Abstract
Clomiphene citrate is widely used by the female population for the management of a wide array of medical conditions especially those related to ovulation, but its use in male population remains controversial. Efficacy of clomiphene is not well established in male hypogonadism and infertility. Its side effects and complications are also poorly studied or reported. We present a case of a man with infertility issues for which he started receiving clomiphene citrate 3 weeks before presenting with progressive symptoms of headache, vomiting, transient blurred vision and diplopia, which eventually turned out to be the symptoms of intracranial venous thrombosis. After excluding the common causes of intracranial venous thrombosis and hypercoagulable state, clomiphene citrate seems the most likely culprit.
Background
Intracranial venous thrombosis in a man as a side effect of clomiphene has never been reported in the literature. This extremely rare association has prompted us to report this to the medical world.
Case presentation
A man in his mid-30s presented to the emergency department with 12 days history of severe headache. He stated that the headache was occipital in location, compressive in nature, 8/10 in severity, radiating to the back of his neck, exacerbated by coughing or sneezing and poorly responsive to pain killers. He also reported of transient blurred and double vision, not related to any specific gaze direction, which started 3 days prior to his presentation. He visited different clinics and was diagnosed with tension headache and/or sinusitis, for which he was given various analgesics and decongestants with little or no benefit.
The patient had a history of infertility. All of his three children were born via in vitro fertilisation. His urologist started him on clomiphene citrate (50 mg orally every other day) 3 weeks prior to his presentation, in order to improve sperm count and motility. The patient was hypertensive, controlled with captopril and an ex-smoker (smoked for 10 years before quitting 2 years ago).
Family history was significant for migraine in his sister, hypertension in both parents and stroke in his father.
Initial physical examination revealed normal visual acuity but transient diplopia mainly on lateral and inferior gaze bilaterally. Funduscopy revealed bilateral papilledema. Rest of the systemic examination was normal.
Investigations
Initial CT scan of the head revealed no abnormalities. MRI of the brain together with magnetic resonance venogram (MRV) was then carried out, showing a hyper-intense late subacute clot in the torcula (confluence of sinuses) extending to left transverse sinus and into the left sigmoid sinus (in the T1 and T2 sequences), as well as a minimal T1 hyper-intensity suggestive of a clot extending into the posterior aspect of the superior sagittal sinus from the torcular region (figures 1 and 2)
Figure 1.

MRV (axial section) of cortical venous sinuses showing clot in the torcula (confluence of sinuses) extending to left transverse sinus and into the left sigmoid sinus. MRV, magnetic resonance venogram.
Figure 2.
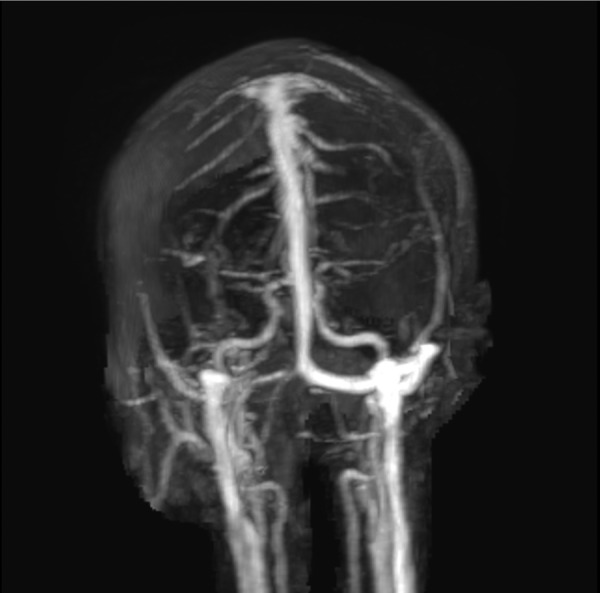
Three-dimensional reconstruction of MRV showing complete opacification of left transverse sinus. MRV, magnetic resonance venogram.
Thrombophilia (ie, factor V Leiden, anti-thrombin III, protein C and S, lupus anticoagulant, anti-cardiolipin antibodies, anti-B2-glycoprotein antibodies, homocysteine levels, vitamin B12 levels) and vasculitic screenings were negative.
Differential diagnosis
As our patient presented with severe headache that was exacerbated by coughing or sneezing and bilateral papilledema, we thought of three differential diagnoses: space-occupying lesion, idiopathic intracranial hypertension and cerebral venous thrombosis. Space-occupying lesion such as tumour was ruled out by performing CT scan of the head with contrast and MRI of the brain. MRV confirmed the diagnosis of intracranial venous sinus thrombosis; hence, we did not proceed to check the cerebrospinal fluid pressure.
Treatment
The patient was started on enoxaparin (80 mg subcutaneous two times per day) and warfarin (3 mg orally once daily). Low-molecular-weight heparin cover was continued for 24 hours after achieving therapeutic INR. The diagnosis was explained to him, and he was advised to stop taking clomiphene citrate. The patient was then continued on warfarin alone with target INR of 2–3 for 6 months.
Outcome and follow-up
The patient had a regular follow-up in the medical outpatient clinic. His symptoms improved dramatically after stopping clomiphene and initiating anticoagulation. His vision also improved on subsequent visits. He continued warfarin for 6 months and then was asked to stop as he showed remarkable recovery and the risk of future thrombosis was low. Follow-up CT venogram showed complete recanalisation of the involved venous sinuses (figure 3).
Figure 3.
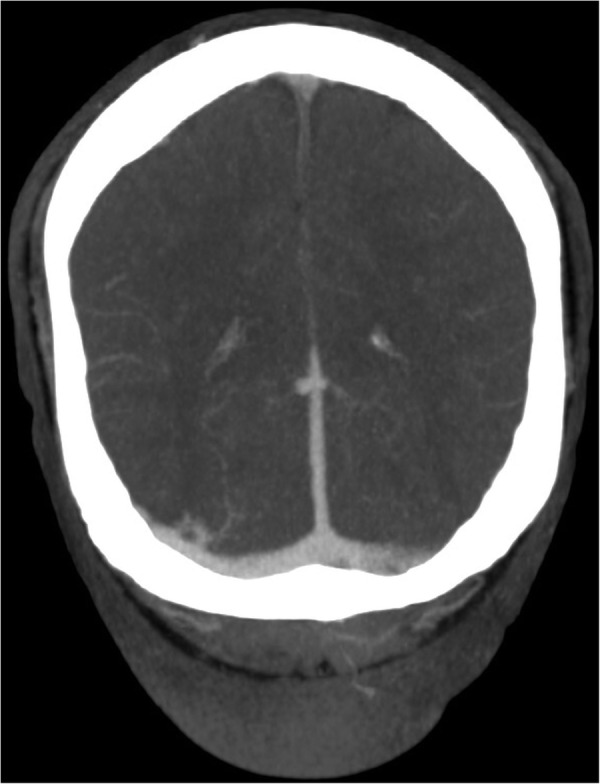
Follow-up CT venography (axial section) showing recanalisation of left transverse venous sinus.
Discussion
Intracranial venous thrombosis, with a frequency of 3–4 cases per million, is a relatively uncommon but potentially fatal (30-day mortality 5.6%) disorder. It occurs more frequently in women especially during pregnancy because of the complex hormonal interactions with prothrombotic factors. It usually occurs in younger population. International Study on Cerebral Venous and Dural Sinuses Thrombosis (ISCVT) showed that 487 of 624 cases (78%) occurred in patients who are <50 years of age.1
Around 85% of the patients having intracranial venous thrombosis are identified to have a risk factor that predisposes them to suffer from this catastrophic intracranial thrombosis.2 Apart from thrombophilia, there is a wide array of causes/risk factors that should be identified as it changes the course of management. Most of the patients with thrombophilia have another risk factor that triggers the onset of clot formation in an already susceptible patient.2 Inherited or acquired thrombophilia, prothrombotic drugs (like OCPs), infections and malignancies are the widely identified causes with the latter two posing more unfavourable outcomes.3
Classified anatomically, in the cerebral venous sinuses, most commonly affected are the superior sagittal sinus (72%) and the lateral sinuses (70%). Approximately 33% of cases involve more than one sinus, and 30%–40% of cases involve the sinuses and the cerebral or cerebellar veins.4
We report a case of a young man with no risk factors other than clomiphene citrate presenting with headache and blurred vision and subsequently diagnosed with cerebral venous thrombosis. To the best of our knowledge, there are no reported cases of intracranial venous thrombosis secondary to clomiphene citrate use in men. The presenting symptom in our case was headache, which is the most commonly reported symptom in this patient (89% as per ISCVT cohort). As compared to men, headache occurs more frequently in women. Patients can have a variety of other clinical features, which vary according to the venous sinus involved, extension of the disease to other sinus, patient's age and involvement of brain parenchyma.
Our patient was using clomiphene for infertility issues. Clomiphene citrate is a selective oestrogen receptor modulator. Clomiphene citrate has been used as a treatment of subfertility in women.5 Although showing mixed results when it is used to treat infertility in men,6 7 it has shown benefits in men with hypogonadism as low doses of clomiphene have resulted in improvement of the testosterone/oestradiol ratio. It also stimulates endogenous androgen production. Thus, it can be used as an alternative to testosterone for male hypogonadism.8 Its use in men is not approved by FDA but is prescribed off-label with human chorionic gonadotropin (HCG) to elevate total testosterone levels and to maintain spermatogenesis in hypogonadal men.
Clomiphene citrate administration causes an increase in pituitary gonadotropins release, followed by increased oestradiol levels, which have a thrombogenic effect. Hence, use of clomiphene may be associated with increased risk of venous thrombosis, particularly if patients have known risk factors.9
Common side effects of clomiphene include headaches, hot flushes, nausea, dizziness, visual disturbance, weight gain and fluid retention. Clomiphene is well known to cause gastrointestinal symptoms, visual disturbance and endocrine disorders.9 It is associated with venous thrombosis, DVT and central retinal vein thrombosis in women with various risk factors and rarely causes ovarian hyperstimulation syndrome. There were also some reports that suggested association of clomiphene in triggering venous thrombosis, for example, central retinal vein occlusion (CRVO),10 or DVT in women having various other thromboembolic risk factors.11 There was also a case of CRVO in a 35-year-old man with factor V Leiden mutation that has been reported.12 However, there are no published reports to date of intracranial venous thrombosis in men or women with or without risk factors associated with the use of clomiphene citrate. Thus, to the best of our knowledge, this is the first case reported.
Learning points.
Side effects of clomiphene include headache, hot flushes, nausea, dizziness, visual disturbance, weight gain, fluid retention and rarely venous thrombosis.
Cerebral venous thrombosis, though rare, should be considered as a side effect of clomiphene in a patient presenting with headache and blurred vision.
Complete thrombophilia workup should be ordered, and other risk factors should be sought after before clomiphene is considered to be culprit.
Footnotes
Contributors: This case was admitted by MZ from A&E Department and managed as in-patient. AA is junior member of the team and has written this case report along with MZ. AZ and DA-M are senior consultants in our department and have either managed the case or helped in writing this case report.
Competing interests: None declared.
Patient consent: Obtained.
Provenance and peer review: Not commissioned; externally peer reviewed.
References
- 1.Saposnik G, Barinagarrementeria F, Brown RD Jr et al. Diagnosis and management of cerebral venous thrombosis: a statement for healthcare professionals from the American Heart Association/American Stroke Association. Stroke 2011;42(4):1158–92. 10.1161/STR.0b013e31820a8364 [DOI] [PubMed] [Google Scholar]
- 2.Ferro JM, Canhão P, Stam J et al. Prognosis of cerebral vein and dural sinus thrombosis: results of the International Study on Cerebral Vein and Dural Sinus Thrombosis (ISCVT). Stroke 2004;35:664–70. 10.1161/01.STR.0000117571.76197.26 [DOI] [PubMed] [Google Scholar]
- 3.Alonso-Cánovas A, Masjuan J, González-Valcárcel J et al. Cerebral venous thrombosis: when etiology makes the difference. Neurologia 2009;24:439–45. [PubMed] [Google Scholar]
- 4.Allroggen H, Abbott RJ. Cerebral venous sinus thrombosis. Postgrad Med J 2000;76:12–5. 10.1136/pmj.76.891.12 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Hughes E, Brown J, Collins JJ et al. Clomiphene citrate for unexplained subfertility in women. Cochrane Database Syst Rev 2010;(1):CD000057 10.1002/14651858.CD000057.pub2 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Willets AE, Corbo JM, Brown JN. Clomiphene for the treatment of male infertility. Reprod Sci 2013;20:739–44. 10.1177/1933719112466304 [DOI] [PubMed] [Google Scholar]
- 7.Roth LW, Ryan AR, Meacham RB. Clomiphene citrate in the management of male infertility. Semin Reprod Med 2013;31:245–50. 10.1055/s-0033-1345271 [DOI] [PubMed] [Google Scholar]
- 8.Shabsigh A, Kang Y, Shabsign R et al. Clomiphene citrate effects on testosterone/estrogen ratio in male hypogonadism. J Sex Med 2005;2:716–21. 10.1111/j.1743-6109.2005.00075.x [DOI] [PubMed] [Google Scholar]
- 9.Viola MI, Meyer D, Kruger T. Association between clomiphene citrate and visual disturbances with special emphasis on central retinal vein occlusion: a review. Gynecol Obstet Invest 2011;71:73–6. 10.1159/000319497 [DOI] [PubMed] [Google Scholar]
- 10.Lee VY, Liu DT, Li CL et al. Central retinal vein occlusion associated with clomiphene-induced ovulation. Fertil Steril 2008;90:2011 e11–2. 10.1016/j.fertnstert.2008.01.056 [DOI] [PubMed] [Google Scholar]
- 11.Benshushan A, Shushan A, Paltiel O et al. Ovulation induction with clomiphene citrate complicated by deep vein thrombosis. Eur J Obstet Gynecol Reprod Biol 1995;62:261–2. 10.1016/0301-2115(95)02193-B [DOI] [PubMed] [Google Scholar]
- 12.Politou M, Gialeraki A, Merkouri E et al. Central retinal vein occlusion secondary to clomiphene treatment in a male carrier of factor V Leiden. Genet Test Mol Biomarkers 2009;13:155–7. 10.1089/gtmb.2008.0104 [DOI] [PubMed] [Google Scholar]


