Abstract
A 58-year-old woman presented with a 4 cm obstructing choledocolith within the proximal common bile duct. She had an extensive operative history resulting in common bile duct to jejunum anastomosis after cholecystectomy. Endoscopic retrograde cholangiopancreatography (ERCP) removal was unsuccessful, and surgical exploration was contraindicated due to multiple comorbidities. Interventional radiologist placement of bilateral transhepatic ureteral access sheaths allowed Urologist evaluation of the biliary tract by ureteroscope. Holmium laser lithotripsy was performed with successful fragmentation of the stone and clearance of the obstruction, without complication. The case is relevant to the growing literature on the management of refractory biliary stones after failed ERCP.
Keywords: Holmium laser, Percutaneous lithotripsy, Interventional radiology, Biliary intervention, Choledocolithiasis
Case report
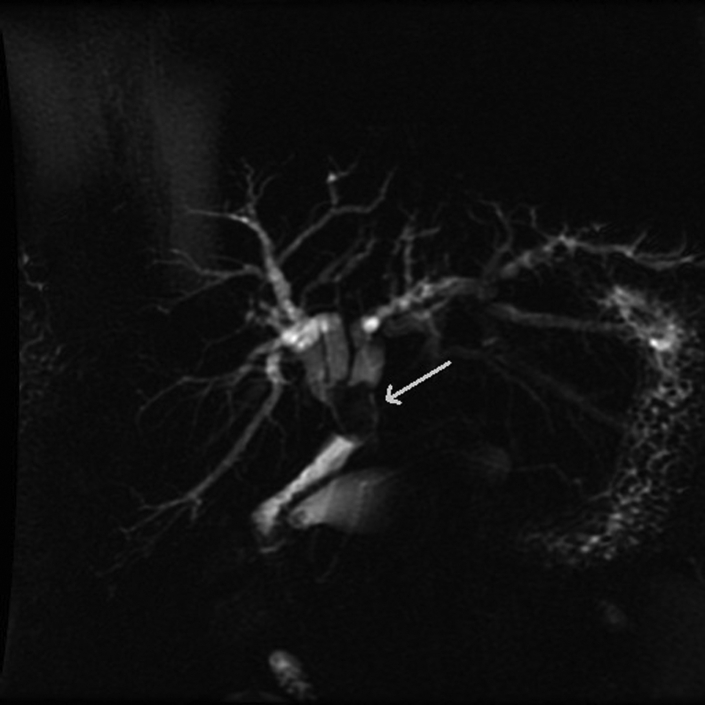
A 58-year-old woman presented with acutely worsening right upper quadrant abdominal pain and intermittent fevers. The patient’s aspartate and alanine aminotransferase levels were elevated, measuring 187 and 233 IU/L, respectively. Her medical and surgical histories were significant for common bile duct (CBD) injury after laparoscopic cholecystectomy, which required reconstruction in 1990 (15 years prior) and subsequent hepaticojejunostomy with Roux-en-Y. Magnetic resonance cholangiopancreatography was performed and outlined the postsurgical anatomy. There was a CBD-jejunum anastomosis and a large 4-cm obstructing choledocolith within the proximal common bile duct (Fig. 1).
Fig. 1.
Magnetic resonance cholangiopancreatography. Thick-slab maximum intensity 3-dimensional-reconstruction image showing the common bile duct-jejunum anastomosis with hypointense 4-cm biliary stone (white arrow) filling the remnant of the extrahepatic common bile duct. There is intrahepatic biliary ductal dilatation.
The interventional radiologist first performed a percutaneous transhepatic cholangiogram which confirmed biliary obstruction. Percutaneous 8-Fr biliary drains (Cook Medical, IN) were then placed bilaterally in the left and right intrahepatic biliary ductal systems and extended past the obstructing stone to coil within the postanastomotic jejunum (Fig. 2). Although this temporarily resolved the biliary obstruction, definitive management was still required.
Fig. 2.
Anteroposterior (AP) projection fluoroscopic biliary cholangiogram showing the placement of bilateral 8-French biliary drains. The coiled ends are in the proximal jejunum, distal to a large obstructing biliary stone. Side holes within each drain are positioned proximally to the stone to decompress the intrahepatic biliary system.
The hospital’s Gastroenterology service was consulted. Endoscopic retrograde cholangiopancreatography (ERCP) was performed, but it was unsuccessful due to difficulties traversing the patient’s postsurgical biliary anatomy. Open surgical intervention would have carried a high risk of morbidity. At this point, a urologic specialist was consulted for an endourologic procedure in conjunction with the interventional radiologist. Ureteroscopy with laser lithotripsy through percutaneous transhepatic ureteral access sheaths was planned to clear her stone burden.
The pre-existing medially and laterally located biliary drains were removed over an angled Glidewire GT (Terumo, NJ). Using two 8-Fr Super Sheath Introducers (Boston Scientific, MA), two 180-cm Super Stiff Amplatz wires (Boston Scientific) were advanced into the postanastomotic bowel from each access. Two 11 × 13-Fr Navigator HD ureteral access sheaths (Boston Scientific) were then advanced over each wire to the level of the stone (Fig. 3).
Fig. 3.
AP fluoroscopic image taken during biliary stone removal. Two 180-cm Boston Scientific Super Stiff Amplatz wires were advanced into the postanastomotic bowel from percutaneous hepatic access on each side. Two 11 × 13-Fr Boston Scientific Navigator HD ureteral access sheaths were then advanced over each wire. The Kelly forceps denote the left-sided (more medial) wire.
The LithoView flexible ureteroscope (Boston Scientific) was assembled and advanced through the lateral sheath to the jejunum. The sheath was then slowly withdrawn until the common bile duct stone was visualized. Using a 360-nm Lumenis VersaPulse holmium laser fiber (Boston Scientific, 0.8 J, 5 Hz), the stone was fragmented into multiple smaller pieces (Fig. 4). A 1.9-Fr Escape nitinol retrieval basket (Boston Scientific) was used to extract a sample fragment for compositional analysis. The remaining fragments were easily irrigated antegrade into the jejunum. A single-action pump was used to control the irrigant flow. The ureteroscope was then withdrawn and passed through the medial sheath. A few smaller stones were identified and were fragmented with the holmium laser in a similar fashion (Fig. 5). No intraoperative or postoperative complications were noted.
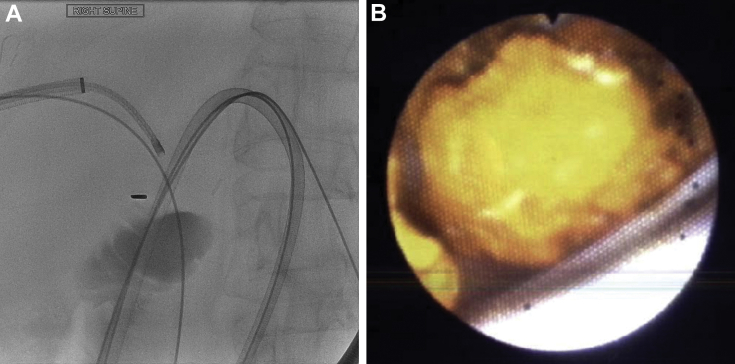
Fig. 4.
(A) Fluoroscopic image of ureteroscope and laser in the right intrahepatic biliary system with tip at region of large biliary stone. (B) Corresponding color ureteroscopic image of a 4-cm stone, just before fracturing with holmium laser. The tip of the ureteral sheath can be seen at the bottom of the image.
Fig. 5.
(A) Fluoroscopic image of ureteroscope in the left (more medial) intrahepatic biliary system with tip at region of residual stone fragments. (B) Corresponding color ureteroscope image showing residual stone fragments which were subsequently passed into jejunum. The white wire in the image correlates with radiodense wire seen in A.
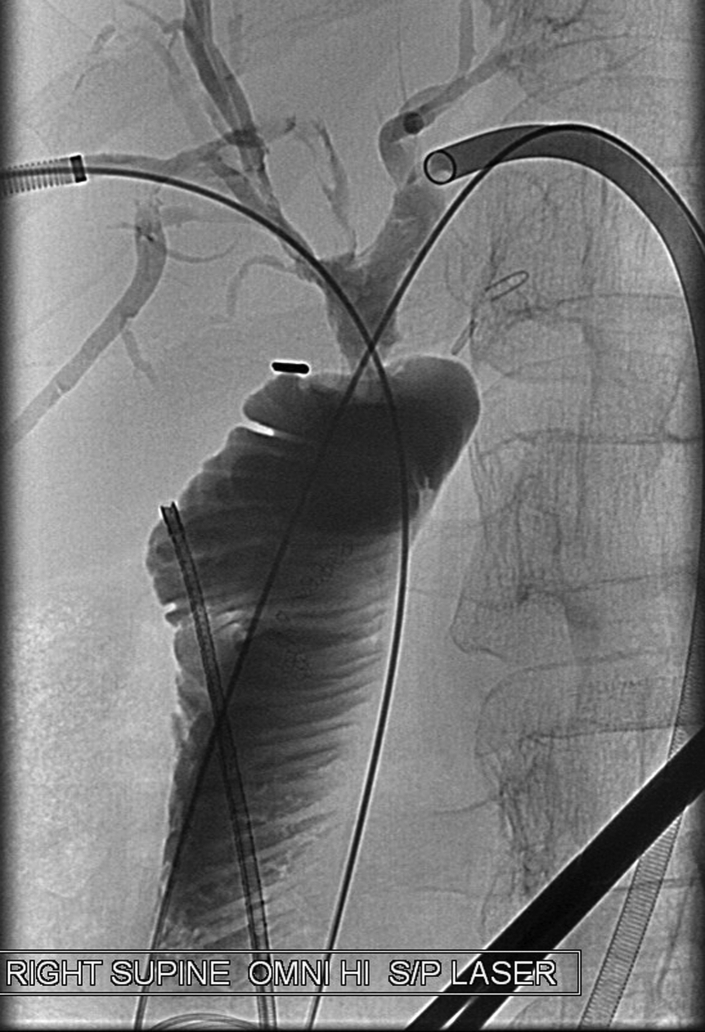
Intraoperative cholangiogram confirmed a patent anastomosis without contrast extravasation (Fig. 6). The ureteroscope was then removed along with both access sheaths. These were replaced with 12-Fr Cook biliary drainage catheters. The patient remained hospitalized for 3 days after the procedure and was discharged without complication. The biliary drains were downsized on subsequent examination at 10 days. These were ultimately removed in follow-up at approximately 1 month. No complications were reported.
Fig. 6.
AP projection fluoroscopic biliary cholangiogram status postholmium laser lithotripsy. The CBD and/or jejunum anastomosis is patent. Bilateral ureteral catheter sheaths and Amplatz wires remain in place at this time. The ureteroscope overlies the patient in the image.
Discussion
Holmium laser lithotripsy for biliary stone disease using interventional and endourologic techniques is uncommon but is a reasonable treatment option in select cases after failed ERCP. ERCP may be challenging in patients with large stones and surgically altered anatomy. Open common bile duct exploration is the current treatment of choice after failed ERCP. However, a percutaneous approach with ureteroscopic lithotripsy is an alternative which may minimize patient morbidity.
Pulsed dye lasers (like the Holmium laser) emit visible light. These lasers have a variety of applications including cardiac valve remodeling, bone tumor ablation, and endoscopic enucleation [1]. During lithotripsy, the laser can be used to fragment stones while minimizing both stone retropulsion and surrounding soft-tissue damage [2].
Patel et al. carried out the largest clinical study to date using a Holmium laser in 69 patients with choledocolithiasis. Among the 69 patients, the biliary stones were successfully removed in 67 patients. The complication rate in this study was 4.1% (with 2 patients who experienced minor bleeding and 1 patient who developed mild post-ERCP pancreatitis) [3].
In this case, minimally invasive percutaneous ureteroscopy and laser lithotripsy obviated the need for an open procedure. As shown by Patel et al. and other reports in the growing Urologic literature [4], [5], [6], gallstone lithotripsy using a holmium laser can be a reasonable and safe alternative for many patients. The interventional radiologist plays an active role in these cases.
The case is relevant to the growing literature on the management of refractory biliary stones. Percutaneous approach and ureteroscopic laser lithotripsy were performed in a difficult post-CBD and/or jejunal anastomotic setting, after failed ERCP.
Footnotes
Competing Interests: The authors have declared that no competing interests exist.
References
- 1.Burdick J.S., Magee D.J., Hernandez E.J., Clark P.J., Miller G. Holmium laser for treatment of left hepatic duct stone. Gastrointest Endosc. 1998;48(5):523–526. doi: 10.1016/s0016-5107(98)70098-7. [DOI] [PubMed] [Google Scholar]
- 2.Lerardi A.M., Fontana F., Petrillo M., Floridi C., Cocozza E., Segato S. Percutaneous transhepatic endoscopic holmium laser lithotripsy for intrahepatic and choledochal biliary stones. Int J Surg. 2013;11(Suppl 1):S36–S39. doi: 10.1016/S1743-9191(13)60011-4. [DOI] [PubMed] [Google Scholar]
- 3.Patel S.N., Rosenkranz L., Hooks B., Tarnasky P.R., Raijman I., Fishman D.S. Holmium-yttrium aluminum garnet laser lithotripsy in the treatment of biliary calculi using single-operator cholangioscopy: a multicenter experience (with video) Gastrointest Endosc. 2014;79(2):344–348. doi: 10.1016/j.gie.2013.07.054. [DOI] [PubMed] [Google Scholar]
- 4.Korkes F., Carneiro A., Nasser F., Affonso B.B., Galastri F.L., Oliveira M.B. Percutaneous treatment of complex biliary stone disease using endourological technique and literature review. Einstein (Sao Paulo) 2015;13(4):611–614. doi: 10.1590/S1679-45082015RC2935. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Rimon U., Kleinmann N., Bensaid P., Golan G., Garniek A., Khaitovich B. Percutaneous transhepatic endoscopic holmium laser lithotripsy for intrahepatic and choledochal biliary stones. Cardiovasc Intervent Radiol. 2011;34(6):1262–1266. doi: 10.1007/s00270-010-0058-x. [DOI] [PubMed] [Google Scholar]
- 6.Ray A.A., Davies E.T., Duvdevani M., Razvi H., Denstedt J.D. The management of treatment-resistant biliary calculi using percutaneous endourologic techniques. Can J Surg. 2009;52(5):407–412. [PMC free article] [PubMed] [Google Scholar]