Abstract
A 22-year-old man presented to a rural hospital in Australia with right-sided pleuritic chest pain, right shoulder pain and dyspnoea. The patient had been receiving chronic asthma therapy without improvement. CT of the chest was performed after an abnormal X-ray, incidentally revealing one of the largest documented right-sided diaphragmatic hernias, with left lung compression due to mediastinal shift. The patient was definitively managed with thoracotomy alone. The contents of the hernia sac included colon and multiple loops of small bowel with a 10 cm neck. Definitive treatment was achieved with significant reduction in hernia size and formation of a neo-diaphragm with composite mesh. The postoperative period was complicated only by a wound infection. Two weeks after discharge the patient remained clinically well. Repeat chest X-ray showed no recurrence of the hernia. Congenital diaphragmatic hernias should be considered in patients with ongoing respiratory symptoms. Thoracotomy provides a safe approach.
Background
In this case report, we present a 20-year-old man with one of the largest documented congenital right-sided diaphragmatic hernias, along with a detailed literature review. Diaphragmatic hernias can be divided into congenital and acquired. Congenital diaphragmatic hernias are commoner in neonates, infants and children but are rare in adults. Acquired diaphragmatic hernias include hiatal, iatrogenic and traumatic.
Case presentation
A 20-year-old man presented to a rural hospital in Victoria, Australia, with right-sided pleuritic chest pain, right sided shoulder pain and shortness of breath. He reported these symptoms intermittently for approximately 2 weeks which worsened in the supine position and resolved at times with paracetamol. Vital signs are represented in table 1.
Table 1.
Vital signs on presentation to hospital
| Vital signs | |
|---|---|
| Blood pressure (mm Hg) | 141/81 |
| Heart rate (bpm) | 122 in sinus rhythm |
| Temperature (°C) | 37.8 |
| Oxygen saturations at room air (%) | 95 |
His past medical history included exercise induced asthma as a child for which he was prescribed inhaler therapy but no longer used routinely. The asthma diagnosis appeared to have been unchallenged since diagnosis. The patient had not been admitted to hospital before presentation, and it appeared that he only saw his local general practitioner. There was no prior radiological investigations or formal spirometry assessments. There was no significant family history. The patient lived at home with his parents. On examination there were no air sounds in the right side of his chest. The patient weighed 122 kg and was 171 cm tall.
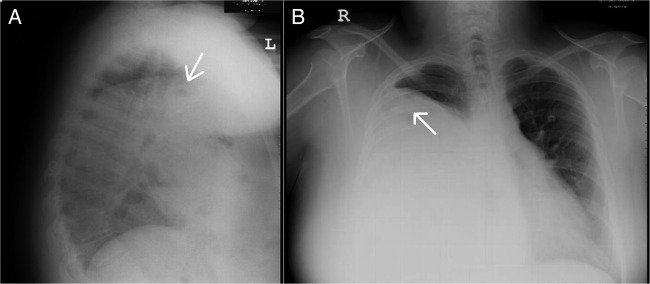
The patient's blood tests were unremarkable. His initial investigations also included a chest X-ray showing a large right-sided pleural collection with evidence of gas occupying virtually the entire right hemithorax with associated displacement of the great vessels and the heart (figure 1).
Figure 1.
Radiograph of (A) lateral film and (B) PA erect plain film showing a large defect in the right hemithorax with associated areas of gas (arrows).
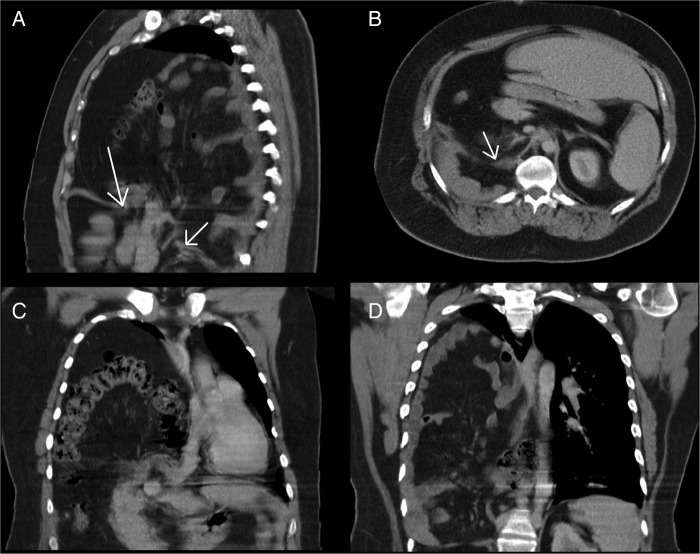
This was followed-up with CT of the chest which showed a very large right-sided diaphragmatic hernia, left-sided mediastinal shift and compression of the left lung (figure 2).
Figure 2.
Multiple detector CT shows (A) defect in the diaphragm with a hernial neck (arrows) measuring 8 cm. (B) Posterior defect (arrow) in the right hemidiaphragm. (C, D) Coronal reconstructions show the extent of visceral organ entrapment in the hernial sac with associated displacement of the heart and great vessels.
The hernia was noted to contain multiple loops of small and large bowel, the neck of the hernia measuring >8 cm. The patient's liver and kidney displaced inferiorly into the left of the midline. On further questioning the patient denied any history of trauma whatsoever.
The patient was diagnosed with a massive congenital right-sided diaphragmatic hernia and referred promptly to the Upper Gastrointestinal Unit and Cardiothoracic Unit, University Hospital, Geelong. The patient was managed in the emergency department of the rural hospital with analgesia and antibiotics. The patient's symptoms improved and he was subsequently discharged.
Over a 4 week period from the initial referral, the patient was seen by an upper gastrointestinal surgeon and a cardiothoracic surgeon with referrals for preoperative investigations (table 2). At this time, the patient's chest pain remained responsive to the analgesia prescribed and no further fevers were reported. The patient was commenced on a 2 week regimen of Optifast with the aim of losing at least 6 kg in weight.
Table 2.
Preoperative investigations
| Predicted | Actual | Per cent predicted (%) | |
|---|---|---|---|
| Spirometry | |||
| FEV1 (Litres) | 4.36 | 1.40 | 32 |
| FVC (Litres) | 5.18 | 1.65 | 31 |
| FEV1/FVC (%) | 84 | 85 | 100 |
| Transthoracic echocardiogram | |||
| Normal appearing left ventricular function and structurally normal tri-leaflet aortic valve | |||
FEV1, forced expiratory volume in 1 s; FVC, forced vital capacity.
The patient provided informed consent for laparoscopic and/or open abdominal approach with video assisted thoracoscopy and/or open thoracotomy for management of the diaphragmatic hernia. The patient's mother and patient were both present, with the patient agreeing to proceed to operation understanding the risks.
Investigations
Chest X-ray
Chest CT
Spirometry
Transthoracic echocardiogram
Treatment
The operation was carried out at the University Hospital, Geelong. The initial attempt was via an abdominal laparoscopic approach, potentially avoiding thoracotomy. This revealed a rotated liver to 90° on its transverse plane with a herniated gallbladder. The hernia sac was found to be densely adhered to the diaphragmatic pleura, which were excised together with the sac. The contents of the hernia included colon and multiple loops of small bowel along with its mesentery. Reduction of the hernia contents was unsuccessful despite multiple attempts. Laparoscopy was abandoned at this point and a right fifth interspace thoracotomy was performed to approach the hernia from above.
The hernia neck was better visualised and estimated to be at least 10 cm through the central tendon of the diaphragm. A sterile plastic bag was utilised to recreate an artificial hernia sac to enclose the small and large bowel in an attempt to reduce them. Despite multiple attempts, the plastic bag was discarded with the herniated contents not fully reducible much beyond 50%. The right upper lobe lung was fully expanded at this stage and occupied only half of the right hemithorax. As expected, the middle and lower right lobes were hypoplastic.
Two Parietex composite meshes were parachuted down to create a neo-diaphragm overlying the remaining herniated contents as a single piece was not large enough to enclose the contents (figure 3). A 20×25 cm mesh was attached to the anterior and medial aspects of the hernia neck with multiple interrupted nylon stitches. A mesh to mesh seam was formed with a second 20×30 cm mesh using a double breasted nylon continuous stitch. The second mesh was fixed laterally using extracorporeal nylon stitches around the right eight rib, posteriorly to the prevertebral fascia and diaphragm, and anteriorly to the diaphragm, chest wall and the hernia.
Figure 3.
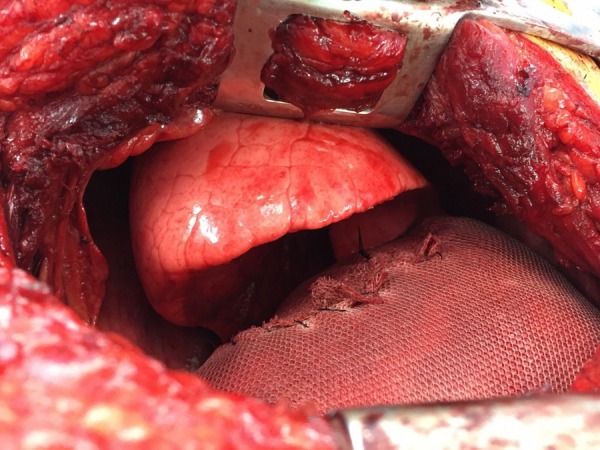
Fully expanded right upper lobe, and on the underside, the hypoplastic middle lobe can be visualised.
Outcome and follow-up
The patient remained in hospital for 17 days. The patient had a fever 14 days postoperatively with a suspicion of a wound site infection. A wound swab performed 2 weeks postoperatively showed Staphylococcus aureus resistant only to penicillin and erythromycin. After 48 hours of intravenous antibiotics, the patient was de-escalated to oral cephalexin. Post-discharge review at 2 weeks showed the wound to be healing very well. A repeat chest X-ray showed that the right upper lobe was still well ventilated and inflated. The right middle and lower lobes showed no further expansion.
Discussion
Congenital diaphragmatic hernias (CDHs) in adults can present a challenge to clinicians, and early recognition and operative care are essential. The literature contains a limited number of reported cases over the past century in adults. Bingham's case series of CDHs grouped these into three types: retrosternal, posterolateral and extensive defects, involving most of a hemidiaphragm,.1 Posterolateral hernias, known as Bochdalek hernias, are the most common with incidence rates of 0.02–0.03% and with a female predominance among symptomatic patients.2–4 The overall reported incidence of asymptomatic Bochdalek hernia in adults is 0.17–6%.5 6
CDHs occur due to failure of fusion between the septum transversum and the pleuroperitoneal folds of the developing diaphragm by the eighth week of gestation. Severe respiratory and circulatory distress in neonates and young children is a common feature in CDHs,.7 8 It is very uncommon for these to present in adulthood, and particularly on the right side (15% vs 85% on the left side).9–11 A classification system based on time of diaphragmatic herniation in life and respiratory development has been proposed.12 Adults tend to present with vague symptoms, including recurrent chronic abdominal pain, nausea/vomiting, constipation, chest pain or shortness of breath.4 13–17 Additional morbidity can include reduced exercise capacity with chronic lung disease, reduced intra-abdominal space complicating future surgery, stunted psychomotor development, stunted growth, nutritional disorders and gastro-oesophageal reflux disease. More serious acute adult presentations of incarceration, volvulus or ischaemia of herniated contents (eg, small or large bowel, stomach) can be a consequence of missed diagnosis.17–20 In our patient, there was left-sided mediastinal shift with left lung compression which, if not operated on, could have progressed.
Clinical examination findings in adult patients may be largely non-specific but lack of air entry to a hemithorax should warrant concern and further review. Initial investigations may include blood tests and a plain chest X-ray. Large hernias can impress on the mediastinum causing shift, lymphatic obstruction causing pleural effusion, pulmonary hypoplasia, pulmonary hypertension, consequential changes in heart function and even compression of the contralateral lung,.17 Associated with this can be other congenital diseases, such as CHARGE syndrome or Goldenhar syndrome,.21 22
Multiple detector CT has been shown to be most effective not only in characterising the diaphragmatic defect but also in planning surgical intervention and repair. CT can also rule out other differentials, such as mediastinal masses, bronchogenic cysts and other congenital malformations of the lung parenchyma.23 24 Our patient also underwent further diagnostic investigations to evaluate heart and lung function.
Management of CDH is exclusively surgical.7 8 23 Indications for surgery in adults can be elective or urgent, guided by the presenting features: acute gastrointestinal symptoms versus chronic abdominal pain or dyspnoea. Elective cases carry approximately 3% mortality whereas in emergencies it can be as high as 32%.25 This can be achieved by laparoscopy, laparotomy, video assisted thoracic surgery (VATS) or thoracotomy but the first approach is debated within the literature.3 7 10 15 19 24 26–39 Combined thoracic and abdominal approaches have also been reported. Laparotomy is favoured within the literature, ideal in patients presenting with an acute abdomen related to diaphragmatic hernias.9 40–42 Case reports in the literature of smaller diaphragmatic hernia repairs have shown success only with the laparoscopic abdominal approach.3 26 The abdominal approach allows perioperative assessment of viscera post reduction and addresses viscera malrotation.
In our case, the first abdominal laparoscopic approach was not successful. The hernia sac could not be excised and the herniated contents could not be reduced satisfactorily. Even with thoracotomy we found difficulty in physically fully reducing the herniated contents safely, possibly due to chronically reduced intra-abdominal space. Nevertheless, thoracotomy seems to be the favoured approach, particularly in elective cases with larger and complex diaphragmatic hernias.15 19 24 Thoracotomy offers a better chance of reducing the hernia by separation from intrathoracic adhesions and direct assessment for compromised viscera before reduction.9
There are also numerous cases in the literature describing the primary VATS approach, especially in adults.4 15 41 43–46 Earliest published reports with VATS in children for diaphragmatic hernia repair date back to 1995 but very few exist for the adult population.47–49 A multicentre study assessing VATS and laparoscopic management for CDH revealed an overall success rate of 67%.50 The benefit of a minimally invasive approach is potentially reduced hospital admission time, overall faster recovery and morbidity.3 27 39 44 51 An obvious point for VATS in diaphragmatic hernia repair is the learning curve that must be overcome.45 52 An increased risk of hypercapnia and acidosis in VATS due to carbon dioxide insufflation is observed in neonates and infants.53 54 Overall recurrence is significantly higher in primary VATS repairs.45 51 55 56 However, in the neonatal subgroup, it is suggested with improving technique, primary VATS repair is showing a decrease in recurrence rates.56
In the short term, severe complications can include visceral injury, abdominal compartment syndrome and severe infection. It is difficult to comment on long term surgical outcomes as they are not known in the adult subgroup. CDHs can present a challenge in adult patients. Clinicians should consider the possibility of undiagnosed diaphragmatic hernias in patients with persistent upper abdominal pain, lack of air entry on chest examination and postprandial dyspnoea. Surgical treatment is an option but preoperative planning is necessary where feasible.
Learning points.
Congenital diaphragmatic hernias must be kept as a differential diagnosis, particularly in failed long term therapy for respiratory disease in adults.
Early surgical referral is necessary for best care for the patient.
Large diaphragmatic hernias may not be completely reducible, and thoracotomy provides easier access in applying mesh to form a neo-diaphragm.
Acknowledgments
The authors would like to thank Dr Sonal Nagra (Surgical Fellow, Barwon Health) for assistance in the final proof reading of the submitted case report.
Footnotes
Contributors: NK: conception and design, acquisition of the data or analysis and interpretation of data. Drafting the article for important intellectual content. Final approval of the version published. GM, C-HY and ML: revising case report critically for important intellectual content. Final approval of the version published. All authors agree to be accountable for the article and to ensure that all questions regarding the accuracy or integrity of the article are investigated and resolved.
Competing interests: None declared.
Patient consent: Obtained.
Provenance and peer review: Not commissioned; externally peer reviewed.
References
- 1.Bingham JAW. Herniation through congenital diaphragmatic defects. Br J Surg 1959;47:1–15. 10.1002/bjs.18004720102 [DOI] [PubMed] [Google Scholar]
- 2.Deprest JA, Gratacos E, Nicolaides K et al. Changing perspectives on the perinatal management of isolated congenital diaphragmatic hernia in Europe. Clin Perinatol 2009;36:329–47. 10.1016/j.clp.2009.03.004 [DOI] [PubMed] [Google Scholar]
- 3.John PH, Thanakumar J, Krishnan A. Reduced port laparoscopic repair of Bochdalek hernia in an adult: a first report. J Minim Access Surg 2012;8:158–60. 10.4103/0972-9941.103131 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Tokumoto N, Tanabe K, Yamamoto H et al. Thoracoscopic-assisted repair of a Bochdalek hernia in an adult: a case report. J Med Case Reports 2010;4:366 10.1186/1752-1947-4-366 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Mullins ME, Stein J, Saini SS et al. Prevalence of incidental Bochdalek's hernia in a large adult population. Am J Roentgenol 2001;177:363–6. 10.2214/ajr.177.2.1770363 [DOI] [PubMed] [Google Scholar]
- 6.Wilbur AC, Gorodetsky A, Hibbeln JF. Imaging findings of adult Bochdalek hernias. Clin Imaging 1994;18:224–9. 10.1016/0899-7071(94)90088-4 [DOI] [PubMed] [Google Scholar]
- 7.Bosenberg AT, Brown RA. Management of congenital diaphragmatic hernia. Curr Opin Anesthesiol 2008;21:323–31. 10.1097/ACO.0b013e3282f9e214 [DOI] [PubMed] [Google Scholar]
- 8.de Buys Roessingh AS, Dinh-Xuan AT. Congenital diaphragmatic hernia: current status and review of the literature. Eur J Pediatr 2009;168:393–406. 10.1007/s00431-008-0904-x [DOI] [PubMed] [Google Scholar]
- 9.Machado NO. Laparoscopic repair of Bochdalek diaphragmatic hernia in adults. N Am J Med Sci 2016;8:65–74. 10.4103/1947-2714.177292 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Shenoy KR, Johri G. Congenital right Bochdalek hernia presenting as emergency in old age: a case report. Indian J Surg 2013;75(Suppl 1):255–6. 10.1007/s12262-012-0570-0 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Kumar A, Maheshwari V, Ramakrishnan T et al. Caecal perforation with faecal peritonitis—unusual presentation of Bochdalek hernia in an adult: a case report and review of literature. World J Emerg Surg 2009;4:16 10.1186/1749-7922-4-16 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Wiseman NE, MacPherson RI. “Acquired” congenital diaphragmatic hernia. J Pediatr Surg 1977;12:657–65. 10.1016/0022-3468(77)90389-X [DOI] [PubMed] [Google Scholar]
- 13.Ahrend TR, Thompson BW. Hernia of foramen of the Bochdalek in the adult. Am J Surg 1971;122:612–15. 10.1016/0002-9610(71)90288-1 [DOI] [PubMed] [Google Scholar]
- 14.Hines GL, Romero C. Congenital diaphragmatic-hernia in the adult. Int Surg 1983;68:349–51. [PubMed] [Google Scholar]
- 15.Laaksonen E, Silvasti S, Hakala T. Right-sided Bochdalek hernia in an adult: a case report. J Med Case Rep 2009;3:9291 10.1186/1752-1947-3-9291 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Osebold WR, Soper RT. Congenital posterolateral diaphragmatic hernia past infancy. Am J Surg 1976;131:748–54. 10.1016/0002-9610(76)90194-X [DOI] [PubMed] [Google Scholar]
- 17.Perhoniemi V, Helminen J, Luosto R. Posterolateral diaphragmatic-hernia in adults—acute symptoms, diagnosis and treatment. Scand J Thoracic Cardiovascular Surg 1992;26:225–7. 10.3109/14017439209099082 [DOI] [PubMed] [Google Scholar]
- 18.Naunheim KS. Adult presentation of unusual diaphragmatic hernias. Chest Surg Clin N Am 1998;8:359–69. [PubMed] [Google Scholar]
- 19.Niwa T, Nakamura A, Kato T et al. An adult case of Bochdalek hernia complicated with hemothorax. Respiration 2003;70:644–6. 10.1159/000075213 [DOI] [PubMed] [Google Scholar]
- 20.Salacin S, Alper B, Cekin N et al. Bochdalek hernia in adulthood—a review and an autopsy case-report. J Forensic Sci 1994;39:1112–16. 10.1520/JFS13692J [DOI] [PubMed] [Google Scholar]
- 21.Eren S, Ciris F. Diaphragmatic hernia: diagnostic approaches with review of the literature. Eur J Radiol 2005;54:448–59. 10.1016/j.ejrad.2004.09.008 [DOI] [PubMed] [Google Scholar]
- 22.Stoll C, Alembik Y, Dott B et al. Associated malformations in cases with congenital diaphragmatic hernia. Genet Couns 2008;19:331–9. [PubMed] [Google Scholar]
- 23.Carrascosa MF, Carrera IA, Garcia J-AS-Q et al. Symptomatic Bochdalek hernia in an adult patient. BMJ Case Rep 2010. 10.1136/bcr.05.2010.2996 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Zhou Y, Du H, Che G. Giant congenital diaphragmatic hernia in an adult. J Cardiothoracic Surg 2014;9:31 10.1186/1749-8090-9-31 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Fingerhut A, Pourcher J, Pelletier JM et al. Two cases of postero-lateral diaphragmatic hernia (congenital Bochdalek hernia) revealed at adult age by severe complications. Operation and cure review of the literature. J Chir (Paris) 1978;115:135–43. [PubMed] [Google Scholar]
- 26.Debergh I, Fierens K. Laparoscopic repair of a Bochdalek hernia with incarcerated bowel during pregnancy: report of a case. Surg Today 2014;44:753–6. 10.1007/s00595-012-0441-0 [DOI] [PubMed] [Google Scholar]
- 27.Dente M, Bagarani M. Laparoscopic dual mesh repair of a diaphragmatic hernia of Bochdalek in a symptomatic elderly patient. Updates Surg 2010; 62:125–8. 10.1007/s13304-010-0022-y [DOI] [PubMed] [Google Scholar]
- 28.Diaz-Legaspe AJ, Goena I, Colina A et al. Posterolateral diaphragmatic hernia in adults. Bochdalek's hernia. Report of a case. Revista de medicina de la Universidad de Navarra 1989;33:207–10. [PubMed] [Google Scholar]
- 29.Frisoni R, Germain A, Ayav A et al. Thoracoscopic treatment of a right Bochdalek hernia in an adult (with video). J Visceral Surg 2014;151:239-. 10.1016/j.jviscsurg.2014.03.002 [DOI] [PubMed] [Google Scholar]
- 30.Hamid KS, Rai SS, Rodriguez JA. Symptomatic Bochdalek hernia in an adult. JSLS 2010;14:279–81. 10.4293/108680810X12785289144719 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Herling A, Makhdom F, Al-Shehri A et al. Bochdalek hernia in a symptomatic adult. Ann Thorac Surg 2014;98:701–4. 10.1016/j.athoracsur.2013.09.074 [DOI] [PubMed] [Google Scholar]
- 32.Kawashima S, Urushihara N, Fukumoto K. Laparoscopic repair of Bochdalek hernia with intrathoracic kidney in a 2-year-old child. Asian J Endosc Surg 2014;7:279–81. 10.1111/ases.12114 [DOI] [PubMed] [Google Scholar]
- 33.Meteroglu F, Sahin A, Oruc M et al. Adult Bochdalek hernia: an analysis of eight patients. Turk Gogus Kalp Damar Cerrahisi Dergisi-Turkish Journal of Thoracic and Cardiovascular Surgery 2015;23:514–18. 10.5606/tgkdc.dergisi.2015.10277 [DOI] [Google Scholar]
- 34.Noh YS, Kim Y, Seo Y et al. Intrathoracic kidney with left-sided Bochdalek hernia in a woman with bacteremic acute pyelonephritis due to Escherichia coil. Korean J Intern Med 2015;30:267–8. 10.3904/kjim.2015.30.2.267 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Onuk O, Tas T, Senturk AB et al. Right-sided Bochdalek hernia with intrathoracic ectopic kidney in an advanced-age adult: a case report. Urol Int 2014;93:368–70. 10.1159/000353100 [DOI] [PubMed] [Google Scholar]
- 36.Roscher R, Buchler M, Bittner R. Bochdalek hernia in the adult. Med Klin (Munich) 1988;83:210–13. [PubMed] [Google Scholar]
- 37.Schumpelick V, Steinau G, Schluper I et al. Surgical embryology and anatomy of the diaphragm with surgical applications. Surg Clin North Am 2000;80:213–39. 10.1016/S0039-6109(05)70403-5 [DOI] [PubMed] [Google Scholar]
- 38.Sutedja B, Muliani Y. Laparoscopic repair of a Bochdalek hernia in an adult woman. Asian J Endosc Surg 2015;8:354–6. 10.1111/ases.12179 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Vega MT, Maldonado RH, Vega GT et al. Late-onset congenital diaphragmatic hernia: a case report. Int J Surg Case Reports 2013;4:952–4. 10.1016/j.ijscr.2013.07.034 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Brown SR, Horton JD, Trivetto E et al. Bochdalek hernia in the adult: demographics, presentation, and surgical management. Hernia 2010; 15:23–30. 10.1007/s10029-010-0699-3 [DOI] [PubMed] [Google Scholar]
- 41.Slesser AA, Ribbans H, Blunt D et al. A spontaneous adult right-sided Bochdalek hernia containing perforated colon. JRSM Short Reports 2011;254 10.1258/shorts.2011.011056 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Thomas S, Kapur B. Adult Bochdalek hernia—clinical-features, management and results of treatment. Jpn J Surg 1991;21:114–19. 10.1007/BF02470876 [DOI] [PubMed] [Google Scholar]
- 43.Costerus S, Zahn K, van de Ven K et al. Thoracoscopic versus open repair of CDH in cardiovascular stable neonates. Surg Endosc 2016;30:2818–24. 10.1007/s00464-015-4560-8 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Fujishiro J, Ishimaru T, Sugiyama M et al. Minimally invasive surgery for diaphragmatic diseases in neonates and infants. Surg Today 2016;46:757–63. 10.1007/s00595-015-1222-3 [DOI] [PubMed] [Google Scholar]
- 45.Zhu Y, Wu Y, Pu Q et al. Minimally invasive surgery for congenital diaphragmatic hernia: a meta-analysis. Hernia 2016;20:297–302. 10.1007/s10029-015-1423-0 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Esmer D, Alvarez-Tostado J, Alfaro A et al. Thoracoscopic and laparoscopic repair of complicated Bochdalek hernia in adult. Hernia 2008;12:307–9. 10.1007/s10029-007-0293-5 [DOI] [PubMed] [Google Scholar]
- 47.Silen ML, Canvasser DA, Kurkchubasche AG et al. Video-assisted thoracic surgical repair of a foramen of Bochdalek hernia. Ann Thorac Surg 1995;60:448–50. 10.1016/0003-4975(95)00100-Y [DOI] [PubMed] [Google Scholar]
- 48.Van der zee DC, Bax NM. Laparoscopic repair of congenital diaphragmatic-hernia in a 6-month-old child. Surg Endosc 1995;9:1001–3. 10.1007/BF00188460 [DOI] [PubMed] [Google Scholar]
- 49.Nakashima S, Watanabe A, Hashimoto M et al. Advantages of video-assisted thoracoscopic surgery for adult congenital hernia with severe adhesion: report of two cases. Ann Thorac Cardiovasc Surg 2011;17:185–9. 10.5761/atcs.cr.09.01528 [DOI] [PubMed] [Google Scholar]
- 50.Gomes Ferreira C, Reinberg O, Becmeur F et al. Neonatal minimally invasive surgery for congenital diaphragmatic hernias: a multicenter study using thoracoscopy or laparoscopy. Surg Endosc 2009;23:1650–9. 10.1007/s00464-009-0334-5 [DOI] [PubMed] [Google Scholar]
- 51.Dingemann C, Ure B, Dingemann J. Thoracoscopic procedures in pediatric surgery: what is the evidence? Eur J Pediatr Surg 2014;24:14–19. 10.1055/s-0033-1350060 [DOI] [PubMed] [Google Scholar]
- 52.Baerg J, Kanthimathinathan V, Gollin G. Late-presenting congenital diaphragmatic hernia: diagnostic pitfalls and outcome. Hernia 2012;16:461–6. 10.1007/s10029-012-0906-5 [DOI] [PubMed] [Google Scholar]
- 53.Bishay M, Giacomello L, Retrosi G et al. Hypercapnia and acidosis during open and thoracoscopic repair of congenital diaphragmatic hernia and esophageal atresia: results of a pilot randomized controlled trial. Ann Surg 2013;258: 895–900. 10.1097/SLA.0b013e31828fab55 [DOI] [PubMed] [Google Scholar]
- 54.Bishay M, Giacomello L, Retrosi G et al. Decreased cerebral oxygen saturation during thoracoscopic repair of congenital diaphragmatic hernia and esophageal atresia in infants. J Pediatr Surg 2011;46:47–51. 10.1016/j.jpedsurg.2010.09.062 [DOI] [PubMed] [Google Scholar]
- 55.Tsao K, Lally PA, Lally KP. Minimally invasive repair of congenital diaphragmatic hernia. J Pediatr Surg 2011;46:1158–64. 10.1016/j.jpedsurg.2011.03.050 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 56.Jancelewicz T, Langer JC, Chiang MP et al. Thoracoscopic repair of neonatal congenital diaphragmatic hernia (CDH): Outcomes after a systematic quality improvement process. J Pediatric Surg 2013;48:321–5. [DOI] [PubMed] [Google Scholar]