Abstract
Objectives
Multimorbidity is prevalent, and knowledge regarding its aetiology is limited. The general pathogenic impact of adverse life experiences, comprising a wide-ranging typology, is well documented and coherent with the concept allostatic overload (the long-term impact of stress on human physiology) and the notion embodiment (the conversion of sociocultural and environmental influences into physiological characteristics). Less is known about the medical relevance of subtle distress or unease. The study aim was to prospectively explore the associations between existential unease (coined as a meta-term for the included items) and multimorbidity.
Setting
Our data are derived from an unselected Norwegian population, the Nord-Trøndelag Health Study, phases 2 (1995–1997) and 3 (2006–2008), with a mean of 11 years follow-up.
Participants
The analysis includes 20 365 individuals aged 20–59 years who participated in both phases and was classified without multimorbidity (with 0–1 disease) at baseline.
Methods
From HUNT2, we selected 11 items indicating ‘unease’ in the realms of self-esteem, well-being, sense of coherence and social relationships. Poisson regressions were used to generate relative risk (RR) of developing multimorbidity, according to the respondents' ease/unease profile.
Results
A total of 6277 (30.8%) participants developed multimorbidity. They were older, more likely to be women, smokers and with lower education. 10 of the 11 ‘unease’ items were significantly related to the development of multimorbidity. The items ‘poor self-rated health’ and ‘feeling dissatisfied with life’ exhibited the highest RR, 1.55 and 1.44, respectively (95% CI 1.44 to 1.66 and 1.21 to 1.71). The prevalence of multimorbidity increased with the number of ‘unease’ factors, from 26.7% for no factor to 49.2% for 6 or more.
Conclusions
In this prospective study, ‘existential unease’ was associated with the development of multimorbidity in a dose–response manner. The finding indicates that existential unease increases people's vulnerability to disease, concordant with current literature regarding increased allostatic load.
Keywords: Multimorbidity, Existential unease, Embodiment, Allostatic overload, Stress
Strength and limitations of this study.
This large, prospective study explores subtle aetiological factors of multimorbidity, a fairly new area of investigation.
The study shows that relatively subtle, existentially demanding life circumstances are associated with the development of multimorbidity.
The data come from a large, homogenous and relatively affluent population. Finding effect of subtle unease on future health even in this population highlights its importance.
The basic science concept allostatic load is key to our hypothesis. We described the participants' allostatic load at the level of tertiary outcomes (established diseases/conditions) in accordance with the literature. Our findings suggest that a subjective experience of existential unease is associated with allostatic load in a long-term perspective.
The findings have relevance for general practice/primary healthcare and raise the question whether attentive, person-centred dialogues can contribute to treatment and prevention of complex disease within the frame of an established doctor–patient relationship.
Introduction
In recent years, there has been increasing interest in the phenomenon multimorbidity, that is, the co-occurrence of two or more chronic diseases in the same individual.1 2 Initially, multimorbidity research tended to focus on older patients and prevalence figures. However, the scope has gradually widened, documenting significant prevalence of multimorbidity also among younger age-groups and, overall, an uneven distribution along social gradients.3–5
The origins of multimorbidity are evidently multifactorial and complex,6 and knowledge as to the true sources is quite limited. We regard the concept allostatic load7 as a central key to understanding why some individuals develop a host of complex, common diseases, while others do not.5 8 9 The model conceptualises how demanding life circumstances (physical and mental) affect the organism over time, and how long-standing unbuffered stress might eventually overtax the body's capacity for adaptation. The result is a tendency to physiological disruption with increased susceptibility to disease.10 11 Allostasis thus depicts the physiology of a process termed embodiment. The notion of embodiment, derived from a phenomenology of the body,12 13 allows to account for how sociocultural experiences and other environmental influences translate into physiological and anthropometric characteristics of the body, whereby clearly relevant for epidemiological research.8 14 15 There is currently no consensus regarding measurement of allostatic load. However, an authoritative researcher in the field characterises three types of allostatic load parameters.11 Well-known risk factors, such as hypertension or hyperlipidaemia, are classified as secondary mediators, while diagnosed diseases are classified as tertiary allostatic outcomes. Consequently, disease development in general and multimorbidity in particular have relevance as indicators of allostatic overload.11
From an epidemiological perspective, the pathogenic impact of traumatic experiences involving neglect and integrity violations is well documented in the somatic and mental domains. There is also clear evidence of a social gradient in health, reflecting how environmental and existential stressors and demands tend to accumulate with increasing social deprivation.16–21 Furthermore, it is becoming increasingly clear how subtle yet long-standing challenges impact on the human physiology and predispose to disease.22–25 Likewise, it is acknowledged that it is subjective experience, not objectively quantifiable events, that becomes biologically inscribed.9 26 This implies that every person perceives and interprets himself or herself, and relations with other people within a socioculturally framed system of values. As practitioners and researchers, we see this as relevant in the clinical setting, but recognise that it is challenging to explore the topic in a scientifically valid manner. Our main hypothesis is that over time, existential Un-ease in the above-mentioned realms might contribute substantially to allostatic load and thereby to the development of complex, medical dis-ease. The present study was designed to further test the plausibility of this argument.
For this purpose, we analysed data from the Norwegian HUNT study. From their comprehensive questionnaire, we identified questions which we suppose to shed light on the respondents' evaluation of self, experienced purpose in life, well-being, and significant, social relations. As noted by the US Centres of Disease Control and Prevention,27 the scientific literature contains a wide range of concepts related to the notion of health-related quality of life, such as well-being, flourishing, life satisfaction and happiness. We have so far not found an established term that accommodates our clinically rooted research question and the applied data set.
We therefore decided to introduce a new term, existential unease, to describe lack of self-esteem, well-being, meaning and/or social interrelatedness. The word ‘existential’ points to existential philosopher Maurice Merleau-Ponty who most explicitly linked experiences to subjectivity and the body by emphasising that human beings by necessity experience the world by means of their bodies,12 thus providing a framework of relevance also for medical research in general19 and epidemiology in particular.14 It is not our primary intention to develop a new tool for research or clinical practice. Our main interest is to contribute some new perspectives on the phenomenon embodiment, particularly with regard to the aetiology of complex disease and multimorbidity.
To sum up, the aim of this study was to prospectively explore associations between existential unease, on the one hand, and indications of general biological disruption, expressed through an increased risk of developing multimorbidity, on the other.
Study population and methods
Our data are derived from the HUNT study, a renowned population-based study carried out in Nord-Trøndelag County in Norway. It has, to date, had three phases. The second phase, HUNT2, was carried out in 1995–1997, whereas HUNT3 took place in 2006–2008. All adults aged over 20 years and receding in the county were invited to participate. In total, 65 237 persons (69.5% of the population) took part in HUNT2 and 50 807 (54.1%) took part in HUNT3. In total, 37 071 persons (73% of the HUNT3 population) took part in both phases.28 Participants in the HUNT study have been considered fairly representative of the Norwegian population.29 However, being a rural area, educational levels and mean income are somewhat lower, and the population is more homogenous than in urban areas, in terms of ethnicity and social gradients.30
The HUNT data were collected by means of questionnaires, physical examinations and blood samples. For this prospective study, we included participants who took part in HUNT2 and HUNT3. We identified individuals who were 20–59 years at baseline and reported 0–1 chronic disease (no multimorbidity), in total 20 365 participants. We subsequently compared individuals reporting multimorbidity in HUNT3 with those who did not (see online supplementary figure S1) to explore possible differences between the groups. Participants aged 60 years or older at baseline were excluded from analysis as the prevalence of multimorbidity increases steeply in older age.5
bmjopen-2016-012602supp.pdf (493.8KB, pdf)
Selection of items reflecting existential unease
The questionnaires integrated in the HUNT2 survey were informed by contemporary theoretical frameworks from various domains, especially sociologist Pierre Bourdieu's theories concerning social and cultural capital,31–33 sociologist Aron Antonovsky's concept Sense of Coherence34 35 and the psychological notions of self-esteem and well-being.36–38 As previously explained, we purposefully selected questions which we considered particularly indicative of an existentially, and thereby also a biologically, demanding lifeworld.12 14
In total, 11 items were included in our analysis. Together they cover thematically related, but nevertheless, distinct perspectives. Two of the items, ‘being satisfied with life’ and ‘having a positive opinion of oneself’, stem from the Rosenberg Self-esteem questionnaire, validated and predominantly applied in sociological studies.36 38 The remaining nine were single-item questions.
The list of questions is presented in online supplementary appendix 1 as they appeared in the HUNT2 questionnaire. The response options were then rearranged to have the reference group of the least stressful or most positive outcome to be presented at the top. For further analyses, response options were collapsed and binary variables were constructed when relevant. Three of the 11 items were originally binary with yes/no answers, but for the others, the two most unfavourable response options were combined to indicate existential unease. Finally, a summation of the binary variables was used as to indicate more distress or unease, and thus, hypothetically, a higher allostatic load.
Assessment of multimorbidity
Multimorbidity was defined according to international consensus as two or more coinciding chronic diseases within the same individual.2 Seventeen chronic conditions were accessible by the same definitions through the questionnaires from HUNT2 and HUNT3. Eleven of these were self-reported in response to the question “have you had or do you have the following medical condition” or “has a doctor said that you have the following condition?” The definition of the remaining six conditions has previously been described in more detail.5 Online supplementary appendix 2 shows a list of the included conditions.
As supplementary analyses, we evaluated adult existential unease with regard to difficult childhood, to link the present study to our previous work on difficult childhood, allostatic load and adult multimorbidity (see online supplementary appendix 3 and figure S2).9
Missing data
For estimations of multimorbidity, as well as for the summation of binary unease factors, missing data were defined as the absence of the disease or unease item in question. In statistical analyses of relative risk (RR), respondents with missing data on each confounder were defined as a specific group.
Statistical analyses
Descriptive analyses were stratified according to the development of multimorbidity between the two phases of the study. The categorical variables were expressed as frequencies with percentages and continuous variables as means with SDs.
Poisson logistic regression for prospective data was used to estimate the RR with 95% CI of multimorbidity associated with each of the different variables expressing unease. The variables were analysed independently. All associations were adjusted for age (continuous) and gender (woman and man) in model 1. In model 2, we also included smoking (no or yes to ‘daily use of cigarettes, cigars and/or pipes'), education (primary, secondary or university) and physical activity (no activity, <3 hours of light activity and no hard activity, >3 hours of light and/or <1 hour of hard activity and 1 hour or more of hard activity per week). To address possible confounding by current undiagnosed depression at baseline, we conducted additional analyses adjusting for indication of current depressive symptoms, defined as eight or more points for depression on the Hospital Anxiety and Depression Scale (HADS) and presented as model 3. Assessment was made for possible multicollinearity between the unease variables, which appeared not to occur.
The same method for Poisson regression was used in the assessment of RR for binary variables, as well as for the variable summing all the binary factors, adjusting for possible confounding by age, gender, smoking, physical activity and education.
The sum of binary variables for existential unease was then grouped as 0, 1–2, 3–4 and 5+ and assessed with regard to developing increasing number of diseases 11 years later as well as with self-reported experience of childhood.
SPSS statistical program (V.22) was used for all analyses.
The article was adjusted to STROBE recommendations for cohort studies in epidemiology.
Results
Prospective data on 20 365 individuals who participated in HUNT2 and HUNT3 were analysed with respect to the development of multimorbidity between the surveys (table 1). In total, 6 277 persons (30.8%) acquired multimorbidity during the 11 years. They were on average older, more likely to be women and smokers, less physically active and had lower education.
Table 1.
Baseline characteristics of participants aged 20–59 years in HUNT2 according to the development of multimorbidity over a period of 11 years*
| Total | Multimorbidity |
||
|---|---|---|---|
| No | Yes | ||
| n=20 365 | n=14 088 | n=6 277 | |
| Mean age | 40.62 (±10.0) | 39.45 (±9.94) | 43.24 (±9.62) |
| Gender | |||
| Women | 10 938 (53.7) | 7 201 (51.1) | 3 737 (59.5) |
| Men | 9 427 (46.3) | 6 887 (48.9) | 2 540 (40.5) |
| Smoking | |||
| No | 13 272 (65.2) | 9 450 (67.1) | 3 822 (60.9) |
| Yes | 3 326 (16.3) | 2 142 (15.2) | 1 184 (18.9) |
| Physical activity | |||
| None | 1 018 (5.0) | 705 (5.0) | 313 (5.0) |
| Low | 5 388 (26.5) | 3 494 (24.8) | 1 894 (30.2) |
| Medium | 6 669 (32.7) | 4 588 (32.6) | 2 081 (33.2) |
| High | 6 747 (33.1) | 4 979 (35.3) | 1 768 (28.2) |
| Education | |||
| Primary | 3 900 (19.2) | 2 340 (16.6) | 1 560 (24.9) |
| Secondary | 10 543 (51.8) | 7 390 (52.5) | 3 153 (50.2) |
| University | 5 735 (28.2) | 4 235 (30.1) | 1 499 (23.9) |
*Percentages and SDs within brackets as appropriate.
Table 2 summarises the RR of developing multimorbidity associated with each of the 11 items indicating existential unease. The factors with the strongest association are ‘being dissatisfied with life’, ‘having a negative opinion of self’, ‘having financial worries’, ‘not feeling calm and good’ and ‘poor self-rated health’, all having RRs above 1.4 for the subgroups indicating most distress in model 2. Adjusting for current depressive symptoms according to the HAD scale attenuated the RR slightly, especially for the subgroups indicating most distress as shown in model 3.
Table 2.
RR of developing multimorbidity within 11 years with regard to different items indicating existential unease in HUNT2, adjusted for common confounders
| Variable | Multimorbidity |
Model 1* | Model 2† |
Model 3‡ |
|||
|---|---|---|---|---|---|---|---|
| No | Yes | RR | RR | 95% CI | RR | 95% CI | |
| Life satisfaction | |||||||
| Satisfied | 7 489 | 2 781 | 1.0 | 1.0 | Ref. | 1.0 | Ref. |
| Somewhat satisfied | 5 060 | 2 473 | 1.18 | 1.16 | 1.10 to 1.23 | 1.16 | 1.10 to 1.23 |
| Neither nor | 1 236 | 836 | 1.47 | 1.44 | 1.33 to 1.56 | 1.40 | 1.29 to 1.52 |
| Somewhat dissatisfied | 112 | 90 | 1.66 | 1.65 | 1.33 to 2.03 | 1.56 | 1.26 to 1.90 |
| Dissatisfied | 49 | 39 | 1.60 | 1.51 | 1.10 to 2.08 | 1.39 | 1.00 to 0.192 |
| Positive self-opinion | |||||||
| Strongly agree | 2 253 | 753 | 1.0 | 1.0 | Ref. | 1.0 | Ref. |
| Agree | 9 012 | 4134 | 1.13 | 1.12 | 1.03 to 1.21 | 1.11 | 1.02 to 1.20 |
| Disagree | 658 | 444 | 1.43 | 1.38 | 1.23 to 1.56 | 1.30 | 1.15 to 1.47 |
| Strongly disagree | 30 | 22 | 1.56 | 1.49 | 0.97 to 2.27 | 1.37 | 0.89 to 2.09 |
| Living a meaningful life | |||||||
| Yes | 10 444 | 4 518 | 1.0 | 1.0 | Ref. | 1.0 | Ref. |
| No | 1 391 | 781 | 1.23 | 1.21 | 1.12 to 1.30 | 1.15 | 1.06 to 1.25 |
| Enjoying work | |||||||
| A great deal | 3 857 | 1 626 | 1.0 | 1.0 | Ref. | 1.0 | Ref. |
| A fair amount | 6 726 | 3 066 | 1.03 | 1.03 | 0.97 to 1.09 | 1.02 | 0.95 to 1.08 |
| Not much | 432 | 240 | 1.23 | 1.21 | 1.05 to 1.38 | 1.16 | 1.01 to 1.33 |
| Not at all | 39 | 20 | 1.25 | 1.23 | 0.79 to 1.91 | 1.15 | 0.73 to 1.79 |
| Financial worries | |||||||
| No, never | 8 786 | 3 723 | 1.0 | 1.0 | Ref. | 1.0 | Ref. |
| Yes, though seldom | 1 966 | 908 | 1.21 | 1.18 | 1.10 to 1.27 | 1.18 | 1.10 to 1.27 |
| Yes, sometimes | 1 016 | 580 | 1.36 | 1.30 | 1.19 to 1.42 | 1.30 | 1.19 to 1.42 |
| Yes, often | 254 | 184 | 1.58 | 1.50 | 1.29 to 1.74 | 1.46 | 1.25 to 1.70 |
| Having enough friends | |||||||
| Yes | 10 002 | 4 424 | 1.0 | 1.0 | Ref. | 1.0 | Ref. |
| No | 1 973 | 958 | 1.12 | 1.13 | 1.06 to 1.22 | 1.10 | 1.03 to 1.18 |
| Distrusting neighbours | |||||||
| Strongly disagree | 4 795 | 1 941 | 1.0 | 1.0 | Ref. | 1.0 | Ref. |
| Somewhat disagree | 3 511 | 1 491 | 1.09 | 1.08 | 1.01 to 1.15 | 1.07 | 1.00 to 1.15 |
| Not sure | 2 047 | 1 057 | 1.22 | 1.19 | 1.10 to 1.28 | 1.17 | 1.09 to 1.27 |
| Somewhat agree | 1 245 | 650 | 1.19 | 1.14 | 1.04 to 1.25 | 1.13 | 1.03 to 1.23 |
| Strongly agree | 322 | 202 | 1.21 | 1.15 | 0.99 to 1.33 | 1.13 | 0.98 to 1.32 |
| Boiling with anger | |||||||
| Almost never | 5 237 | 2 239 | 1.0 | 1.0 | Ref. | 1.0 | Ref. |
| Sometimes | 5 571 | 2 580 | 1.05 | 1.03 | 0.97 to 1.09 | 1.02 | 0.96 to 1.08 |
| Quite often | 713 | 345 | 1.14 | 1.13 | 1.01 to 1.27 | 1.11 | 0.99 to 1.24 |
| Almost always | 267 | 139 | 1.14 | 1.10 | 0.93 to 1.31 | 1.09 | 0.92 to 1.30 |
| Feel calm and good | |||||||
| Almost all the time | 5 877 | 2 325 | 1.0 | 1.0 | Ref. | 1.0 | Ref. |
| Often | 4 793 | 2 184 | 1.10 | 1.09 | 1.03 to 1.16 | 1.09 | 1.03 to 1.15 |
| Sometimes | 1 352 | 881 | 1.39 | 1.36 | 1.26 to 1.47 | 1.3 | 1.20 to 1.41 |
| Never | 47 | 38 | 1.71 | 1.67 | 1.21 to 2.30 | 1.47 | 1.06 to 2.05 |
| Sleeping problems affecting work | |||||||
| No | 11 223 | 4 831 | 1.0 | 1.0 | Ref. | 1.0 | Ref. |
| Yes | 770 | 556 | 1.39 | 1.39 | 1.27 to 1.51 | 1.34 | 1.22 to 1.46 |
| Self-rated health | |||||||
| Very good | 4309 | 1037 | 1.0 | 1.0 | Ref. | 1.0 | Ref. |
| Good | 8782 | 4279 | 1.56 | 1.51 | 1.41 to 1.62 | 1.51 | 1.41 to 1.62 |
| Not so good | 881 | 886 | 2.26 | 2.16 | 1.97 to 2.37 | 2.12 | 1.93 to 2.33 |
| Poor | 25 | 26 | 2.34 | 2.24 | 1.52 to 3.31 | 2.23 | 1.50 to 3.23 |
*Adjusted for age and gender.
†Adjusted for age, gender, smoking, physical activity and education.
‡Adjusted for same as model 2 and current depressive symptoms.
RR, relative risk.
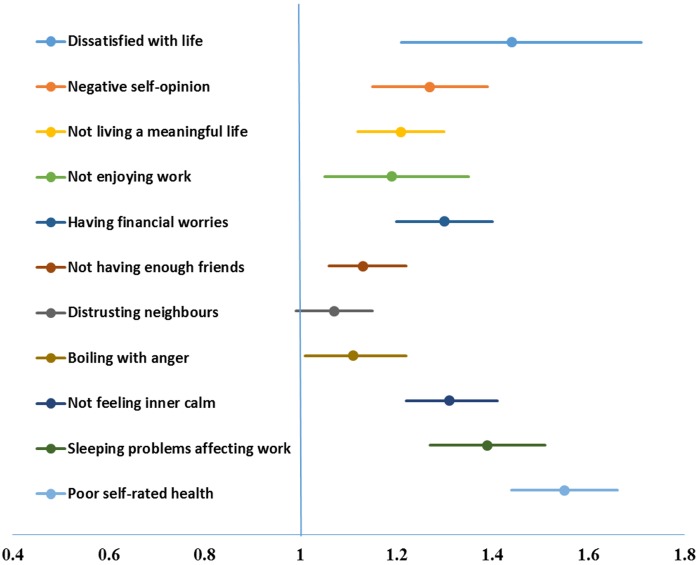
The RRs changed slightly after constructing binary factors from the unease items (see figure 1). For the binary model, ‘being dissatisfied with life’, ‘poor self-rated health’, ‘having sleeping problems affecting work’, ‘not feeling calm and good’ and ‘having financial worries’, all had a RR above 1.3. When assessing according to gender, the results were quite similar, except for ‘not having enough friends’ which was a stronger predictor for women and ‘boiling with anger but not showing it’ which was a stronger predictor for men.
Figure 1.
RR of developing multimorbidity within 11 years with regard to different binary factors indicating existential unease in HUNT2, adjusted for possible confounders. RR, relative risk.
We then evaluated the effect of increasing numbers of unease factors in relation to multimorbidity (figure 2). There we found a dose–response association in RR from having one factor, RR being 1.18 (95% CI 1.11 to 1.25) up to RR 1.81 (95% CI 1.50 to 2.18) for six or more, the prevalence of multimorbidity being 26.7% for those with zero factors at baseline and linearly increasing up to 49.2% for those with six or more. Figure 3 shows that those with no unease factors are more likely to remain free from multimorbidity after 11 years of follow-up, compared to those reporting unease. With an increasing number of unease factors, the prevalence of 2, 3 or 4+ diseases at follow-up becomes higher, with 2.8% among those with no unease factor having 4+ diseases, compared to 8.8% among those with five or more unease factors.
Figure 2.
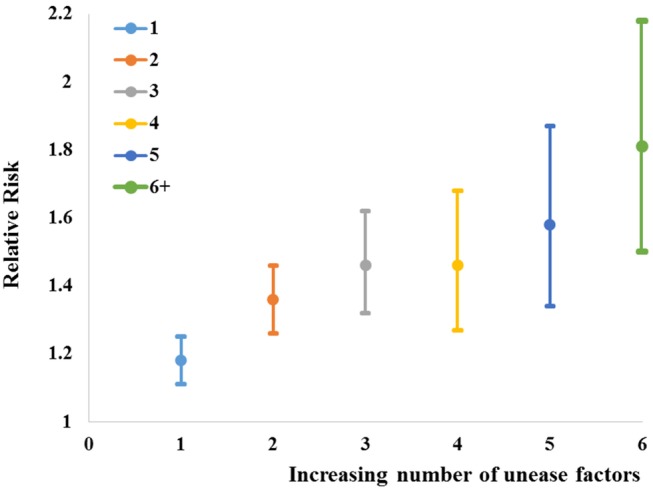
RR of developing multimorbidity within 11 years according to an increasing number of factors indicating existential unease in HUNT2, adjusted for possible confounders and with zero factors as reference. RR, relative risk.
Figure 3.
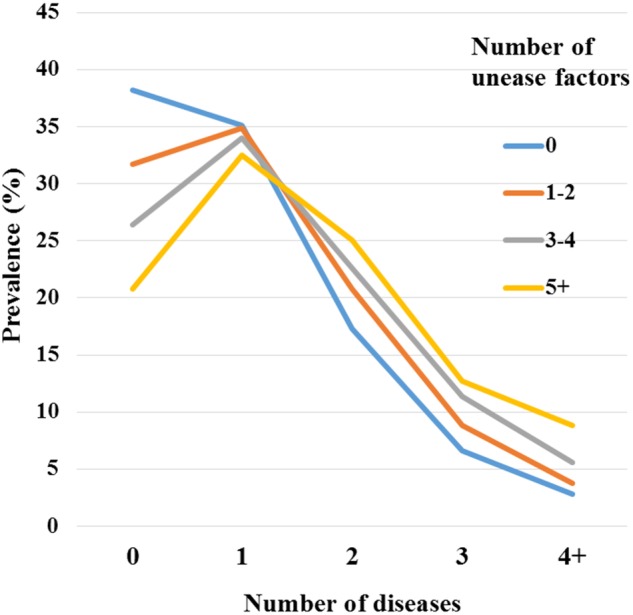
Prevalence of different numbers of diseases in HUNT3 with regard to an increasing number of factors indicating existential unease in HUNT2. RR, relative risk.
Finally, we looked at the number of unease factors in light of self-reported childhood experiences (see online supplementary figure S2 with comments).
Discussion
In this comprehensive population-based study, baseline indications of what we conceptualised as ‘existential unease’ were associated with the risk of developing multimorbidity 11 years later. The increase in RR with an increasing number of unease indicators suggests something similar of a dose–response effect as more existential domains become involved. The findings support our initial hypothesis that existential unease might contribute to allostatic load and thereby increase the susceptibility to disease in a life-course perspective.
The questions used in our study were originally based on the sociological and psychological theories (ie, sense of coherence, social capital, self-esteem and well-being, as previously mentioned), which were from the beginning theoretically associated with the concept of health. We will not open a discussion pertaining to the medical relevance of each particular theory or concept as it was originally formulated, but highlight that recent research from a variety of sources sheds light on their biological relevance. Our findings are, for instance, in concordance with studies of the pathogenic impact of perseverative cognition, ruminations and worries.39 Correspondingly, low self-esteem,40 unfairness,41 lack of well-being,25 42 work dissatisfaction,43 loneliness,44 lack of social relationships,45 subjective social–evaluative threat46 and anger47 have been related to impaired health. A perceived lack of purpose in life has recently been connected to allostatic load,48 49 as has compromised sleep quality.50–52
The strong association shown between poor self-rated health and multimorbidity in our study is concordant with extensive literature on self-rated health in connection to disease development and mortality, where it has been shown to be a powerful independent risk factor.53 However, the strong association shown for many of the other items, such as ‘dissatisfaction with life’, ‘negative self-opinion’, ‘financial worries’ and ‘lack of inner calm’, gives a wider view of how different aspects of our existence or life world can significantly affect future health.
With regard to the included survey questions, it is not evident to what extent they all represent precursors of chronically impaired biological function, as some of them might tap into an early pathogenic process not yet manifested as clinical disease. Recent evidence has suggested a relationship between self-rated health and allostatic load.53 54 In other words, a subjective perception of poor health might develop concomitantly with, and not prior to, high allostatic load. The same might, to a certain extent, pertain to impaired sleep, but according to our clinical experience and in line with existing evidence55 we also see sleep to be a relevant indicator of primary unease. Although the exact, causal contribution of each individual ‘unease’ factor cannot be fully determined, the clinical relevance of considering such factors is likely to persist.
Our finding of a dose–response increase in RR of multimorbidity, as well as increasing prevalence of higher number of diseases, as the number of existential unease factors accumulates, is interesting in light of the results of the ACE study,17 which found a linear increase in disease prevalence with an increasing number of adverse experience categories. In both cases, the notion of dose refers to an increasing number of adversity (or unease) types, not the intensity or frequency of any one exposure. Our supplementary analysis adds to the picture of causal relations, as we found that childhood difficulties are related to existential unease (see online supplementary figure S2 with comments). In both instances, it is likely that allostatic load, and eventually the susceptibility to complex disease, increases with the number or types of adversity or unease involved.
The demographic difference between the groups developing multimorbidity and remaining healthy in our study is in line with current literature.1 3 Multimorbidity is generally more prevalent in older populations and lower socioeconomic groups, and shows a gendered pattern with higher prevalence in women.1 3 However, in our study, the impact of unease items on disease development did not differ between genders. The almost equal effect suggests that although the impact of specific types of adversities or distress might be gendered, experiencing unease as such might undermine health in men and women.
Another interesting finding in our study was the small changes in RRs for multimorbidity development after adjusting for confounders. Adjusting for physical activity, smoking and educational level attenuated the findings only slightly. The same was the case when adjusting for current depressive symptoms. This concords with literature showing that current depressed mood might not be a confounder but a mediator when evaluating subjective experience.56 In our study, however, the effect of these factors appears to be weak.
Strength and limitations of the empirical analysis
The main strength of our analysis lies in the generally high quality of the HUNT database.30 The fact that the HUNT population is ethnically quite homogenous and relatively affluent, with good and equitable access to primary healthcare,29 is also a strength, as it lowers the potential for confounding by socioeconomic factors not fully accounted for in the analysis. However, as the HUNT study was not designed with the present study in mind, some limitations apply. The 17 diagnoses available for assessing self-reported multimorbidity were fewer than would have been ideal for a comprehensive assessment. However, a count of 12 or more chronic conditions should lead to a fair evaluation of multimorbidity.1 A similar problem arose regarding the definition of the phenomenon we termed ‘existential unease’. This category is not based on a validated battery of questions, but on a purposeful collection of items which we deemed particularly relevant on the basis of clinical experience and existing evidence, allowing for reflection on empirical data in light of theoretical or experiential preknowledge. This might represent a methodological weakness, but from the perspective of innovation, it can be seen as a strength. Our approach sheds new light on the biological relevance of various established psycho-social concepts and theories and thereby might contribute to increased appreciation of the broad relevance of the epidemiological concept embodiment. Another potential methodological weakness is selection bias occurring between the two survey phases. A comparison between participants and non-participants in HUNT3 showed that the latter were older, weaker and with more morbidity.28 57 It is possible that some of the individuals who experienced substantial worsening of their health between the two phases were lost to follow-up. This might imply underestimation of the multimorbidity prevalence in HUNT3.
Conclusions and implications
Based on data from an unselected, general Norwegian population, the present prospective study demonstrates an intriguing connection between subtle indicators of existential unease and the development of multimorbidity later in adult life. The RR of multimorbidity rose as the number of statements reflecting unease increased. The findings are concordant with an increasing body of literature describing how distressing challenges tend to affect the human physiology by rising allostatic load, whereby undermining health through embodiment of the ‘wear and tear’7 of a burdening everyday life.
From the perspective of primary care, our findings highlight the importance of an encompassing, person-centred approach, not the least in the face of complex disease and multimorbidity.58 59 Subjective experiences pertaining to the self, one's life project and relationships with other people apparently matter, in a literal sense. As we conclude so, it is, however, not our intention to medicalise every aspect of the human lifeworld and suggest that human happiness should be subjected to systematic, medical surveillance.60 What we hope to contribute to is a more comprehensive medical understanding that does justice to the human nature.61 This is ultimately a fundamental prerequisite for good healthcare.
Acknowledgments
The Nord-Trøndelag Health Study (the HUNT study) is a collaboration between the HUNT Research Centre (Faculty of Medicine, Norwegian University of Science and Technology NTNU), Nord-Trøndelag County Council, Central Norway Health Authority and the Norwegian Institute of Public Health. The authors thank the HUNT Research Centre for contributing data and Steinar Krokstad for assistance regarding background information on the HUNT study.
Footnotes
Contributors: The theoretical background and research question was developed by MOT, LG, JAS and ALK. Statistical analyses were performed by MOT, JAS, HP and TILN. All authors contributed to writing of the article.
Funding: The HUNT3 Survey was mainly funded by the Norwegian Ministry of Health, the Norwegian University of Science and Technology, the Norwegian Research Council (the FUGE program), Central Norway Regional Health Authority, the Nord-Trøndelag County Council and the Norwegian Institute of Public Health. The present analysis received support from the Research Fund of the Icelandic College of Family Physicians. The funders had no role in study design, data collection or analysis, decision to publish or preparation of the manuscript.
Competing interests: None declared.
Patient consent: Obtained.
Ethics approval: Each participant in the HUNT study signed a written consent regarding the screening and the use of data for research purposes. The study was approved by the Norwegian Data Inspectorate and the Regional Committee for Ethics in Medical Research.
Provenance and peer review: Not commissioned; externally peer reviewed.
Data sharing statement: Owing to restrictions related to patient consent and Norwegian privacy laws, data are available on request. More information is available at the following URL (http://www.ntnu.edu/hunt/data) and interested parties may contact Dr Steinar Krokstad (steinar.krokstad@ntnu.no) with further questions.
References
- 1.Fortin M, Stewart M, Poitras ME et al. . A systematic review of prevalence studies on multimorbidity: toward a more uniform methodology. Ann Fam Med 2012;10:142–51. 10.1370/afm.1337 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.World Health Organization. The World Health Report 2008: Primary Health Care—now more than ever. http://www.who.int/whr/2008/en/ (accessed 5 May 2016).
- 3.Barnett K, Mercer SW, Norbury M et al. . Epidemiology of multimorbidity and implications for health care, research, and medical education: a cross-sectional study. Lancet 2012;380:37–43. 10.1016/S0140-6736(12)60240-2 [DOI] [PubMed] [Google Scholar]
- 4.Marmot MG. Understanding social inequalities in health. Perspect Biol Med 2003;46(Suppl 3):S9–23. [PubMed] [Google Scholar]
- 5.Tomasdottir MO, Getz L, Sigurdsson JA et al. . Co-and multimorbidity patterns in an unselected Norwegian population: cross-sectional analysis based on the HUNT study and theoretical reflections concerning basic medical models. Eur J Pers Cent Healthc 2014;2:335–45. [Google Scholar]
- 6.Bousquet J, Anto JM, Sterk PJ et al. . Systems medicine and integrated care to combat chronic noncommunicable diseases. Genome Med 2011;3:43 10.1186/gm259 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.McEwen BS. Protective and damaging effects of stress mediators. N Engl J Med 1998;338:171–9. 10.1056/NEJM199801153380307 [DOI] [PubMed] [Google Scholar]
- 8.Delpierre C, Barboza-Solis C, Torrisani J et al. . Origins of health inequalities: the case for Allostatic Load. Longit Life Course Stud 2016;7:25. [Google Scholar]
- 9.Tomasdottir MO, Sigurdsson JA, Petursson H et al. . Self reported childhood difficulties, adult multimorbidity and allostatic load. A cross-sectional analysis of the Norwegian HUNT study. PLoS ONE 2015;10:e0130591 10.1371/journal.pone.0130591 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Beckie TM. A systematic review of allostatic load, health, and health disparities. Biol Res Nurs 2012;14:311–46. 10.1177/1099800412455688 [DOI] [PubMed] [Google Scholar]
- 11.McEwen BS. Biomarkers for assessing population and individual health and disease related to stress and adaptation. Metab 2015;64(Suppl 3):S2–S10. [DOI] [PubMed] [Google Scholar]
- 12.Merleau-Ponty M. Phenomenology of perception. London: Routledge, 1989. [Google Scholar]
- 13.Miilunpalo S, Vuori I, Oja P et al. . Self-rated health status as a health measure: the predictive value of self-reported health status on the use of physician services and on mortality in the working-age population. J Clin Epidemiol 1997;50:517–28. [DOI] [PubMed] [Google Scholar]
- 14.Krieger N. Embodiment: a conceptual glossary for epidemiology. Epidemiol Community Health 2005;59:350–5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Krieger N, Davey Smith G ‘Bodies count,’ and body counts: social epidemiology and embodying inequality. Epidemiol Rev 2004;26:92–103. 10.1093/epirev/mxh009 [DOI] [PubMed] [Google Scholar]
- 16.Danese A, McEwen BS. Adverse childhood experiences, allostasis, allostatic load, and age-related disease. Physiol Behav 2012;106:29–39. 10.1016/j.physbeh.2011.08.019 [DOI] [PubMed] [Google Scholar]
- 17.Felitti VJ, Anda RF, Nordenberg D et al. . Relationship of childhood abuse and household dysfunction to many of the leading causes of death in adults. The Adverse Childhood Experiences (ACE) Study. Am J Prev Med 1998;14:245–58. [DOI] [PubMed] [Google Scholar]
- 18.Getz L, Kirkengen AL, Ulvestad E. The human biology—saturated with experience. Tidsskr Nor Laegeforen 2011;131:683–7. 10.4045/tidsskr.10.0874 [DOI] [PubMed] [Google Scholar]
- 19.Kirkengen AL. The lived experience of violation: how abused children become unhealthy adults. Bucharest: Zeta Books, 2010. [Google Scholar]
- 20.Marmot M, Bell R. Fair society, healthy lives. Public Health 2012;126(Suppl 1):S4–S10. 10.1016/j.puhe.2012.05.014 [DOI] [PubMed] [Google Scholar]
- 21.Marmot M, Shipley M, Brunner E et al. . Relative contribution of early life and adult socioeconomic factors to adult morbidity in the Whitehall II study. J Epidemiol Community Health 2001;55:301–7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Berger M, Sarnyai Z ‘More than skin deep’: stress neurobiology and mental health consequences of racial discrimination. Stress 2015;18:1–10. 10.3109/10253890.2014.989204 [DOI] [PubMed] [Google Scholar]
- 23.Damjanovic AK, Yang Y, Glaser R et al. . Accelerated telomere erosion is associated with a declining immune function of caregivers of Alzheimer's disease patients. J Immunol 2007;179:4249–54. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Gallagher S, Phillips AC, Drayson MT et al. . Parental caregivers of children with developmental disabilities mount a poor antibody response to pneumococcal vaccination. Brain Behav Immun 2009;23:338–46. 10.1016/j.bbi.2008.05.006 [DOI] [PubMed] [Google Scholar]
- 25.Steptoe A, Dockray S, Wardle J. Positive affect and psychobiological processes relevant to health. J Pers 2009;77:1747–76. 10.1111/j.1467-6494.2009.00599.x [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Ulvestad E. Psychoneuroimmunology: the experiential dimension. Methods Mol Biol 2012;934:21–37. 10.1007/978-1-62703-071-7_2 [DOI] [PubMed] [Google Scholar]
- 27.Centers for Disease Control and Prevention. Health-related quality of life. http://www.cdc.gov/hrqol/wellbeing.htm (accessed 13 Jul 2016).
- 28.Krokstad S, Langhammer A, Hveem K et al. . Cohort profile: the HUNT study, Norway. Int J Epidemiol 2013;42:968–77. 10.1093/ije/dys095 [DOI] [PubMed] [Google Scholar]
- 29.Vikum E, Krokstad S, Westin S. Socioeconomic inequalities in health care utilisation in Norway: the population-based HUNT3 survey. Int J Equity Health 2012;11:48 10.1186/1475-9276-11-48 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Krokstad S, Knudtsen MS. Folkehelse i endring. Helseundersøkelsen i Nord-Trøndelag. HUNT 1 (1984–86)—HUNT 2 (1995–97)—HUNT 3 (2006–08). (Public health development. The HUNT Study, Norway). Levanger, Norway: HUNT Research Center, 2011. [Google Scholar]
- 31.Bourdieu P. The logic of practice. Cambridge: Polity Press, 1990. [Google Scholar]
- 32.Mackenbach JD, Lakerveld J, van Lenthe FJ et al. . Neighbourhood social capital: measurement issues and associations with health outcomes. Obes Rev 2016;17(Suppl 1):96–107. 10.1111/obr.12373 [DOI] [PubMed] [Google Scholar]
- 33.Rocco L, Suhrcke M. Is social capital good for health? A European perspective. Copenhagen: World Health Organization, 2012. [Google Scholar]
- 34.Antonovsky A. The structure and properties of the sense of coherence scale. Soc Sci Med 1993;36:725–33. [DOI] [PubMed] [Google Scholar]
- 35.Eriksson M, Lindstrom B. Antonovsky's sense of coherence scale and the relation with health: a systematic review. J Epidemiol Community Health 2006;60:376–81. 10.1136/jech.2005.041616 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Dobson C, Goudy WJ, Keith PM et al. . Further analysis of Rosenberg′s self-esteem scale. Psychol Rep 1979;44: 639–41. [Google Scholar]
- 37.Pressman SD, Cohen S. Does positive affect influence health? Psycholl Bull 2005;131:925–71. [DOI] [PubMed] [Google Scholar]
- 38.Robins RW, Hendin HM, Trzesniewski KH. Measuring global self-esteem: construct validation of a single-item measure and the Rosenberg Self-Esteem scale. Pers Soc Psychol Bull 2001;27:151–61. [Google Scholar]
- 39.Ottaviani C, Thayer JF, Verkuil B et al. . Physiological concomitants of perseverative cognition: a systematic review and meta-analysis. Psychol Bull 2016;142:231–59. 10.1037/bul0000036 [DOI] [PubMed] [Google Scholar]
- 40.Trzesniewski KH, Donnellan MB, Moffitt TE et al. . Low self-esteem during adolescence predicts poor health, criminal behavior, and limited economic prospects during adulthood. Dev Psychol 2006;42:381–90. 10.1037/0012-1649.42.2.381 [DOI] [PubMed] [Google Scholar]
- 41.De Vogli R, Ferrie JE, Chandola T et al. . Unfairness and health: evidence from the Whitehall II Study. J Epidemiol Community Health 2007;61:513–8. 10.1136/jech.2006.052563 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Keyes CL, Simoes EJ. To flourish or not: positive mental health and all-cause mortality. Am J Public Health 2012;102:2164–72. 10.2105/AJPH.2012.300918 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Faragher EB, Cass M, Cooper CL. The relationship between job satisfaction and health: a meta-analysis. Occup Environ Med 2005;62:105–12. 10.1136/oem.2002.006734 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Holt-Lunstad J, Smith TB, Baker M et al. . Loneliness and social isolation as risk factors for mortality: a meta-analytic review. Perspect Psychol Sci 2015;10:227–37. 10.1177/1745691614568352 [DOI] [PubMed] [Google Scholar]
- 45.Holt-Lunstad J, Smith TB, Layton JB. Social relationships and mortality risk: a meta-analytic review. PLoS Med 2010;7: e1000316 10.1371/journal.pmed.1000316 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Lehman BJ, Cane AC, Tallon SJ et al. . Physiological and emotional responses to subjective social evaluative threat in daily life. Anxiety Stress Coping 2015;28:321–39. 10.1080/10615806.2014.968563 [DOI] [PubMed] [Google Scholar]
- 47.Tsenkova VK, Carr D, Coe CL et al. . Anger, adiposity, and glucose control in nondiabetic adults: findings from MIDUS II. J Behav Med 2014;37:37–46. 10.1007/s10865-012-9460-y [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48.Cohen R, Bavishi C, Rozanski A. Purpose in life and its relationship to all-cause mortality and cardiovascular events: a meta-analysis. Psychosom Med 2016;78:122–33. 10.1097/PSY.0000000000000274 [DOI] [PubMed] [Google Scholar]
- 49.Zilioli S, Slatcher RB, Ong AD et al. . Purpose in life predicts allostatic load ten years later. J Psychosom Res 2015;79: 451–7. 10.1016/j.jpsychores.2015.09.013 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50.Juster RP, McEwen BS. Sleep and chronic stress: new directions for allostatic load research. Sleep Med 2015;16:7–8. 10.1016/j.sleep.2014.07.029 [DOI] [PubMed] [Google Scholar]
- 51.McEwen BS, Karatsoreos IN. Sleep deprivation and circadian disruption: stress, allostasis, and allostatic load. Sleep Med Clin 2015;10:1–10. 10.1016/j.jsmc.2014.11.007 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 52.Zisapel N. Sleep and sleep disturbances: biological basis and clinical implications. Cell Mol Life Sci 2007;64:1174–86. 10.1007/s00018-007-6529-9 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 53.Waller G. Self-rated health—from epidemiology to patient encounter. Umea University, 2015. [Google Scholar]
- 54.Vie TL, Hufthammer KO, Holmen TL et al. . Is self-rated health a stable and predictive factor for allostatic load in early adulthood? Findings from the Nord Trondelag Health Study (HUNT). Soc Sci Med 2014;117:1–9. 10.1016/j.socscimed.2014.07.019 [DOI] [PubMed] [Google Scholar]
- 55.Friedman EM, Hayney MS, Love GD et al. . Social relationships, sleep quality, and interleukin-6 in aging women. Proc Natl Acad Sci USA 2005;102:18757–62. 10.1073/pnas.0509281102 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 56.Kraus MW, Adler N, Chen TW. Is the association of subjective SES and self-rated health confounded by negative mood? An experimental approach. Health Psychol 2013;32:138–45. 10.1037/a0027343 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 57.Langhammer A, Krokstad S, Romundstad P et al. . The HUNT study: participation is associated with survival and depends on socioeconomic status, diseases and symptoms. BMC Med Res Methodol 2012;12:143 10.1186/1471-2288-12-143 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 58.Mjolstad BP, Kirkengen AL, Getz L et al. . Standardization meets stories: contrasting perspectives on the needs of frail individuals at a rehabilitation unit. Int J Qual Stud Health Well-being 2013;8:21498. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 59.Starfield B. Is patient-centered care the same as person-focused care? Perm J 2011;15:63–9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 60.Vogt H, Hofmann B, Getz L. The new holism: P4 systems medicine and the medicalization of health and life itself. Med Health Care Philos 2016;19:307–23. 10.1007/s11019-016-9683-8 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 61.Kirkengen AL, Thornquist E. The lived body as a medical topic: an argument for an ethically informed epistemology. J Eval Clin Pract 2012;18:1095–101. 10.1111/j.1365-2753.2012.01925.x [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
bmjopen-2016-012602supp.pdf (493.8KB, pdf)