Abstract
We describe a patient with an incidental finding of a large mass adjacent to the heart detected on a screening CT scan. The differential diagnosis included primary and secondary tumours of the heart. Subsequent investigation with trans-thoracic echocardiogram and cardiac MRI confirmed a diagnosis of a giant pericardial lipoma, one of the common benign primary cardiac tumours.
Background
Primary tumours of the heart are exceedingly rare, accounting for <5% of all cardiac tumours.1 Lipoma is a collection of fat cells which usually occur in the skin and are rarely found around the heart. Presentation of cardiac tumours such as lipoma is a spectrum, varying from asymptomatic to chest pain, breathlessness, dizziness or syncope.
We report a case of an asymptomatic patient with an incidental finding of a mass around the base of her heart on a health screening CT scan. Further investigation showed this mass to be a giant pericardial lipoma. This case describes the largest asymptomatic pericardial lipoma reported in the literature. Increasing access to cardiovascular health screening of asymptomatic people with CT and other imaging is likely to increase detection of cardiac masses, and physicians must be aware of their investigation and management.
Case presentation
An asymptomatic woman aged 55 years was referred to our outpatient cardiology clinic for investigation from the private health sector. She underwent a screening CT scan as part of a private health assessment which found her to have a 15×10 cm mass around the base of the heart (figure 1).
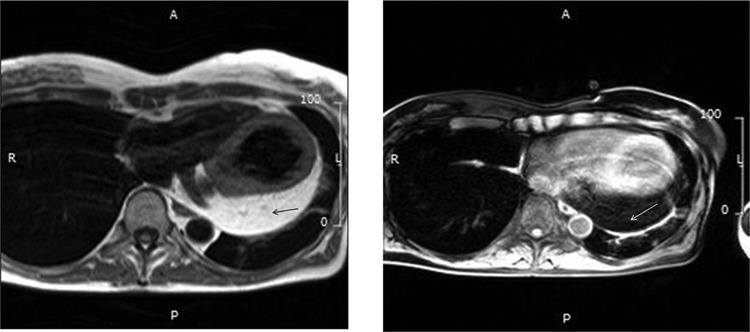
Figure 1.
Cardiac CT scan image, showing a large pericardial mass (white arrow) with low signal intensity (<0 Hounsfield Units).
She was an active person, with no history of adverse symptoms on exertion, including chest pain, dyspnoea or syncope. She had no family history of cardiovascular disease, or cardiac tumours.
Physical examination was unremarkable. There were no clinical signs of heart failure. Heart sounds were normal with no added sounds or murmurs.
Investigations
The patient underwent further investigation as an outpatient, to establish a diagnosis and to look for evidence of a mass effects compromising cardiovascular function.
Twelve-lead ECG showed sinus rhythm at 90 bpm with left axis deviation.
The screening CT scan showed a large low attenuation (<0 Hounsfield Units) intrapericardial mass that conform to the pericardial space. There were no mass effects seen. The appearances raised the suspicion of a lipoma.
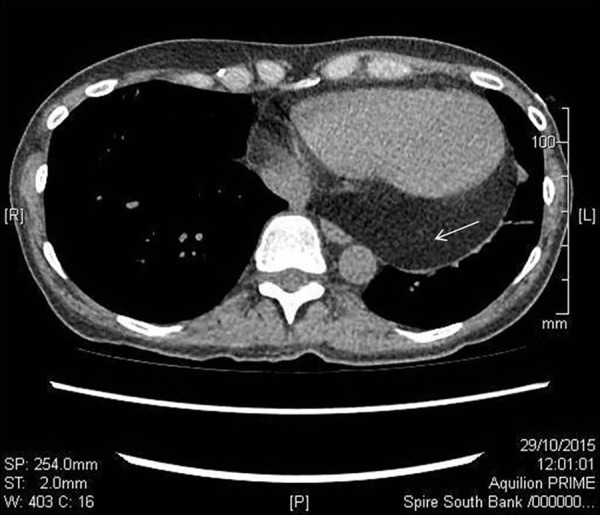
Echocardiography showed normal biventricular function with a well-demarcated echogenic mass within the pericardium (figure 2).
Figure 2.
Trans-thoracic echocardiogram (parasternal short-axis view) showing pericardial mass (dotted line).
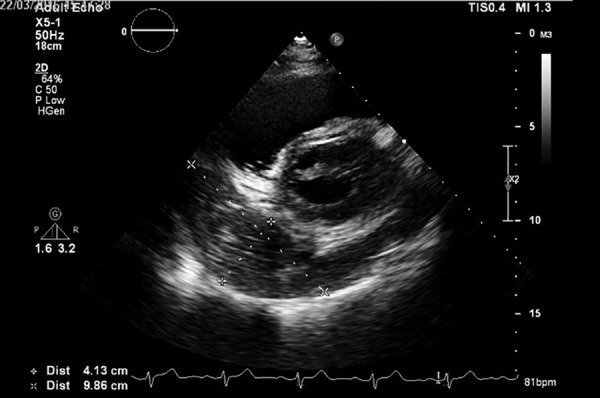
Cardiac MRI identified a large mass (12×5 cm) contained within the pericardium, extending around the basal to midlateral left ventricular wall and basal to apical inferior surface of the right ventricle and left ventricle. The mass had high signal intensity on T1-weighted imaging with signal loss following fat suppression and did not exhibit any delayed enhancement following gadolinium contrast administration confirming a fat-containing lesion, that is, lipoma within the pericardium (video 1, figure 3).
Figure 3.
Cardiac MRI. T1-weighted imaging (left) showing a well-defined pericardial mass with high signal intensity (black arrow) with signal loss following fat suppression (right). This suggests that it is likely to be a lipoma within the pericardium.
Video 1.
Video of cardiac MRI, showing a large mass contained within the pericardium, which extends around the basal to midlateral left ventricular wall and basal to apical inferior surface of the right ventricle and the left ventricle.
Differential diagnosis
Ninety-five per cent of cardiac tumours are metastases to the heart. The most common primary tumour is lung cancer (37%), followed by breast (10%) and haematological malignancies, including leukaemia and lymphoma (10–20%).2 3 The management of cardiac masses should therefore include clinical assessment and investigation for common primary tumours.
Treatment, outcome and follow-up
Her case was discussed in the multidisciplinary Heart Team meeting. Based on the clinical and radiological findings and her asymptomatic status, there was no indication to recommend surgical excision of the lipoma. Outpatient follow-up with clinical assessment and annual surveillance MRI scanning has been initiated to monitor for growth of the lipoma and the development of attributable symptoms. The onset of symptoms or detection of mass effects caused by the lipoma would be a mandate for surgical excision.
Discussion
Cardiac masses are uncommon and can be categorised as neoplastic or non-neoplastic (thrombi, cysts and prominent anatomic structures). Ninety-five per cent of cardiac tumours are metastatic in origin. Primary tumours of the heart are very rare clinical findings, accounting for only 5% of all cardiac tumours. In a population-based study in Italy, the incident rate for primary cardiac tumours was 1.38 per 100 000 populations per year. About 90.5% of primary cardiac tumours were benign, and only 9.5% malignant. The primary cardiac tumours were myxoma (48%), fibroelastoma (15%), lipoma (15%), rhabdomyoma (8%), haemangioma (5%), sarcoma (5%), lymphoma (2%) and pericardial haemangiopericytoma (2%).4 5
We describe the largest asymptomatic pericardial lipoma reported in the literature.
Cardiac lipomas can occur at any age and affects both genders equally. Half of the lipomas originate from the subendocardium, a quarter from the subpericardium and a quarter from the myocardium.6 7 Cardiac lipomas are often asymptomatic, unless the mass compromises cardiac function. Patients may present with non-specific symptoms, including chest pain, dyspnoea and syncope.5 This may be due to compression of a cardiac chamber (usually right atrium or right ventricle), vessel or coronary artery, infiltration, obstruction, valvular regurgitation or constriction.8
Cardiac imaging plays a central key role in the non-invasive investigation of primary cardiac tumour. Cardiac CT scan may distinguish between aetiologies based on location, morphology and tissue characteristics, including radiodensity.
Figure 1 shows a mass of low attenuation which is characteristic of a lipoma. This can be distinguished from a myxoma which has a higher attenuation and liposarcoma which has a heterogenous signal intensity.5
Cardiac MRI provides higher soft-tissue resolution and the ability to evaluate the extent of the mass in great detail. Video 1 shows the pericardial mass which extends around the left and right ventricular walls. Figure 3 shows the mass with high intensity on T1-weighted imaging with signal loss following fat suppression, confirming the diagnosis of lipoma. Fatty tissue shows high signal intensity on T1-weighted sequences, whereas most cardiac tumours are isointense relative to the myocardium on T1-weighting.9
Access to health screening including cross-sectional imaging for the asymptomatic population is increasing. Moreover, availability and usage of echocardiographic and cross-sectional imaging to investigate patients in hospital is also expanding. An unwanted and inevitable outcome of the drive to screen healthy people to facilitate earlier detection of prognostically important disease is the increasing frequency of the chance finding of ‘incidentalomas’. Physicians and citizens must consider this possibility and the potential implications before embarking on any screening test. Cardiologists must have a good understanding of the aetiology, investigation and management of cardiac masses.
Patient’s perspective.
This is an interesting conundrum for me. I was offered a private health check, which revealed I was largely healthy, but also that I have a large pericardial lipoma. So far, there have been no symptoms. I have been told to watch for breathlessness, ankle swelling and dizziness, which I will do. The consultant has been reassuring in that he does not think it is cancerous, but has also said that the best way forward is to monitor it. I hope that the doctors will be able to learn from my condition. I am also hopeful that, having discovered it accidentally, it does not cause me problems, but at least I am aware and if I had any symptoms, much of the detective work has now been completed. The interesting debate is about the way the NHS can cope with the creep of the private sector—and also, where is the line between prevention and intervention? Without the private sector, I would not have been able to have such an indepth health check without showing any symptoms of concern. Now, I know there is something that could become a problem. That is good, however, I am now ‘in the system’. If I never show any signs of ill health because of this, is it a wise use of public money to give me MRI scans, visits to the consultant etc? Or, if it does become a problem, is it better that I have spent the money myself to diagnose? Whichever way, I am pleased that the NHS is there for me and has a plan of action to look after me—and provide information that could help other patients.
Learning points.
Primary cardiac tumours are a rare clinical finding.
Ninety-five per cent of cardiac tumours are metastatic, and management must include investigation for the common primary tumours.
Presentation varies from asymptomatic to chest pain, dyspnoea and syncope.
Cardiac imaging including echocardiography, cardiac CT and cardiac MRI plays a role in the non-invasive investigation of cardiac tumours.
‘Incidentalomas’ are an inevitable consequence of increasing usage of health screening.
Acknowledgments
The authors thank the patient for giving her consent to write the case report as well as contributing to the patient's perspective. Helga Perry, Electronic Systems & Resources Librarian at University Hospitals Coventry & Warwickshire NHS Trust, provided support with manuscript preparation and proof reading. Jason McAllister, Medical photographer at University Hospitals Coventry and Warwickshire NHS Trust, provided support with image editing.
Footnotes
Contributors: HS gained patient’s consent, made the literature search, wrote the draft and liaised with other authors for the final form of the case report. DVA gave constructive revision of the case report, selecting and analysis of figures or video LT and RW made the literature search and constructive revision of the case report.
Competing interests: None declared.
Patient consent: Obtained.
Provenance and peer review: Not commissioned; externally peer reviewed.
References
- 1.Singh S, Singh M, Kovacs D et al. A rare case of a intracardiac lipoma. Int J Surg Case Rep 2015;9:105–8. 10.1016/j.ijscr.2015.02.024 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Bussani R, De-Giorgio F, Abbate A et al. Cardiac metastases. J Clin Pathol 2007;60:27–34. 10.1136/jcp.2005.035105 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Goldberg AD, Blankstein R, Padera RF. Tumors metastatic to the heart. Circulation 2013;128:1790–4. 10.1161/CIRCULATIONAHA.112.000790 [DOI] [PubMed] [Google Scholar]
- 4.Cresti A, Chiavarelli M, Glauber M et al. Incidence rate of primary cardiac tumors: a 14-year population study. J Cardiovasc Med (Hagerstown) 2016;17:37–43. 10.2459/JCM.0000000000000059 [DOI] [PubMed] [Google Scholar]
- 5.Puvaneswary M, Edwards JRM, Bastian BC et al. Pericardial lipoma: ultrasound, computed tomography and magnetic resonance imaging findings. Australas Radiol 2000;44:321–4. 10.1046/j.1440-1673.2000.00821.x [DOI] [PubMed] [Google Scholar]
- 6.Roberts WC, Spray TL. Pericardial heart disease: a study of its causes, consequences, and morphologic features. Cardiovasc Clin 1976;7:11–65. [PubMed] [Google Scholar]
- 7.Crockett JE, Decker D, Reed W et al. Lipoma of the heart. Am J Cardiol 1964;14:394–8. 10.1016/0002-9149(64)90084-0 [DOI] [PubMed] [Google Scholar]
- 8.Noly PE, Mongeon FP, Rochon A. Pericardial constriction caused by a giant lipoma. Circulation 2016;133:1709–12. 10.1161/CIRCULATIONAHA.115.020318 [DOI] [PubMed] [Google Scholar]
- 9.Hananouchi GI, Goff WB. Cardiac lipoma: six year follow up with MRI characteristics, and a review of the literature. Magn Reson Imaging 1990;8:825–8. 10.1016/0730-725X(90)90021-S [DOI] [PubMed] [Google Scholar]