Abstract
Introduction
Degenerative lumbar spinal stenosis (DLSS) is a major public health problem and the primary reason why older adults seek lumbar spine surgery. Acupuncture may be effective for DLSS, but the evidence supporting this possibility is still limited.
Methods and analysis
A total of 80 participants with DLSS will be randomly allocated to either an acupuncture group or a sham acupuncture (SA) group at a ratio of 1:1. 24 treatments will be provided over 8 weeks. The primary outcome is the score change of the Modified Roland-Morris Disability Questionnaire (RMDQ) responses from baseline to week 8. The secondary outcomes include the assessment of lower back pain and leg pain using the Numeric Rating Scale (NRS), the change in the number of steps per month, and the assessment of the specific quality of life using the Swiss Spinal Stenosis Questionnaire (SSSQ). We will follow-up with the participants until week 32. All of the participants who received allocation will be included in the statistical analysis.
Ethics/dissemination
This protocol has been approved by the Research Ethical Committee of Guang'anmen Hospital (Permission number: 2015EC114) and Fengtai Hospital of Integrated Traditional and Western Medicine (Permission number: 16KE0409). The full data set will be made available when this trial is completed and published. Applications for the release of data should be made to ZL (principal investigator).
Trial registration number
Keywords: Lumbar spinal stenosis, acupuncture, efficacy, randomized controlled trial
Strengths and limitations of this study.
This is a placebo-controlled trial using non-penetrating needles, which might provide a valid blinding effect to participants and minimise the placebo effect.
A 24-week follow-up can assess whether a sustained effect of acupuncture for degenerative lumbar spinal stenosis can persist for a long period.
As acupuncture is a manipulated intervention, it is difficult to blind the acupuncturists to the treatment modalities.
Background
Lumbar spinal stenosis (LSS) is one of the major causes of pain and numbness in the back and legs, with degenerative lumbar spinal stenosis (DLSS) as the most common type.1 2 DLSS is commonly characterised by diminished available space for the neural and vascular elements in the lumbar spinal canal secondary to degenerative changes. These changes lead to a variable clinical syndrome such as intermittent claudication and back, gluteal and lower extremity pain and fatigue all of which are accompanied by limited daily function and impaired quality of life.3–5 According to the Framingham study, the prevalence of relative (≤12 mm) and absolute (≤10 mm) LSS in a random community population 60–69 years of age was 47.2% and 19.4%, respectively.6 In general, ageing results in spine degeneration after the age of 65, and DLSS is the main reason that people over the age of 65 years seek lumbar spine surgery.5 7
According to the recommendations of the North American Spine Society (NASS), treatment options include surgical therapy, epidural steroid injections and physical therapy.8 Randomised trials indicate that for patients severely affected by spinal stenosis, surgery offers greater efficacy than non-surgical treatments.9 10 However, the complications and costs of surgery should also be considered, especially for older patients.11 In addition, Kovacs et al12 found that after 10 years of follow-up, patient satisfaction between the surgical and non-surgical groups were similar, suggesting that the outlook for a study examining conservative therapies is promising. Some experts assert that it is necessary to undergo systematic conservative therapy before resorting to surgical repair. Furthermore, the ineffectiveness of conservative treatment is one of the indications for surgery.13–15 Although epidural steroid injections can relieve pain in the back and legs, this treatment often fails to improve pain in the lower extremity and claudication.16 17 For acupuncture, there has been insufficient evidence to either recommend or criticise its use. In 2013, Kim et al18 conducted a systematic review and meta-analysis which found that acupuncture either with electrical stimulation or in combination with other related techniques might be beneficial compared with acupuncture therapy alone. However, the evidence was poor and limited by trials rated as having a high risk of bias and substantial clinical heterogeneity. Thus, their conclusion could not prove the efficacy of acupuncture for DLSS. One of our previous cohort studies signified that acupuncture might relieve the symptoms of DLSS.19 In addition, an unpublished pilot study conducted last year included 12 participants also indicated that compared with sham acupuncture (SA), acupuncture can alleviate the pain symptoms as measured by Modified Roland-Morris Disability Questionnaire (RMDQ) and Numeric Rating Scale (NRS) after 8 weeks of treatment. However, owing to the insufficient sample size and lack of a long-term follow-up period, more substantial clinical trials are still needed to support the evidence that acupuncture may be an optional treatment for DLSS in the future.
Methods
Objective
To assess the efficacy and safety of acupuncture on relieving the symptoms of DLSS and improving the quality of life of patients with DLSS.
Hypotheses
Compared with SA, acupuncture will significantly relieve the symptoms of DLSS after an 8-week treatment measured by valid instruments.
Acupuncture will have a sustained effect for DLSS after 8 weeks of treatment.
Study design
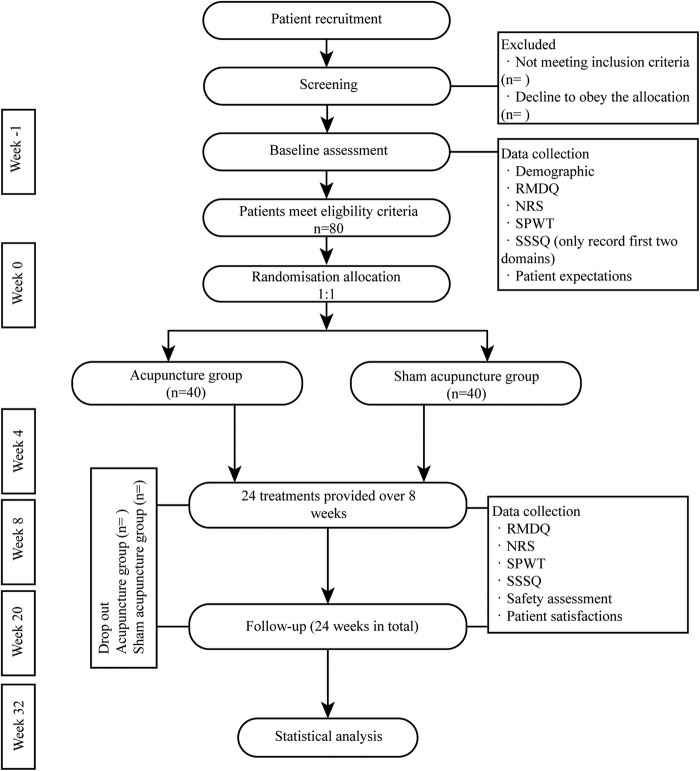
This is a randomised, placebo-controlled, observer-blinded and patient-blinded multicentre superiority trial with two parallel groups using a 1:1 allocation ratio. The protocol had been developed following the Standard Protocol Items: Recommendations for Interventional Trials (SPIRIT) and STandards for Reporting Interventions in Clinical Trials of Acupuncture (STRICTA) guidelines.20 21 A diagram of the trial design is shown in figure 1.
Figure 1.
Diagram of trial design. NRS, Number Rating Scale; RMDQ, Modified Roland-Morris Disability Questionnaire; SPWT, self-paced walking test; SSSQ, Swiss Spinal Stenosis Questionnaire.
Participants and recruitment
In total, 80 participants will be recruited through public posters and from the Guang'anmen Hospital and Fengtai Hospital of Integrated Traditional and Western Medicine website. The clinicians will be responsible for enrolling participants who are willing to undergo acupuncture treatment for DLSS. The assistant researchers will assess and record the participants' baseline status. After the written informed consent has been obtained, eligible participants will be randomly allocated according to a group number generated by a third party.
Randomisation and allocation concealment
The Institute of Clinical Pharmacology affiliated with Guang'anmen Hospital will be responsible for randomly grouping participants and is involved in neither the treatment nor data collection for this study. Using a block size of 4 in a scheduled computer-generated randomisation programme, the final group assignments will be sealed in opaque envelopes. To ensure the proper management of the randomisation procedure, the sequence numbers will be printed on the outside of the opaque envelope, and the group assignment will be sealed inside. All envelopes will be numbered sequentially. The envelopes will be delivered according to the patients' sequence numbers, and the acupuncturist will be informed of the random numbers and group assignments by either telephone or email.
Blinding
Owing to the characteristics of acupuncture, none of the acupuncturists involved in this trial can be blinded to the assignments. However, the participants will be blinded as they do not know their assignments, and the SA used in this trial can guarantee a good blinding effect as the location of the selected acupoints are in the blind spots of participants. The assessors and statisticians for the data collection and analysis will be blinded to the assignments. In addition, participants will be asked to answer the following question during week 8 to test the blinding effect: ‘Do you think you have received real acupuncture treatment?’ The participants can choose ‘yes’ or ‘no’ as an answer. We will analyse the percentage of participants who answered ‘yes’ in both groups after the final treatment. If the results show no significant difference in the response to this question between the two groups, they could suggest that the blinding effect is sufficient.
Participants
Inclusion criteria
Participants who meet the requirements for a diagnosis of DLSS as defined by the NASS8 as well as all of the following conditions will be considered for enrolment.
Using the NRS questionnaire to report buttock/leg pain>low back pain>4 points.
A Roland-Morris score of at least 7.
Mild, moderate or severe lumbar central canal spinal stenosis identified by MRI or CT scan. Central stenosis will be classified mainly based on the mid-sagittal diameter measured in millimetres at the narrowest intervertebral level. The classifications are mild (more than 13 mm), moderate (11–13 mm) and severe (<11 mm).22
Age 50–80 years.
Signed consent and willingness to participate in the trial.
Exclusion criteria
Congenital stenosis of the vertebral canal, serious indications of DLSS (eg, segmental muscular atrophy, bowel and bladder disturbances), lumbar tuberculosis, lumbar vertebral tumours or vertebral body compression fracture.
Spinal instability requiring surgery.
Severe vascular, pulmonary or coronary artery disease that limits ambulation, including recent myocardial infarction.
Participants who are cognitively impaired such that they are unable to give informed consent or provide accurate data.
Clinical comorbidities that could interfere with the collection of data concerning pain and function.
Acupuncture treatments within the past 30 days.
Administration of medications for pain control (eg, non-steroidal anti-inflammatory drugs or herbal anti-inflammatory agents) during the week prior to collecting the baseline.
Intervention
Intervention group
Acupuncturists who have completed 5 years of undergraduate study and have 2 years of clinical experience will administer the acupuncture or SA. The intervention protocol and acupoints selection were based on the expert's experience and previous clinical research.19 The acupoints of Shenshu (BL23), Dachangshu (BL25), Weizhong (BL40), Chengshan (BL57) and Taixi (KI3) will be used (table 1). All acupoints will be localised according to the WHO Standard Acupuncture Locations.23 During the treatment, participants will lie in the prone position, and the acupuncturists will use 75% alcohol pads to sterilise the skin around the acupuncture points. Subsequently, sterile disposable steel needles (Huatuo, Suzhou, China; 0.3 mm×40 mm/0.3 mm×75 mm) will be inserted into the selected acupuncture points, which are covered with adhesive pads. For the bilateral BL25, the needle will be inserted vertically at ∼40–70 mm to induce a sensation of soreness (de qi). For the other four acupoints (BL23, BL40, BL57 and KI3), the needles will be inserted to a depth of 10–15 mm, gently rotated three times and lifted to achieve de qi. There will be 24 treatment sessions, with 1 session scheduled three times a week. Patients will undergo a 30 min treatment per session.
Table 1.
Summary of the acupoints' location
| Acupoints | Location |
|---|---|
| Shenshu (BL23) | In the lumbar region, at the same level as the inferior border of the spinous process of the second lumbar vertebra, 1.5 Bone-cun lateral to the posterior median line |
| Dachangshu (BL25) | In the lumbar region, at the same level as the inferior border of the spinous process of the fourth lumbar vertebra, 1.5 Bone-cun lateral to the posterior median line |
| Weizhong (BL40) | On the posterior aspect of the knee, at the midpoint of the popliteal crease |
| Chengshan (BL57) | On the posterior aspect of the leg, at the connecting point of the calcaneal tendon with the two muscle bellies of the gastrocnemius muscle |
| Taixi (KI3) | On the posteromedial aspect of the ankle, in the depression between the prominence of the medal malleolus and the calcaneal tendon |
Control group
The acupuncturists will use blunt tip needles that cannot penetrate the skin or stimulate deep tissues. Thrusting and twisting motions will be used by acupuncturists to simulate the treatment and aid in blinding the patients. The sham needle used in this trial had a blunt tip similar to the Streitberger needle,24 which has been proven as a useful placebo control.25 Each placebo needle consists of four parts: the needle handle, needle body, blunt tip and adhesive pad (an illustration of the placebo needle used in this trial is shown as figure 2). The chosen acupoints, treatment duration and frequency of sessions for participants in the SA group will be the same as in the acupuncture group.
Figure 2.
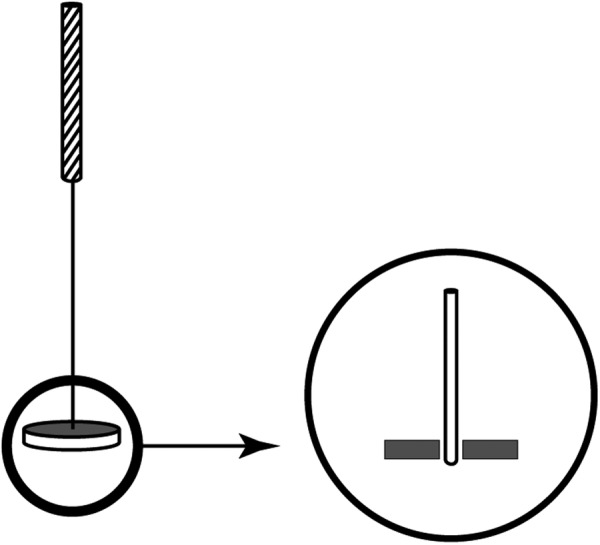
Illustration of sham acupuncture.
Outcome
Primary outcome
The primary outcome measure is the score change in the Modified Roland-Morris Disability Questionnaire (with scores ranging from 0 to 24 and higher scores suggesting greater impairment) compared with baseline at week 8.
The RMDQ is a reliable and valid back pain-specific functional status questionnaire. Disability is measured respective to physical function activities and activities of daily living, including eating and sleeping. The RMDQ contains 24 questions, and after each question, the phrase ‘caused by low back pain’ appears. In this study, we will modify the above phrase to ‘caused by buttock and leg pain’ after each question, which will be more suitable for participants who have sciatica.26 To measure the symptoms of the participants with DLSS after 8 weeks of treatment, participants will be asked to complete the Chinese version of the RMDQ.
Secondary outcomes
The score change in the RMDQ compared with baseline at weeks 4, 20 and 32.
The score change in the pain rating of low back, and buttock and leg using the Number Rating Scale (NRS, with scores ranging from 0 to 10 and higher scores indicating greater pain) compared with baseline at weeks 4, 8, 20 and 32. The pain symptoms will be graded using the 11-grade NRS by the patients themselves.27 28 We will offer two scales for the participants each week, including one for measuring buttock and leg pain and another for measuring low back pain. Participants should answer with the average score of period since the most recent follow-up. Assessments will be made at baseline, from 1 to 8 weeks, and at 20 and 32 weeks after the first treatment.
The score change in the self-paced walking test (SPWT) compared with baseline at weeks 4, 8, 20 and 32. The walking function of participants with claudication will be evaluated using the SPWT, which was invented by Bassey et al29 and was initially used to evaluate cardiovascular disease. Tomkins et al30 adapted the SPWT to assess the walking function of patients with LSS. In this trial, participants will be required to walk at their customary speed (between 8:30 and 9:30 after breakfast on the weekends), and they will stop when the symptoms of DLSS appear; the number of steps will be recorded by pedometer.
The score change in the Swiss Spinal Stenosis Questionnaire (SSSQ) will be compared with baseline at weeks 4, 8, 20 and 32. The symptoms and functions will be evaluated using the SSSQ, which consists of three domains: symptom severity (eg, overall pain, pain frequency, numbness, feebleness; with scores ranging from 1 to 5 and higher scores indicating worse symptoms), physical function (walking, activity; with scores ranging from 1 to 4 and higher scores indicating worse function) and satisfaction with the degree of treatment efficacy (with scores ranging from 1 to 4 and higher scores indicating less satisfaction). This assessment will be completed at baseline and at 4, 8, 20 and 32 weeks after the first treatment.31–33
Patient expectations of the effectiveness of acupuncture will be recorded at baseline. The expectations regarding whether acupuncture might help alleviate DLSS will be assessed at baseline. This scale includes four brief questions to investigate whether patients are confident that the acupuncture treatment will help alleviate their DLSS and whether the degree of expectation can affect the primary outcome: ‘Do you think acupuncture can work?’, ‘Do you think acupuncture can help your DLSS?’, ‘Which intervention do you prefer?’ and ‘Did you receive your preferred intervention?’.
Table 2 presents the data collection times.
Table 2.
Time of data collection
| Treatment phase (weeks) |
Follow-up phase (weeks) |
||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|
| Measures | Baseline | w 1 | w 2 | w 3 | w 4 | w 5 | w 6 | w 7 | w 8 | w 20 | w 32 |
| RMDQ | × | × | × | × | × | ||||||
| NRS | × | × | × | × | × | × | × | × | × | × | × |
| SPWT | × | × | × | × | × | ||||||
| SSSQ | × | × | × | × | × | ||||||
| Patient expectations | × | ||||||||||
NRS, Number Rating Scale; RMDQ, Modified Roland-Morris Disability Questionnaire; SPWT, self-paced walking test; SSSQ, Swiss Spinal Stenosis Questionnaire; w, week.
Safety assessment
For safety assessment, acupuncture-related adverse events such as severe sharp pain (visual analogue scale ≥7), haematomas or bleeding around the side of needle, nausea or fainting during treatment, and other discomfort after acupuncture will be assessed throughout the study in both groups. In addition, adverse events unrelated to acupuncture such as the common cold, cough, diarrhoea, constipation and headache will also be recorded by the observers.
Data management and monitoring
All investigators who have completed good clinical practice training will independently collect the data and assess the effects of the treatments. A remote data capture system will be used to store data on a password-protected computer that will store recorded data in a secure environment. In principle, clinical information will not be released without the permission of the principal investigator (ZL), with the exception of an emergency or as necessary for monitoring and auditing by the data monitoring committee. All paper and electronic versions of the case report form will be preserved in the secure research archives at Guang'anmen Hospital for 10 years and will only be viewed by the research team. In addition, an independent data monitoring committee has been established to review the results of any adverse events to decide whether the trial should continue. The committee comprises an orthopaedist, a medical statistician and an epidemiologist.
Rescue medication
In general, ingestion of painkillers is forbidden during the trial because they may potentially effect the accuracy of the data. However, if participants declare that the pain is unbearable during the study period, celecoxib capsules will be administered (J20030098 Pfizer Pharmaceuticals LLC; 1.2 g/box) to alleviate pain (200 mg by mouth once daily for 3 days). Any medicine administered should be carefully recorded in the case report form in addition to any other concomitant medications.
Statistical methods
Sample size
The sample size calculation is based on the superiority two-sided test with the null hypothesis that the difference between the groups with regard to the score change in the RMDQ from baseline to week 8 is not more than 2.25 points. The primary outcome is the score change in the RMDQ from baseline to week 8. According to the report of Patrick et al,26 the minimal clinically important difference (MCID) of the RMDQ is 2–3 points; therefore, we choose 2.25 points as a conservative estimate of the MCID for the RMDQ score. Based on our previous pilot study and assumptions, the mean reduction of RMDQ score in the acupuncture and SA groups was 4.7 and 2.4, with an SD of 3.8 points in both groups. The sample size was calculated using WinPepi software V.11.6.34 We estimated α=0.05 and β=0.2, allowing for 15% attrition. Finally, we plan to recruit 80 participants, 40 in each group, which can provide 80% power to detect an intergroup difference of more than 2.25 points in the RMDQ.
Statistical analysis
Data from the trial will be entered into SPSS software V.21.0 (IBM SPSS Statistics, IBM Corp, Somers, New York, USA), and data analysis will be based on the intention-to-treat analysis data set, which includes all participants who were assigned to a group. The main objective of this trial is to assess the score change in the RMDQ between the groups from baseline to week 8. We will use the independent sample t-test for the analysis, and if the distribution is abnormal, non-parametric Wilcoxon statistics will be used to test the null hypothesis. For the secondary outcome data provided by scales or questionnaires such as the NRS, SPWT and SSSQ, an independent sample t-test will be used for comparison between the independent samples, and non-parametric tests may also be used in case of abnormal distribution. Linear regression will be used to explore the relationship between the expectations and primary outcomes as well as to examine whether the patients' expectations can affect their treatment. For any random data missing, a multiple imputation will be used; however, we will endeavour to ensure that all data points analysed are actual collected data. A χ2 test will be used to assess the satisfaction (assessed by third domain of SSSQ) and safety of the treatments.
Research ethics
This trial is in accordance with the Declaration of Helsinki35 and has been approved by the Research Ethical Committee of Guang'anmen Hospital affiliated with the China Academy of Chinese Medicine Science (Permission number: 2015EC114) and Fengtai Hospital of Integrated Traditional and Western Medicine (Permission number: 16KE0409). All participants will be required to provide written informed consent prior to enrolment in the trial.
Discussion
To date, in the majority of randomised controlled trials that have compared basic acupuncture to other types of acupuncture for treating DLSS, it is difficult to assess the efficacy of acupuncture.18 In this trial, we designed an SA group as a controlled comparison group to identify the efficacy of real acupuncture. In acupuncture research, the use of an SA control is helpful for determining the efficacy of acupuncture for treating a disorder. However, owing to the characteristics of acupuncture, it is hard to use a placebo needle on patients. Based on a randomised controlled cross-over trial, the SA that will be implemented in this study will serve as a valid control25 because it can produce a good blinding effect to patients from two groups. This might balance the placebo effect between the two groups and reveal the efficacy of acupuncture for DLSS.
Additionally, we selected RMDQ as the primary outcome in combination with MCID to calculate the sample size for this trial, which will improve the analysis in reaching a final conclusion. RMDQ is one of the most commonly used instruments for lower back pain.36 Owing to its simple and readily understood questions, the RMDQ assessment is easy to complete. Other widely used scales and questionnaires such as the NRS, SPWT and SSSQ will also play auxiliary roles in evaluating the results regarding whether acupuncture can ameliorate the symptoms and improve the quality of life for patients with DLSS.
Finally, we established a 24-week follow-up (weeks 9–32) to observe the sustained effects of acupuncture on DLSS after the end of the treatment sessions. There are still limitations that should be noted. As acupuncture is a manipulated intervention, blinding for acupuncturists is hard to implement. However, the outcome evaluators in this trial will be blinded to assignment to decrease the potential bias. Additionally, because the pilot study that was used to estimate the sample size of this trial was small, there might be an overestimation of the acupuncture effect. At the end of this trial, we hope that the results will provide more reliable evidence and clarify the value of acupuncture as a treatment for patients with DLSS.
Acknowledgments
The authors would like to express their sincere thanks to Professor Lawrence Mbuagbaw (Department of Clinical Epidemiology and Biostatistics, McMaster University) for his help in improving the methodological quality of this manuscript. The authors would also like to take this opportunity to show their sincere gratitude to Mr Brendan Melchiorri (Department of Advanced International Studies, Johns Hopkins University), for his advice and improvements to this manuscript.
Footnotes
Contributors: ZL is the principal investigator of this trial. ZL, ZQ and YD contributed to the development of the research question and trial design. ZQ and JW contributed to the drafting of the manuscript, and ZL edited the final manuscript. JZ, XL and LY are responsible for the recruitment and treatment of patients. All authors read and approved the final manuscript.
Competing interests: None declared.
Patient consent: Obtained.
Ethics approval: Research Ethical Committee of Guang'anmen Hospital affiliated with the China Academy of Chinese Medicine Science.
Provenance and peer review: Not commissioned; externally peer reviewed.
Data sharing statement: The full data set will be made available when this trial is completed and published. Application for the data to be released should be made in contact to ZL (principle investigator).
References
- 1.Berman BM, Langevin HM, Witt CM et al. Acupuncture for chronic low back pain. N Engl J Med 2010;363:454–61. 10.1056/NEJMct0806114 [DOI] [PubMed] [Google Scholar]
- 2.Atlas SJ, Delitto A. Spinal stenosis: surgical versus nonsurgical treatment. Clin Orthop Relat Res 2006;443:198–207. 10.1097/01.blo.0000198722.70138.96 [DOI] [PubMed] [Google Scholar]
- 3.Genevay S, Atlas SJ. Lumbar spinal stenosis. Best Pract Res Clin Rheumatol 2010;24:253–65. 10.1016/j.berh.2009.11.001 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Siebert E, Pruss H, Klingebiel R et al. Lumbar spinal stenosis: syndrome, diagnostics and treatment. Nat Rev Neurol 2009;5:392–403. 10.1038/nrneurol.2009.90 [DOI] [PubMed] [Google Scholar]
- 5.Deyo RA, Ciol MA, Cherkin DC et al. Lumber spinal fusion: a cohort study of complications, reoperations, and resource use in the Medicare population. Spine 1993;18:1463–70. 10.1097/00007632-199318110-00010 [DOI] [PubMed] [Google Scholar]
- 6.Kalichman L, Cole R, Kim DH et al. Spinal stenosis prevalence and association with symptoms: the Framingham Study. Spine J 2009;9:545–50. 10.1016/j.spinee.2009.03.005 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Deyo RA, Gray DT, Kreuter W et al. United States trends in lumbar fusion surgery for degenerative conditions. Spine 2005;30:1441–5. 10.1097/01.brs.0000166503.37969.8a [DOI] [PubMed] [Google Scholar]
- 8.Kreiner DS, Shaffer WO, Baisden JL et al. An evidence-based clinical guideline for the diagnosis and treatment of degenerative lumbar spinal stenosis (update). Spine J 2013;13:734–43. 10.1016/j.spinee.2012.11.059 [DOI] [PubMed] [Google Scholar]
- 9.Malmivaara A, Slatis P, Heliovaara M et al. Surgical or nonoperative treatment for lumbar spinal stenosis? A randomized controlled trial. Spine 2007;32:1–8. 10.1097/01.brs.0000251014.81875.6d [DOI] [PubMed] [Google Scholar]
- 10.Weinstein JN, Tosteson TD, Lurie JD et al. Surgical versus nonsurgical therapy for lumbar spinal stenosis. N Engl J Med 2008;358:794–810. 10.1056/NEJMoa0707136 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Deyo RA, Mirza SK, Martin BI et al. Trends, major medical complications, and charges associated with surgery for lumbar spinal stenosis in older adults. JAMA 2010;303:1259–65. 10.1001/jama.2010.338 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Kovacs FM, Urrutia G, Alarcon JD. Surgery versus conservative treatment for symptomatic lumbar spinal stenosis: a systematic review of randomized controlled trials. Spina 2011;36:e1335–51. 10.1097/BRS.0b013e31820c97b1 [DOI] [PubMed] [Google Scholar]
- 13.Slätis P, Malmivaara A, Heliövaara M et al. Long-term results of surgery for lumbar spinal stenosis: a randomized controlled trail. Eur Spine J 2011;20:1174–81. 10.1007/s00586-010-1652-y [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Sengapta DK, Herkowitz HN. Lumbar spinal stenosis. Treatment strategies and indications for surgery. Orthop Clin North Am 2003;34:281–95. 10.1016/S0030-5898(02)00069-X [DOI] [PubMed] [Google Scholar]
- 15.Gelalis ID, Amaoutoqlou C, Christoforou G et al. prospective analysis of surgical outcomes in patients undergoing decompressive laminectomy and posterior instrumentation for degenerative lumbar spinal stenosis. Acta Orthop Traumatol Turc 2010;44:235–40. 10.3944/AOTT.2010.2278 [DOI] [PubMed] [Google Scholar]
- 16.Manchikanti L, Cash KA, McManus CD et al. Preliminary results of a randomized, equivalence trial of fluoroscopic caudal epidural injections in managing chronic low back pain: part 4-spinal stenosis. Pain Physician 2008;11:833–48. [PubMed] [Google Scholar]
- 17.Armon C, Argoff CE, Samuels J et al. Assessment: use of epidural steroid injections to treat radicular lumbosacral pain: report of the therapeutics and technology assessment subcommittee of the American academy of neurology. Neurology 2007;68:723–9. 10.1212/01.wnl.0000256734.34238.e7 [DOI] [PubMed] [Google Scholar]
- 18.Kim KH, Kim TH, Lee BR et al. Acupuncture for lumbar spinal stenosis: a systematic review and meta-analysis. Complement Ther Med 2013;21:535–56. 10.1016/j.ctim.2013.08.007 [DOI] [PubMed] [Google Scholar]
- 19.Liu ZS, Zhao H, Xie LM et al. Therapeutic effect of acupuncture on intermittent claudication of second retrograde lumbar spinal stenosis. Chinese Acupunct Moxibust 2004;24: 461–4. [Google Scholar]
- 20.Chan AW, Tetzlaff JM, Gøtzsche PC et al. SPIRIT 2013 explanation and elaboration: guidance for protocols of clinical trials. BMJ 2013;346:e7586 10.1136/bmj.e7586 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.MacPherson H, Altman DG, Hammerschlag R et al. Revised STandards for Reporting Interventions in Clinical Trials of Acupuncture (STRICTA): extending the CONSORT statement. J Evid Based Med 2010;3:140–55. 10.1111/j.1756-5391.2010.01086.x [DOI] [PubMed] [Google Scholar]
- 22.Botwin K, Brown LA, Fishman M et al. Fluoroscopically guided caudal epidural steroid injections in degenerative lumber spinal stenosis. Pain Physician 2007;10:547–58. [PubMed] [Google Scholar]
- 23.WHO Regional Office for the Western Pacific. WHO standard acupuncture point locations in the Western Pacific Region. Manila, Philippines, 2008. [Google Scholar]
- 24.Streitberger K, Kleinhenz J. Introducing a placebo needle into acupuncture research. Lancet 1998;352:364–5. 10.1016/S0140-6736(97)10471-8 [DOI] [PubMed] [Google Scholar]
- 25.Liu BY, Xu HF, Ma R et al. Effect of blinding with a new pragmatic placebo needle: a randomized controlled crossover study. Medicine 2014;93:e200 10.1097/MD.0000000000000200 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Patrick DL, Deyo RA, Atlas SJ et al. Assessing health-related quality of life in patients with sciatica. Spine 1995;20:1899–908. 10.1097/00007632-199509000-00011 [DOI] [PubMed] [Google Scholar]
- 27.Dworkin RH, Turk DC, Farrar JT et al. Core outcome measures for chronic pain clinical trials: IMMPACT recommendations. Pain 2005;113:9–19. 10.1016/j.pain.2004.09.012 [DOI] [PubMed] [Google Scholar]
- 28.Jensen MP, Karoly P. Self-report scales and procedures for assessing pain in adults. Handbook of Pain Assessment, second edition. New York: The Guilford Press, 2001:15–34. [Google Scholar]
- 29.Bassey EJ, Fentem PH, MacDonald IC et al. Self-paced walking as a method for exercise testing in elderly and young men. Clin Sci Mol Med 1976;51:609–12. [DOI] [PubMed] [Google Scholar]
- 30.Tomkins CC, Battie MC, Rogers T et al. A criterion measure of walking capacity in lumbar spinal stenosis and its comparison with a treadmill protocol. Spine 2009;34:2444–9. 10.1097/BRS.0b013e3181b03fc8 [DOI] [PubMed] [Google Scholar]
- 31.Iversen MD, Katz JN. Examination findings and self-reported walking capacity in patients with lumbar spinal stenosis. Phys Ther 2001;81:1296–306. [PubMed] [Google Scholar]
- 32.Stucki G, Daltroy L, Liang MH et al. Measurement properties of a self-administered outcome measure in lumbar spinal stenosis. Spine 1996;21:796–803. 10.1097/00007632-199604010-00004 [DOI] [PubMed] [Google Scholar]
- 33.Tuli SK, Yerby SA, Katz JN. Methodological approaches to developing criteria for improvement in lumbar spinal stenosis surgery. Spine 2006;31:1276–80. 10.1097/01.brs.0000217615.20018.6c [DOI] [PubMed] [Google Scholar]
- 34.Abramson JH. WINPEPI (PEPI-for-Windows): computer programs for epidemiologists. Epidemiol Perspect Innov 2004;1:6 10.1186/1742-5573-1-6 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.World Medical Organization. Declaration of Helsinki. BMJ 1996;313:1448–9. [Google Scholar]
- 36.Chapman JR, Norvell DC, Hermsmeyer JT et al. Evaluating common outcomes for measuring treatment success for chronic low back pain. Spine 2011;36(21 Suppl):S54–68. 10.1097/BRS.0b013e31822ef74d [DOI] [PubMed] [Google Scholar]