Abstract
Right ventricular (RV) pacing has been reported to result in ventricular dyssynchrony, heart failure, and increased mortality. Pacing associated deterioration of left ventricular (LV) systolic function has been termed pacing-induced cardiomyopathy (PICM). While upgrading to biventricular pacing (BiVP) is an effective therapy for PICM, permanent His-bundle pacing (HBP) can be a physiological alternative to BiVP. We present a patient with PICM who responded dramatically to permanent HBP.
Keywords: Cardiac resynchronization therapy, Cardiomyopathy, His-bundle pacing
1. Introduction
Right ventricular (RV) pacing can lead to progressive left ventricular (LV) systolic dysfunction and heart failure due to electrical and mechanical dyssynchrony. The deleterious effect of RV pacing on LV systolic function has been termed pacing-induced cardiomyopathy (PICM). Upgrading to biventricular pacing (BiVP) reverses LV remodeling in patients with PICM as it does in primary BiVP recipients. On the other hand, in patients requiring cardiac resynchronization therapy (CRT), permanent His-bundle pacing (HBP) can be a physiological alternative to BiVP. We present a patient with PICM who was treated successfully by permanent HBP.
2. Case report
An 87-year-old woman with chronic heart failure and chronic kidney disease (CKD) was admitted to our hospital due to worsening dyspnea and lower extremity edema. She had undergone permanent pacemaker implantation 6 years before because of 2:1 atrioventricular (AV) block with a narrow QRS complex (Fig. 1A). Her medications included torasemide 4 mg, carvedilol 5 mg, and valsartan 40 mg. A 12-lead electrocardiogram (ECG) showed atrial sensed ventricular pacing with a QRS duration of 140 ms (Fig. 1B). Pacemaker interrogation revealed that her native cardiac rhythm remained 2:1 AV block with a narrow QRS, and ventricular pacing was greater than 99%. Echocardiography showed a left ventricular ejection fraction (LVEF) of 33%. Chest X-ray revealed an enlarged cardiothoracic ratio (CTR) of 60% and bilateral pleural effusions (Fig. 2A). Coronary angiography and echocardiography performed before pacemaker implantation had revealed normal coronary arteries and a LVEF of 65%, respectively. PICM was highly suspected. Further medical treatment with carperitide and intravenous furosemide did not improve the pleural effusions or LVEF. CRT by either HBP or a standard LV lead was considered. Because the patient׳s native cardiac rhythm remained 2:1 AV block with a narrow QRS, we thought HBP would be better than BiVP, and thus we attempted permanent HBP as the first-line treatment. Although the His bundle (HB) electrogram could not be clearly identified, narrow QRS complexes suggesting nonselective HBP (His capture fused with local ventricular septal capture) were easily obtained using a SelectSecure 3830 screw-in lead inserted through a SelectSite C304 deflectable catheter (Medtronic, Minneapolis, MN, USA) by pace-mapping the AV septum. The pacing thresholds of the HB and the adjacent septal myocardium were 1.0 V/0.4 ms and 0.75 V/0.4 ms, respectively. The HB pacing lead was connected to the LV port of a biventricular (BiV) pacemaker (Viva CRT-P, Medtronic). We chose this device because it has no sensing ability in the LV lead (in this case, the HB lead) and thus does not cause double counts with a delay in the HV interval and safety pacing in RV pacing. The BiV pacemaker was programmed to DDD mode with a LV–RV delay of 80 ms. This delay was set to provide back-up RV pacing in case the HB pacing lead failed to capture the right ventricle. After the 1-week follow-up, the pacing threshold of the HB had improved slightly to 0.75 V/0.4 ms, while that of the adjacent septal myocardium was 1.0 V/0.4 ms. Echocardiography at 1 month after the upgrade demonstrated improvement in the patient׳s LVEF from 33% to 45%, and the brain natriuretic peptide level decreased from 1208 pg/ml to 97 pg/ml.
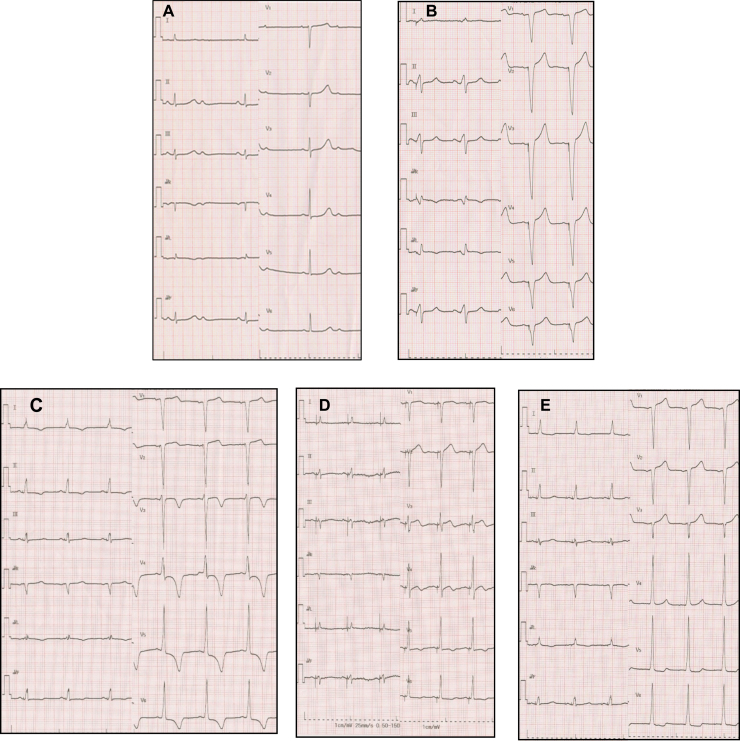
Fig. 1.
(A) The patient׳s native cardiac rhythm showing 2:1 AV block with narrow QRS complexes (QRS duration of 90 ms). (B) ECG at admission. Atrial sensed ventricular pacing with QRS duration of 140 ms. (C) ECG immediately after implantation of HB pacing lead. Atrial sensed ventricular pacing (BiV pacing mode) suggesting nonselective HBP (His-capture fused with ventricular septal capture) evidenced by a narrow QRS with a duration of 110 ms and the presence of a slurred upstroke immediately after pacing spike indicating local myocardial capture. Also note T-wave changes suggesting cardiac memory. (D) ECG at the 1-week follow-up recorded at pacing output setting of 0.75 V/0.4 ms (HB threshold). Note the isoelectronic interval between the pacing spike and QRS onset and QRS morphology similar to native QRS, suggesting pure HB capture. (E) ECG at the 6-month follow-up. AV sequential pacing (BiV pacing mode) showing nonselective HBP with QRS duration of 105 ms.
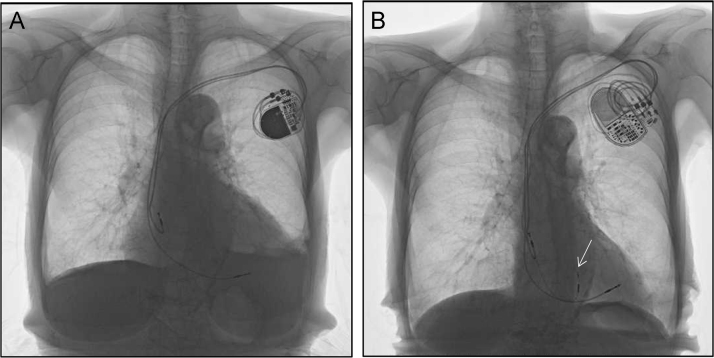
Fig. 2.
(A) Chest X-ray at admission showing enlarged cardiothoracic ratio of 60% with bilateral pleural effusions. (B) Chest X-ray at the 6-month follow-up showing reduction in cardiothoracic ratio to 45% without pleural effusion. Arrow indicates the tip of the His-bundle pacing lead.
At the 6-month follow-up, she was asymptomatic. Chest X-ray revealed improvement of the CTR to 45% without pleural effusion (Fig. 2B). Echocardiography demonstrated further improvement of her LVEF to 55%. The pacing threshold of the HB remained stable at 0.75 V/0.4 ms and that of the adjacent septal myocardium was 1.0 V/0.4 ms. ECGs following HBP are shown in Fig. 1C, D, and E.
3. Discussion
Upgrading to BiVP has been reported as an effective therapy for PICM; however, about 30–40% of patients do not respond to this treatment [1]. In addition, performing BiVP can be challenging with a long procedural time and might even be impossible due to the coronary sinus anatomy. Rehwinkel et al. demonstrated that upgrading to HBP could be an effective alternative to BiVP for PICM with preserved His-Purkinje conduction [2].
Because our patient׳s native rhythm remained 2:1 AV block with a narrow QRS, we attempted HBP as the first-line treatment based on the assumption that His-Purkinje conduction might be preserved. Another benefit of HBP in this patient with CKD is that the use of iodinated contrast media could be avoided. HBP using a deflectable lead delivery system was easily achieved with a fluoroscopic time of 8 minutes. Lustgarten et al. reported that HB pacing lead placement with this system was no more difficult and took less time to implant than placement of a LV lead [3].
Our patient is thought to be a super-responder to CRT by HBP although the form of HBP was nonselective. However, there seems to be no significant clinical difference between selective HBP (His-only capture) and nonselective HBP because both forms do not alter physiological impulse conduction and possibly maintain rapid and synchronous LV activation. Indeed, Catanzariti et al. reported that no difference was observed between the two forms of HBP at acute measures of dyssynchrony [4].
Most patients with PICM having a native narrow QRS have preserved His-Purkinje conduction, and therefore upgrading to HBP would be expected to restore physiological synchronous LV activation. Recently, Vijayaraman et al. demonstrated that His-Purkinje conduction could be normalized by permanent HBP in 76% of patients with infranodal AV block and a wide QRS complex, indicating intra-His block [5]. This finding suggests that many patients with PICM having a native wide QRS might have preserved distal His-Purkinje conduction, and permanent HBP at the distal HB (distal to the site of the block/delay) could restore physiological synchronous LV activation.
The HB pacing threshold remained excellent in our patient at the 6-month follow-up; however, long-term follow-up is necessary. Theoretically, HBP is a more physiological treatment than BiVP in patients with PICM having preserved His-Purkinje conduction. Further studies are needed to evaluate the long-term safety and efficacy of permanent HBP in patients with PICM.
In conclusion, we present a patient with PICM who was successfully upgraded to HBP. This case shows that permanent HBP can be an effective alternative to BiVP with significant improvements in heart failure symptoms and LVEF.
Conflict of interest
All authors declare no conflict of interest related to this study.
References
- 1.Fröhlich G., Steffel J., Hürlimann D. Upgrading to resynchronization therapy after chronic right ventricular pacing improves left ventricular remodelling. Eur Heart J. 2010;31:1477–1485. doi: 10.1093/eurheartj/ehq065. [DOI] [PubMed] [Google Scholar]
- 2.Rehwinkel A.E., Müeller J., Vanburen P.C. Ventricular resynchronization by implementation of direct His bundle pacing in a patient with congenital complete AV block and newly diagnosed cardiomyopathy. J Cardiovasc Electrophysiol. 2011;22:818–821. doi: 10.1111/j.1540-8167.2010.01969.x. [DOI] [PubMed] [Google Scholar]
- 3.Lustgarten D.L., Calame S., Crespo E.M. Electrical resynchronization induced by direct His-bundle pacing. Heart Rhythm. 2010;7:15–21. doi: 10.1016/j.hrthm.2009.09.066. [DOI] [PubMed] [Google Scholar]
- 4.Catanzariti D., Maines M., Cemin C. Permanent direct his bundle pacing does not induce ventricular dyssynchrony unlike conventional right ventricular apical pacing. An intrapatient acute comparison study. J Interv Card Electrophysiol. 2006;16:81–92. doi: 10.1007/s10840-006-9033-5. [DOI] [PubMed] [Google Scholar]
- 5.Vijayaraman P., Naperkowski A., Ellenbogen K.A. Electrophysiologic insights into site of atrioventricular block. Lessons from permanent His bundle pacing. JACC: Clin Electrophysiol. 2015;1:571–581. doi: 10.1016/j.jacep.2015.09.012. [DOI] [PubMed] [Google Scholar]