Abstract
A man aged 53 years was admitted to our hospital due to general malaise, fever and chills for the past 24 hours. He had a history of chronic alcoholic liver disease. The blood tests showed leucocytosis with neutrophilia, lactic acidosis and acute-phase reactants. The blood cultures were positive for Parvimonas micra, an anaerobic pathogen which is part of the flora of the oral cavity. There was no evidence of abscess formation in either the examination or the imaging tests, but in the work-up that followed, a gastroscopy showed a stenotic oesophageal mass that turned out to be an invasive squamous cell carcinoma.
Background
Parvimonas micra (formerly Peptostreptococcus micros) is a Gram-positive anaerobic cocci species, known to be commensal in the oral cavity. It is related to polymicrobial infections, such as periodontitis and sinusitis,1 and other infections outside the oral mucosa, such as intracranial abscesses, pericarditis and necrotising fasciitis. Despite these infections, anaerobic cocci are sometimes isolated in a pure culture, which is why it is important to take into account the clinical relevance of these microorganisms and be aware of some of the predisposing conditions (immunosuppression, cancer-related conditions, wounds in mucous membranes, etc), in order to establish a proper diagnosis and initiate an appropriate antibiotic treatment.2
Case presentation
A man aged 53 years with a history of alcohol abuse and chronic alcoholic liver disease was admitted to our hospital with general malaise, fever and chills for the past 24 hours. He also had anorexia, asthenia and weight loss. Five years earlier, he had been admitted due to an acute oesophageal variceal haemorrhage. Since then, he had only been taking propranolol 40 mg three times a day. The physical examination revealed thinness, periodontitis and bad breath. His systolic blood pressure was 85 mm Hg, diastolic blood pressure was 60 mm Hg and heart rate was 105 bpm. On auscultation, heart and breath sounds were normal. There was hepatomegaly, but no ascites or leg swelling.
Investigations
Initial laboratory tests showed white cell count of 21 760/μL with 85% neutrophils, haemoglobin level of 16.3 g/dL and platelet count of 93 000/μL. Lactic acidosis and raised inflammatory markers were found: pH 7.26, pCO2 24.5 mm Hg, HCO3 17 mmol/L, arterial lactate 5 mmol/L (normal range: 0.5–1.6 mmol/L), C reactive protein 141 mg/dL (normal range: <5 mg/dL) and procalcitonin 12.12 μL (normal range: <0.05 μL). Liver and kidney functions were normal. Chest X-ray was normal and abdominal ultrasound examination did not show any abscesses or signs of intra-abdominal infection or inflammation. The liver, however, appeared to be cirrhotic.
Blood cultures later revealed P. micra (susceptible to linezolid, vancomycin, penicillin and piperacillin–tazobactam), but empirical intravenous broad-spectrum antibiotic therapy had been started due to signs of sepsis at the time of admission. Urine cultures were normal.
Echocardiogram, which was performed to rule out infective endocarditis, was normal.
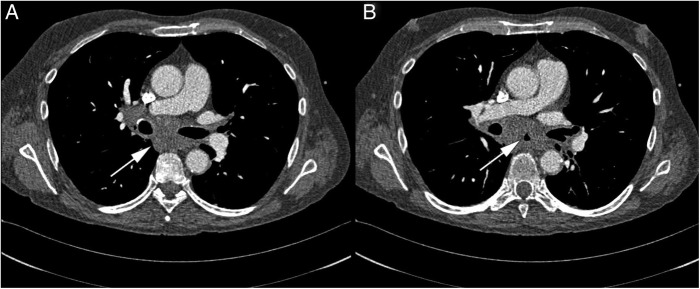
CT scans of the abdomen and pelvis showed a 5×2.8×3 cm mass in the subcarinal region, embracing the distal oesophagus (figure 1). A gastroscopy was therefore performed, which revealed an exophytic ulcerated mass taking up over 70% of the inside circumference of the oesophagus. This mass appeared to be malignant (figure 2). A biopsy of the lesion showed squamous carcinoma of the oesophagus.
Figure 1.
In this CT, both slides show the mass immediately behind the heart, between the two major bronchi. In slide B, the arrow is showing the oesophageal lumen, whereas in slide A, the mass is causing stenosis. The mass embraces pulmonary vessels and the two bronchi.
Figure 2.
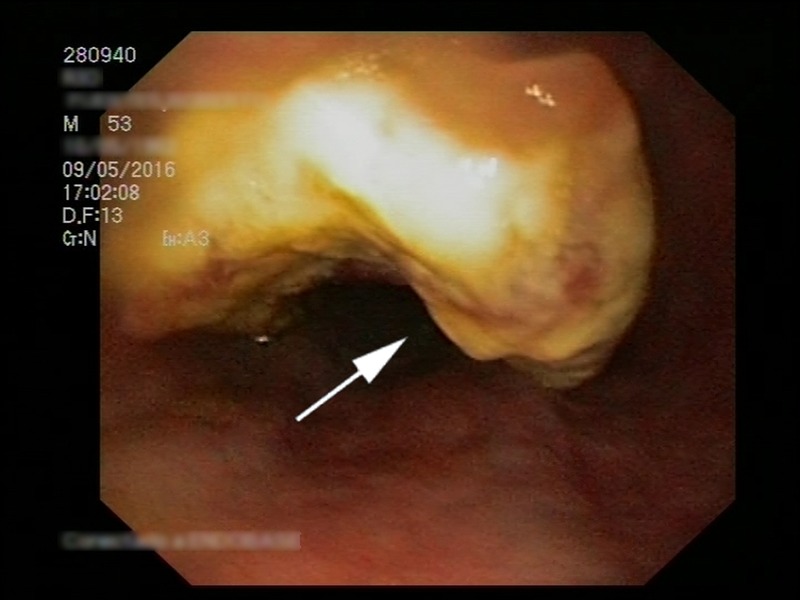
The gastroscopy reveals the exophytic mass, which is occluding the oesophagus.
Treatment, outcome and follow-up
On admission, before the blood culture results were available, the signs and symptoms suggested sepsis with no apparent foci of infection.
APACHE II and SOFA scores were performed in order to assess the severity of the sepsis. The results were 21 and 8 points, respectively.
As mentioned before, an empirical broad-spectrum antibiotic treatment with meropenem 1 g three times a day was therefore started. We noted a rapid improvement in the patient's physical condition, fever clearance and normalisation of inflammatory markers.
Once the blood culture results were available, we consulted the infectious disease department, who recommended that we should continue the antibiotic therapy with meropenem, given the possibility of an overlooked polymicrobial infection. The patient received antibiotic treatment for 14 days.
Regarding the oesophageal tumour, the CT revealed that it was locally advanced. The patient was offered active cancer treatment but decided against it, so he was given palliative care only. Six weeks after diagnosis, the patient passed away.
Discussion
The normal commensal microbiota is colonising the skin and mucosa, which are an otherwise very effective barrier. However, this barrier can be compromised or the patient may be immunosuppressed. In such cases, opportunistic bacteria become pathogenic and can cause severe infections, including soft-tissue infections, brain abscesses, lung, bone, joint and female genital tract infections.3
Anaerobic cocci are isolated from 25% to 30% of blood cultures and tissue samples, but since they are frequently isolated from polymicrobial infections, their clinical role sometimes remains uncertain.3 Over the last decade, there have been several case reports related to anaerobic bacteria, either bacteraemia or severe infections, presumably due to more complex patients and the improvement of microbiological techniques.4 As such, the clinical relevance of anaerobic infections is becoming increasingly important. Anaerobic cocci have presumably been insufficiently studied and their clinical significance has therefore been overlooked.
Parvimonas micra was formerly known as Pe. micros and was reclassified as P. micra in 2006.5 It is a normal commensal pathogen of the gingival and gastrointestinal tract, known for causing periodontitis and other infections of the oral cavity.6 However, it has also been related to extraoral cavity infections, such as chronic wounds, leg ulcers, lung abscesses, endocarditis and diabetic foot infections.3 Some predisposing conditions (immunosuppression, cancer, diabetes mellitus, haematological disorders, skin and mucosal damage) can make P. micra pathogenic and cause bacteraemia or opportunistic infections, such as purulent pericarditis in immunosuppressed patients.7
Our patient had poor oral hygiene and presumably periodontal disease. Indeed, several case reports involve the presence of previous periodontitis with spondylodiscitis due to P. micra.8
But more importantly, there was a relevant underlying condition: locally advanced carcinoma of the oesophagus, which might have played a significant role in the P. micra infection. A paper has been recently published, in which a patient with advanced adenocarcinoma of the rectum presented with necrotising fasciitis9 caused by a polymicrobial infection, and P. micra was involved (it was, however, reported as Pe. micros). It is reasonable to believe that these underlying diseases (periodontal disease, alcohol-use disorder, liver cirrhosis, oesophageal tumour) predisposed the patient to present with bacteraemia caused by P. micra.
While P. micra bacteraemia in the immunocompromised patient might not be so rare, bacteraemia due to possible translocation in patients with stomach cancer can be acceptable as a predisposing condition.
Sometimes, anaerobic bacteria cannot be isolated from conventional tissue or blood cultures, but there are some new identification techniques that can prevent these infections from being overlooked, such as 16S rRNA gene sequencing or multiplex PCR assay.3 10 Along with the isolation in pure cultures, these new techniques should help us to take into account the clinical relevance of infections due to commensal organisms.
SOFA and APACHE scores11 were performed to assess the severity of the sepsis, along with the mentioned laboratory test. The overall mortality rate of anaerobic bacteraemia is high (15–35%), so antibiotic therapy must be started when an anaerobic infection is suspected.2 Parvimonas micra is highly susceptible to antibiotics, as depicted in our patient. If an abscess or a source of infection is identified, surgical drainage is compulsory. However, we were unable to detect the primary site of the infection.
Learning points.
Parvimonas micra is an anaerobic organism which can become an opportunistic pathogen in certain conditions.
Neoplasms, diabetes mellitus, decubitus ulcers, cirrhosis, surgical wounds, haematological disorders and immunosuppression conditions are the main underlying causes of bacteraemia, sepsis or serious anaerobic infections. Clinicians should be aware of these opportunistic organisms in patients at high risk.
Along with the severity of the infection, the underlying conditions may pose a risk of severe complications or a fatal outcome.
Even when patients do not have apparent foci of infection, these predisposing conditions should make us consider occult bacteraemia in febrile patients and recommend hospitalisation for empirical antibiotic therapy. This treatment should not be delayed if severe sepsis is suspected. Surgical drainage is compulsory when an abscess is present.
Footnotes
Twitter: Follow Rafael García Carretero at @rafa_linux
Contributors: RGC wrote the first draft; EL-H and MO-V made interesting suggestions; OV-G helped in the translation into English.
Competing interests: None declared.
Patient consent: Obtained.
Provenance and peer review: Not commissioned; externally peer reviewed.
References
- 1.Shchipkova AY, Nagaraja HN, Kumar PS. Subgingival microbial profiles of smokers with periodontitis. J Dent Res 2010;89:1247–53. 10.1177/0022034510377203 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Brook I. Anaerobic infections in children. Adv Exp Med Biol 2011;697:117–52. 10.1007/978-1-4419-7185-2_10 [DOI] [PubMed] [Google Scholar]
- 3.Murphy EC, Frick IM. Gram-positive anaerobic cocci—commensals and opportunistic pathogens. FEMS Microbiol Rev 2013;37:520–53. 10.1111/1574-6976.12005 [DOI] [PubMed] [Google Scholar]
- 4.Lassmann B, Gustafson DR, Wood CM et al. . Reemergence of anaerobic bacteremia. Clin Infect Dis 2007;44:895–900. 10.1086/512197 [DOI] [PubMed] [Google Scholar]
- 5.Tindall BJ, Euzeby JP. Proposal of Parvimonas gen. nov. and Quatrionicoccus gen. nov. as replacements for the illegitimate, prokaryotic, generic names Micromonas Murdoch and Shah 2000 and Quadricoccus Maszenan et al. 2002, respectively. Int J Syst Evol Microbiol 2006;56(Pt 11):2711–13. [DOI] [PubMed] [Google Scholar]
- 6.Belstrøm D, Fiehn NE, Nielsen CH et al. . Differentiation of salivary bacterial profiles of subjects with periodontitis and dental caries. J Oral Microbiol 2015;7:27429 http://www.ncbi.nlm.nih.gov/pmc/articles/PMC4390560/ [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Taylor GK, Elliott L, Sosin MD et al. . Complication of etanercept treatment for rheumatoid arthritis—purulent pericarditis caused by a commensal organism. BMJ Case Rep 2012;2012:bcr0120125644 10.1136/bcr.01.2012.5644 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Uemura H, Hayakawa K, Shimada K et al. . Parvimonas micra as a causative organism of spondylodiscitis: a report of two cases and a literature review. Int J Infect Dis. 2014;23:53–5. 10.1016/j.ijid.2014.02.007 [DOI] [PubMed] [Google Scholar]
- 9.Ferreira L, Alexandrino H, Soares Leite J et al. . Locally advanced adenocarcinoma of the rectum presenting with necrotising fasciitis of the perineum: successful management with early aggressive surgery and multimodal therapy. BMJ Case Rep 2015;2015:bcr2015213245 10.1136/bcr-2015-213245 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Woo PCY, Teng JLL, Yeung JMY et al. . Automated identification of medically important bacteria by 16S rRNA gene sequencing using a novel comprehensive database, 16SpathDB. J Clin Microbiol 2011;49:1799–809. 10.1128/JCM.02350-10 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Wang JY, Chen YX, Guo SB et al. . Predictive performance of quick Sepsis-related Organ Failure Assessment for mortality and ICU admission in patients with infection at the ED. Am J Emerg Med 2016;34:1788–93. 10.1016/j.ajem.2016.06.015 [DOI] [PubMed] [Google Scholar]