Abstract
We describe the case of a man aged 43 years who presented with a 2-week history of a palpable lump in the right proximal penile shaft. This was preceded by a 6-month history of perineal pain, accompanied by erectile dysfunction. An urgent MRI scan of his penis identified a thrombus within the right crus and corpus of the penis. His thrombophilia screen was normal. The patient was started on oral anticoagulation and a phosphodiesterase inhibitor (PDE-5i) to prevent thrombus progression and maintain erectile function. At 5 months, the patients' symptoms had resolved and an MRI showed a reduction in the thrombus size. MRI is a useful imaging modality to diagnose a thrombus within the corpus cavernosum in patients presenting with a history of penile and perineal pain together with a palpable lump. The non-enhancement of the lesion helps to differentiate this from alternative rare lesions within the penis and perineum.
Background
Partial segmental thrombosis of the corpus cavernosum (PSTCC) is a rare condition and ∼58 cases have been reported in 35 publications since 1976 when the first 2 cases were described.1–35 Physicians should be aware of this rare condition in a patient presenting with penile or perineal pain associated with a palpable lump. Such cases should initially be investigated using pelvis and penile MRI imaging, started on anticoagulant treatment and referred to a specialist centre for ongoing management.
Case presentation
A man aged 43 years presented with a 2-week history of a palpable lump in the proximal right side of the penile shaft following a 6-month history of perineal pain. There was no preceding history of penile or perineal trauma and the lump was present with a flaccid penis. He also described a new onset of erectile dysfunction manifesting as partial tumescence since the onset of pain 6 months earlier and difficulty engaging in penetrative sexual intercourse. From his medical history, he had well-controlled hypertension and was a keen cyclist.
On examination, the lump in the right penile shaft extended into the right crus. The distal penile shaft was normal and the remainder of the clinical examination was unremarkable.
Differential diagnosis
The differential diagnosis was a PSTCC or an underlying neoplastic lesion within the corpus such as a sarcoma.
Investigations
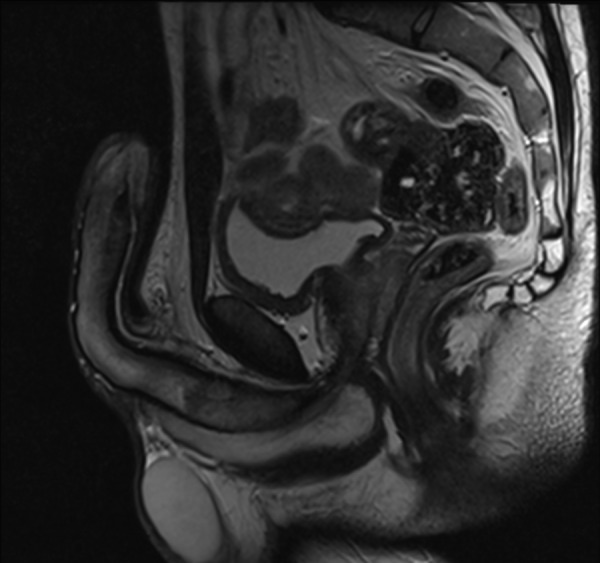
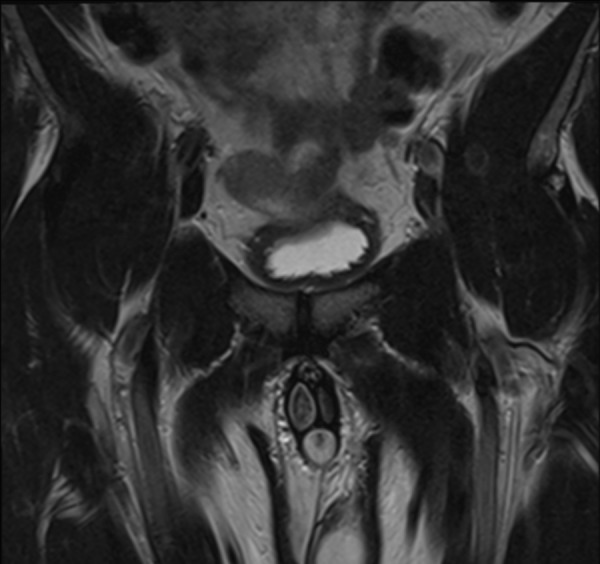
An urgent MRI of the pelvis and penis was performed. This revealed a 10 cm thrombus in the right corpus cavernosum which appeared expanded and with heterogenous low T2 signal (figures 1 and 2). T1-weighted MRI showed high T1 signal within the lesion, in keeping with relatively acute thrombus and no enhancement following contrast (figures 3 and 4). No pelvic organ abnormality was detected.
Figure 1.
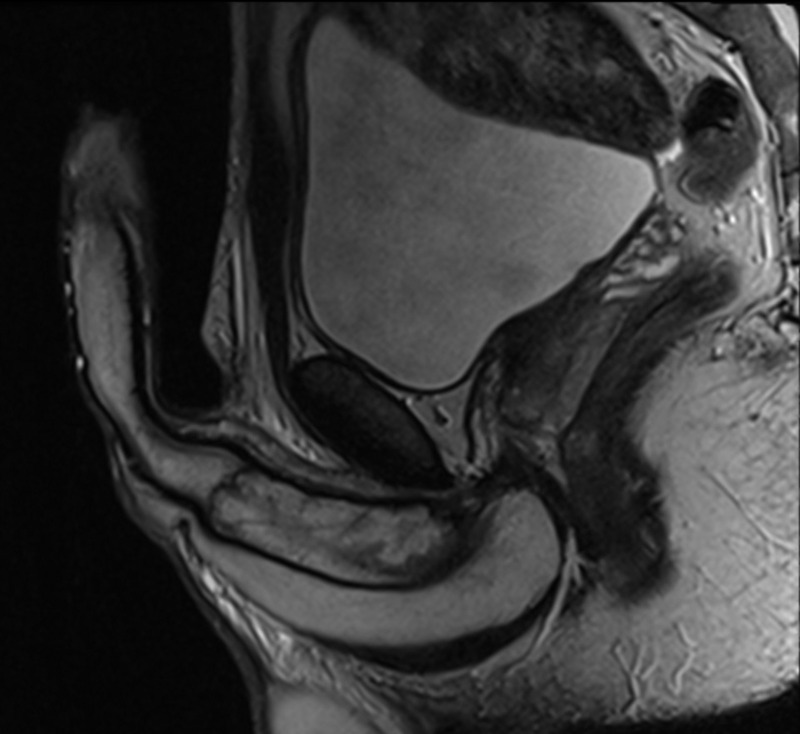
Proximal partial segmental thrombosis of the corpus cavernosum with a potential fibrous septum (T2-weighted sagittal MRI).
Figure 2.
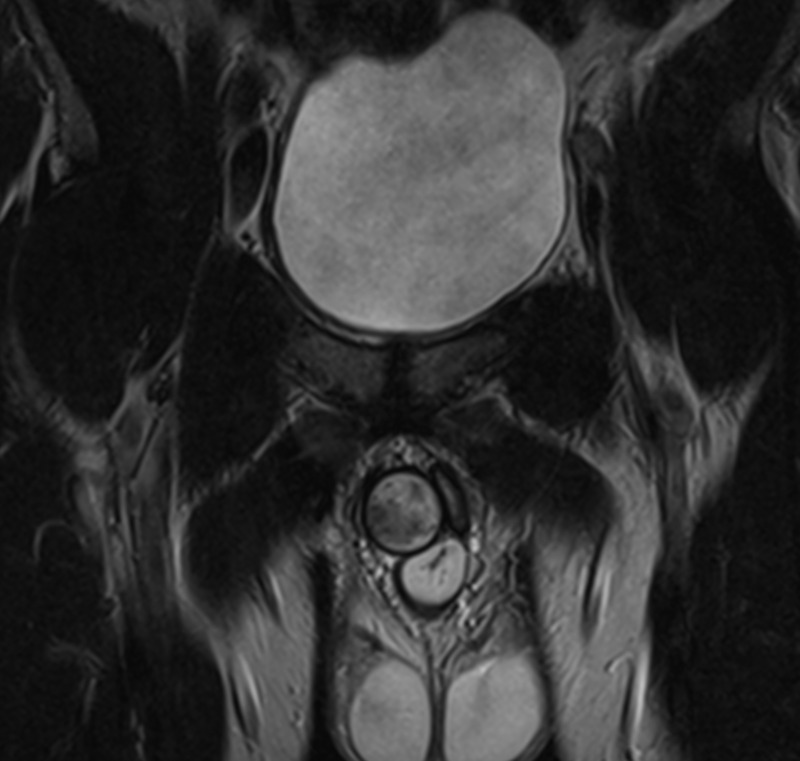
Distended right corpus cavernosum with thrombus (T2-weighted coronal MRI).
Figure 3.
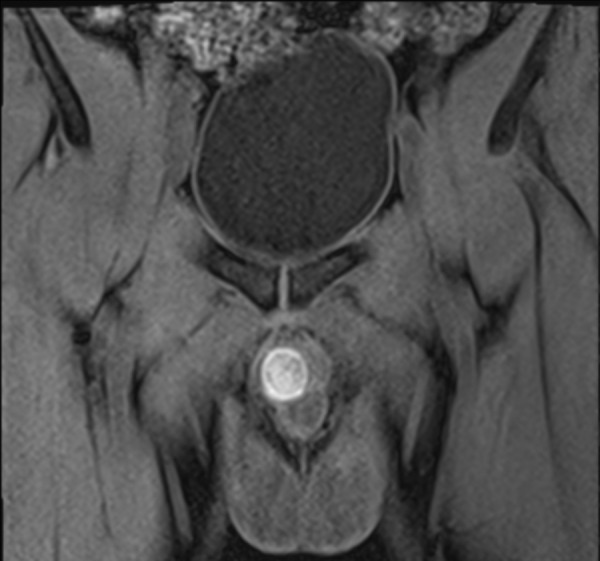
Distended right corpus cavernosum with an acute thrombus (white) (precontrast T1-weighted MRI).
Figure 4.
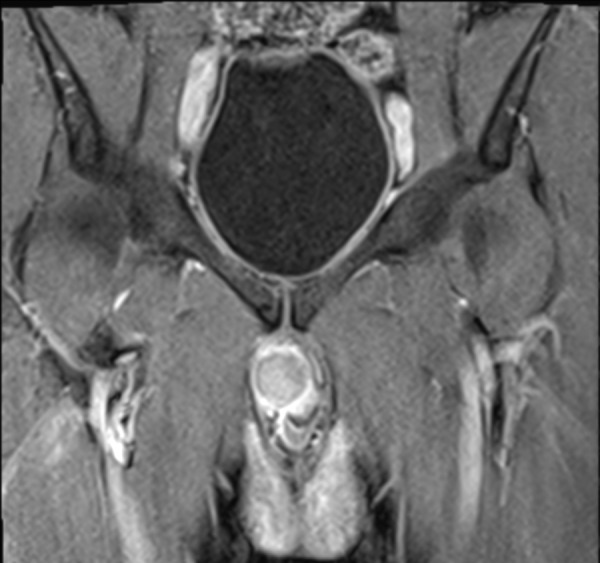
Non-enhancement of the thrombus following contrast (postcontrast T1-weighted MRI).
Coagulation studies revealed a mildly raised fibrinogen of 4.2 g/L, but prothrombin time (13 s), international normalised ratio (1.05), activated partial thromboplastin time (32 s) and thrombin time (17 s) were all within normal limits.
Treatment
He was started on aspirin 75 mg and a PDE-5i (tadalafil 5 mg once daily) to treat the erectile dysfunction. Following a haematology consultation, he was started on a direct inhibitor of activated factor Xa, rivaroxaban 20 mg. His perineal and penile pain were managed with paracetamol and non-steroidal anti-inflammatory medication when required.
Outcome and follow-up
Following 5 months of oral anticoagulant treatment, the lump had reduced in size on clinical examination and the patient was able to achieve normal erections using 5 mg daily tadalafil and had no development of penile curvature. His pain had also improved. Follow-up MRI showed that the segmental thrombus reduced in size to 7.5 cm, with a thin rim of normal cavernosal tissue appearing circumferentially; the high T1 signal resolved in keeping with maturation of the thrombus (figures 5–8). Further imaging 4 months later showed a further reduction in the size of the thrombus and a decision was made to stop the oral anticoagulants.
Figure 5.
Resolving partial segmental thrombosis of the corpus cavernosum (T2-weighted sagittal MRI).
Figure 6.
Thin rim of normal cavernosal tissue appearing circumferentially in the right corpus cavernosum (T2-weighted coronal MRI).
Figure 7.

Low T1 signal matured thrombus (precontrast T1-weighted coronal MRI).
Figure 8.

Non-enhancement of the thrombus following contrast (postcontrast T1-weighted MRI).
A year later, this patient remained well with no recurrence of PSTCC and able to achieve good erections without the need for ongoing treatment with a PDE-5i.
Discussion
PSTCC is a rare condition, with only 58 cases reported in the literature and usually presents in young men with a mean age of 31 (range 18–59 years).1–35 However, as more patients with acute and chronic perineal and genital pain are investigated with MRI, there are likely to be more cases diagnosed.9 13 15 17 18 20 21 23 24 27 28 30 32–35
The underlying cause is still unclear, but in earlier case reports where surgical exploration was the preferred management for pain, a fibrous septum was found within the corpus cavernosum separating the proximal part of the thrombus from the uninvolved distal corpus cavernosum.1–3 11 23 27 33 Ilicki et al27 suggested a two-hit model in which a transverse membrane divides the corpus into a proximal and distal portion and a trigger event such as microtrauma during vigorous sexual activity or prolonged cycling resulting in the formation of the thrombus. 36 We suspect that the cause of the PSTCC in this case was a combination of microtrauma during cycling and the presence of a fibrous septum illustrated in figure 1.9 11 14 18 30 31 33 36 This theory has also been proposed in recent case series published by Weyne et al.33
Risk factors associated with PSTCC are: haematological abnormalities such as thrombophilia or sickle-cell disease; alcohol or drug abuse such as cocaine or marijuana and hypercoagulability associated with dehydration, surgery, malignancy and long-distance flights.8 16 18 27 31 34 35 Hyperhomocysteinaemia and a-blockers have also been associated with PSTCC.21 24
The most common symptoms described in the literature are perineal and penile pain together with a palpable lump.2 4 6 7 9 10 13 16–18 26 27 29 32–35 Depending on the position of the thrombus, the penis can appear semierect.6 27 32 33 It almost always occurs unilaterally and bilateral PSTCC has been rarely reported.1 33 Although it has been described in the past as partial priapism, a prolonged and painful erection is not always present.1–8 10 The more appropriate term partial segmental thrombosis of the corpus cavernoum was introduced in 1988.9 Erectile dysfunction is also reported but generally improves within 3–6 months of conservative treatment with anticoagulants without the need for ongoing pharmacotherapy.16 17 29
It is important to establish the cause of the perineal pain and mass in the early stages of presentation, and to exclude an underlying inflammatory or malignant lesion.32 37 In cases where the presentation and history are unclear or a malignancy is suspected, computerised tomography imaging is advisable.6 16 22 37 Contrast-enhanced MRI, contrast-enhanced ultrasound (CEUS) or ultrasound Doppler can be used to confirm the presence of the thrombus within the corpus cavernosum, as a well-defined non-enhancing mass.9 13 14 17 18 20 22 23 32 Although CEUS is cheaper than performing serial MRI imaging, it is operator-dependent.32
This condition has been treated by percutaneous or surgical intervention in the past, either by needle aspiration, shunt procedure or open surgical evacuation of the thrombus.1–4 6 7 16 24 29 33 Although conservative management of PSTCC has been described in the literature since 1988 with comparable clinical outcomes, in cases where significant pain persists despite oral analgesia, an evacuation of the thrombus is justified.9 11 16 24 29 33
Historically, all patients receiving conservative treatment for PSTCC have had a good outcome irrespective of treatment modality. Kimball et al9 in 1988 did not administer any medical treatment and resolution of the thrombus began within a month of its occurrence. Additionally, several cases have reported successful treatment of PSTCC with aspirin or non-steroidal anti-inflammatory drugs (NSAIDs) alone.11 18 23 25 31 However, low molecular weight heparin (LMWH) has been used more frequently in practice for the treatment of PSTCC, although the benefit over NSAIDs is unclear.13 17 18 20 26 27 29 32 33
We report the first case successfully treated with oral rivaroxaban and a PDE-5i. Considering the similarities between PSTCC and deep vein thrombosis, we considered treating our patient with a Xa inhibitor because of its non-invasive administration compared with LMWH and the dosage did not require monitoring during treatment. Although Xa inhibitors have certain benefits in their administration, there have not been any treatment failures reported with aspirin or NSAIDs and the risks and benefits from each drug need to be considered. Additionally, any clinician considering Xa inhibitors for the treatment of PSTCC should consult a haematologist first and all patients should undergo routine blood tests and a thrombophilia screen on presentation prior to starting anticoagulants.27 32 33
Sequential imaging with MRI is advised as this will identify thrombus resolution in conjunction with a clinical assessment and can help in guiding the medical management. A further MRI scan once the thrombus has completely resolved can help in identifying a fibrous septum which was not evident in earlier imaging.33 Owing to minimal long-term data on outcomes, we recommend a follow-up by a specialist for at least 1 year, especially in the presence of erectile dysfunction or cavernosal fibrosis. PSTCC recurrence and long-term complications following medical management are still unknown and patients should be warned about this prior to discharge from specialist follow-up.30 31 33
Learning points.
Segmental thrombosis of the corpus cavernosum is rare, but should be suspected when a patient presents with perineal or penile pain and a palpable lump.
MRI of the pelvis and penis (T2-weighted and T1-weighted precontrast and postcontrast images) will identify a thrombus within the corpus cavernosum. The high T1 signal is the most important feature to look out for.
Patients should be referred for a specialist assessment and appropriate anticoagulants should be started following a haematology review. As the evidence of this disease is based only on case studies; medical treatment and follow-up should be adjusted to the patients' needs and risk factors.
Footnotes
Contributors: MC wrote the article and AP, NR and AM participated in the editing of the article.
Competing interests: None declared.
Patient consent: Obtained.
Provenance and peer review: Not commissioned; externally peer reviewed.
References
- 1.Hillis RS, Weems WL. Priapism: an unusual presentation. J Urol 1976;116:124–5. [DOI] [PubMed] [Google Scholar]
- 2.Gottesman JE. Recurrent partial priapism. Urology 1976;7:519–20. 10.1016/0090-4295(76)90195-3 [DOI] [PubMed] [Google Scholar]
- 3.Johnson GR, Corriers JN Jr. Partial priapism. J Urol 1980;124:147–8. [DOI] [PubMed] [Google Scholar]
- 4.Llado J, Peterson LJ, Fair WR. Pripism of the proximal penis. J Urol 1980;123:779–80. [DOI] [PubMed] [Google Scholar]
- 5.Roa RM, Roa LM. [Partial priapisms. Proximal priapism. Report of a case]. Arch Esp Urol 1981;34:297–300. [PubMed] [Google Scholar]
- 6.Burkhalter JL, Morano JU. Partial priapism: the role of CT in its diagnosis. Radiology 1985;156:159 10.1148/radiology.156.1.4001404 [DOI] [PubMed] [Google Scholar]
- 7.Borrelli M, Glina S, Wroclawski ER et al. Segmental priapism. Urol Int 1986;41:156–7. 10.1159/000281187 [DOI] [PubMed] [Google Scholar]
- 8.Sparwasser C, Danz B, Thon WF. [Segmental unilateral priapism—a case report]. Urologe A 1988;27:266–8. [PubMed] [Google Scholar]
- 9.Kimball DA, Yuh WT, Farner RM. MR diagnosis of penile thrombosis. J Comput Assist Tomogr 1988;12:604–7. 10.1097/00004728-198807000-00012 [DOI] [PubMed] [Google Scholar]
- 10.De Zan A, Gamba P, Piana P et al. [A case of priapism of the proximal corpora cavernosa]. Minerva Urol Nefrol 1993;45:29–30. [PubMed] [Google Scholar]
- 11.Ptak T, Larsen CR, Beckmann CF et al. Idiopathic segmental thrombosis of the corpus cavernosum as a cause of partial priapism. Abdom Imaging 1994;19:564–6. 10.1007/BF00198267 [DOI] [PubMed] [Google Scholar]
- 12.Albrecht W, Stackl W. Treatment of partial priapism with an intracavernous injection of etilefrine. JAMA 1997;277:378 10.1001/jama.1997.03540290030027 [DOI] [PubMed] [Google Scholar]
- 13.Thiel R, Kahn T, Vögeli TA. Idiopathic partial thrombosis of the corpus cavernosum. Urol Int 1998;60:178–80. 10.1159/000030246 [DOI] [PubMed] [Google Scholar]
- 14.Machtens SA, Kuczyk MA, Becker AJ et al. Partial unilateral penile thrombosis: magnetic resonance imaging and management. J Urol 1998;160:494–5. 10.1016/S0022-5347(01)62935-5 [DOI] [PubMed] [Google Scholar]
- 15.Schneede P, Schmeller N, Müller-Lisse UG et al. Partial priapism. Case report and review of the literature of diagnostic and therapeutic measures. Urologe A 1999;38:179–83. [DOI] [PubMed] [Google Scholar]
- 16.Lewis JH, Javidan J, Keoleian CM et al. Management of partial segmental priapism. Urology 2001;57:169 10.1016/S0090-4295(00)00851-7 [DOI] [PubMed] [Google Scholar]
- 17.Pegios W, Rausch M, Balzer JO et al. MRI and color-coded duplex sonography: diagnosis of partial priapism. Eur Radiol 2002;12:2532–5. 10.1007/s00330-001-1199-8 [DOI] [PubMed] [Google Scholar]
- 18.Goeman L, Joniau S, Oyen R et al. Idiopathic partial thrombosis of the corpus cavernosum: conservative management is effective and possible. Eur Urol 2003;44:119–23. 10.1016/S0302-2838(03)00217-3 [DOI] [PubMed] [Google Scholar]
- 19.Horger DC, Wingo MS, Keane TE. Partial segmental thrombosis of corpus cavernosum: case report and review of world literature. Urology 2005;66:194 10.1016/j.urology.2005.01.011 [DOI] [PubMed] [Google Scholar]
- 20.Dubois F, Lesur G, Azzouzi AR et al. [Partial thrombosis of the corpus cavernosum. Must a clotting disorder be systematically investigated?] Prog Urol 2007;17:866–8. 10.1016/S1166-7087(07)92310-6 [DOI] [PubMed] [Google Scholar]
- 21.Blaut S, Schneider M, Zschuppe E et al. [Partial unilateral penile thrombosis of corpus cavernosum due to hyperhomocysteinemia. Case report and references]. Urologe A 2008;47:748–52. 10.1007/s00120-008-1650-4 [DOI] [PubMed] [Google Scholar]
- 22.Asbach P, Oelrich B, Haase O et al. Acute partial segmental thrombosis of the corpus cavernosum: imaging findings on ultrasound, computed tomography, and magnetic resonance imaging. Clin Imaging 2008;32:400–2. 10.1016/j.clinimag.2008.02.022 [DOI] [PubMed] [Google Scholar]
- 23.Galvin SD, Letts JA, Sampangi NR. Magnetic resonance imaging of partial segmental priapism (segmental thrombosis of corpus cavernosum). Urology 2009;73:275–6. 10.1016/j.urology.2008.06.040 [DOI] [PubMed] [Google Scholar]
- 24.Kilinc M, Piskin M, Guven S et al. Partial priapism secondary to tamsulosin: a case report and review of the literature. Andrologia 2009;41:199–201. 10.1111/j.1439-0272.2008.00908.x [DOI] [PubMed] [Google Scholar]
- 25.Patel RP, Mucksavage P, Ramchandani P et al. Idiopathic partial thrombosis of the corpus cavernosum. Urology 2010;76:1373–4. 10.1016/j.urology.2009.12.058 [DOI] [PubMed] [Google Scholar]
- 26.Głuchowski J, Bławat A, Kordasz J et al. Partial segmental thrombosis of the corpus cavernosum. Cent Eur J Urol 2011;64:264–5. 10.5173/ceju.2011.04.art19 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Ilicki J, Krauss W, Anderson SO. Partial segmental thrombosis of the corpus cavernosum: a case report and a review of the literature. Urology 2012;79:708–12. 10.1016/j.urology.2011.11.032 [DOI] [PubMed] [Google Scholar]
- 28.Pepe P, Panella P, Candiano G et al. Partial priapism secondary to idiophatic segmental thrombosis of corpora cavernosa. Arch Ital Urol Androl 2012;84:101–3. [PubMed] [Google Scholar]
- 29.Hoyerup P, Azawi NH. Partial priapism. BMJ Case Rep 2013;2013:bcr2013200031 10.1136/bcr-2013-200031 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Hulth M, Albersen M, Fode M et al. Idiopathic partial thrombosis of the corpus cavernosum: aetiology, diagnosis and treatment. Scand J Urol 2013;47:163–8. 10.3109/00365599.2012.698305 [DOI] [PubMed] [Google Scholar]
- 31.Kropman RF, Schipper J. Hematoma or ‘Partial Priapism’ in the proximal part of the corpus cavernosum. J Sex Med 2014;11:2618–22. 10.1111/jsm.12388 [DOI] [PubMed] [Google Scholar]
- 32.Sauer S, Goltz JP, Gassenmaier T et al. Partial segmental thrombosis of the corpus cavernosum (PSTCC) diagnosed by contrast-enhanced ultrasound: a case report. BMC Urol 2014;14:100 10.1186/1471-2490-14-100 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Weyne E, Schillebeeckx C, Jamaer C et al. Idiopathic partial thrombosis (IPT) of the corpus cavernosum: a hypothesis-generating case series and review of the literature. J Sex Med 2015;12:2118–25. 10.1111/jsm.13036 [DOI] [PubMed] [Google Scholar]
- 34.Eovaldi B, Dunn DP. Case report: corpus cavernosum thrombosis occurring during a long-range aviation mission initially diagnosed as lymphoma. Mil Med 2015;180:e608–10. 10.7205/MILMED-D-14-00506 [DOI] [PubMed] [Google Scholar]
- 35.Gomez Gomez E, Campos Hernandez JP, Cazalilla M et al. Partial thrombosis of the corpus cavernosum: should we dig deeper into coagulopathy disorders? Andrologia 2016; 10.1111/and.12572 10.1111/and.12572 [DOI] [PubMed] [Google Scholar]
- 36.Leibovitch I, Mor Y. The vicious cycling: bicycling related urogenital disorders. Eur Urol 2005;47:277–86. 10.1016/j.eururo.2004.10.024 [DOI] [PubMed] [Google Scholar]
- 37.Gentile G, Broccoli A, Brunocilla E et al. An isolated penile mass in a young adult turned out to be a primary marginal zone lymphoma of the penis. A case report and a review of literature. Anticancer Res 2013;33:2639–42. [PubMed] [Google Scholar]


