Description
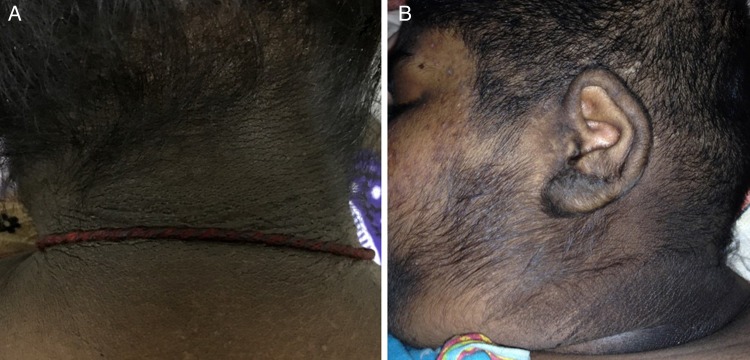
A 14-year-old girl without diabetes presented with recurrent attacks of generalised tonic–clonic seizures for the past 3 years which had partially been controlled with phenytoin and not with sodium valproate or levetiracetam. A detailed history revealed that each of those episodes was probably related to recurrent spontaneous hypoglycaemia. She was severely obese (body mass index: 36.54 kg/m2) with acanthosis nigricans (AN), facial acne and hirsutism (figure 1). During her hospital stay she developed spontaneous hypoglycaemia (plasma glucose: 25 mg/dL) and biochemical evaluation of the critical sample documented hyperinsulinaemic hypoglycaemia (serum insulin: 16.8 (>3 µIU/mL); C peptide: 3.46 (>0.6 ng/mL); β-hydroxybutyrate: 0.01 (<2.7 mmol/L)). The triphasic CT scan of abdomen revealed a 31×29 mm mass in the neck of the pancreas (figure 2). Screening for other components of multiple endocrine neoplasia type 1 (MEN-1) syndrome was negative. She underwent enucleation of the pancreatic mass and the histopathology was consistent with insulinoma. The postoperative period was complicated by development of grade 1 external pancreatic fistula and infection and gaping of the surgical wound for which she was put on antibiotics, total parenteral nutrition, octreotide and proton pump inhibitors. She recovered fully following conservative management and did not have any further episodes of hypoglycaemia or seizure following surgery and interestingly, at 4 weeks postoperatively, we noticed significant reduction of her AN (figure 3).
Figure 1.
Acanthosis nigricans (A and B), facial acne and hirsutism (B) before surgery.
Figure 2.
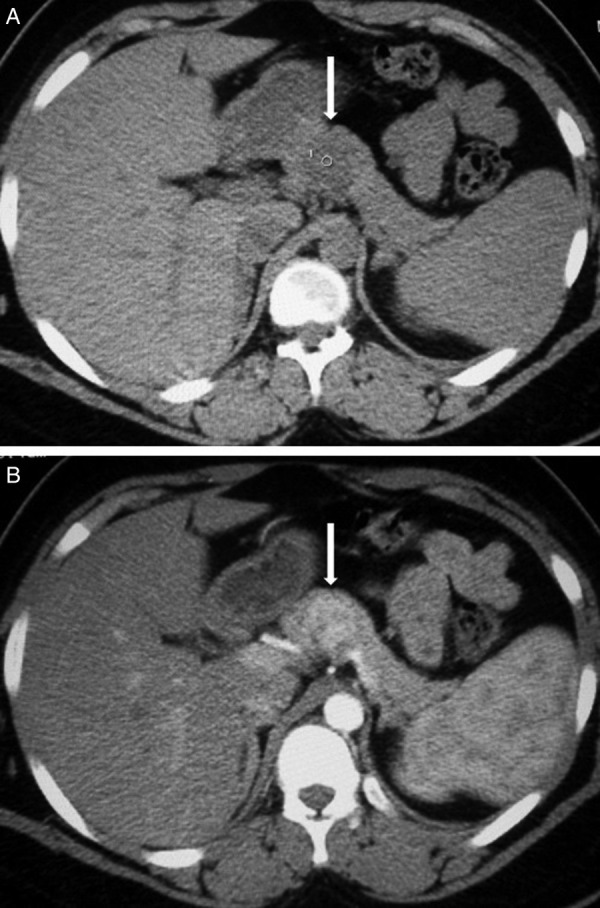
Mass over the neck of pancreas seen in triphasic CT scan of abdomen (white arrows) which is hypodense in non-contrast image (A) and shows heterogeneous enhancement following IV contrast (B).
Figure 3.

Near complete resolution of acanthosis nigricans at 4 weeks following surgery.
AN, a brown to black velvety hyperpigmentation of the skin predominantly affecting nape of the neck, axilla and groin develops due to epidermal proliferation. It is commonly associated with obesity, type 2 diabetes, polycystic ovarian syndrome, cancers and different monogenic causes of insulin resistance. Insulin resistance has traditionally been thought to be the basic underlying defect and AN is considered a cutaneous marker of insulin resistance. Insulin at relatively higher concentration crosses the dermoepidermal junction to reach the keratinocytes and binds to insulin-like growth factor receptor-1 (IGF-1R) to promote local proliferation of keratinocytes and fibroblasts. In addition to this direct effect, hyperinsulinaemia reduces insulin-like growth binding proteins (IGFBPs) and thereby increases circulatory free IGF-1 levels, which subsequently promote cell growth after binding to IGF-1R.
AN can also be seen in patients with elevated circulatory insulin without underlying insulin resistance. Some benign tumours such as insulinoma are found to be associated with AN. However, the frequency of AN in patients with insulinoma is quite rare and in one of the published series of 31 patients with insulinoma, none had AN.1 Moreover, reported insulinoma patients with acanthosis had much higher circulatory insulin levels unlike this girl.2 Amelioration of hyperinsulinaemia following successful surgery has been shown to improve AN in patients with insulinoma.3
We believe that the exact mechanism of AN in insulinoma is yet to be found and the rare occurrence of AN in this group of patients requires further research into the pathogenesis and its relation with circulatory insulin concentration.
Learning points.
Hypoglycaemia should be ruled out in all patients with recurrent seizure and acanthosis nigricans.
Elevated circulatory insulin level without insulin resistance is perhaps sufficient to cause acanthosis nigricans.
Normalising insulin level after successful surgery results in prompt resolution of acanthosis nigricans in patients with insulinoma.
Footnotes
Contributors: SP, PPC, HB and GS were involved in diagnosis, work-up and management of the patient. SP, PPC and HB performed the literature search and wrote the manuscript. GS finalised the manuscript.
Competing interests: None declared.
Patient consent: Obtained.
Provenance and peer review: Not commissioned; externally peer reviewed.
References
- 1.Jyotsna VP, Rangel N, Pal S et al. . Insulinoma: diagnosis and surgical treatment. Retrospective analysis of 31 cases. Indian J Gastroenterol 2006;25:244–7. [PubMed] [Google Scholar]
- 2.Jyotsna VP, Raizada N, Chakraborty S et al. . Acanthosis nigricans in insulinoma. Indian J Endocrinol Metab 2014;18:739 doi:10.4103/2230-8210.139223 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Ghosh S, Roychaudhury B, Mukhopadhyay S et al. . Clearance of acanthosis nigricans associated with insulinoma following surgical resection. QJM 2008;101:899–900. doi:10.1093/qjmed/hcn098 [DOI] [PubMed] [Google Scholar]