Abstract
Background
The risk of ischaemic heart disease (IHD) is largely influenced by lifestyle. Interestingly, cohort studies show that anxiety in general is associated with increased risk of IHD, independent of established risk factors for cardiovascular disease. Health anxiety is a specific type of anxiety characterised by preoccupation of having, acquiring or possibly avoiding illness, yet little is known about lifestyle and risk of disease development in this group.
Aim
Investigate whether health anxiety is prospectively associated with IHD, and whether a potential association can be explained by the presence or absence of established risk factors for cardiovascular diseases.
Methods
Incident IHD was studied among 7052 participants in the community-based Hordaland Health Study (HUSK) during 12 years follow-up by linkage to the Cardiovascular Diseases in Norway (CVDNOR) project. Scores above 90th centile of the Whiteley Index defined health anxiety cases. Associations were examined with the Cox proportional regression models.
Results
During follow-up, 6.1% of health anxiety cases developed IHD compared with 3.0% of non-cases, yielding a gender-adjusted HR of 2.12 (95% CI 1.52 to 2.95). After adjustments for established cardiovascular risk factors, about 70% increased risk of IHD was found among cases with health anxiety (HR: 1.73 (95% CI 1.21 to 2.48)). The association followed a dose–response pattern.
Conclusions
This finding corroborates and extends the understanding of anxiety in various forms as a risk factor for IHD. New evidence of negative consequences over time underlines the importance of proper diagnosis and treatment for health anxiety.
Keywords: Health anxiety, Ischemic heart disease, EPIDEMIOLOGY
Strengths and limitations of this study.
This prospective cohort study ensured complete follow-up of participants in a community-based health survey due to linkage with a nationwide cardiovascular research project.
The exposure health anxiety was assessed by self-report with the Whiteley Index (WI), while the outcome ischaemic heart disease (IHD) was reported by physicians via patient administrative systems in hospitals or at death certificates.
WI do not discern between ‘imagined’ illness or more legitimate reasons for concern. To reduce the impact of high levels of health anxiety due to actual illness, participants with prevalent or 12 months incident IHD were excluded.
Low participation rate at the community-based health survey of 63%, representing a greater threat to the validity of studies estimating prevalence rather than risks.
Health anxiety is characterised by persistent preoccupation of having or acquiring a serious illness, misattribution of bodily symptoms and urge to seek medical advice in the absence of physical pathology.1 2 As a result, persons with health anxiety stay activated and alert to bodily symptoms in order to detect, or even avoid, illness. Symptoms of health anxiety may range from trivial to severe, and in the most intense form including disease conviction, the diagnostic criteria for hypochondriasis might be met.3 As the leading cause of premature death in Norway,4 as well as in many other middle to high-income countries, ischaemic heart disease (IHD) is reasonably a frequent subject of concern among persons with health anxiety.5 The risk of IHD is largely influenced by health behaviours, and it has been estimated that close to 90% of the burden of cardiovascular diseases worldwide could be avoided with healthier lifestyle in terms of diet, reduction in tobacco consumption and increased level of physical activity.6
Anxiety disorders and IHD have several symptoms in common, such as chest discomfort, palpitations, nausea, sweating and tachypnoea. Additionally, anxiety disorders in general are associated with increased risk of IHD.7 8 Following almost 250 000 persons for an average of 11 years, a meta-analysis from 2010 estimated 26% increased risk of coronary heart disease among persons with anxiety, independent of demographics, biological factors and health behaviours.8 This analysis relied on an overall heterogeneous measure of anxiety, counting single studies using instruments assessing generalised anxiety disorders, worry, panic attacks and phobic disorders. The authors concluded that anxiety should be regarded as an independent risk factor for coronary heart disease, and that future research ought to confirm the association using other valid and reliable measures of anxiety. Certainly, the issue of causality between anxiety and IHD has been of great interest, and a recent meta-analysis provided evidence supporting a causal association between anxiety and cardiovascular diseases in general, suggesting anxiety to be targeted in preventive cardiology.9
Whether an increased risk of IHD also applies to persons suffering from health anxiety has, to the best of our knowledge, not been examined. Safety-seeking behaviour such as monitoring and frequent check-ups of symptoms associated with heart disease may contribute to a reduced risk of IHD in health anxiety compared with anxiety in general. Further, one could hypothesise that individuals with health anxiety, due to their health concerns, endorse a lifestyle that reduces the risk of IHD. Yet, little is known about health-related behaviours such as smoking, physical activity and alcohol consumption in this group.
By linking a community-based health study with information on hospitalisations and death due to IHD, the aims of the present study were to examine (1) whether health anxiety is prospectively associated with incident IHD and (2) whether a potential association can be explained by the presence or absence of established risk factors for cardiovascular diseases.
Methods
Study population: the Hordaland Health Study
The Hordaland Health Study (HUSK) is a community-based health survey with baseline examinations conducted during 1997–1999 as a collaboration between the National Health Screening Service, the University of Bergen and local health services.10 All persons born 1953–1957 who resided in Hordaland County on 31 December 1997 (n=29 400) received a personal invitation to participate in the study. Data collection encompassed two sets of questionnaires and one brief physical examination at which weight, height and blood pressure were measured and a blood sample was drawn. Questionnaire 1 was included with the mailed invitation to participate in the study and was collected at the health examination, during which participants randomly were given one of two versions of questionnaire 2 to be filled in at home and returned by mail. Participation rate at the health examination was 63%. Of these, about 85% returned the second questionnaire. Persons who did not meet at the examination or did not return the second questionnaire received one reminder by mail.
Exposure: health anxiety measured by Whiteley Index
The presence of health anxiety was assessed by the Whiteley Index (WI). Developed by Pilowsky11 in the 1960s, this widely used self-report instrument is considered a classic screening tool for health anxiety and hypochondriasis.12 The index consists of 14 items, each scored from 1 to 5, aiming to assess the disease dimensions phobia, somatic preoccupation and disease conviction. However, the three-dimensional factor structure has been questioned in later studies,13 and the use of a one-factor solution summarising the scores on all items is recommended and widely used.13 The internal consistency, stability and concurrent validity of WI is considered to be good, both in samples from medical outpatient clinics, general practice and the general population.13 In the present study, scores for each of the 14 items were summarised and the 90th centile was used as a cut-off for cases of health anxiety, corresponding to the highest prevalence estimate of illness anxiety disorder in the general population reported in the DSM-V.1 In additional analyses, scores on WI were operationalised in quintiles and as a continuous variable.
Outcome: IHD
The research project ‘Cardiovascular diseases in Norway 1994–2009’ (CVDNOR) is a collaboration between the University of Bergen and the Norwegian Knowledge Center for the Health Services, and has retrospectively collected data on hospitalisations and deaths due to CVD during 1994–2009.14 15 In brief, data on hospital stays coded with a CVD diagnosis as main or secondary diagnoses were retrieved from the electronic Patient Administrative System (PAS) in all Norwegian somatic hospitals, while information on persons with a CVD diagnosis on the death certificate, regardless of whether they had been hospitalised for a CVD-related diagnosis, was obtained from the Norwegian Cause of Death Registry. Data quality is considered good.16 The main outcome in the present study was incident IHD diagnosed at least 1 year after participation in HUSK and until 31 December 2009, defined as a primary or secondary diagnosis or underlying cause of death with ICD-10 code I20–I25.17 Participants in HUSK were linked with CVDNOR through their personal identification number, unique to each Norwegian resident.
Covariates
Based on knowledge of established risk factors for IHD,18 we adjusted the analyses for several covariates assessed at baseline in HUSK. Information on gender and age was obtained from the Norwegian Population Registry. Based on self-reported information, we defined persons as cohabiting if they had reported marital status as ‘married’ or ‘partner’, highest achieved education was categorised as ‘college or university’, ‘high school’ or ‘less than high school’. The number of alcohol units per 14 days was categorised according to tertiles in 0, 1–5 and ≥6 units, whereas physical activity was categorised as mean hours with hard physical activity per week ranging from 0 to ≥3, defined as perspirating and being out of breath. Self-reported information on smoking was categorised as never, former and current. Height and weight were measured at the examination, body mass index (BMI) was calculated as weight (kg)/height (m)2, and categorised as underweight (≤19.9), normal (20.0–24.9), overweight (25.0–29.9) and obese (≥30). Systolic blood pressure (mm Hg), total cholesterol (mg/dL) and HDL (mg/dL) were measured at the examination, and categorised in quintiles. Additionally, we utilised self-reported data on the presence of diabetes and first-degree relative with acute myocardial infarction (AMI) before 60 years.
Study sample and statistical procedures
The population eligible for inclusion in this study was participants answering the WI, included in V.1 of questionnaire 2 in HUSK (n=7113). A total of 794 (11.2%) participants had missing information on ≥1 of the 14 items on the WI. In the main analyses, participants responding on 9–13 items of the index were given imputed values equal to the mean score of the items with valid responses (n=773), while persons with <9 valid responses were excluded from the sample (n=21). To reduce the risk of reverse causality due to high levels of health anxiety among persons with prevalent and early-onset incident IHD, we excluded persons who had been hospitalised due to IHD from 1994 until participation in HUSK (n=30), as well as participants who were hospitalised or died due to IHD during the first 12 months after the HUSK baseline examination (n=10). This yielded a final sample of 7052 participants who were followed from baseline until hospitalisation or death, or until 31 December 2009, with a maximum follow-up of 12 years. In a sensitivity analysis of the effect of non-response, only persons with complete responses on all 14 items on the WI were included (n=6279). A recent confirmatory factor analysis (CFA) and item response theory analysis using baseline data from HUSK argued against the use of the 14-item WI as it did not yield a satisfactory CFA fit, and suggested the use of a 6-item one-factor solution.19 Accordingly, a sensitivity analysis summarising only the 6 recommended items with cut-off at score equal to the 90th centile was conducted.
The distribution of covariates by cases of health anxiety was examined using descriptive statistics. Associations between health anxiety and incident IHD were examined using the Cox proportional regression analyses in four models adjusted for (1) gender, (2) gender, cohabiting and education (sociodemographic factors), (3) gender, alcohol consumption, physical activity, diabetes, BMI, first-degree relative with AMI before 60 years, smoking, total cholesterol, HDL cholesterol and systolic blood pressure (CVD risk factors) and (4) all factors combined. The analyses were repeated stratified by gender. Effect estimates are presented as HRs with 95% CIs. To visually explore the association between health anxiety and risk of IHD, we used the Cox proportional hazards regression model fitting WI scores using restricted cubic splines with three knots.20 Listwise deletion was employed for cases with missing information on the covariates in the multivariate analyses (between 0% and 20%). All analyses were conducted in SPSS (IBM Corp. Released 2013. IBM SPSS Statistics for Windows VA, New York: IBM Corp), and figures were constructed in Stata (StataCorp. 2013. Stata Statistical Software: Release V.13. College Station TSL).
Ethics
The study protocol was approved by the Regional Ethics Committee of Western Norway (REK) (ref 2013/1764) and the Norwegian Data Inspectorate. The linkage between HUSK and CVDNOR was approved by REK. Written informed consent was obtained from all participants at the time of the baseline health examination.
Results
Participants who scored ≥31 on WI constituted the 90th centile and were defined as cases with health anxiety. Among these, the mean WI score was 36.8 (SE 0.22), while the mean score among non-cases was 20.9 (SE 0.05). Health anxiety was positively associated with disadvantageous responses on most of the a priori selected risk factors for IHD, except for lower than usual alcohol consumption. No differences in the distribution of systolic blood pressure were found (table 1).
Table 1.
Characteristics of 7052 participants in the Hordaland Health Study (HUSK) without prevalent or 12-month incident ischaemic heart disease (hospitalisation or death with I20–I25)
| Non-cases health anxiety* N=6342 (%) |
Cases health anxiety† N=710 (%) |
p Value for difference | |
|---|---|---|---|
| Age‡ | 43.1 (1.55) | 43.2 (1.61) | 0.005§ |
| Missing | 0 (0) | 0 (0) | |
| Gender (male) | 3305 (52.1) | 361 (50.8) | 0.521¶ |
| Missing | 0 (0) | 0 (0) | |
| Cohabiting | 4754 (75.0) | 470 (66.2) | <0.001¶ |
| Missing | 0 (0) | 0 (0) | |
| Education | |||
| Less than high school | 1035 (16.3) | 168 (23.7) | <0.001¶ |
| High school | 2939 (46.3) | 323 (45.5) | |
| College or university | 2318 (36.5) | 213 (30.0) | |
| Missing | 50 (0.8) | 6 (0.8) | |
| Usual alcohol consumption per 14 days (units) | |||
| 0 | 1587 (25.0) | 197 (27.7) | 0.008¶ |
| 1–5 | 1744 (27.5) | 159 (22.4) | |
| ≥6 | 1765 (27.8) | 191 (26.9) | |
| Missing | 1246 (19.6) | 163 (23.9) | |
| Activity (hours per week) | |||
| 0 | 1704 (26.9) | 231 (32.5) | 0.002¶ |
| <1 | 1704 (26.9) | 204 (28.7) | |
| 1–2 | 1789 (28.2) | 174 (24.5) | |
| ≥3 | 919 (14.5) | 77 (10.8) | |
| Missing | 226 (3.6) | 24 (3.4) | |
| Diabetes (yes) | 61 (1.0) | 15 (2.1) | 0.006¶ |
| Missing | 34 (0.5) | 7 (1.0) | |
| First-degree relative with AMI before 60 years of age (yes) | 957 (15.1) | 128 (18.0) | 0.004¶ |
| Missing or unknown | 196 (3.1) | 34 (4.8) | |
| BMI | |||
| ≤19.9 | 254 (4.0) | 32 (4.5) | 0.011¶ |
| 20.0–24.9 | 2909 (45.7) | 285 (40.1) | |
| 25.0–29.9 | 2476 (39.0) | 288 (40.6) | |
| ≥30.0 | 704 (11.1) | 103 (14.5) | |
| Missing | 7 (0.1) | 2 (0.3) | |
| Total cholesterol quintiles (mg/dL) | |||
| 1st (<183.7) | 1265 (20.0) | 133 (18.8) | 0.552¶ |
| 2nd (≥183.7, <202.3) | 1262 (19.9) | 141 (19.9) | |
| 3rd (≥202.3, <221.2) | 1262 (19.9) | 141 (19.9) | |
| 4th (≥221.2, <244.8) | 1282 (20.2) | 134 (18.9) | |
| 5th (≥244.8) | 1261 (19.9) | 159 (22.5) | |
| Missing | 11 (0.2) | 2 (0.3) | |
| HDL quintiles (mg/dL) | |||
| 1st (<37.0) | 1173 (18.5) | 172 (24.3) | <0.001¶ |
| 2nd (≥37.0, <43.0) | 1235 (19.5) | 153 (21.6) | |
| 3rd (≥43.0, <49.5) | 1302 (20.6) | 136 (19.2) | |
| 4th (≥49.5, <58.1) | 1279 (20.2) | 126 (17.8) | |
| 5th (≥58.1) | 1342 (21.2) | 121 (17.1) | |
| Missing | 11 (0.2) | 2 (0.3) | |
| Systolic BP quintiles (mm Hg) | 128.5 (0.17) | 128.3 (0.53 | |
| 1st (<116.7) | 1247 (19.9) | 155 (22.2) | 0.536¶ |
| 2nd (≥116.7, <123.7) | 1247 (19.9) | 134 (19.2) | |
| 3rd (≥123.7, <130.3) | 1189 (19.0) | 119 (17.0) | |
| 4th (≥130.3, <139.0) | 1129 (20.6) | 143 (20.5) | |
| 5th (≥139.0) | 1288 (20.6) | 147 (21.1) | |
| Missing | 16 (0.3) | 2 (0.3) | |
| Smoking | |||
| Current | 2488 (39.2) | 341 (48.0) | <0.001¶ |
| Former | 1783 (28.1) | 187 (26.3) | |
| Never | 2064 (32.5) | 181 (25.5) | |
| Missing | 7 (0.1) | 1 (0.1) | |
*Score under 90th centile (<31 points) of Whiteley Index.
†Score equal to or above 90th centile (≥31 points) of Whiteley Index.
‡Mean (st.dev).
§Independent samples t-test.
¶Pearson χ2.
After excluding persons with an ischaemic heart event (hospitalisation or death) occurring the first year after baseline, 234 (3.3%) participants had an ischaemic heart event during follow-up, 6.1% of cases compared with 3.0% of non-cases. The mean time to event was 7.3 years (SE 2.91). Gender-adjusted HR for the association between cases of health anxiety and an incident IHD event was 2.12 (95% CI 1.52 to 2.95) (table 2). Established CVD risk factors explained part of the association; however, the fully adjusted model showed 73% increased risk of incident IHD among cases with health anxiety (table 2). Among the included single risk factors, separate adjustments for smoking, HDL cholesterol and education attenuated the association most (data not shown). Gender-stratified analyses gave slightly higher effect estimates for women than men (table 2), but no significant gender interaction was found. Further, the association between health anxiety and IHD was no longer significant for women after adjustments for CVD risk factors and all covariates combined.
Table 2.
HRs for incident ischemic heart disease (IHD) comparing cases with and without health anxiety*
| Total sample (n=7052) | Men (n=3666) | Women (n=3386) | |
|---|---|---|---|
| 234 (3.3) | 173 (4.7) | 61 (1.8) | |
| N events (%) | HR (95% CI) | HR (95% CI) | HR (95% CI) |
| Adjusted for gender | 2.12 (1.52 to 2.95) | 2.09 (1.42 to 3.09) | 2.19 (1.16 to 4.11) |
| Adjusted for sociodemographic factors† | 2.00 (1.43 to 2.79) | 1.93 (1.30 to 2.86) | 2.14 (1.14 to 4.04) |
| Adjusted for CVD risk factors‡ | 1.73 (1.22 to 2.47) | 1.79 (1.18 to 2.71) | 1.61 (0.80 to 3.25) |
| Adjusted for all covariates§ | 1.73 (1.21 to 2.48) | 1.78 (1.17 to 2.71) | 1.58 (0.78 to 3.20) |
IHD were events occurring 1–12 years after baseline participation in the Hordaland Health Study (HUSK). Estimates are adjusted separately for blocks of covariates and all covariates combined.
*Score equal to or above 90th centile of Whiteley Index (≥31 points).
†Gender, cohabiting and education.
‡Gender, alcohol consumption, physical activity, diabetes, BMI, first-degree relative with AMI before 60 years, smoking, total cholesterol, HDL cholesterol, systolic blood pressure.
§Gender, cohabiting, education, alcohol consumption, physical activity, diabetes, BMI, first-degree relative with AMI before 60 years, smoking, total cholesterol, HDL cholesterol, systolic blood pressure.
Restricting these analyses to participants with complete responses on all the WI items yielded similar results for the association between health anxiety and incident IHD (gender-adjusted HR: 2.19 (95% CI 1.57 to 3.07), fully adjusted HR: 1.80 (95% CI 1.25 to 2.59)). Although sensitivity analysis including only the 6 items on the WI previously shown to yield the best factor structure19 slightly attenuated the strength of the association, this analysis also confirmed that high levels of health anxiety was significantly associated with incident IHD (gender-adjusted HR: 1.83 (95% CI 1.29 to 2.59), fully adjusted HR: 1.50 (95% CI 1.03 to 2.18)).
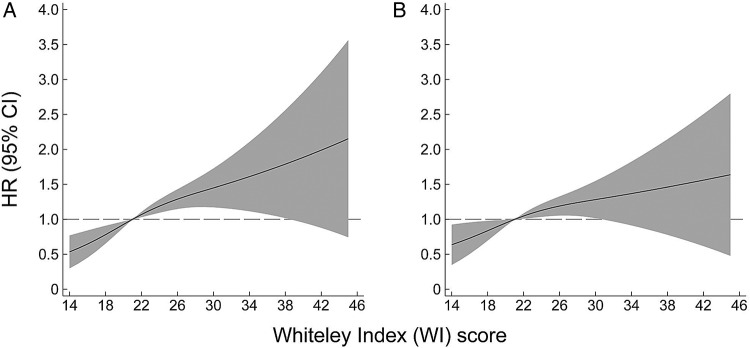
Operationalising scores on the WI in quintiles and as a continuous variable revealed a dose–response pattern of the association (table 3 and figure 1). A significant trend with increased strength of the association by increasing scores on WI was found in all four models (table 3), while figure 1 revealed a linear association between scores on WI and subsequent risk of IHD, in the gender adjusted (part A) and fully adjusted models (part B).
Table 3.
HR for incident ischaemic heart disease events 1–12 years after baseline participation in the Hordaland Health Study (HUSK) by quintiles of Whiteley Index
| N=7052 | Quintiles of Whiteley Index (corresponding scores on Whiteley Index) |
p Value for trend | ||||
|---|---|---|---|---|---|---|
| 1st (14–16) | 2nd (17–19) | 3rd (20–22) | 4th (23–25) | 5th (≥26) | ||
| N events (%) | 16 (1.7) | 48 (2.9) | 43 (3.0) | 58 (3.7) | 69 (4.6)) | |
| HR (95% CI) | HR (95% CI) | HR (95% CI) | HR (95% CI) | HR (95% CI) | <0.001* | |
| Adjusted for gender | (ref) | 1.82 (1.04 to 3.21) | 1.95 (1.10 to 3.47) | 2.43 (1.40 to 4.23) | 3.06 (1.78 to 5.28) | <0.001 |
| Adjusted for gender and sociodemographic factors† | (ref) | 1.83 (1.04 to 3.22) | 1.94 (1.09 to 3.44) | 2.34 (1.34 to 4.07) | 2.86 (1.66 to 4.94) | <0.001 |
| Adjusted for CVD risk factors‡ | (ref) | 1.67 (0.93 to 3.00) | 1.70 (0.93 to 3.09) | 2.14 (1.21 to 3.80) | 2.36 (1.33 to 4.17) | 0.001 |
| Adjusted for all covariates§ | (ref) | 1.66 (0.93 to 2.99) | 1.71 (0.94 to 3.11) | 2.13 (1.20 to 3.78) | 2.35 (1.33 to 4.16) | 0.002 |
Estimates are adjusted separately for blocks of covariates and all covariates combined.
*Linear by linear association.
†Gender, cohabiting and education.
‡Gender, alcohol consumption, physical activity, diabetes, BMI, first-degree relative with AMI before 60 years, smoking, total cholesterol, HDL cholesterol, systolic blood pressure.
§Gender, cohabiting, education, alcohol consumption, physical activity, diabetes, BMI, first-degree relative with AMI before 60 years, smoking, total cholesterol, HDL cholesterol, systolic blood pressure.
Figure 1.
Associations (HRs) between score on Whiteley Index and risk of incident ischaemic heart disease events 1–12 years after participation in the Hordaland Health Study (HUSK). Score on Whiteley. Index is fitted using restricted cubic splines with three knots in the Cox proportional hazard regression models. Solid line represents HR and shaded area 95% CI. (A) Model adjusted for gender only. (B) Fully adjusted model, including gender, cohabiting, education, alcohol consumption, physical activity, diabetes, BMI, first-degree relative with AMI before 60 years, smoking, total cholesterol, HDL cholesterol, systolic blood pressure.
Health anxiety often exist comorbid to other psychiatric disorders, such as general anxiety and depression.21 Additionally, regarded as an anxiety disorder, health anxiety obviously shares many features with anxiety in general, and a sharp distinction between the conditions is difficult to draw. Nevertheless, in an attempt to investigate a possible more specific effect of health anxiety on risk of IHD, we conducted post hoc analyses adjusting for the presence of anxiety and depression at baseline in HUSK measured by the Hospital Anxiety and Depression Scale, subscale for anxiety (HADS-a) and depression (HADS-d).22 Cases with health anxiety had the mean HADS-a and HADS-d of 8.01 (SE: 0.15) and 5.54 (SE: 0.16), while non-cases scored 4.27 (SE 0.04) and 2.89 (SE 0.36), respectively. The Pearson's correlation coefficient between WI and HADS-a and Hads-d were 0.48 (p=0.00) and 0.37 (p=0.00), respectively. HR for the association between health anxiety and IHD adjusted for gender and HADS-a was 1.65 (95% CI 1.14 to 2.38), corresponding HR adjusted for gender and HADS-d was 1.89 (95% CI 1.33 to 2.59), while the HR adjusted for gender and HADS-a and HADS-d was 1.64 (95% CI 1.14 to 2.37). However, adding measures of anxiety to the fully adjusted model outlined in tables 2 and 3 resulted in a no longer significant association between health anxiety and IHD, evident from an HR of 1.33 (95% CI 0.90 to 1.98) for the fully adjusted model in addition to adjustments for HADS-a and HR of 1.31 (95% CI 0.88 to 1.97) for the fully adjusted model in addition to adjustments for HADS-a and HADS-d. Including adjustments of HADS-d only to the previously fully adjusted model yielded an HR of 1.56 (95% CI 1.06 to 2.28).
Discussion
Using self-reported information on health anxiety from a community-based study linked with data on hospitalisations and death, we found a dose–response association between increasing levels of health anxiety and risk of incident IHD. Relative to persons with lower levels of health anxiety, persons with health anxiety defined as scores on the WI equal to or above the 90th centile had ∼70% increased risk of incident IHD events after adjustment for established CVD risk factors. The finding was confirmed in sensitivity analyses according to a recent CFA and when solely including persons with complete responses on the exposure variable.
Health anxiety and risk factors for IHD
Relative to persons with low levels of health anxiety, persons with high levels reported less hours of hard physical activity per week, higher prevalence of smoking, yet fewer units of alcohol consumed on average per week. With the exception of an Australian population-based study showing approximately twofold odds of current smoking among participants with health anxiety,21 health behaviours in health anxiety are sparsely examined. Lower levels of hard physical activity could possibly be explained by fear of forcing or putting strain on the body, while the divergent results on substance use in terms of higher levels of smoking yet lower levels of alcohol use are more difficult to explain. One may speculate that smoking can be used as a tranquillizer in an attempt to relieve tension, while the use of alcohol reduces bodily control, and is therefore perhaps more often avoided among persons with health anxiety.
Health anxiety and incident IHD
Several studies have established a prospective association between anxiety disorders and IHD,7 8 and there is evidence of a causal association between anxiety and cardiovascular diseases.9 Findings from the Norwegian longitudinal Nord-Trøndelag Health Study (HUNT) suggest a possible dose–response pattern between anxiety, measured by the anxiety subscale of the Hospital Anxiety and Depression Scale, and incident myocardial infarction.23 However, in that study, the association was fully explained by adjusting for gender, age, cohabiting, education, smoking, physical activity, BMI, total cholesterol, diabetes and systolic blood pressure.23 This contrasts our finding of a dose–response association between increasing levels of health anxiety and IHD persisting after adjustments for a range of established CVD risk factors.
The novel finding of an association between health anxiety and incident IHD is in line with, but additionally extends, the current understanding of anxiety as an independent risk factor for incident IHD and cardiac mortality.8 It further indicates that characteristic behaviour among persons with health anxiety, such as monitoring and frequent check-ups of symptoms, does not reduce the risk of IHD events. The persistent and exaggerated attention to symptoms may rather contribute to continuous and high activation of the hypothalamic–pituitary–adrenal axis, placing strain on bodily systems and, in turn, increasing the risk of cardiovascular diseases. Reduced heart rate variability and acceleration of the atherosclerotic process has been suggested as mechanisms possibly explaining the increased risk of IHD among persons with anxiety.24 25 In a French study investigating over 700 persons free of coronary artery disease at baseline, high levels of anxiety was associated with an almost twofold increase in thickness of the intima media of the carotid arteries, as well as more than threefold increased risk of plaque occurrence during 4 years of follow-up.24
In the gender-stratified analyses in table 2, the association between health anxiety and IHD was no longer significant for women after adjustments for established CVD risk factors. This finding must be interpreted with caution, as no significant gender interaction was found. Further, no previous studies on the prospective association between anxiety and risk of IHD or cardiovascular diseases have, to the best of our knowledge, found evidence of effect modification by gender.8 9 23 In the general population, women develop IHD one decade later in life compared with men.26 Thus, our findings are likely explained by the expected low event rate of IHD for women in this relatively young cohort of participants followed from their 40s into early 60s, resulting in wider CIs and non-significant associations when including numerous covariates in the more adjusted models.
Limitations
Despite a prospective design linking a community-based health survey with comprehensive information on subsequent hospitalisations and death ensuring complete follow-up of participants, this study is also affected by limitations. First, even though the WI is a validated and frequently used instrument to assess health anxiety, it relies on self-reported symptoms and does not discern between health anxiety due to ‘imagined’ illness or more legitimate reasons for concern, such as known risk for IHD. We tried to reduce the impact of high levels of health anxiety due to actual illness by excluding participants with prevalent and 12 months incident IHD. As the CVDNOR project spans the years 1994–2009, we could not exclude participants in HUSK diagnosed with IHD earlier than 1994; however, we argue that this represents a minor bias as the prevalence of IHD among persons younger than 40 years of age is very low.26 Further, if the atherosclerotic process precedes health anxiety, our results might be affected by residual confounding as we lack data in HUSK on subclinical IHD and atherosclerosis. Arguing against this, a Swedish cohort of close to 50 000 men aged 18–20 years examined for military service, presumably before start of the atherosclerotic process, confirmed that anxiety present in early adulthood independently predicted subsequent coronary heart disease.7 Second, low participation rate and non-participation always challenges the generalisability of results from population-based studies. A previous study of the HUSK population showed higher risk of being awarded disability pension for neurotic, stress-related or somatoform disorders as well as for diseases in the circulatory system among nonparticipants.27 In general, non-participation represents a greater threat to the validity of results from studies estimating prevalence rather than risks, and we argue that this is a minor threat to the internal validity of our results; nevertheless, an underestimation of the true association cannot be excluded. Third, health anxiety was associated with established risk factors for IHD such as diabetes, lower levels of education and living alone. These covariates may be confounders for the association between health anxiety and IHD, and were therefore adjusted for in the analyses. However, some of them may also be regarded as mediators in the association, as disadvantageous lifestyle, living without a partner and low educational level could be the result of anxiety earlier in life. By adjusting for such possible mediators, our estimates of the association between health anxiety and IHD will represent an underestimation of the true association. Fourth, we did not have information on a range of additional conditions that are likely to be associated with both health anxiety and increased risk of IHD, such as, for example, pulmonary diseases and malignancies. As a result, residual confounding cannot be ruled out. Finally, a sharp distinction between health anxiety and other psychiatric conditions is challenging to draw, as health anxiety often exists comorbid to other psychiatric disorders,21 and, regarded an anxiety disorder, obviously shares many features of anxiety in general. To reduce the risk of overadjustments, we decided against including measures of anxiety and depression in the main model of this study as symptoms of health anxiety correlate to a large extent with symptoms of these conditions. This is particularly evident for anxiety in general, reflected in the relatively strong correlation between WI and HADS-a likely explaining the no longer significant finding between health anxiety and IHD when including measures of anxiety in the fully adjusted model.
Implications
Persons with high levels of health anxiety have about 70% increased risk of IHD relative to persons with lower levels after adjustments for established CVD risk factors, including lifestyle factors. This finding is of public health significance as IHD is one of the main causes of morbidity and mortality worldwide.4 If persons with high levels of health anxiety stay alert with the intention to better ‘control’ and ‘detect’ early signs of severe somatic diseases, it might contribute to unintentional harmful effects as the autonomous activation associated with anxiety in general likely is associated with increased risk of IHD. These findings illustrate the dilemma for clinicians between reassuring the patient that current physical symptoms of anxiety do not represent heart disease, contrasted against the emerging knowledge on how anxiety, over time, may be causally associated with increased risk of IHD.9 At best, this finding might encourage patients to seek treatment for health anxiety and to trust their heart.
Footnotes
Contributors: LIB, Faculty of Medicine and Dentistry, University of Bergen, Bergen, and Psychiatric Division, Haukeland University Hospital, Bergen, designed, analysed and interpreted the data, drafted the article, approved the final version, has agreed to be accountable for all aspects of the work and is the guarantor of the study. JCS, Norwegian Institute of Public Health, designed, analysed and interpreted the data, revised the manuscript for important intellectual content, approved the final version of the manuscript and has agreed to be accountable for all aspects of the work. GS, Faculty of Medicine and Dentistry, University of Bergen, Bergen, designed, analysed and interpreted the data, revised the manuscript for important intellectual content, approved the final version of the manuscript and has agreed to be accountable for all aspects of the work. JI, Faculty of Medicine and Dentistry, University of Bergen, Bergen, designed, analysed and interpreted the data, revised the manuscript for important intellectual content, approved the final version of the manuscript and has agreed to be accountable for all aspects of the work. IW, Dr Med. Faculty of Medicine and Dentistry, University of Bergen, Bergen and Haraldsplass Deaconal University Hospital, Bergen, designed the study, revised the manuscript for important intellectual content, approved the final version of the manuscript and has agreed to be accountable for all aspects of the work. SEV, Faculty of Medicine and Dentistry, University of Bergen, Bergen and Norwegian Institute of Public Health, designed, analysed and interpreted the data, revised the manuscript for important intellectual content, approved the final version of the manuscript and has agreed to be accountable for all aspects of the work. GST, Faculty of Medicine and Dentistry, University of Bergen, Bergen, designed, analysed and interpreted the data, revised the manuscript for important intellectual content, approved the final version of the manuscript and has agreed to be accountable for all aspects of the work. AKK, Faculty of Medicine and Dentistry, University of Bergen, Bergen and Norwegian Institute of Public Health, designed, analysed and interpreted the data, revised the manuscript for important intellectual content, approved the final version of the manuscript and has agreed to be accountable for all aspects of the work. All authors had full access to all of the data in the study (including statistical reports and tables) and take responsibility for the integrity of the data and the accuracy of the data analysis.
Funding: Contribution by each of the authors is considered part of their general work as researchers funded by their respective employers, and the study received no additional funding.
Competing interests: None declared.
Ethics approval: Regional Ethics Committee of Western Norway (ref 2013/1764) and the Norwegian Data Inspectorate.
Provenance and peer review: Not commissioned; externally peer reviewed.
Data sharing statement: The Norwegian Institute of Public Health owns the data used in the study. According to their legal department, the data cannot be deposited online as the study participants have not explicitly been informed about, nor approved data sharing when signing the informed consent when the study was undertaken in 1997–1999. Further, the ethical approval for the study obliges us, in general terms, to protect the privacy of the participants. Readers can apply for access and permission to analyse data from the Hordaland Health Study. Application form and general information can be found at http://husk-en.b.uib.no, and questions may be directed to project coordinator kari.juul@igs.uib.no
References
- 1.American Psychiatric Association. Diagnostic and statistical manual of mental disorders. 5th edn DSM-V, 2013. [Google Scholar]
- 2.Tyrer P, Eilenberg T, Fink P et al. Health anxiety: the silent, disabling epidemic. BMJ 2016;353:i2250 10.1136/bmj.i2250 [DOI] [PubMed] [Google Scholar]
- 3.Starcevic V. Hypochondriasis and health anxiety: conceptual challenges. Br J Psychiatry 2013;202:7–8. 10.1192/bjp.bp.112.115402 [DOI] [PubMed] [Google Scholar]
- 4. Institute for Health Metrics and Evaluation, University of Washington. The global burden of disease: Generating Evidence, Guiding Policy, Report, 2013. http://www.healthdata.org/sites/default/files/files/policy_report/2013/GBD_GeneratingEvidence/IHME_GBD_GeneratingEvidence_FullReport.pdf.
- 5.Noyes R Jr, Carney CP, Hillis SL et al. Prevalence and correlates of illness worry in the general population. Psychosomatics 2005;46:529–39. 10.1176/appi.psy.46.6.529 [DOI] [PubMed] [Google Scholar]
- 6.Forouzanfar MH, Alexander L, Anderson HR et al. , Global Burden of Disease Risk Factors Collaborators. Global, regional, and national comparative risk assessment of 79 behavioural, environmental and occupational, and metabolic risks or clusters of risks in 188 countries, 1990–2013: a systematic analysis for the Global Burden of Disease Study 2013. Lancet 2015;386:2287–323. 10.1016/S0140-6736(15)00128-2 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Janszky I, Ahnve S, Lundberg I et al. Early-onset depression, anxiety, and risk of subsequent coronary heart disease: 37-year follow-up of 49,321 young Swedish men. J Am Coll Cardiol 2010;56:31–7. 10.1016/j.jacc.2010.03.033 [DOI] [PubMed] [Google Scholar]
- 8.Roest AM, Martens EJ, de Jonge P et al. Anxiety and risk of incident coronary heart disease: a meta-analysis. J Am Coll Cardiol 2010;56:38–46. 10.1016/j.jacc.2010.03.034 [DOI] [PubMed] [Google Scholar]
- 9.Batelaan NM, Seldenrijk A, Bot M et al. Anxiety and new onset of cardiovascular disease: critical review and meta-analysis. Br J Psychiatry 2016;208:223–31. 10.1192/bjp.bp.114.156554 [DOI] [PubMed] [Google Scholar]
- 10. The Hordaland Health Study (HUSK). http://husk-en.b.uib.no/
- 11.Pilowsky I. Dimensions of hypochondriasis. Br J Psychiatry 1967;113:89–93. 10.1192/bjp.113.494.89 [DOI] [PubMed] [Google Scholar]
- 12.Hiller W, Rief W, Fichter MM. Dimensional and categorical approaches to hypochondriasis. Psychol Med 2002;32:707–18. 10.1017/S0033291702005524 [DOI] [PubMed] [Google Scholar]
- 13.Speckens AE, Spinhoven P, Sloekers PP et al. A validation study of the Whitely Index, the Illness Attitude Scales, and the Somatosensory Amplification Scale in general medical and general practice patients. J Psychosom Res 1996;40:95–104. 10.1016/0022-3999(95)00561-7 [DOI] [PubMed] [Google Scholar]
- 14.Sulo G, Vollset SE, Nygård O et al. Cardiovascular diseases and diabetes mellitus in Norway during 1994-2009: CVDNOR—a nationwide research project. Nor J Epidemiol 2013;23:101–7. [Google Scholar]
- 15. CVDNOR: Cardiovascular diseases in Norway. http://cvdnor.b.uib.no/
- 16. Igland J TG, Ebbing M, Nygård O, et al. The CVDNOR project: Cardiovascular Diseases in Norway 1994–2009. Description of data and data quality. Report, 2013. http://cvdnor.b.uib.no/files/2013/08/CVDNOR-Data-and-Quality-Report1.pdf.
- 17. The World Health Organisation. The ICD-10 classification of mental and behavioural disorders. 1992. http://www.who.int/classifications/icd/en/
- 18. The Framingham Heart Study, a project of the National Heart, Lung and Blood Institute and Boston University. Hard Coronary Heart Disease (10 year risk). https://www.framinghamheartstudy.org/risk-functions/coronary-heart-disease/hard-10-year-risk.php.
- 19.Veddegjaerde KE, Sivertsen B, Wilhelmsen I et al. Confirmatory factor analysis and item response theory analysis of the Whiteley Index. Results from a large population based study in Norway. The Hordaland Health Study (HUSK). J Psychosom Res 2014;77:213–18. 10.1016/j.jpsychores.2014.06.011 [DOI] [PubMed] [Google Scholar]
- 20.Desquilbet L, Mariotti F. Dose–response analyses using restricted cubic spline functions in public health research. Stat Med 2010;29:1037–57. 10.1002/sim.3841 [DOI] [PubMed] [Google Scholar]
- 21.Sunderland M, Newby JM, Andrews G. Health anxiety in Australia: prevalence, comorbidity, disability and service use. Br J Psychiatry 2013;202:56–61. 10.1192/bjp.bp.111.103960 [DOI] [PubMed] [Google Scholar]
- 22.Bjelland I, Dahl AA, Haug TT et al. The validity of the Hospital Anxiety and Depression Scale. An updated literature review. J Psychosom Res 2002;52:69–77. 10.1016/S0022-3999(01)00296-3 [DOI] [PubMed] [Google Scholar]
- 23.Gustad LT, Laugsand LE, Janszky I et al. Symptoms of anxiety and depression and risk of acute myocardial infarction: the HUNT 2 study. Eur Heart J 2014;35:1394–403. 10.1093/eurheartj/eht387 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Paterniti S, Zureik M, Ducimetière P et al. Sustained anxiety and 4-year progression of carotid atherosclerosis. Arterioscler Thromb Vasc Biol 2001;21:136–41. 10.1161/01.ATV.21.1.136 [DOI] [PubMed] [Google Scholar]
- 25.Chalmers JA, Quintana DS, Abbott MJ et al. Anxiety disorders are associated with reduced heart rate variability: a meta-analysis. Front Psychiatry 2014;5:80 10.3389/fpsyt.2014.00080 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Sulo G, Igland J, Nygard O et al. Favourable trends in incidence of AMI in Norway during 2001–2009 do not include younger adults: a CVDNOR project. Eur J Prevent Cardiol 2014;21:1358–64. 10.1177/2047487313495993 [DOI] [PubMed] [Google Scholar]
- 27.Knudsen AK, Hotopf M, Skogen JC et al. The health status of nonparticipants in a population-based health study: the Hordaland Health Study. Am J Epidemiol 2010;172:1306–14. 10.1093/aje/kwq257 [DOI] [PubMed] [Google Scholar]