The breakdown of professional groups included was as follows: physiotherapists—18, occupational therapists—five, podiatrist—one, sonographer–one, and X-ray technologists—two. Research was conducted in a variety of geographical locations including Australia [33], [34], [39], [40], [50], [51], the United Kingdom [42], the United States of America [13], [14], [18], [38], [44], Nigeria [32], the State of Kuwait [36], Malaysia [49], Sweden [43], Korea [54], Turkey [53], the Republic of Slovenia [52], Israel [16], Italy [46], [47], Canada [41], Spain [48], and Bangladesh [45]. Gender differences within study populations reflected the professional group work populations of those specific countries. Four studies, undertaken in Nigeria, the State of Kuwait, Korea, and Bangladesh, had a higher ratio of males to females in their sample populations [32], [36], [45], [54]; this reflects the underlying gender distribution of the target populations of those countries. For example, in Australia, females outnumber males in professions, such as physiotherapy (77% females vs. 33% males [56]), while in Nigeria, male physiotherapists outnumber females (37.7% females vs. 62.3% males [32].
3.1. Outcome measures
Studies in this review that employed a cross-sectional research design reported the use of a survey tool. However, clear description of survey content and the outcome measures used were not consistently reported across the studies in this review (Table 2). The standardized Nordic questionnaire was the most commonly used measure to identify body location and frequency of musculoskeletal symptoms [37]. Variation in survey content and limited detail on question content make comparisons of outcomes difficult between the included cross-sectional studies.
Six studies [16], [18], [32], [42], [50], [53] included in this review utilized a survey tool developed by Cromie et al [33]. The Cromie et al [33] survey tool consists of two parts, the first developed by the authors and the second part is the standardized Nordic questionnaire [37]. Each of the six studies reported making modifications to the survey. However, reporting of the changes was not clear; thus, a comparison of results between the five studies is difficult.
3.2. Prevalence
Prevalence of WMSDs was reported using a range of different time periods. The two most common time periods were “career prevalence,” defined as the number of WMSDs reported over the duration of a person's career and a “1-year prevalence,” defined as the number of WMSDs that have occurred in the previous 12 months. Glover [57] suggests that 1-year prevalence may provide a more accurate representation of prevalence as recall bias of participants is reduced. One study [58] reported 4-week prevalence and was excluded from the current review as it did not meet the inclusion criteria.
Comparison of injury prevalence rates between professional groups was examined in two studies [40], [45]. Darragh and colleagues [40] reported a small difference in WMSD injuries between occupational therapists and physiotherapists (45% and 47%, respectively), while Islam et al [45] reported higher rates of 92% and 97%, respectively. The small difference between the professional groups remains consistent across both studies. Darragh et al [40] propose that the variation between the rates arises from organizational differences rather than from the particular characteristics of specific jobs.
3.2.1. Career prevalence
Career prevalence was reported in 10 studies [16], [33], [34], [41], [42], [47], [49], [50], [51], [52] (Table 3). Reported career prevalence ranged from 40% [34] to 91% [33]. Outcome measures used in these studies varied. Six of the studies [16], [33], [42], [49], [50] used the Nordic questionnaire [37] to collect data on WMSDs, while West and Gardner [34], Rugelj [52], and Dyrkacz et al [41] used self-designed tools. The studies that used self-designed tools recorded the three lowest WMSD career prevalence rates of 47.4% [52], 40% [34], and 55.7% [41], while the tools based on the Nordic questionnaire recorded prevalence rates ranging from 63% [50] to 91% [33]. No obvious correlations could be detected between increased WMSD prevalence and location, gender, or environmental factors [16], [33], [34], [41], [42].
3.2.2. One-year prevalence
Seventeen studies reported 1-year prevalence (see Table 3); variance in the results using this outcome measure was higher than in studies that used career prevalence as a measure. One-year prevalence is defined by Adegoke et al [32] as a WMSD that resulted in “…discomfort, injuries or pain due to their work and lasting more than 3 days in the last 12 months in any part of the body.” One-year prevalence was reported to be between 28% [38] and 96% [18], [44]. All studies, with the exception of those of Rugelj [52], Dyrkacz et al [41], West and Gardner [34], and Islam et al [45], based some or all of their survey tools on the Nordic WMSD survey [37].
Career prevalence rates for WMSDs were higher than 1-year prevalence rates in all studies that included both measures [16], [33], [34], [42], [50]. Four studies [16], [33], [42], [50] used survey tools based on the works of Cromie and colleagues [15] and the Nordic WMSD survey tool [37], while West and Gardner [34] and used a self-designed survey. West and Gardner [34] report a 15% decrease between 1-year and career prevalence. Similar differences between the two measures were reported in other studies [33], [34], [50]. These other studies are in the opposite direction to that of West and Gardner [34], with career prevalence being higher than 1-year prevalence. Cromie et al [33] report a 1-year WMSD prevalence of 82.8% and a career WMSD prevalence of 91%, Glover et al [42] report a 10% increase from 1-year WMSD prevalence of 58% to career WMSD prevalence of 68%. Rozenfeld et al [16] report the smallest change from 80% to 83% between 1-year and career WMSD prevalence, while Passier and McPhail [50] report the largest difference of WMSD prevalence from 63% (1-year prevalence) to 80.4% (career prevalence). These relatively low differences may indicate under-reporting of WMSD career prevalence rates or that those with injuries and disorders are leaving the profession.
3.3. Area of injury
Reporting of WMSDs in specific body parts was undertaken in two ways: as a percentage of either the whole sample or those who had reported experiencing a WMSD (Table 3). For example, Adegoke et al [32] report a prevalence of lower back injuries of 69.8% in 126 participants, while Campo et al [38] reported that, of the 28% of people who reported a WMSD, 6.6% reported lower back as the affected area. Across all studies, the low back area was the most commonly reported area of injury. Nineteen studies (Table 4) reported lower back injury prevalence ranging from 6.6% to 83% [13], [14], [16], [18], [32], [33], [34], [36], [38], [43], [44], [45], [47], [48], [49], [50], [52], [53], [54].
Table 4.
Career, one-year prevalence rates, and percentage of participants reporting pain in specific body areas
| Authors | Risk factors identified | Consequence of WMSD (%) |
|---|---|---|
| Adegoke et al 2008 [32] | Gender, low BMI, inexperience | Change in working position 13% left the profession |
| Alrowayeh et al 2010 [36] | Gender effect in lower back, neck, and shoulders only | |
| Bork et al 1996 [13] | Gender, work setting, age of patient, specialty | 2.9% of saw a physician 75% changed their work activities |
| Campo et al 2008 [38] | Job factors | 13% saw a physician 7% lost work time 2% changed settings 0.5% left the profession |
| Campo et al 2009 [14] | Job factors | |
| Cromie et al 2000 [33] | Age, job factors | 7.4% lodged workers' compensation claim 13.6% had taken sick leave 84.2% continued working with discomfort 61% sought treatment 42.2% had daily activities affected 17.7% changed their specialty of practice 3.2% left the profession |
| Darragh et al 2009 [40] | Amount of work, type of work | |
| Dyrkacz et al 2012 [41] | Job factors | 67.1% reported injury 49.5% sought medical attention 92.5% continued to work after being injured |
| Glover et al 2005 [42] | Inexperience, age | 61% sought informal treatment 39% saw a physician 16% reported their injury 10% completed a workplace incident form |
| Grooten et al 2011 [43] | Job factors | 57.6% had pain interfering with work |
| Hill et al 2009 [44] | Abdominal girth | |
| Islam et al 2015 [45] | Age, gender | |
| Lorusso et al 2007 [47] | Age, length of employment | |
| Losa et al 2010 [48] | Marital status, age | |
| Nordin et al 2011 [49] | Gender, BMI | |
| Passier and McPhail 2011 [50] | 63.2% of WMSDs were self-managed 10.5% saw a physician 27.6% saw a PT 6.5% reported injury 3% lodged in workers compensation claim 59% continued working 30% worked in modified work tasks 6.5% continued working with no pain or impact on work 19.7% took leave from work |
|
| Rozenfeld et al 2010 [16] | Job factors, inexperience 45% in the first 5 y | 64.5% modified treatment 10.8% changed work settings |
| Rugelj 2003 [52] | 18% visited a doctor 21% took sick leave |
|
| Salik and Ozcan 2004 [53] | Job factors | 69% visited a doctor 46% reported injury |
| Sin Ho, Jin Gang 2013 [54] | Gender, Job factors, Inexperience | 37.8% changed patient treatment 14.2% changed expertise area 52.2% were considering job transfer |
| Vieira et al 2016 [18] | Level of experience, less hours of direct patient care, type or work | |
| West and Gardner 2001 [34] | Inexperience 56% in the first 5 y, job factors | 77% sought physio treatment 45% took prescribed medication 42% saw a physician 24% took time off on sick leave only 4% took time off on workers compensation 41% changed duties 39% changed work setting |
BMI, body mass index; PT, physiotherapist; WMSD, work-related musculoskeletal injury and disorder.
Prevalence rates for injuries of the neck ranged from 4.9% [38] to 65% [45], shoulder from 0.95% [48] to 73% [44], and upper back from 2.4% [38] to 70% [45]. Other areas of the body with reported WMSDs included the wrist/hand, knee, hip/thigh, ankle/foot, and the thumb.
Areas of injury tended to be associated with specific job-related tasks of each occupational group. For example, sonographers reported the highest prevalence of shoulder injuries (73%) [44], while occupational therapists and physiotherapists performing manual therapy tasks reported pain and discomfort in the fingers and hands [13], [16], [34], [41].
3.4. Risk factors for WMSD
Risk factors associated with WMSD development varied across the reviewed studies (Table 4). The role of gender as a risk factor for WMSD was mixed. Six studies [13], [32], [36], [45], [49], [54] reported that females were associated with an increased WMSD risk in some body areas, and four studies [34], [38], [47], [53] found no correlation. Females were generally overrepresented in sample populations, as described earlier. Age was found to be a risk factor in five studies [33], [42], [45], [47], [48] with younger AHPs at a higher risk of developing a WMSD.
Location of the workplace and type of work undertaken were also identified as risk factors for WMSD development [13], [18], [34], [40]. Those working in acute care and outpatient rehabilitation were identified to be at a greater risk of WMSD development compared with those working in community-based settings and private practice [40].
Five studies [13], [38], [42], [53], [54] asked participants to identify factors that contributed to the development of their WMSDs. Factors identified by participants were predominately physical in nature and included working in awkward positions [54], working in the same position [53], bending or twisting, transferring patients [13], [38], lifting [42], performing tasks monotonously [42], performing repetitive tasks [53], a high number of patients [54], and a lack of rest breaks [54].
Three studies [14], [44], [47] explored the relationship between psychosocial factors and WMSDs. Two of these studies [14], [44] examined the relationship between WMSDs and job strain, and reported that low job control and high levels of stress increased the risk of WMSDs in males only. The same finding was not reported for the females included in the study.
3.5. Treatment of WMSDs
Thirteen articles explored the range of treatment options used by those with a WMSD [13], [16], [32], [33], [34], [38], [41], [42], [43], [50], [52], [53], [54] (Table 4). Analysis of these 13 articles found that more people reported experiencing a WMSD than seeking treatment. Individuals often utilized self-treatment strategies, such as massage, stretching, or ultrasound [33], [42]. Lost work days were not associated with medical treatment or whether the injury was reported, suggesting that AHPs are more likely to take sick leave to manage a WMSD than to make an official claim or report their injury to a supervisor [33], [42], [50], [52]. Under-reporting of WMSDs in health care professions has been reported elsewhere [11], [23] and also by studies included in this review [33], [40], [52], [57], [58].
4. Discussion
A 1-year prevalence rate of between 28% [38] and 96% [18], [44] indicates AHPs are at high risk of developing a WMSD. Many studies have reported the reticence of allied health employees to report a WMSD [33], [38], [40], [42], [50], [52]. Cromie et al [39] report that a perception among physiotherapists was that “to discuss WMSDs was apparently to admit that they failed to live up to the standard required…”. Rosenman et al [24] reported that many workers with occupational injuries do not submit a claim for workers' compensation. Analysis of the results from the studies in this review suggest that self-reported career prevalence WMSD injury rates vary [33], [52] in contrast to injury reports [33], [41]. This suggests that AHPs are not consistent in their reporting of injuries, and as such compensation statistics are unlikely to reflect actual injury rates in AHPs.
Glover and colleagues [42] suggested that WMSD prevalence and risk factors identified by individuals may vary due to inconsistencies in the definitions of WMSDs used in the studies. Definitions of WMSDs ranged from a more general description such as “a job-related ache or pain or discomfort” [13] to the more specific stating “a report of WMSD rated at least 4/10 on visual analogue scale and lasting more than 1 week or presenting more than once a month” [38]. This variation makes comparisons of WMSD prevalence rates difficult and may, in part, explain the large variance in prevalence rates reported across studies.
Prevalence measures, such as career and 1-year prevalence, have their strengths and weaknesses. Career prevalence is likely to be affected by recall bias due to the potential time between injury and data collection of the study. Studies measuring career prevalence may, therefore, under-report actual WMSD numbers. One-year prevalence measures were used by some studies [13], [14], [16], [18], [32], [33], [34], [36], [38], [42], [43], [44], [45], [48], [50], [53], [54] to reduce bias issues associated with career prevalence data. One-year prevalence measures may be less influenced by recall bias than by career bias.
Inexperience was identified as a risk factor for WMSD development. The survivor effect [59], [60] has been well described in some studies, and affords an alternative explanation to the relationship between inexperience and WMSD risk. WMSD risk factors identified by participants were predominately physical in nature. This may be due to survey design and the fact that questions relating to psychosocial factors were not routinely included in the questionnaires used. The work environment was not well described in the studies examined here. This is a substantial gap in the literature given the important relationship between work environment and development of WMSDs [61].
The heterogeneity of the studies included in this review makes establishing a core set of common risk factors for WMSDs challenging. The majority of studies included in this systematic review were observational, retrospective, cross-sectional studies. Limitations of a cross-sectional design are well described elsewhere [62], and include issues of temporality and bias (response, recall, and selection). An inclusive search strategy revealed a limited scope of literature concerning WMSDs in the AHPs (Table 1). As defined by Allied Health Professions Australia [9], all 16 titles were included in the search terms, yet only five groups were represented in the literature: physiotherapy, occupational therapy, sonography, podiatry, and medical imaging. Significant differences in the outcome measures used, including the survey tools, definitions of WMSDs, and time frames used from injury onset, make comparisons across the literature difficult. Future studies should aim to adopt greater consistency in the survey tools employed and in the definitions of WMSDs, to ensure meaningful comparisons within and across professional groups.
5. Conclusion
Results from the current review suggest that AHPs may experience a WMSD in their career. High risk factors associated with the development of a WMSD include being a younger therapist, having fewer years of experience, and being exposed to higher levels of manual and repetitive tasks.
High-quality research is needed, which employs consistent outcome measures to improve the ability to draw meaningful comparisons across studies. While research supports the complex multifactorial nature of WMSD development, most of the studies included in the current review focused predominately on the physical factors, with negligible attention being given to psychosocial environmental hazards or risks. The high prevalence rates found in this review suggest a need for more effective WMSD risk reduction interventions. In order to achieve this, accurate identification of all the relevant hazards and risks for AHPs is required, suggesting a direction for future research.
Conflicts of interest
This work was completed by the authors with no external funding or grant sources.
References
- 1.Safe Work Australia . 2013. Compendium of Workers' Compensation Statistics 2010–2011. [Google Scholar]
- 2.Baldwin A., Woods K., Copeland Simmons M. Diversity of the allied health workforce: the unmet challenge. J Allied Health. 2006;34:116–120. [PubMed] [Google Scholar]
- 3.Colins K., Jones M., McDonnell A., Read S., Jones R., Cameron A. Do new roles contribute to job satisfaction and retention of staff in nursing and professions allied to medicine? J Nurs Manag. 2000;8:3–12. [PubMed] [Google Scholar]
- 4.Dodd J., Saggers S., Wildy H. Retention in the allied health workforce: boomers, generation X and generation Y. J Allied Health. 2009;38:215–219. [PubMed] [Google Scholar]
- 5.Lyons K., Lapin J., Young B. A study of job satisfaction of nursing and allied health graduates from a mid-Atlantic university. J Allied Health. 2003;32:10–17. [PubMed] [Google Scholar]
- 6.O'Toole K., Schoo A., Hernan A. Why did they leave and what can they tell us? Allied health professionals leaving rural settings. Aust Health Rev. 2010;34:66–72. doi: 10.1071/AH09711. [DOI] [PubMed] [Google Scholar]
- 7.Stagnitti K., Schoo A., Dunbar J., Reid C. An exploration of issues of management and intention to stay: allied health professionals in South West Victoria, Australia. J Allied Health. 2006;35:226–232. [PubMed] [Google Scholar]
- 8.Wilson N. Factors that affect job satisfaction and intention to leave of allied health professionals in a metropolitan hospital. Aust Health Rev. 2015;39:290–294. doi: 10.1071/AH14198. [DOI] [PubMed] [Google Scholar]
- 9.Allied Health Professions Australia (AHPA). About AHPA [Internet]. 2013 [cited 2016 Mar 12]. Available from: http://wwwahpacomau/Home/aboutAHPA/BenefitsofMembership/CurrentMembershipaspx.
- 10.Dawson A.P., McLennan S.N., Schiller S.D., Jull G.A., Hodges P.W., Stewart S. Interventions to prevent back pain and back injury in nurses: a systematic review. Occup Environ Med. 2007;64:642–650. doi: 10.1136/oem.2006.030643. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Gropelli T.M., Corle K. Nurses' and therapists experiences with occupational musculoskeletal injuries. AAOHN J. 2010;58:159–166. doi: 10.3928/08910162-20100316-01. [DOI] [PubMed] [Google Scholar]
- 12.Oakman J., Macdonald W., Wells Y. Developing a comprehensive approach to risk management of musculoskeletal disorders in non-nursing health care sector employees. Appl Ergon. 2014;45:1634–1640. doi: 10.1016/j.apergo.2014.05.016. [DOI] [PubMed] [Google Scholar]
- 13.Bork B.E., Cook T.M., Rosecrance J.C., Engelhardt K.A., Thomason M.E., Wauford I.J., Worley R.K. Work-related musculoskeletal disorders among physical therapists. Phys Ther. 1996;76:827–835. doi: 10.1093/ptj/76.8.827. [DOI] [PubMed] [Google Scholar]
- 14.Campo M.A., Weiser S., Koenig K.L. Job strain in physical therapists. Phys Ther. 2009;89:946–956. doi: 10.2522/ptj.20080322. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Cromie J.E., Robertson V.J., Best M.O. Occupational health and safety in physiotherapy: guidelines for practice. Aust J Physiother. 2001;47:43–51. doi: 10.1016/s0004-9514(14)60297-x. [DOI] [PubMed] [Google Scholar]
- 16.Rozenfeld V., Ribak J., Danziger J., Tsamir J., Carmeli E. Prevalence, risk factors and preventive strategies in work-related musculoskeletal disorders among Israeli physical therapists. Physiother Res Int. 2010;15:176–184. doi: 10.1002/pri.440. [DOI] [PubMed] [Google Scholar]
- 17.Sharan D., Ajeesh P.S. Injury prevention in physiotherapists—a scientific review. Work. 2012;41(Suppl 1):1855–1859. doi: 10.3233/WOR-2012-0397-1855. [DOI] [PubMed] [Google Scholar]
- 18.Vieira E.R., Svoboda S., Belniak A., Brunt D., Rose-St Prix C., Roberts L., da Costa B.R. Work-related musculoskeletal disorders among physical therapists: an online survey. Disabil Rehabil. 2016;38:552–557. doi: 10.3109/09638288.2015.1049375. [DOI] [PubMed] [Google Scholar]
- 19.Hignett S. Intervention strategies to reduce musculoskeletal injuries associated with handling patients: a systematic review. Occup Environ Med. 2003;60:E6. doi: 10.1136/oem.60.9.e6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Macdonald W., Evans O. 2006. Research on the prevention of musculoskeletal disorders Stage 1: literature review. [Google Scholar]
- 21.Macdonald W. Workload, stress and psychosocial factors as hazards for musculoskeletal disorders. J Occup Health Saf. 2004;20:37–47. [Google Scholar]
- 22.Safe Work Australia . 2013. Issues in the measurement and reporting of work health and safety performance: a review. [Google Scholar]
- 23.Menzel N.N. Underreporting of musculoskeletal disorders among health care workers: research needs. AAOHN J. 2008;56:487–494. doi: 10.3928/08910162-20081201-06. [DOI] [PubMed] [Google Scholar]
- 24.Rosenman K.D., Gardiner J.C., Wang J., Biddle J., Hogan A., Reilly M.J., Roberts K., Welch E. Why most workers with occupational repetitive trauma do not file for workers' compensation. J Occup Environ Med. 2000;42:25–34. doi: 10.1097/00043764-200001000-00008. [DOI] [PubMed] [Google Scholar]
- 25.Law M., Stewart D., Pollock N., Letts L., Bosch J., Westmorland M. McMaster University; 1998. Critical review form – quantitative studies. [Google Scholar]
- 26.Letts L., Wilkins S., Law M., Stewart D., Bosch J., Westmorland M. McMaster University; 2007. Critical review form—qualitative studies, version 2.0. [Google Scholar]
- 27.Critical Appraisal Skills Programme . 2013. Systematic review checklist. [Google Scholar]
- 28.Caragianis S. The prevalence of occupational injuries among hand therapists in Australia and New Zealand. J Hand Ther. 2002;15:234–241. doi: 10.1016/s0894-1130(02)70006-9. [DOI] [PubMed] [Google Scholar]
- 29.Snodgrass S.J., Rivett D.A., Chiarelli P., Bates A.M., Rowe L.J. Factors related to thumb pain in physiotherapists. Aust J Physiother. 2003;49:243–250. doi: 10.1016/s0004-9514(14)60140-9. [DOI] [PubMed] [Google Scholar]
- 30.Wajon A., Ada L., Refshauge K. Work-related thumb pain in physiotherapists is associated with thumb alignment during performance of PA pressures. Man Ther. 2007;12:12–16. doi: 10.1016/j.math.2005.09.003. [DOI] [PubMed] [Google Scholar]
- 31.Ruess L., O'Connor S.C., Cho K.H., Hussain F.H., Howard W.J., III, Slaughter R.C., Hedge A. Carpal tunnel syndrome and cubital tunnel syndrome: work-related musculoskeletal disorders in four symptomatic radiologists. Am J Roentgenol. 2003;181:37–42. doi: 10.2214/ajr.181.1.1810037. [DOI] [PubMed] [Google Scholar]
- 32.Adegoke B.O., Akodu A.K., Oyeyemi A.L. Work-related musculoskeletal disorders among Nigerian physiotherapists. BMC Musculoskelet Disord. 2008;9:112. doi: 10.1186/1471-2474-9-112. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Cromie J.E., Robertson V.J., Best M.O. Work-related musculoskeletal disorders in physical therapists: prevalence, severity, risks, and responses. Phys Ther. 2000;80:336–351. doi: 10.1093/ptj/80.4.336. [DOI] [PubMed] [Google Scholar]
- 34.West D.J., Gardner D. Occupational injuries of physiotherapists in North and Central Queensland. Aust J Physiother. 2001;47:179–186. doi: 10.1016/s0004-9514(14)60265-8. [DOI] [PubMed] [Google Scholar]
- 35.Alnaser M.Z. Occupational musculoskeletal injuries in the health care environment and its impact on occupational therapy practitioners: a systematic review. Work. 2007;29:89–100. [PubMed] [Google Scholar]
- 36.Alrowayeh H.N., Alshatti T.A., Aljadi S.H., Fares M., Alshamire M.M., Alwazan S.S. Prevalence, characteristics, and impacts of work-related musculoskeletal disorders: a survey among physical therapists in the State of Kuwait. BMC Musculoskelet Disord. 2010;11:116. doi: 10.1186/1471-2474-11-116. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Kuorinka I., Jonsson B., Kilbom A., Vinterberg H., Biering-Sorensen F., Andersson G., Jørgensen K. Standardised Nordic questionnaire for the analysis of musculoskeletal symptoms. Appl Ergon. 1987;18:233–237. doi: 10.1016/0003-6870(87)90010-x. [DOI] [PubMed] [Google Scholar]
- 38.Campo M., Weiser S., Koenig K.L., Nordin M. Work-related musculoskeletal disorders in physical therapists: a prospective cohort study with 1-year follow-up. Phys Ther. 2008;88:608–619. doi: 10.2522/ptj.20070127. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Cromie J.E., Robertson V.J., Best M.O. Work-related musculoskeletal disorders and the culture of physical therapy. Phys Ther. 2002;82:459–472. [PubMed] [Google Scholar]
- 40.Darragh A.R., Huddleston W., King P. Work-related musculoskeletal injuries and disorders among occupational and physical therapists. Am J Occup Ther. 2009;63:351–362. doi: 10.5014/ajot.63.3.351. [DOI] [PubMed] [Google Scholar]
- 41.Dyrkacz A.P., Mak L.Y., Heck C.S. Work-related injuries in Canadian occupational therapy practice. Can J Occup Ther. 2012;79:237–247. doi: 10.2182/cjot.2012.79.4.5. [DOI] [PubMed] [Google Scholar]
- 42.Glover W., McGregor A., Sullivan C., Hague J. Work-related musculoskeletal disorders affecting members of the Chartered Society of Physiotherapy. Physiotherapy. 2005;91:138–147. [Google Scholar]
- 43.Grooten W.J., Wernstedt P., Campo M. Work-related musculoskeletal disorders in female Swedish physical therapists with more than 15 years of job experience: prevalence and associations with work exposures. Physiother Theory Pract. 2011;27:213–222. doi: 10.3109/09593985.2010.481323. [DOI] [PubMed] [Google Scholar]
- 44.Hill J.J., 3rd, Slade M.D., Russi M.B. Anthropometric measurements, job strain, and prevalence of musculoskeletal symptoms in female medical sonographers. Work. 2009;33:181–189. doi: 10.3233/WOR-2009-0865. [DOI] [PubMed] [Google Scholar]
- 45.Islam M., Habib M., Hafez M., Nahar N., Lindstrom-Hazel D., Rahman M. Musculoskeletal complaints among physiotherapy and occupational therapy rehabilitation professionals in Bangladesh. Work. 2015;50:379–386. doi: 10.3233/WOR-151994. [DOI] [PubMed] [Google Scholar]
- 46.Kumar S., Moro L., Narayan Y. Perceived physical stress at work and musculoskeletal discomfort in X-ray technologists. Ergonomics. 2004;47:189–201. doi: 10.1080/00140130310001617958. [DOI] [PubMed] [Google Scholar]
- 47.Lorusso A., Bruno S., L'Abbate N. Musculoskeletal complaints among Italian X-ray technologists. Ind Health. 2007;45:705–708. doi: 10.2486/indhealth.45.705. [DOI] [PubMed] [Google Scholar]
- 48.Losa I.M., Becerro D.B.V.R., Salvadores F.P. Self-reported musculoskeletal disorders in podiatrists at work. Med Lav. 2010;102:502–510. [PubMed] [Google Scholar]
- 49.Nordin N.A., Leonard J.H., Thye N.C. Work-related injuries among physiotherapists in public hospitals: a Southeast Asian picture. Clinics (Sao Paulo) 2011;66:373–378. doi: 10.1590/S1807-59322011000300002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50.Passier L., McPhail S. Work-related injuries amongst occupational therapists: a preliminary investigation. Br J Occup Ther. 2011;74:143–147. [Google Scholar]
- 51.Passier L., McPhail S. Work related musculoskeletal disorders amongst therapists in physically demanding roles: qualitative analysis of risk factors and strategies for prevention. BMC Musculoskelet Disord. 2011;12:24. doi: 10.1186/1471-2474-12-24. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 52.Rugelj D. Low back pain and other work-related musculoskeletal problems among physiotherapists. Appl Ergon. 2003;34:635–639. doi: 10.1016/S0003-6870(03)00059-0. [DOI] [PubMed] [Google Scholar]
- 53.Salik Y., Ozcan A. Work-related musculoskeletal disorders: a survey of physical therapists in Izmir-Turkey. BMC Musculoskelet Disord. 2004;5:27. doi: 10.1186/1471-2474-5-27. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 54.Sin Ho C., Jin Gang H., Taesung K., Jooyen K., Heesoo K., Ju Sang L., Ji-Hae W. Work-related musculoskeletal disorders among Korean physical therapists. J Phys Ther Sci. 2013;25:55–59. [Google Scholar]
- 55.Hammer G.P., Prel J-Bd, Blettner M. Avoiding bias in observational studies part 8 of a series on evaluation of scientific publications. Dtsch Arztebl Int. 2009;106:664–668. doi: 10.3238/arztebl.2009.0664. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 56.Schofield D.J., Fletcher S.L. The physiotherapy workforce is ageing, becoming more masculinised, and is working longer hours: a demographic study. Aust J Physiother. 2007;53:121–126. doi: 10.1016/s0004-9514(07)70045-4. [DOI] [PubMed] [Google Scholar]
- 57.Glover W. Work-related strain injuries in physiotherapists: prevalence and prevention of musculoskeletal disorders. Physiotherapy. 2002;88:364–372. [Google Scholar]
- 58.Campo M., Darragh A.R. Work-related musculoskeletal disorders are associated with impaired presenteeism in allied health care professionals. J Occup Environ Med. 2012;54:64–70. doi: 10.1097/JOM.0b013e31823c768a. [DOI] [PubMed] [Google Scholar]
- 59.Arrighi H.M., Hertz-Picciotto I. The evolving concept of the healthy worker survivor effect. Epidemiology. 1994;5:189–196. doi: 10.1097/00001648-199403000-00009. [DOI] [PubMed] [Google Scholar]
- 60.Carpenter L.M. Some observations on the healthy worker effect. Br J Ind Med. 1987;44:289–291. doi: 10.1136/oem.44.5.289. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 61.Oakman J., Chan S. Risk management: where should we target strategies to reduce work-related musculoskeletal disorders? Saf Sci. 2014;73:99–105. [Google Scholar]
- 62.Graham M. How do we know what we know? Epidemiology in health research. In: Liamputtong P., editor. Research methods in health. Oxford University Press; Melbourne, Australia: 2010. pp. 219–233. [Google Scholar]
- 63.W.F. Blair, Work Related Musculoskeletal Disorder (WMSDs): A reference book for prevention: M. Hagberg et al., Taylor and Francis, Inc., 1900 Frost Road, Suite 101, Bristol, PA 19007.
- 64.Holder N.L., Clark H.A., DiBlasio J.M., Hughes C.L., Scherpf J.W., Harding L., Shepard K.F. Cause, prevalence, and response to occupational musculoskeletal injuries reported by physical therapists and physical therapist assistants. Phys Ther. 1999;79:642–652. doi: 10.1093/ptj/79.7.642. [DOI] [PubMed] [Google Scholar]
- 65.Karasek R.A. Job Demands, Job Decision Latitude, and Mental Strain: Implications for Job Redesign. Adm Sci Q. 1979;24:285–308. [Google Scholar]