Abstract
Colon cancer metastasis to bone is extremely rare and has devastating consequences on patients’ quality of life. Furthermore, radiofrequency ablation in conjunction with cementoplasty to nonweight bearing, flat bones has not been widely reported as palliative treatment for pain as a result of bone metastasis. Here, we present a case of a 47-year-old man who developed a sternal metastasis from an invasive adenocarcinoma of the colon originally diagnosed several years prior. The pain from the metastasis was originally treated with external beam radiation therapy, but after 6 weeks of continuous pain, it was retreated using radiofrequency ablation in conjunction with cementoplasty.
Keywords: Sternal augmentation, Cementoplasty, Colon cancer metastasis
Introduction
In 2016, about 1,685,210 new cancer cases are expected to be diagnosed and about 595,690 Americans are expected to die of cancer the same year. Of the 1,685,210 new cases in 2016, it is estimated that 95,270 will be due to colon cancer. Colorectal cancer is currently the third leading cause of cancer death for both men and women [1]. Although surgical removal of a primary colorectal tumor has proven to be beneficial, 30% of patients subsequently develop a metastasis [2], [3]. The most common sites of metastasis are the liver, lungs, and draining lymph nodes [4].
Although it is common for colon cancer to metastasize to the liver and lungs, mainly due to pattern of blood flow and molecular signal proteins, it is widely accepted that colon cancer rarely metastasize to bone [5]. The most common sites for bone metastasis are typically within the axial skeleton and can lead to skeletal-related events such as severe bone pain, pathologic fracture, and the need for surgery to bone as a result of the metastasis [6].
Radiation therapy, analgesics, neurolysis, implantable neuromodulatory procedures, and physical therapy have been used to help treat the pain associated with bone metastasis [7]. Furthermore, treatment for skeletal metastasis is multidisciplinary and requires the combined efforts of orthopedic surgeons, radiation oncologists, and interventional radiologists [8]. Aside from the approaches mentioned previously, percutaneous ablation has been accepted as an effective and minimally invasive technique for treatment of pain associated with metastasis [9]. We present a case where radiofrequency ablation (RFA) was used in conjunction with cement injection as palliative treatment for colon cancer metastasis to the sternum after failure of radiation therapy.
Case presentation
A 47-year-old Caucasian man presented to the emergency department with a chief complaint of chest pain for a period of about 4 months. He was diagnosed with costochondritis and treated with pain medications. His medical history included a diagnosis of colon cancer, T3N0, low-to-moderate differentiated adenocarcinoma in August 2012. During that time, he had presented to the emergency room with complaints of abdominal pain, and he was later diagnosed as having a ruptured appendix. When taken for surgery, it was noted that he had invasive adenocarcinoma, and he underwent a right colectomy. The pathology report was consistent with a 9 × 4 × 3-cm tumor, which was low grade, well to moderately differentiated, and invaded through the muscularis propria into the subserousa. Twenty-six lymph nodes were evaluated and noted to be negative for metastatic disease, and hence, the patient was staged as pT3N0Mx colon adenocarcinoma and was subsequently treated with adjuvant chemotherapy and noted to be without any evidence of the disease about 7-8 months later.
However, since the pain did not improve, the patient underwent computed tomography (CT) of the chest, which showed areas of bronchiectasis with ill-defined opacities and nodularity within both lungs with the right greater than the left. The sternum was noted to be expanded. Subsequently, a positron emission tomography/CT was performed, and it was noted that he had widespread hypermetabolic lesions distributed throughout the body suggesting metastatic disease.
There were also abnormal hypermetabolic areas in the mediastinum and hilum. Furthermore, there was increased density on CT in the midsternum with expansion of the sternum corresponding to the hypermetabolic area (Fig. 1). The patient complained of excruciating pain when the area was palpated, and he was unable to remove his shirt without assistance and the pain interfered with his activities of daily living. When the patient returned to the clinic for further evaluation and treatment for his metastatic cancer with radiation therapy to the painful boney lesions, he complained of significant chest pain and reports that the pain is 9 of 10. On taking oxycodone and the MS Contin, his pain level went down to 6-7. Over the course of 2-3 weeks after the completion of the radiation, he had lost 20 lbs and noted a decreased appetite.
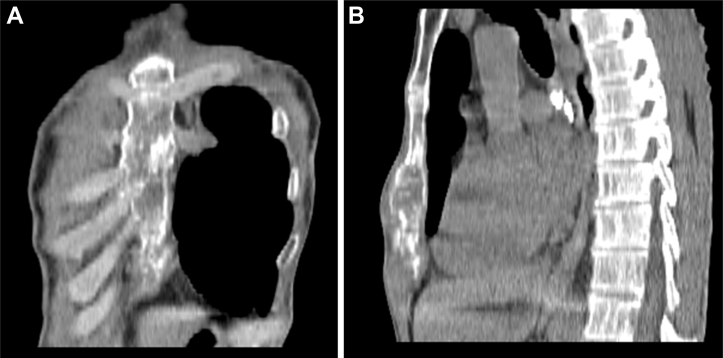
Fig. 1.
A coronal (A) and sagittal (B) reconstructed views of the untreated sternum demonstrating the enlargement of the body of the sternum at the site of the metastatic colon cancer.
He was referred to the interventional radiology service for treatment of his bone pain. He was placed under general anesthesia, and the CT was used to place the 8-ga bone access needle into the sternum at a shallow angle so that it would be less likely to puncture the posterior cortex (Fig. 2). A purpose-designed bipolar radiofrequency (RFA) probe (DFINE, Inc, San Jose, CA) was placed into the tumor so that the RFA field encompassed the entire tumor and proceeded to heat the tumor to 52 C with an elliptical cross-section field size of 2 × 3 cm. Any heating of tissues above 46 C will result in permanent tissue damage and necrosis. The probe was then removed and 4 ml of polymethylmethacrylate (PMMA) cement injected into the cavity formed by the RFA within the sternum (Fig. 3). The procedure was completed, and the patient went to the post anesthesia care unit for recuperation. Two hours later, the patient stated that he had no pain, and this continued for 6 months until his disease burden became overwhelming, and he died 9 months after the procedure without recurrence at the site of treatment.
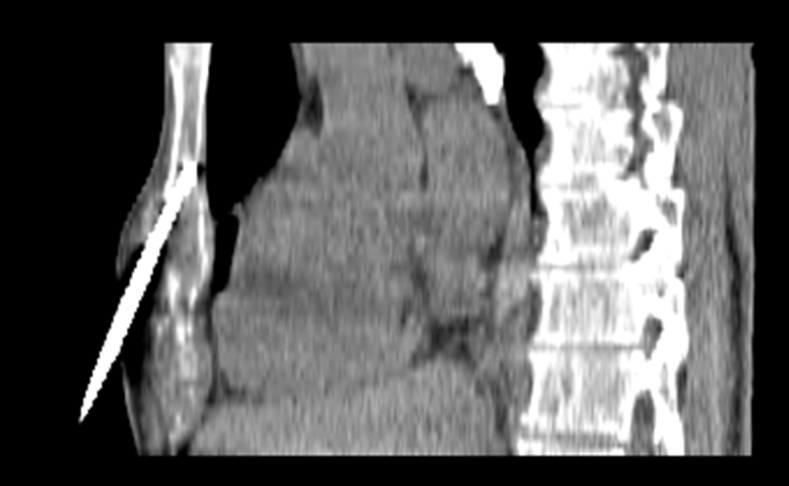
Fig. 2.
A sagittal reconstruction showing the bone guide needle and RFA probe entering the sternum.
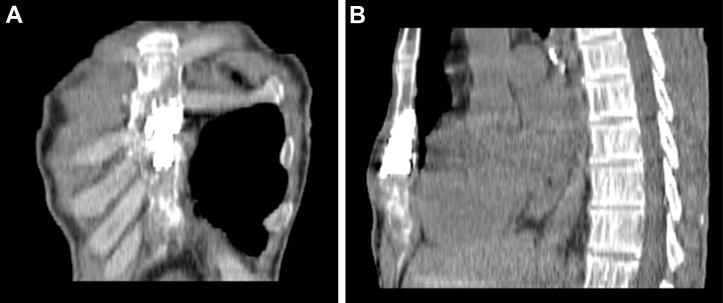
Fig. 3.
A coronal (A) and sagittal (B) reconstruction demonstrating the filling of the interior of the sternum with PMMA cement at the site of the metastasis.
Discussion
Colon cancer commonly metastasizes to the liver and lymph nodes, but it is distinctly unusual for it to metastasize to bone. While this lesion had been radiated for pain relief, this therapy is effective after about 6 weeks, and this particular patient did not respond to the therapy in three weeks. While radiation therapy is the standard of care for boney metastases, it takes time to take effect and is effective in 60%-70% of cases. Direct tumor RFA and cement placement have been noted to be close to immediately effective and performed on an outpatient basis. The length of effectiveness of the procedure is usually around 6-9 months, but it can be performed several times if necessary [10]. It should be viewed as an adjunct to radiation therapy not a replacement. If there are several extremely painful lesions that prevent the patient from undergoing radiation therapy, these lesions can be addressed by this method, and the patient sent for radiation treatment of his remaining metastases. Alternatively, if the metastases do not respond to the radiation, this method may be used as a second-line therapy.
Cementoplasty, also known as osteoplasty or vertebroplasty, requires a percutaneous injection of PMMA cement into the bone [9]. This procedure has been used for treatment of painful bone metastasis and can be used alone or as an adjunct to ablation [9]. Typically, this treatment has been used to treat malignancies or fractures of weight-bearing bones and is thought to contribute to pain relief due to: (1) bone stabilization; (2) direct tissue toxicity; (3) neurolysis; and (4) thermal injury [7].
While cementoplasty for weight-bearing bones has proven to be beneficial in pain management of bone metastasis, cementoplasty for nonweight-bearing, flat bones is still largely unreported in medical literature [7]. In 2012, Shah reported a case of a 58-year-old man who was diagnosed with a sternal mass due to metastasis from lung cancer. The patient was treated via sternal kyphoplasty and reported no pain on palpation after the procedure [7]. Similarly, Zhou et al. presented a case of a 67-year-old woman hospitalized with serious chest pain localized to the anterior chest wall. The patient was treated via percutaneous osteoplasty and reported a signification reduction 7 days postprocedure; at her 6-month follow-up visit, the patient still reported no pain [11].
This is an unusual case in that it demonstrates the effective combination of RFA of the tumor combined with the use of PMMA cement. Both modalities will cause tumor death, but the combination decreases the risk of recurrence at the augmentation site [12], [13].
Footnotes
Competing Interests: The authors have declared that no competing interests exist.
References
- 1.American Cancer Society . American Cancer Society; Atlanta: 2016. Cancer Facts & Figures 2016. [Google Scholar]
- 2.Itatani Yoshiro Y. The role of chemokines in promoting colorectal cancer invasion/metastasis. Int J Mol Sci. 2016;17(5) doi: 10.3390/ijms17050643. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Schlüter Kerstin K. Organ-specific metastatic tumor cell adhesion and extravasation of colon carcinoma cells with different metastatic potential. Am J Pathol. 2006;169(3):1064–1073. doi: 10.2353/ajpath.2006.050566. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Ko F.C., Liu J.M., Chen W.S., Chiang J.K., Lin T.C., Lin J.K. Risk and patterns of brain metastases in colorectal cancer: 27-year experience. Dis Colon Rectum. 1999;42(11):1467–1471. doi: 10.1007/BF02235049. [DOI] [PubMed] [Google Scholar]
- 5.Roth Eira S.E. Does colon cancer ever metastasize to bone first? a temporal analysis of colorectal cancer progression. BMC Cancer. 2009;9:274. doi: 10.1186/1471-2407-9-274. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Coleman Robert R. Treatment of metastatic bone disease and the emerging role of Radium-223. Semin Nucl Med. 2016;46(2):99–104. doi: 10.1053/j.semnuclmed.2015.10.012. [DOI] [PubMed] [Google Scholar]
- 7.Shah Rinoo V.R. Sternal kyphoplasty for metastatic lung cancer: image-guided palliative care, utilizing fluoroscopy and sonography. Pain Med. 2012;13(2):198–203. doi: 10.1111/j.1526-4637.2011.01299.x. [DOI] [PubMed] [Google Scholar]
- 8.Jehn Christian F.C. Management of metastatic bone disease algorithms for diagnostics and treatment. Anticancer Res. 2016;36(6):2631–2637. [PubMed] [Google Scholar]
- 9.Kurup A.N., Callstrom M.R. Ablation of skeletal metastases: current status. J Vasc Interv Radiol. 2010;21(8):242–250. doi: 10.1016/j.jvir.2010.05.001. [DOI] [PubMed] [Google Scholar]
- 10.Anchala P.R., Irving W.D., Hillen T.J., Friedman M.V., Georgy B.A., Coldwell D.M. Treatment of spine metastatic lesions with a navigational bipolar radiofrequency ablation device: a multi-center retrospective study. Pain Phys. 2014;17(4):317–327. [PubMed] [Google Scholar]
- 11.Zhou B., Wu C.G., Li M.H., Gu Y.F., Cheng Y.D. Percutaneous osteoplasty for painful sternal lesion from multiple myeloma. Skeletal Radiol. 2009;38(3):281–285. doi: 10.1007/s00256-008-0620-7. [DOI] [PubMed] [Google Scholar]
- 12.Lane M.D., Le H.B., Lee S., Young C., Heran M.K., Badii M. Combination radiofrequency ablation and cementoplasty for palliative treatment of painful neoplastic bonemetastasis: experience with 53 treated lesions in 36 patients. Skeletal Radiol. 2011;40(1):25–32. doi: 10.1007/s00256-010-1010-5. [DOI] [PubMed] [Google Scholar]
- 13.Botton E., Edeline J., Rolland Y., Vauléon E., Le Roux C., Mesbah H. Cementoplasty for painful bone metastases: a series of 42 cases. Med Oncol. 2012;29(2):1378–1383. doi: 10.1007/s12032-011-9939-3. [DOI] [PubMed] [Google Scholar]