Highlights
-
•
Porocarcinoma is a rare but aggressive type of skin malignancy.
-
•
Reporting new cases is mandatory to outline the course of the disease.
-
•
We systematically reviewed the literature with a new case report.
Keywords: Case report, Poroma, Porocarcinoma, Eccrine
Abstract
Introduction
Eccrine porocarcinoma is a very rare type of skin cancer. It is an aggressive dermatological malignancy. We presented a 62-year-old male with long history of a mass in left forearm complicated by distant metastasis and death. A rapid review of literature has been presented.
Conclusion
Eccrine porocarcinoma is a rare but aggressive type of skin disease. It may arise de novo or complicate a benign skin lesion. Wide local resection is recommended.
1. Introduction
Eccrine porocarcinoma (EP) is a very rare type of skin cancer that is sometime confused with other forms of dermatological malignancies. [1] Pinkus and Mehregan were the first to describe EP in 1963. [2] Although the exact prevalence is not known, according to some authors, it accounts for 0.005% to 0.01% of all cutaneous tumors. [3], [4] Patient age varies according to different studies, ranging from 21 to 90. [5], [6] It predominantly occurs in elderly people who are more than 60 years old and has a female predominance. [4]
The tumor favors extremities, particularly the feet and legs. [7] The propensity to form multiple cutaneous metastases is an unusual characteristics of EP. [7] It may also associate with visceral metastasis with a fatal outcome. [7] Surgical resection is the mainstay of treatment modality. [8] In line with SCARE criteria, we reported a single case of EP with systematic review of reported cases in literatures. [9]
2. Patient information
A 62-year-old Kurdish male, Presented with a swelling on his left forearm for 10 years, increasing in size in last two months, he was known case of hypertension and underwent inguinal hernia repair 10 years ago.
2.1. Clinical findings
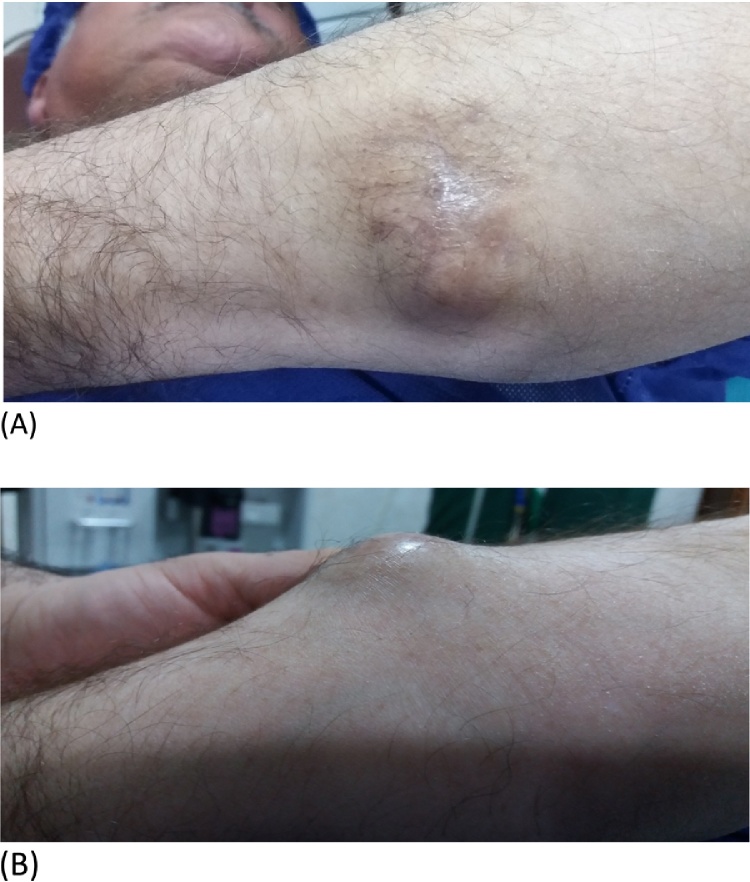
A hard mass on his posteromedial aspect of left mid-forearm, measuring about 3 × 2 centimeters, non-tender and fixed to the skin (Fig. 1).
Fig. 1.
clinical appearance of the swelling. (A) Posterior view. (B) Lateral view.
2.2. Diagnostic assessment
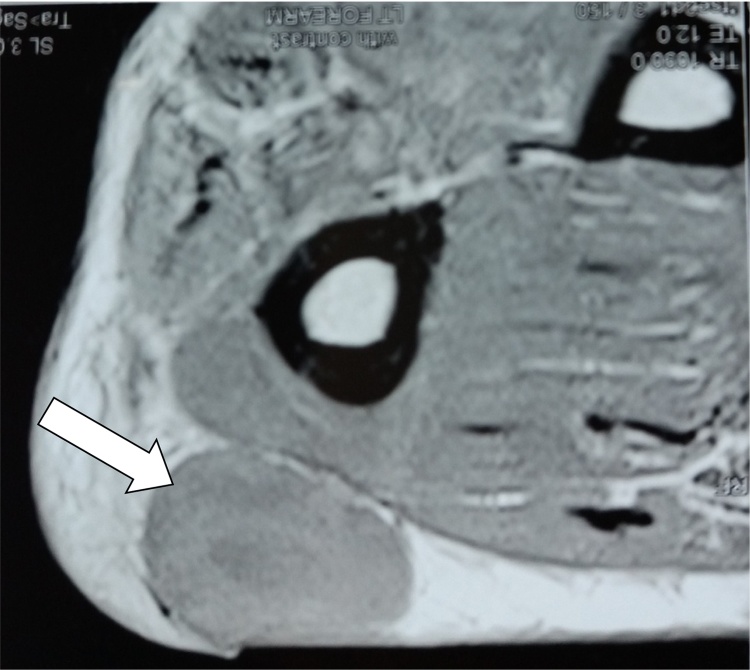
Hematological tests were normal including erythrocyte sedimentation rate (ESR). Doppler ultrasound of the left elbow showed ill defined intramuscular hypoechoic lesion, measuring about 32 × 21 millimeters. Magnetic resonant image showed well defined oval mass within subcutaneous mass fat tissue with mild post-contrast enhancement without evidence of surrounding invasion (Fig. 2). The professional diagnosis of benign cystic lesion was made especially dermoid cyst and lipoma.
Fig. 2.
Cross sectional magnetic resonant image of the lesion showing well defined homogenous mass (white arrow) without invading surrounding tissues.
2.3. Therapeutic intervention
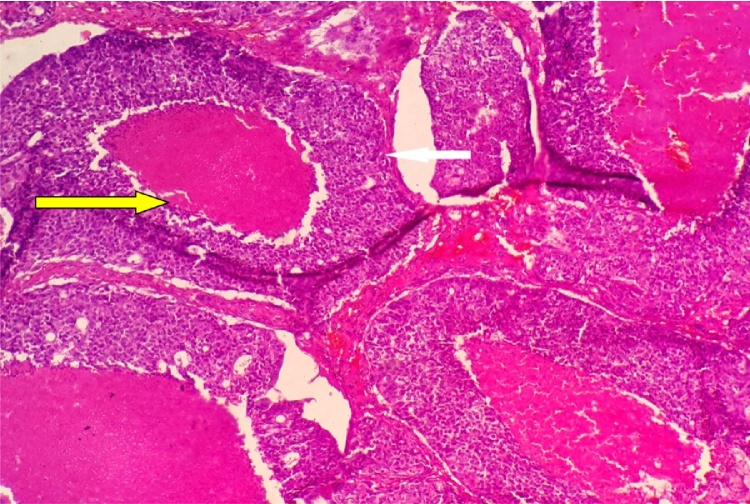
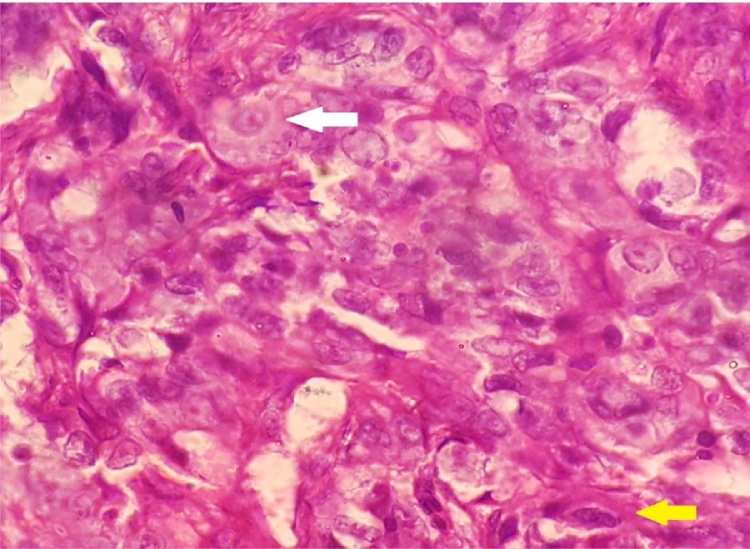
Under local anesthesia, by transverse elliptical incision. Excision of the mass was performed with its cystic wall. Histopathological result showed lobules of tumor cells, composing of 2 patterns. Eosinophilic and clear cells arranging in nodular, nest and solid sheets. The eosinophil cells are polyhedral to fusiform with variable cytoplasm and indistinct cell borders. The nuclei are hyperchromatic, round to oval with indistinct nucleoli. The clear cells are large polyhedral with abundant clear cytoplasm and distinct cell borders. Mitosis was abundant. Extensive central necrosis was found, (Fig. 3, Fig. 4). Immunohistochemistry confirmed EP.
Fig. 3.
Large islands of tumor cells (white arrow) with central necrosis (yellow arrow).
Fig. 4.
Tumor cells demonstrating marked nuclear pleomorphism and prominent nucleoli (white arrow). There are large polyhedral cells with abundant clear cytoplasm (yellow arrow).
2.4. Follow-up and outcome
The patient was referred to oncologist for re-assessment. All body positron emission tomography (PET) scan showed distant metastasis to the chest, cervical lymph nodes and brain. The patient started receiving chemotherapy and radiation therapy to the brain. Two months later, his condition deteriorated and the patient died from respiratory failure.
3. Discussion
EP is a very rare dermatological problem. Since its first description by Pinkus and Mehregan in 1963, about 250 cases have been reported in different language literatures. [10] Among reported cases, 8th decade of life is the ideal age of affection followed by 7th decade (Table 1).[1], [3], [6], [10], [11], [25], [26], [27], [28], [29], [30], [31], [32], [33], [34] EP does not have predilection for specific part of the body. [24] Arslan et al. stated that it tends to involve most frequently in the extremities especially lower limbs, followed by trunk and head while current literature review showed that EP occurs most commonly at the lower limbs (35%) followed by head(24%) and upper limbs (14%) (Table 2). [2], [6], [7], [10], [11], [12], [14], [15], [16], [19], [20], [21], [23], [25], [27], [29], [30], [33], [34], [35] However, the occurrence of EP is not correlated with the areas with highest concentration of hair (palmoplantar region).[18] The current patient complained from EP of the posteromedial aspect of the left forearm. To best of our knowledge, EP has never been reported in this area. It has been reported to involve the upper limb in seven cases (affecting axilla in two patients, shoulders in two cases, upper arm in other three patients and finger in one individual).[6], [10], [14], [16], [27], [34], [35] Although several authors have reported the tendency of the tumor to occur more commonly among female gender or equally affect both genders, [3], [4], [10] the current review showed that 60% of reported cases are male patients. [2], [3], [13], [11], [16], [17], [19], [23], [25], [27], [28], [31], [32] EP occurs as a single mass or nodule in 72% of the cases, ulceration (26%), and as a discharging sinus in 2% of cases. [1], [2], [3], [4], [5], [6], [7], [8], [9], [10], [11], [12], [13], [14], [15], [16], [17], [18], [19], [20], [21], [22], [23], [24], [25], [26], [27], [28], [29], [30], [31], [32], [33], [34], [35], [36] Although the pre-invasive markers and the pathogenesis of EP are not clear, according to some papers, risk factors include exposure of the affected area to trauma, burning, or radiotherapy, immunosuppressive drugs especially after organ transplantation, prolonged exposure to ultraviolet light and AIDS. [10] The gross examination is an important part of the assessment. [24] Pedunculated tumor appears to be less aggressive. Ulceration and multinodularity are among signs of aggressiveness with increased risk of local recurrence and distant metastasis. [24] EP may develop de novo or complicate an eccrine poroma, chronic lymphatic leukaemia, nevus sebaceous and actinic lesions. [35] Some time, a long duration of history is present. This is may be explained by the fact that some Eps arise from a preexisting benign condition especially its benign counterpart, poroma. [35] Robson et al. reported the ratio of malignant transformation from benign poroma to malignant one to be around 18%.[36] Our case presented with 10 year history of a mass in his postero-medial aspect of left forearm without significant symptoms apart from last 2 months which increased in size rapidly. Metastasis is reported to occur in 20% of patients while current review among 36 studies and 61 patients showed that metastasis occur in 26%. The most common affected organ to which EP metastise is lymph nodes (60%) followed by chest (13%), Table 3 shows the involved organs in literatures with their frequency of affection [1], [6], [10], [11], [14], [16], [22], [24], [25], [28], [31], [33], [34]. Our case showed metastasis to lung, cervical lymph nodes and brain. Mortality rate in case of metastasis increases dramatically reaching to 80% in case of distant metastasis and 65% when only lymph nodes are affected. [10], [24] In current case, the patient died 2 months after detection of metastasis by investigations although he was free of symptoms meanwhile. EP cells appear to be more pleomorphic than benign poroid counterpart, with more irregular nuclear shape and size with evident nucleoli and chromatin granules. They show necrosis and invasive growth in the dermis. [24] The malignancy arises from terminal cells of the Intra-epidermal part of the duct of the sweat gland (acrosyringium).[18] It may arise and extend from the epidermis to various depth of the dermis, and sometime the subcutaneous fat is also involved by the disease. [18] Histological characteristics that may have prognostic Importance include the tumor depth, lymphovascular invasion and the number of mitosis. [10] In our case, we did not see vascular invasion, neither radiologically nor surgically, while histopathological examination showed increased mitotic activity. Differential diagnoses include squamous and basal cell carcinomas, amelanotic melanoma, seborrheic keratosis, cutaneous lymphoma,verruca vulgaris, skin metastases of different types of cancer and other diseases such as Paget, Bowen and hydroacanthoma simplex. [10] In our case, we suspected benign cystic lesions like dermoid and lipoma. Regardless of subtypes, cytological diagnosis of dermatological malignancies sometimes is insufficient for choosing main lines of therapy. Histological confirmation and even immunohistochemistry examination is always necessary for a definitive diagnosis. [1] In this case, for the diagnostic and therapeutic purpose, we performed local resection under local anesthesia. The latter was preferred by the patient. Wide local resection of the tumor is the main line of treatment and the cure rate has been reported to be around 70–80%.[3] Clearance of regional lymph nodes is necessary if involved in the pathology, in case of poorly differentiated tumor, and when there is recurrence. [18], [35] Up to date, enough data are not present to recommend the use of adjuvant therapy (both chemotherapy and radiotherapy) in the treatment of EP. Plunkett et al. have observed a clinical and radiological response to chemotherapy in a 45 year old female patient with history of renal transplant with a metastatic EP. [14]
Table 1.
Distribution of reported cases according to their age groups.
| Age group (year) | Number of reported cases/% | References |
|---|---|---|
| 0–20 | 0/0 | |
| 21–30 | 3/5 | [5], [12], [13] |
| 31–40 | 0/0 | |
| 41–50 | 6/11 | [6], [14], [15], [16] |
| 51–60 | 9/16 | [2], [6], [7], [13], [17], [18], [19] |
| 61–70 | 12/21 | [4], [6], [21], [22], [23], [24] |
| 71–80 | 18/32 | [1], [3], [6], [11], [25], [26], [27], [28], [29], [30] |
| 81–90 | 8/14 | [6], [10], [30], [31], [32], [33], [34] |
Table 2.
Reported organ involved by primary EP with their frequency.
| Site | Number of reported cases | References |
|---|---|---|
| Lower limb | 18/35 | [6], [7], [15], [19], [20], [21], [30], [33], [34] |
| head | 12/24 | [2], [6], [11], [12], [23], [25], [29], [35] |
| Upper limb | 7/14 | [6], [10], [14], [16], [27], [34], [35] |
| trunk | 4/8 | [6], [22], [24], [32] |
| abdomen | 4/8 | [4], [5], [6] |
| scrotum | 3/6 | [13], [28] |
| Auricle | 1/2 | [3] |
| Chest wall | 1/2 | [30] |
| Inguinal region | 1/2 | [1] |
Table 3.
Organs to which EP metastize to with their frequency of affection.
EP is a rare but aggressive type of skin disease. It may arise de novo or complicate a benign skin lesion. Early intervention with wide local resection is recommended.
Informed consent
Informed consent was taken from the family for the publication of this report.
Author contribution
Abdulwahid M. Salih: surgeon performing the operation.
F.H. Kakamad: surgeon performing the operation. Drafting the manuscript.
Goran M. Rauf: pathologist examining the specimen and follow up.
Rawand A. Essa, Masrur S.A, Shvan H.M, Rawezh Q.M, Hunar A.H, Dahat A.H and Snur Othman: drafting the manuscript and reviewing the literature.
Ethical approval
Approval has been taken from bioscience center.
Conflict of interest
There is no conflict of interest
Funding
No source to be stated.
Ethical approval
Approval has been taken from bioscience center.
Consent
Consent has been taken.
Guarantor
Fahmi Hussein kakamad.
References
- 1.Kalogeraki A. A cytologic approach of eccrine porocarcinoma. Acta Med. Port. 2013;26(July–August (4)):467–470. [PubMed] [Google Scholar]
- 2.Asghar Porocarcinoma: A Rare Sweat Gland Malignancy. J. Coll. Phys. Surg. Pak. 2009;19(6):389–390. [PubMed] [Google Scholar]
- 3.Chang Eccrine porocarcinoma of the auricle: a case report. Kaohsiung J. Med. Sci. 2009;25(7):401–404. doi: 10.1016/S1607-551X(09)70534-0. [DOI] [PubMed] [Google Scholar]
- 4.Choi A rare case of abdominal porocarcinoma. Arch. Plast. Surg. 2014;26(1):91–93. doi: 10.5999/aps.2014.41.1.91. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Parmar Eccrine porocarcinoma presenting as an abdominal wall mass in apatient with ulcerative colitis—a rare case report. Int. J. Surg. Case Rep. 2016;23:40–43. doi: 10.1016/j.ijscr.2016.03.046. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Mehregan Eccrine adenocarcinoma. Arch. Dermatol. 1983;119:104–114. doi: 10.1001/archderm.119.2.104. [DOI] [PubMed] [Google Scholar]
- 7.Sharathkumar EccrinePorocarcinoma: a case report. J. Clin. Diagn. Res. 2013;7(12):67–296. [Google Scholar]
- 8.Smita EccrinePorocarcinoma of the scalp: a rare case report with review of literature. J. Clin. Diagn. Res. 2016;5(January (1)):ED15–ED16. doi: 10.7860/JCDR/2016/16083.7149. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Agha The SCARE statement: consensus-based surgical case report guidelines. Int. J. Surg. 2016 doi: 10.1016/j.ijsu.2016.08.014. (article in press) [DOI] [PubMed] [Google Scholar]
- 10.Arslan Eccrineporocarcinoma: a case report and literature review. J. Clin. Exp. Invest. 2013;4(3):370–373. [Google Scholar]
- 11.Zeidan Treatment of eccrineporocarcinoma with metastasis to the parotid gland using intensity-modulated radiation therapy: a case report. J. Med. Case Rep. 2010;4(1):15. doi: 10.1186/1752-1947-4-147. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Masamatti Eccrine porocarcinoma of the scalp: a rare case report with review of literature. J. Clin. Diagn. Res. 2016;10(January (1)):15–16. doi: 10.7860/JCDR/2016/16083.7149. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Han Eccrineporoma and porocarcinoma on the same unusual location: report on two cases. An. Bras. Dermatol. 2015;90(3 Suppl. (1)):S69–S72. doi: 10.1590/abd1806-4841.20153415. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Plunkett Metastatic eccrineporocarcinoma: response to docetaxel (Taxotere) chemotherapy. Annu. Oncol. 2001;12:411–414. doi: 10.1023/a:1011196615177. [DOI] [PubMed] [Google Scholar]
- 15.Manimaran Eccrine porocarcinoma associated with an eccrine poroma. Online J. Health Allied SCS. 2014;13(2):1–4. [Google Scholar]
- 16.Devi Primary axillary porocarcinoma: a rare cutaneous tumour. J. Clin. Diagn. Res. 2016;10(2):4–6. doi: 10.7860/JCDR/2016/15278.7171. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Pal Eccrine porocarcinoma of scalp: a rare case report. Iran. J. Pathol. 2015;10(1):65–68. [PMC free article] [PubMed] [Google Scholar]
- 18.Huet Metastasizing eccrine porocarcinoma: report of a case and review of the literature. J. Am. Acad. Dermatol. 1996;35(5):861–864. doi: 10.1016/s0190-9622(96)90105-x. [DOI] [PubMed] [Google Scholar]
- 19.Ishida Letter to editor pigmented porocarcinoma: a case report with review of the literature. Int. J. Clin. Exp. Pathol. 2013;6(12):3033–3035. [PMC free article] [PubMed] [Google Scholar]
- 20.Walsh A case of eccrineporocarcinoma. J. R. Soc. Med. 1990;83(8):529–530. doi: 10.1177/014107689008300819. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Vandeweyer Eccrineporocarcinoma: a case report. Acta Chir. Belg. 2006;106(1):121–123. doi: 10.1080/00015458.2006.11679853. [DOI] [PubMed] [Google Scholar]
- 22.Li Keratin profiles may differ between intraepidermal and intradermal invasive eccrineporocarcinoma. Clin. Nucl. Med. 2007;32:743–745. [Google Scholar]
- 23.Gerber Eccrine porocarcinoma of the head: an important differential diagnosis in the elderly patient. Dermatology. 2008;216:229–233. doi: 10.1159/000112931. [DOI] [PubMed] [Google Scholar]
- 24.Blandamura Porocarcinoma detected by fine needle aspiration biopsy of a node metastasis a case report. ActaCytologica. 1997;41:4. doi: 10.1159/000333525. [DOI] [PubMed] [Google Scholar]
- 25.Ritter Intracranial extension of an eccrineporocarcinoma: case report and review of the literature. J. Neurosurg. 1999;90(1):138–140. doi: 10.3171/jns.1999.90.1.0138. [DOI] [PubMed] [Google Scholar]
- 26.Lloyd Eccrineporocarcinoma: a case report and review of the literature. Can. J. Plast. Surg. 2003;11(3):153–156. doi: 10.1177/229255030301100304. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Kurokawa Keratin profiles may differ between intraepidermal and intradermal invasive eccrineporocarcinoma. Oncol. Rep. 2006;16(3):473–478. [PubMed] [Google Scholar]
- 28.Eng Porocarcinoma associated with extramammary paget's disease. J. Cutan. Pathol. 1974;1:249–255. doi: 10.1111/j.1600-0560.1974.tb00635.x. [DOI] [PubMed] [Google Scholar]
- 29.Fung Eccrine porocarcinoma of the face. Hong Kong Dermatol. Venereol. 1999;7(2):72–74. [Google Scholar]
- 30.Goh Sarcomatoid eccrine porocarcinoma: report of two cases and a review of the literature. J. Cutan. Pathol. 2007;34:55–60. doi: 10.1111/j.1600-0560.2006.00556.x. [DOI] [PubMed] [Google Scholar]
- 31.Bhat Primary Eccrine Porocarcinoma of the finger with transit forearm and axillary metastasis. Ann. Plast. Surg. 2011;66(4):344–346. doi: 10.1097/SAP.0b013e3181e35c8d. [DOI] [PubMed] [Google Scholar]
- 32.Kazakov Sebaceous differentiation in poroid neoplasms: report of 11 cases, including a case of metaplastic carcinoma associated with apocrine poroma (sarcomatoid apocrine porocarcinoma) Am. J. Dermatopathol. 2008;30(1):21–26. doi: 10.1097/DAD.0b013e31815f2ae3. [DOI] [PubMed] [Google Scholar]
- 33.Suzaki Dermoscopic features of eccrineporocarcinoma arising from hidroacanthoma simplex. Dermatol. Res. Pract. 2010;1(1):1–4. doi: 10.1155/2010/192371. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Pinkus Epidermotropic eccrine carcinoma. a case combining features of eccrine poroma and paget's dermatosis. Arch. Dermatol. 1963;88:597–606. doi: 10.1001/archderm.1963.01590230105015. [DOI] [PubMed] [Google Scholar]
- 35.Ferri Metastasizing eccrine porocarcinoma of the nose: case- report with immunohistochemical study and review of the literature. Internet J. Otorhinolaryngol. 2007;7(2):1–6. [Google Scholar]
- 36.Robson Eccrine porocarcinoma (malignant eccrine poroma): a clinicopathologic study of 69 cases. Am. J. Surg. Pathol. 2001;25:710–720. doi: 10.1097/00000478-200106000-00002. [DOI] [PubMed] [Google Scholar]