Description
A 36-year-old man had been diagnosed with type 2 diabetes and put on twice daily premixed insulin for severe hyperglycaemia and osmotic symptoms about 3 months prior to his presentation to us. He was injecting himself with U-40 insulin syringe subcutaneously over anterior abdomen with proper technique and regular rotation of the injection sites. After about 2 months after starting insulin he had noticed multiple firm nodules appearing over the injection sites. The nodules were painless, became fluctuant over the course of time and used to burst spontaneously with discharge of pus. He had been put on several courses of oral antibiotics over the previous 2 months without any symptomatic relief. Some of the swellings required incision and drainage of the underlying pus. Gram stain and both aerobic and anaerobic culture of the drained pus were negative on multiple occasions.
A thorough systemic examination did not reveal any abnormality. Complete blood count including erythrocyte sedimentation rate was normal. Mantoux test with 5 tuberculin unit was negative. Histopathological examination of the scrapings from abscess wall revealed features of chronic inflammation with Langhans giant cells and granuloma formation. No fungal element was detected in the potassium hydroxide preparation but Ziehl-Neelsen (ZN) stain of direct smear from the pus showed acid-fast bacilli (figure 1). Growth in BacT/Alert 3D 60 culture system was positive on sixth day. The organism was identified as Mycobacterium tuberculosis complex (MTb complex) using PCR-based line probe assay (Hain Lifescience, GenoType Mycobacterium CM) (figure 2). The causative organism was further confirmed to be MTb complex and drug sensitivity performed by GenoType MTBDR Plus V2 (PCR-based line probe assay) documented that the organism was sensitive to isoniazid and rifampin. The organism formed a buff-coloured rough colony on Lowenstein-Jensen media after 5 weeks of incubation and was found to be niacin test, nitrate reduction test and pyrazinamidase test positive confirming M. tuberculosis. The patient was successfully treated with Category I antitubercular drug for 6 months without recurrence (figure 3).
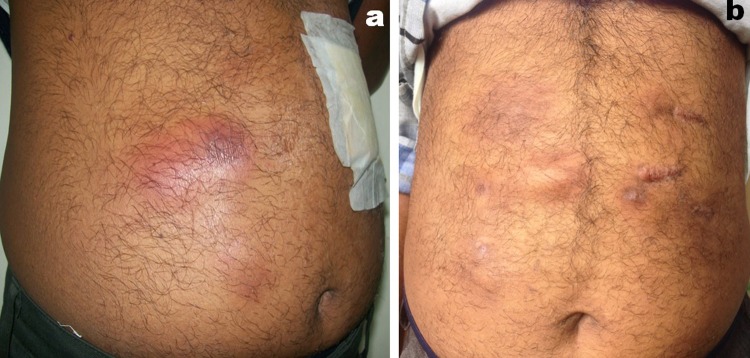
Figure 1.
Direct smear from the pus showing acid-fast bacilli under oil immersion (Centre of the field).
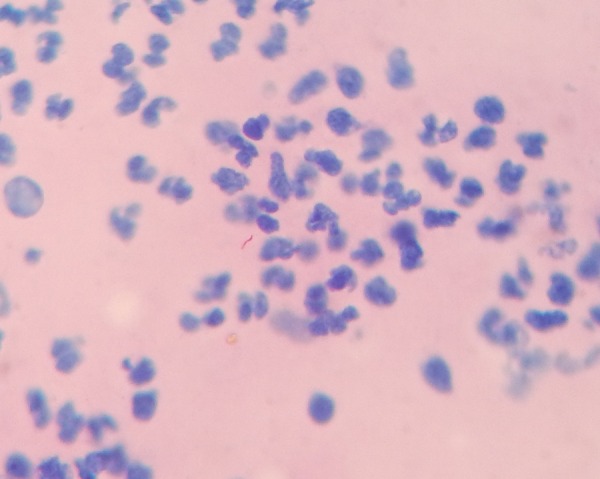
Figure 2.
Line probe assay hybridisation strip showing band against TUB indicating MTb complex. It also shows that the organism is sensitive to isoniazide (band against inh A, inh WT1 and inhWT2) and rifampicin (Band against katG Wt). MTb complex, Mycobacterium tuberculosis complex.
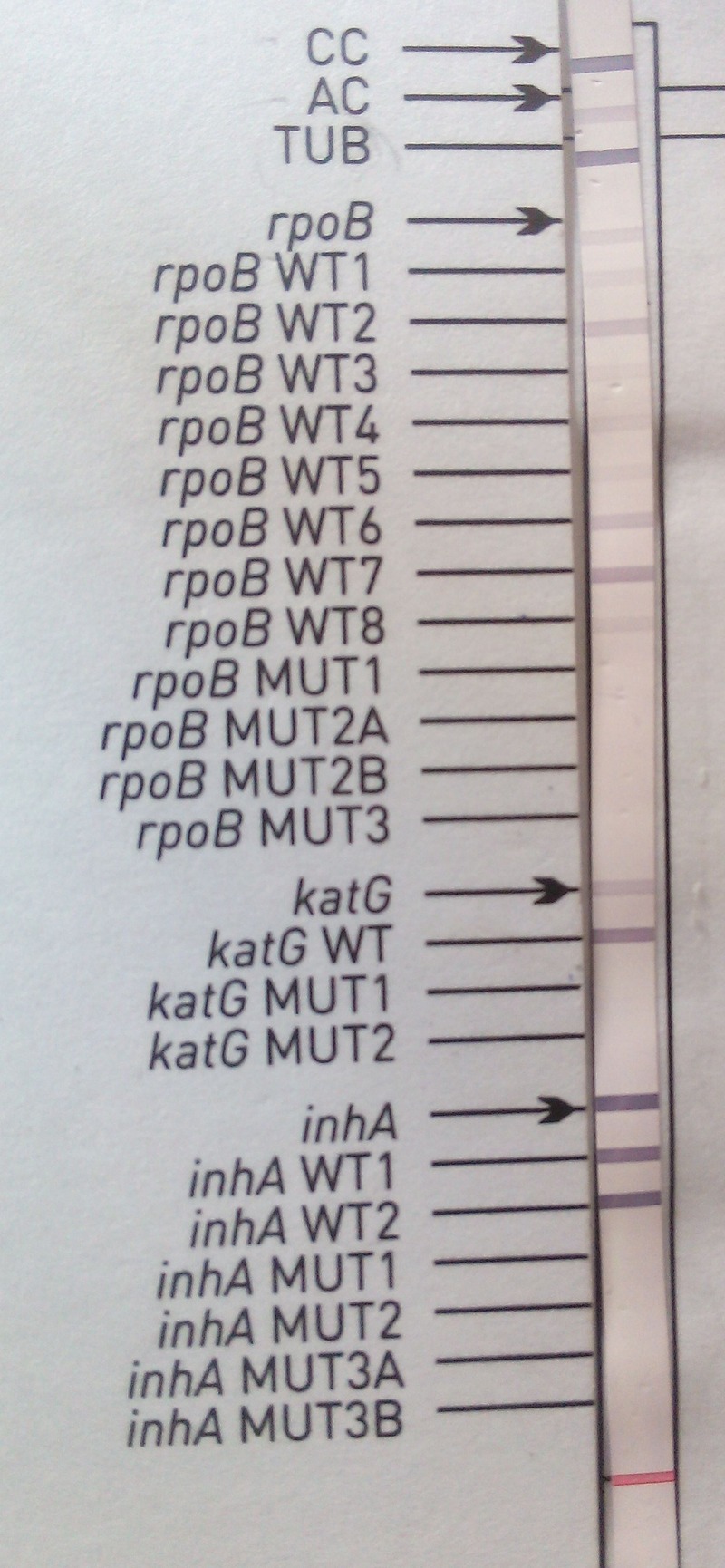
Figure 3.
Clinical photograph showing multiple subcutaneous nodules over insulin injection sites (a) and complete healing with scar formation after a course of antitubercular therapy (b).
The members of MTb complex include M. tuberculosis, M. bovis, M. bovis BCG, M. africanum, M. microti, M. canettii and M. pinnipedii. Among these the last three rarely cause human infections. M. africanum is confined to East and West tropical Africa and the rest are distributed worldwide. In India M. tuberculosis and M. bovis are commonly encountered. India, a country with the highest burden of tuberculosis as per the latest data provided by the WHO has an incidence of 2.2 million cases out of a global incidence of 9.6 million The most common route of infection of MTb complex is through droplet nuclei usually involving the lungs, genitourinary tract, lymph nodes, central nervous system, bone and joints, peritoneum and pericardium. While extrapulmonary tuberculosis accounts for about 10–15% cases, cutaneous tuberculosis comprises only a small proportion (<2%) of all forms of tuberculosis. Primary cutaneous infection is either caused by the so-called occult haematogenous tuberculosis by sporadic dissemination from the initial focus or via regional lymph node and thoracic duct before development of delayed hypersensitivity or by primary inoculation at injection site.1 2 Infection over Insulin injection sites is not uncommon among patients with diabetes. Most of these are due to bacterial infections; however, there are several reports of atypical mycobacterial infection as well. In this patient, the pus was sterile on repeated culture and our differentials included MTb complex, Mycobacterium other than tuberculosis (MOTT), zygomycosis, Fusarium, Candida, actinomycetes and fastidious organisms like Legionella or Mycoplasma hominis. We found acid-fast bacilli in ZN stain using 20% H2SO4 as the decolourising agent, which could exclude Actinomycetes, as these are acid fast only in modified ZN stain (Kinyoun method), and the non-acid-fast fastidious bacteria. Line probe assay was performed to differentiate between MTb Complex and MOTT. M. tuberculosis infection over insulin injection site has rarely been reported; even in those cases, the diagnosis of M. tuberculosis was not convincing.3 To conclude, tubercular infection though rare should be considered in patients having antibiotic-resistant sterile abscesses over the insulin injection sites.
Learning points.
Primary tubercular infection of the insulin injection site is one of the rare complications of insulin therapy.
Postinjection tubercular abscess should be considered in the differential diagnosis of insulin site infection especially if the drained pus is repeatedly sterile and the infection is resistant to antibiotics.
A correct and timely diagnosis of primary cutaneous tuberculosis avoids unnecessary antibiotic usage and surgical interventions.
Footnotes
Contributors: PPC was involved in diagnosis, patient management, literature search and preparing the manuscript. MC and SD was involved in laboratory diagnosis, literature search and preparing the manuscript.
Competing interests: None declared.
Patient consent: Obtained.
Provenance and peer review: Not commissioned; externally peer reviewed.
References
- 1.Speert DP. Tuberculosis. In: Krugman S, Katz SI, Gershon AA et al. eds. Infectious diseases of children. 9th edn Missouri: Mosby, 1992:551–2. [Google Scholar]
- 2.Kovats F, Miskovits G, Hutas I. Experimental studies on the formation of tuberculous abscesses following intramuscular injections. Orv Hetil 1955;96:1126–9. [PubMed] [Google Scholar]
- 3.Tomar R, Gupta A, Wilkhoo NS et al. Tubercular abscess following intramuscular injections. Med J Armed Forces India 2007;63:374–5. doi:10.1016/S0377-1237(07)80024-4 [DOI] [PMC free article] [PubMed] [Google Scholar]