Abstract
Objective
Switzerland has mountains and valleys complicating the access to a hospital and critical care in case of emergencies. Treatment success for acute myocardial infarction (AMI) or stroke depends on timely treatment. We examined the relationship between distance to different hospital types and mortality from AMI or stroke in the Swiss National Cohort (SNC) Study.
Design and setting
The SNC is a longitudinal mortality study of the census 2000 population of Switzerland. For 4.5 million Swiss residents not living in a nursing home and older than 30 years in the year 2000, we calculated driving time and straight-line distance from their home to the nearest acute, acute with emergency room, central and university hospital (in total 173 hospitals). On the basis of quintiles, we used multivariable Cox proportional hazard models to estimate HRs of AMI and stroke mortality for driving time distance groups compared to the closest distance group.
Results
Over 8 years, 19 301 AMI and 21 931 stroke deaths occurred. Mean driving time to the nearest acute hospital was 6.5 min (29.7 min to a university hospital). For AMI mortality, driving time to a university hospital showed the strongest association among the four types of hospitals with a hazard ratio (HR) of 1.19 (95% CI 1.10 to 1.30) and 1.10 (95% CI 1.01 to 1.20) for men and women aged 65+ years when comparing the highest quintile with the lowest quintile of driving time. For stroke mortality, the association with university hospital driving time was less pronounced than for AMI mortality and did not show a clear incremental pattern with increasing driving time. There was no association with driving time to the nearest hospital.
Conclusions
The increasing AMI mortality with increasing driving time to the nearest university hospital but not to any nearest hospital reflects a complex interplay of many factors along the care pathway.
Keywords: Distance to hospital, acute myocardial infarction, mortality
Strengths and limitations of this study.
Data from a nationwide cohort with almost complete mortality follow-up during the study period were used to investigate the relationship between distance from home to hospital and dying from acute myocardial infarction (AMI) or stroke.
Driving time and straight-line distance quantify the actual travel time by car and the distance when using helicopter transportation.
We lacked information on the exact location where the AMI or stroke occurred, but as the average age of persons experiencing an AMI or stroke is clearly above the retirement age of 65 years, home can be assumed to be a good approximation for the place of the event.
Information whether death occurred before being admitted to a hospital was lacking in our data but should be accounted for in future research.
Introduction
Life-threatening diseases such as acute myocardial infarction (AMI) or stroke need immediate medical intervention. Multiple factors can influence the time to treatment and thus survival. These include time from the event to the alert of emergency medical services (EMS), presence of a person to perform cardiopulmonary resuscitation, availability of an automated external defibrillator, travel time to a hospital with necessary specialised treatment (eg, thrombolysis or percutaneous coronary intervention (PCI)) and door-to-balloon time.
The European guidelines on myocardial revascularisation indicate that the greatest benefit from reperfusion therapy occurs 2–3 hours after onset.1 The recommendations for ST segment elevation myocardial infarction (STEMI) and non-ST segment elevation acute coronary syndrome (NSTE-ACS) differ according to available treatment and patient risk profile. Patients with STEMI should be treated without delay, whereas patients with NSTE-ACS should receive revascularisation within 24 hours, but in any event no later than 72 hours after onset. However, high-risk patients with NSTE-ACS should undergo urgent coronary angiography within 2 hours of onset. In patients with STEMI, primary PCI without previous fibrinolysis is now recommended over fibrinolysis as the preferred reperfusion therapy if it can be provided in a timely manner by experienced operators. However, if PCI cannot be performed within 120 min of contact with the health system, patients should receive fibrinolysis followed by angiography.1
In a Danish study of patients with STEMI for whom the time from first contact with the healthcare system to initiation of reperfusion therapy was no longer than 60 min had a long-term mortality of 15.4%, clearly lower than the 30.8% mortality of patients with a delay of 181 to 360 min.2 An Italian study showed that with higher distance from place of residence to the nearest hospital, the risk of out-of-hospital mortality increased.3 In Arkansas, the risk of AMI mortality was higher for the population living in neighbourhoods with a long driving time to the nearest PCI-capable hospital.4 In a study from Greece, more than 10 km distance from the place of AMI onset to the hospital was associated with delayed hospital arrival.5 Patients with AMI being referred via field triage, a prehospital diagnosis by ambulance staff, direct referral to a hospital being specialised in the treatment of patients with AMI, and short time to presentation at a high-volume primary PCI centre were factors that reduced the time to EMS contact and start of reperfusion therapy as well as improved health outcomes as, for example, survival.6–9
The 2008 European guidelines for stroke treatment recommend intravenous thrombolysis within 3 hours of stroke onset.10 The following year, the treatment window was extended to 4.5 hours.11 The American Heart Association/American Stroke Association updated in 2013 their guidelines for early management of patients with acute ischaemic stroke regarding endovascular treatment. The results of new randomised clinical trials provided evidence that endovascular therapy with a stent retriever when performed within 6 hours from onset improved the results for recanalisation rates and clinical outcome.12 Hospital type (eg, academic hospital, primary stroke centre) and hospital volume of treated patients with stroke as well as the travel time were associated in several studies with risk of dying from a stroke.13–15
The windows for reperfusion therapy in patients with AMI and stroke indicate prompt notification of the EMS and rapid transportation to the nearest hospital with the appropriate treatment facilities. Geographical inequalities in the provision of healthcare have been shown to influence the likelihood of dying from AMI or stroke.
In Switzerland, the structural planning of hospitals and their service type happens at the level of the 26 cantons with some coordination across cantons.16 The decision of emergency services to which hospital to admit possible patients with AMI or stroke is regionally organised via the cantonal rescue coordination centres. In 2011, an intercantonal agreement defined for the first time eight accredited stroke centres (http://www.neurovasc.ch/index.php/stroke-units.html), among them all the university hospitals. Inhabitants of remote areas, peripheral valleys or mountainous regions often face long travel distances to the nearest hospital, which may not necessarily be a hospital specialised in AMI or stroke treatment with a catheter laboratory or a stroke unit. This will affect transport time, treatment and survival. Switzerland has a high-hospital density and efficient ambulance and air rescue services,17 which should reduce AMI and stroke mortality for people living farther from hospitals. However, no study has yet assessed the relation between AMI and stroke mortality, and distance to hospitals in Switzerland. We therefore used Swiss National Cohort (SNC) data to assess for the years 2000 to 2008 how AMI and stroke mortality in Switzerland relate to distance as driving time from home to different types of hospitals.
Data and methods
Swiss National Cohort
The SNC is a longitudinal study that links census data for the entire population of Switzerland with mortality and emigration records. In addition to sociodemographic and economic variables, the SNC also includes the geographical coordinates of residences. However, owing to the lack of a unique person identifier and the anonymous death registry in Switzerland, the records of the census of 2000 and the death and emigration records up to 2008 were linked using deterministic and probabilistic linkage methods based on sex, date of birth, place of residence, nationality, marital status, religion, profession and, if available, date of birth of partner or children. The SNC and details regarding the linkage process are described in detail elsewhere.18–20
Hospital information
Annually, the Federal Office for Health (FOH) derives key figures for Swiss hospitals from hospital characteristics and discharge statistics available from the Swiss Federal Statistical Office (SFSO, http://www.bag.admin.ch/kzss). However, those data do not provide addresses and further information for all individual hospitals when a single corporate entity operates more than one hospital in one town or canton. We therefore used additional data from the Federal Office of Topography (swisstopo) and TomTom to locate individual hospitals.
We derived the geographical coordinates of the FOH data set using the Geocoding Tools of ArcGIS 10.3 from ESRI based on the TomTom MultiNet Shapefile (2011) for Switzerland which provides several data sets to geocode, to navigate, or which includes points of interests such as hospital location. To identify additional hospital locations, we compared the coordinates of the FOH data set with the hospital coordinates that are provided by swisstopo, and the hospital coordinates provided by the TomTom MultiNet Shapefile. We deleted duplicates and checked for further information about the hospitals via the Internet. We merged the data sets to create one data set with the following information on hospitals operating in 2008: type of hospital (acute care, acute care with emergency room (ER) 24/7, central hospital and university hospital) and geographical coordinates. The wording ‘acute care hospital’ is used to differentiate between hospitals providing the full range of hospital care and institutions which only provide very selected care, like psychiatric inpatient or rehabilitation facilities.
Distance calculation using geographical information system
We calculated two related measures of the distance between residences and hospitals using ArcGIS 10.3: straight-line distance and driving time. Driving times for the road network of Switzerland were calculated using the TomTom MultiNet Shapefile (2011) and ArcGIS Network Analyst. To model the road options for ambulances, we excluded ferries, car-train tunnels and walkways, but included pedestrian areas. Since not all buildings are immediately adjacent to streets, we measured the straight-line distance to the next traversable street segment, assumed 15 km/hour speed for travelling this distance, and adjusted driving distance and time accordingly. These data were then added to the SNC database.
Selection of records
Originally, 7 280 246 persons were included in the 2000 census. We excluded people younger than 30 years at the 2000 census because cardiovascular disease deaths are quite rare in this age group (2 534 036 persons). We also excluded records having no or imprecise building coordinates that are necessary for the calculation of exact distance to hospital (188 423 persons). These buildings also had no Swiss neighbourhood index of socioeconomic position (SSEP) values21 because exact location was necessary for the calculation of the SSEP. Persons with institutional residences, who are older and have poorer health, were also excluded because they have higher stroke or AMI risk than the general population (67 348 persons). Finally, 4 490 439 persons remained in the study. Only records with deaths that were identified by stringent probabilistic linkage were included as death records. Individuals were followed from 5 December 2000 until death, emigration or the end of the study period on 31 December 2008, whichever was first.
The primary cause of death was coded using the International Classification of Disease, Injuries and Causes of Death, 10th revision (ICD-10). Deaths by AMI were coded with I21 or I22 and by stroke with I60, I61, I63 or I64. We performed time-to-event analyses with outcome AMI death or stroke death (separate analyses). We calculated rates by dividing the number of AMI or stroke deaths by the number of person-years at risk and HRs for variables of interest using Cox proportional hazard models.
We analysed the association of driving time and straight-line distance with stroke and AMI mortality using three different Cox proportional hazard models. For the time-to-event analysis, we used individual’s age as time axis, that is, the age at which they were at census 2000 was the starting time and the age at which the event of interest occurred (or emigration or 31 December 2008) was the stopping time. With the choice of this time axis, Cox proportional hazards regression provides HRs for the included predictors which are adjusted for the individual’s age. To account for calendar effects, we used the Stata command stsplit to create a variable dividing the time of observation into an early and a later period. The three models include the following information:
Model 1: hospital distance (driving time or straight-line distance), calendar effect
Model 2: hospital distance, calendar effect, sex, nationality, civil status, religion, education, household type and language region
Model 3: hospital distance, calendar effect, sex, nationality, civil status, religion, education, household type, language region, SSEP and urbanisation.
Analyses were stratified for the younger (30–64 years) and older (≥65 years) persons because other SNC studies have shown differences in the younger and older SNC population.22 23 Additionally, we performed separate analyses for men and women because tests of the proportional hazards assumption showed a strong violation for the sex variable. For further information about the categories of the variables included in the analyses, see table 1. Driving time and straight-line distance to each of the four different hospital types (nearest acute hospital, acute hospital with ER, central hospital or nearest university hospital) were divided by quintiles into five groups. In the Cox regression analyses, we then compared the four more distant groups to the lowest group (see online supplementary appendix 1 and 2 for the quintiles used in our analyses). The map in online supplementary appendix 3 is illustrating the driving distance quintiles to university hospitals for all included buildings in Switzerland and the settlement distribution due to the mountain range of the Alps. Statistical analyses were carried out in Stata V.13 (Stata Corporation, College Station, Texas, USA).
Table 1.
Characteristics of the whole study population and specifically of persons who had died from stroke or AMI during the study period
| Characteristics | Study population |
Stroke deaths |
AMI deaths |
|||||||
|---|---|---|---|---|---|---|---|---|---|---|
| Crude rate per 100 000 |
Crude rate per 100 000 |
|||||||||
| Number | Per cent | Number | Per cent | Rate | 95% CI | Number | Per cent | Rate | 95% CI | |
| All | 4 490 439 | 100 | 21 931 | 100 | 63.8 | 63 to 64.7 | 19 301 | 100 | 56.2 | 55.4 to 57 |
| Gender | ||||||||||
| Male | 2 156 749 | 48 | 9361 | 42.7 | 57.1 | 55.9 to 58.3 | 11 446 | 59.3 | 69.8 | 68.5 to 71.1 |
| Female | 2 333 690 | 52 | 12 570 | 57.3 | 70.0 | 68.8 to 71.2 | 7855 | 40.7 | 43.7 | 42.8 to 44.7 |
| Age (years) | ||||||||||
| 30–34 | 549 551 | 12.2 | 53 | 0.2 | 1.2 | 0.9 to 1.6 | 62 | 0.3 | 1.4 | 1.1 to 1.8 |
| 35–39 | 603 925 | 13.4 | 88 | 0.4 | 1.8 | 1.5 to 2.3 | 174 | 0.9 | 3.6 | 3.1 to 4.2 |
| 40–44 | 547 237 | 12.2 | 162 | 0.7 | 3.7 | 3.2 to 4.4 | 287 | 1.5 | 6.6 | 5.9 to 7.4 |
| 45–49 | 491 143 | 10.9 | 240 | 1.1 | 6.2 | 5.4 to 7 | 479 | 2.5 | 12.3 | 11.3 to 13.5 |
| 50–54 | 478 402 | 10.7 | 344 | 1.6 | 9.1 | 8.2 to 10.2 | 790 | 4.1 | 21.0 | 19.6 to 22.5 |
| 55–59 | 438 264 | 9.8 | 466 | 2.1 | 13.6 | 12.4 to 14.9 | 1065 | 5.5 | 31.1 | 29.3 to 33.1 |
| 60–64 | 342 555 | 7.6 | 744 | 3.4 | 28.2 | 26.3 to 30.3 | 1212 | 6.3 | 46.0 | 43.4 to 48.6 |
| 65–69 | 306 346 | 6.8 | 1440 | 6.6 | 61.9 | 58.8 to 65.2 | 1780 | 9.2 | 76.5 | 73 to 80.2 |
| 70–74 | 267 196 | 6 | 2685 | 12.2 | 136.8 | 131.7 to 142 | 2750 | 14.2 | 140.1 | 134.9 to 145.4 |
| 75–79 | 219 519 | 4.9 | 4596 | 21 | 303.6 | 295 to 312.5 | 3662 | 19 | 241.9 | 234.2 to 249.9 |
| 80–84 | 140 276 | 3.1 | 5408 | 24.7 | 625.0 | 608.5 to 641.9 | 3553 | 18.4 | 410.6 | 397.3 to 424.3 |
| 85–89 | 76 053 | 1.7 | 3941 | 18 | 999.5 | 968.8 to 1031.2 | 2554 | 13.2 | 647.8 | 623.1 to 673.4 |
| 90–94 | 25 576 | 0.6 | 1516 | 6.9 | 1429.7 | 1359.5 to 1503.5 | 798 | 4.1 | 752.6 | 702.1 to 806.6 |
| 95+ | 4396 | 0.1 | 248 | 1.1 | 1773.0 | 1565.5 to 2008 | 135 | 0.7 | 965.1 | 815.3 to 1142.5 |
| Neighbourhood index of SEP | ||||||||||
| Lowest quintile | 898 100 | 20 | 4511 | 20.6 | 66.2 | 64.3 to 68.1 | 4240 | 22 | 62.2 | 60.3 to 64.1 |
| Second quintile | 898 083 | 20 | 4786 | 21.8 | 69.9 | 68 to 71.9 | 4336 | 22.5 | 63.4 | 61.5 to 65.3 |
| Third quintile | 898 089 | 20 | 4577 | 20.9 | 66.6 | 64.7 to 68.6 | 4119 | 21.3 | 59.9 | 58.1 to 61.8 |
| Fourth quintile | 898 081 | 20 | 4210 | 19.2 | 61.0 | 59.2 to 62.8 | 3599 | 18.6 | 52.1 | 50.4 to 53.9 |
| Highest quintile | 898 086 | 20 | 3847 | 17.5 | 55.6 | 53.9 to 57.4 | 3007 | 15.6 | 43.5 | 42 to 45.1 |
| Type of household | ||||||||||
| Single person household | 927 282 | 20.7 | 9048 | 41.3 | 132.5 | 129.8 to 135.2 | 6846 | 35.5 | 100.2 | 97.9 to 102.6 |
| Household with 2 or more persons | 3 563 157 | 79.3 | 12 883 | 58.7 | 46.8 | 46 to 47.6 | 12 455 | 64.5 | 45.3 | 44.5 to 46.1 |
| Marital status | ||||||||||
| Single | 646 207 | 14.4 | 1925 | 8.8 | 38.4 | 36.7 to 40.2 | 1692 | 8.8 | 33.8 | 32.2 to 35.4 |
| Married | 3 110 107 | 69.3 | 10 609 | 48.4 | 44.2 | 43.4 to 45 | 10 865 | 56.3 | 45.3 | 44.4 to 46.1 |
| Widowed | 356 153 | 7.9 | 8151 | 37.2 | 337.5 | 330.3 to 344.9 | 5405 | 28 | 223.8 | 217.9 to 229.9 |
| Divorced | 377 972 | 8.4 | 1246 | 5.7 | 42.6 | 40.3 to 45.1 | 1339 | 6.9 | 45.8 | 43.4 to 48.3 |
| Urbanisation | ||||||||||
| Urban | 1 301 289 | 29 | 7458 | 34 | 75.9 | 74.2 to 77.6 | 6171 | 32 | 62.8 | 61.2 to 64.4 |
| Periurban | 2 034 574 | 45.3 | 8602 | 39.2 | 54.9 | 53.8 to 56.1 | 7652 | 39.6 | 48.9 | 47.8 to 50 |
| Rural | 1 154 576 | 25.7 | 5871 | 26.8 | 66.2 | 64.6 to 67.9 | 5478 | 28.4 | 61.8 | 60.2 to 63.5 |
| Language region | ||||||||||
| German | 3 241 186 | 72.2 | 16 187 | 73.8 | 65.2 | 64.2 to 66.2 | 14 075 | 72.9 | 56.7 | 55.7 to 57.6 |
| French | 1 034 224 | 23 | 4726 | 21.5 | 60.1 | 58.4 to 61.8 | 4223 | 21.9 | 53.7 | 52.1 to 55.3 |
| Italian | 215 029 | 4.8 | 1018 | 4.6 | 61.9 | 58.2 to 65.8 | 1003 | 5.2 | 61.0 | 57.3 to 64.9 |
| Religious affiliation | ||||||||||
| Protestant churches | 1 664 535 | 37.1 | 10 755 | 49 | 84.6 | 83 to 86.2 | 8841 | 45.8 | 69.5 | 68.1 to 71 |
| Roman Catholic church | 1 900 346 | 42.3 | 8481 | 38.7 | 58.3 | 57.1 to 59.6 | 7844 | 40.6 | 54.0 | 52.8 to 55.2 |
| No religious affiliation | 521 035 | 11.6 | 1140 | 5.2 | 28.3 | 26.7 to 30 | 1274 | 6.6 | 31.6 | 29.9 to 33.4 |
| Other/unknown | 404 523 | 9 | 1555 | 7.1 | 50.5 | 48.1 to 53.1 | 1342 | 7 | 43.6 | 41.3 to 46 |
| Nationality | ||||||||||
| Swiss | 3 685 922 | 82.1 | 20 630 | 94.1 | 72.7 | 71.7 to 73.7 | 17 961 | 93.1 | 63.3 | 62.4 to 64.2 |
| Non-Swiss | 804 517 | 17.9 | 1301 | 5.9 | 21.8 | 20.6 to 23 | 1340 | 6.9 | 22.4 | 21.3 to 23.7 |
| Education | ||||||||||
| Compulsory education or less | 1 069 769 | 23.8 | 9989 | 45.5 | 127.1 | 124.7 to 129.7 | 7830 | 40.6 | 99.7 | 97.5 to 101.9 |
| Upper secondary level education | 2 319 761 | 51.7 | 9278 | 42.3 | 51.6 | 50.6 to 52.7 | 8666 | 44.9 | 48.2 | 47.2 to 49.3 |
| Tertiary level education | 997 825 | 22.2 | 2293 | 10.5 | 29.6 | 28.4 to 30.8 | 2478 | 12.8 | 32.0 | 30.7 to 33.2 |
| Not known | 103 084 | 2.3 | 371 | 1.7 | 47.8 | 43.2 to 52.9 | 327 | 1.7 | 42.1 | 37.8 to 47 |
AMI, acute myocardial infarction; SEP, socioeconomic position.
bmjopen-2016-013090supp_appendix1.pdf (37.7KB, pdf)
bmjopen-2016-013090supp_appendix2.pdf (38.6KB, pdf)
bmjopen-2016-013090supp_appendix3.pdf (4.4MB, pdf)
Overview of study population
In 2008, 173 hospitals providing acute care were operating in Switzerland. Of these, 138 had an emergency department (ED), 12 were central hospitals and 5 were university hospitals. The distance calculation used 1 293 780 buildings. Of the 4 490 439 study participants, 48% were male, 76.8% were aged 30 to 64 years, 79.3% lived in households with two or more persons, 69.3% were married, 25.7% lived in rural regions and 72.2% resided in German-speaking Switzerland. About 42.3% were Catholics, 17.9% did not have Swiss citizenship and 22.2% had tertiary level education (see table 1).
Results
Over the 8 years of the study period, 381 659 persons (8.5% of 4 490 439) died. About 51.6% of the deceased were men. A total of 21 931 died of stroke (42.7% male) and 19 301 (59.3% male) died of AMI. The crude mortality rate per 100 000 persons was 63.8 for stroke and 56.2 for AMI (see table 1).
The average driving time to an acute hospital was 6.5 min (maximum 65 min) and 80.8% of persons in the SNC data set could access an acute hospital in <10 min. Just 1.3% had to travel 20 min or more. Seven minutes was the average driving time to an acute hospital with ER, while to reach a central hospital 17.4 min on average were necessary. The average driving time to a university hospital was 29.7 min (maximum 178 min), while 58.2% had to travel 20 min or more (see online supplementary appendix 4, for straight-line distance driving time see online supplementary appendix 5).
bmjopen-2016-013090supp_appendix4.pdf (68.1KB, pdf)
bmjopen-2016-013090supp_appendix5.pdf (68.6KB, pdf)
Results of the Cox proportional hazard model analyses
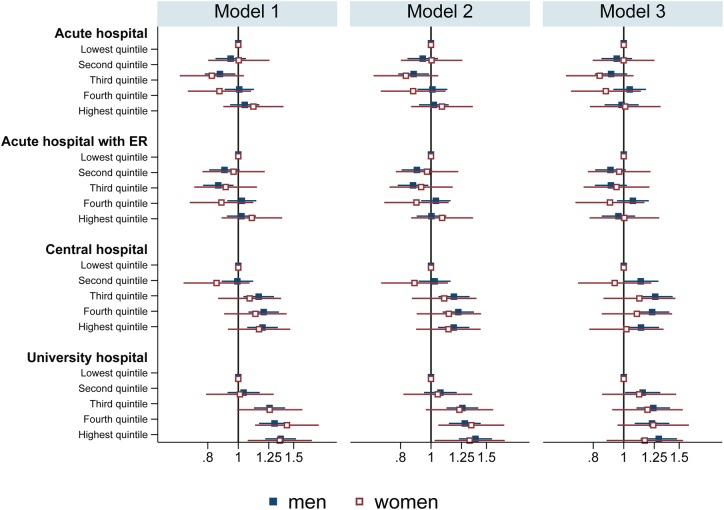
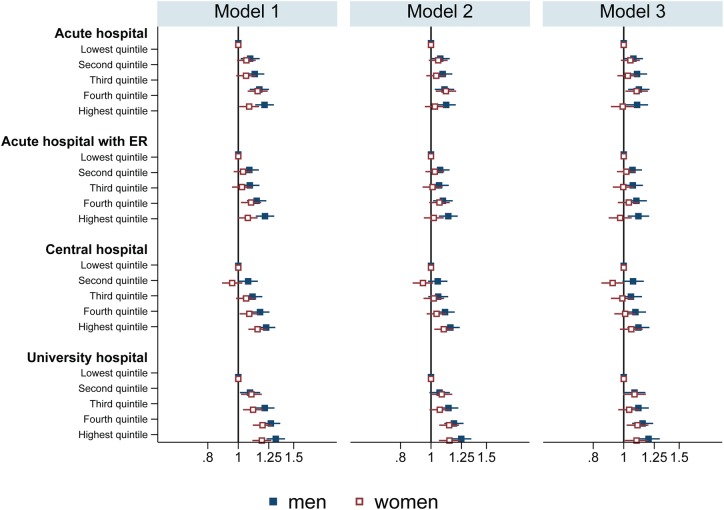
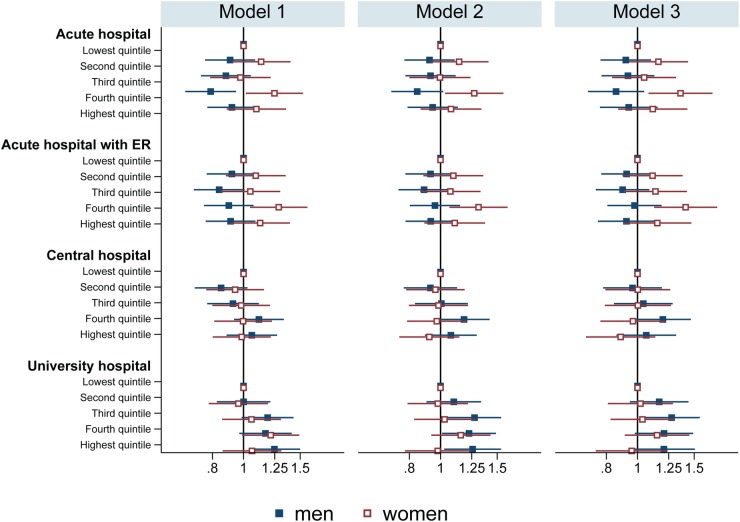
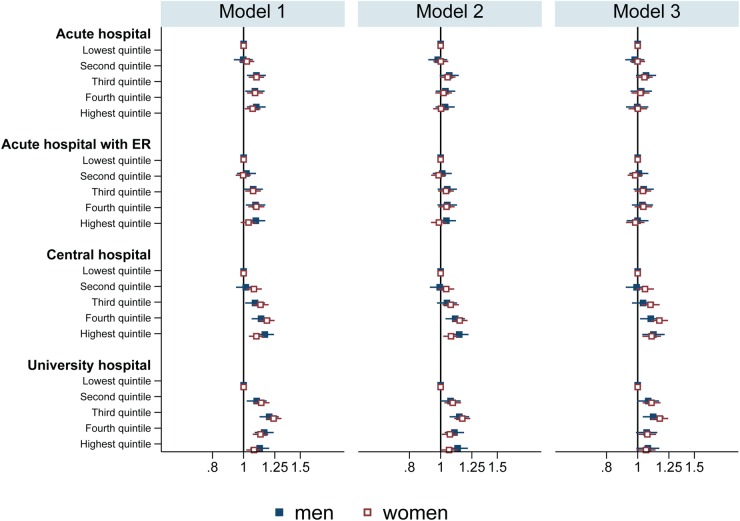
We ran 192 Cox analyses, 96 for driving time and 96 for straight-line distance. Figures 1–4 present the results of these analyses of AMI and stroke deaths for the 30–64 and 65 and older age groups separated by sex. Each figure displays the results of 24 separate analyses (12 for men, 12 for women) for the three models and the driving time to the four different hospital types are displayed (see the tables in online supplementary appendices 6–13 for the exact numbers of the driving time analyses and online supplementary appendices 14–21 for the results of the straight-line distance analyses).
Figure 1.
Results of the Cox proportional hazard model analyses of AMI mortality—driving time quintiles for male and female persons aged 30–64 years under models 1 to 3 for the four different hospital types. AMI, acute myocardial infarction.
Figure 2.
Results of the Cox proportional hazard model analyses of AMI mortality—driving time quintiles for male and female persons aged 65 years and older under models 1 to 3 for the four different hospital types. AMI, acute myocardial infarction.
Figure 3.
Results of the Cox proportional hazard model analyses of stroke mortality—driving time quintiles for male and female persons aged 30–64 years under models 1 to 3 for the four different hospital types.
Figure 4.
Results of the Cox proportional hazard model analyses of stroke mortality—driving time quintiles for male and female persons aged 65 years and older under models 1 to 3 for the four different hospital types.
bmjopen-2016-013090supp_appendix6.pdf (46.1KB, pdf)
bmjopen-2016-013090supp_appendix7.pdf (46.2KB, pdf)
bmjopen-2016-013090supp_appendix8.pdf (46.3KB, pdf)
bmjopen-2016-013090supp_appendix9.pdf (46KB, pdf)
bmjopen-2016-013090supp_appendix10.pdf (46.1KB, pdf)
bmjopen-2016-013090supp_appendix11.pdf (46.1KB, pdf)
bmjopen-2016-013090supp_appendix12.pdf (46KB, pdf)
bmjopen-2016-013090supp_appendix13.pdf (45.8KB, pdf)
bmjopen-2016-013090supp_appendix14.pdf (46.1KB, pdf)
bmjopen-2016-013090supp_appendix15.pdf (46.3KB, pdf)
bmjopen-2016-013090supp_appendix16.pdf (46KB, pdf)
bmjopen-2016-013090supp_appendix17.pdf (46KB, pdf)
bmjopen-2016-013090supp_appendix18.pdf (46.4KB, pdf)
bmjopen-2016-013090supp_appendix19.pdf (46.2KB, pdf)
bmjopen-2016-013090supp_appendix20.pdf (46.2KB, pdf)
bmjopen-2016-013090supp_appendix21.pdf (46.1KB, pdf)
AMI mortality
In younger women (30–64 years), driving time to the nearest acute hospital, hospital with an ER or central hospital was not associated with AMI mortality. The increased AMI mortality with driving time to the nearest university hospital in model 1 diminished in model 2 and disappeared in the fully adjusted model 3 for young women (see figure 1 or online supplementary appendix 6). In younger men, driving time to the nearest central or university hospital was associated with AMI mortality in all three models. For the distance to a university hospital, the hazard of dying from an AMI increased with every quintile. The highest HR of model 3 for a university hospital was observed in the highest quintile with HR=1.29 (95% CI 1.13 to 1.48). For a central hospital, no linear trend was evident. The highest HRs of model 3 were observed for the third (HR=1.26, 95% CI 1.11 to 1.43) and fourth (HR=1.23, 95% CI 1.09 to 1.40) distance groups (see figure 1 or online supplementary appendix 7).
The association of driving time to an acute, central or university hospital found in model 1 for older women (65+ years), diminished in model 2 and disappeared in the fully adjusted model (see figure 2 and online supplementary appendix 8). In contrast, in older men, increasing driving time to all types of hospitals was associated in all three models, although the HRs decreased from model 1 to model 3 and just showed an effect from the fourth quintile onwards, except for acute hospitals in the fully adjusted model (see figure 2 and online supplementary appendix 9).
Stroke mortality
The impact of driving time on stroke mortality is less pronounced than it is for AMI mortality, especially in younger persons (see figures 3 and 4). We found no clear relationship between stroke mortality and driving time for the men and women aged 30 to 64 years (see figure 3). In young women, we found an association of driving time to acute and acute hospital with an ER and stroke mortality always only in the fourth quintile in all three models (acute hospital, model 3: HR=1.36, 95% CI 1.08 to 1.71; acute hospital with ER, model 3: HR=1.41, 95% CI 1.13 to 1.77) (see online supplementary appendix 10). No clear pattern was found for young men (see figure 3 and online supplementary appendix 11). In model 1 for an acute hospital, living in the fourth driving time quintile was protective (HR=0.79, 95% CI 0.66 to 0.95), while for a university hospital living in the highest quintile increased the hazard dying from stroke (HR=1.25, 95%CI 1.04 to 1.50). In the second model, from the third quintile onwards, the stroke mortality risk is increased, but in the fully adjusted model, just the HR of the third quintile is statistically significant (HR=1.28, 95% CI 1.05 to 1.56). In older women and men (figure 4), model 1 showed significant associations between driving time to all types of hospital and stroke mortality. No relationship between driving time to acute hospitals and those with an ER was seen in models 2 and 3 for both men and women. Stroke mortality in older women generally increased with driving time to central and university hospitals in all 3 models, though results were greatest in the fourth quintile (central hospital) or third quintile (university hospital) (see figure 4 and online supplementary appendix 12). In contrast, in older men, the increase in the HR for driving time to the nearest central hospital is linear in all three models, but in model 1 it is just statistically significant for the fourth (HR=1.10, 95% CI 1.02 to 1.19) and highest (HR=1.12, 95% CI 1.03 to 1.21) driving time quintile. For university hospitals, we found higher HR in all models compared to the increased stroke mortality. Compared to the lowest quintile of driving time to a university hospital, we found higher stroke mortality in older men in all three models, but it was not a linear increase. Additionally, in the fully adjusted model 3, only the HR of the third quintile was statistically significant (HR=1.12, 95% CI 1.04 to 1.20) (see figure 4 and online supplementary appendix 13).
Discussion
Main findings
Risk of dying from AMI increased with distance (in driving time) from a central or university hospital for male persons younger and older than 65 years in the SNC. For female persons, this is just true for driving time to the nearest university hospital. For stroke mortality, however, a significant association was just observed with distance to the nearest central and university hospitals in male and female persons aged 65 years and older. However, we did not observe a clear dose–response relationship, as the strongest association was seen when comparing the third (university hospital, male and female) and fourth (central hospital, female) quintiles to the first quintile of distance. For those younger than 65 years, stroke mortality was not clearly associated with distance from any type of hospital once the analyses were adjusted for relevant individual and regional characteristics. Only for the fourth driving time quintile to an acute hospital and those with an ER, we observed a significant increase in stroke mortality in women. Although we found statistically significant increased hazards for AMI and stroke mortality with increasing distance to central and university hospitals, the HRs were relatively small and could be the result of residual confounding.
Possible mechanisms
Our study analysed the outcome of dying from AMI or stroke, which can be seen as the end of a rather complex chain of events and interventions: (1) experiencing the AMI/stroke, (2) someone noticing the AMI/stroke (the patient, if able, or otherwise someone else), (3) alerting the EMS, (4) cardiopulmonary resuscitation and defibrillation if needed by patients with AMI, (5) transport to a treatment facility, (6) treatment, (7) rehabilitation. Differences observed in AMI/stroke mortality by hospital distance could arise in any element of this chain.
The positive association of stroke mortality with distance in those over 65 years might be explained by differences in the awareness and interpretability of stroke symptoms by patients themselves, or by persons in the same household or workplace. Certainly, alarm time might be longer for older people living alone than younger people living in family households. Another possibility is that elderly people, who are known to be at higher risk for stroke,24 might also be more susceptible to time delays due to comorbidities or physical or biochemical disturbances that may accompany a stroke. It might also be possible that, similar to patients with trauma who have been observed to have lower trauma unit admission rates with higher age,25 patients with stroke—especially those from rural areas where the awareness of stroke symptoms might be lower—have lower primary stroke unit admission rates and increased mortality. In any event, treatment of patients who live far from a hospital with a stroke unit might more effectively rely on air transport by helicopter. This preference of the helicopter over the ambulance vehicle might be a possible explanation for the non-linear effect that we found in the stroke mortality analysis for driving time and straight-line distance in central and university hospitals for the elderly (see figure 4). The highest HRs were found in the third or fourth quintile and decreases again in the fourth or highest quintile.
Early after occurrence, AMI (especially STEMI) can have poor survival, while mortality from stroke often occurs later due to secondary sequelae such as secondary cerebral bleeding in the infarct territory, haemodynamic instability or pulmonary complications. Furthermore, patients with stroke might suffer severe neurological impairment, increasing with increasing time to revascularisation, but still survive. This might explain why the association between AMI and distance to hospital was more pronounced in all age groups compared to patients with stroke.
Study limitations
As noted above, the SNC does not contain information on the exact location of a person when he or she had a stroke or heart attack. Since the average ages of all persons dying from stroke and AMI were, respectively, 82 and 78, we assumed that the vast majority of stroke or AMI events occurred at or close to home and reasonably, we believe, we used home to hospital distance in our analyses.
We located SNC participants at a place of residence in the 2000 census, which was also the basis for defining the neighbourhood index of socioeconomic position.21 However, over the years 2001 to 2008, residents could have moved (some surely did) and that information is not available in the SNC data. For those who died, the SNC also has information about the community (but not exact geocode) of the residence at death. Of the 381 659 people who died in our study population, 19 785 (5.2%) did not die in the same community in which they lived at the census 2000 (1089 in stroke cases, 908 in AMI cases).
Information on whether a patient was admitted, to which hospital, was not available. We partially addressed this problem by including the distance to different types of hospitals as patients will be admitted to different specialised hospitals depending on their diagnosis/symptoms.
Catheter laboratories and stroke units provide the best evidence-based treatments for patients with AMI and stroke.1 10 26 It would have been ideal to know the distance to hospitals that have catheter laboratories or stroke units. However, in Switzerland, healthcare is mainly organised at the cantonal level with 26 cantons in charge of healthcare planning and organisation.16 Information on which treatment services are available at each hospital does not exist in a national database, and this includes catheter labs and stroke units operating in the years 2000 to 2008. At the local level, rescue crews are supposed to know which hospitals on which day and hour can receive patients who are in need of specialised AMI or stroke treatments.
Strengths
This study benefits from data that form a true nationwide cohort with almost complete follow-up during the study period for persons 30 years or older at the 2000 census. All Swiss hospitals operating in 2008 were included and classified by type. Owing to Swiss topography, we decided to calculate driving time instead of only using straight-line distance because driving time is a more accurate measure of access in peripheral and rural areas.27 However, in the mountains and other remote regions, emergency medical transportation might be carried out by helicopter. Therefore, we also calculated straight-line distance to model helicopter flight distance. We found that results were comparable to driving time (see online supplementary appendices 14–21).
Comparison with other studies
Several studies have found that AMI and stroke mortality increase with distance to hospital,3 4 28–32 whereas others have not found such an association.33–36
Other outcomes than mortality have also been investigated such as referral to and enrolment in a chronic disease management programme for cardiac rehabilitation which was less likely in patients in Ontario, Canada who lived 60 or more minutes from a cardiac rehabilitation site.37 Therefore, it is important to distinguish healthcare usage from emergency treatment in the association of accessibility of healthcare facilities and outcomes.
When investigating the association of distance to hospital and increased risk of death in patients with life-threatening emergencies, Nicholl et al38 justified the exclusion of out-of-hospital cardiac arrests from their study because survival depends on time from call to treatment by ambulance staff rather than time or distance from scene to hospital. In contrast, Evenson et al39 emphasise that in acute stroke care prehospital delay—the time from onset of symptoms to hospital arrival—contributes the major proportion of delay time. Since the SNC lacks detailed information about circumstances and place of death (eg, death before being reached, death during transport, death in nursing home or hospital), we could not perform sensitivity analyses by excluding prehospital deaths. What we did do, however, was to exclude persons who lived in institutions at the 2000 census from all analyses because treatment decisions for such persons, most of whom are elderly, might differ from those still living at home by, for example, the existence of do not resuscitate orders.
Conclusion
Male and female AMI mortality increased with increasing driving distance to central and university hospitals in the Swiss population both in those under and over 65 years of age, while stroke mortality increased in those aged 65 years and older and not in those younger than 65 years. This association reflects a complex interplay of many factors along the care pathway.
Acknowledgments
This work was supported by the Swiss National Science Foundation (grant number: 138056). In addition, the authors thank the Swiss Federal Statistical Office for providing mortality and census data and for the support which made the Swiss National Cohort and this study possible. The Swiss National Cohort was supported by the Swiss National Science Foundation (grant nos. 3347CO-108806, 33CS30_134273 and 33CS30_148415). The members of the Swiss National Cohort Study Group are Matthias Egger (Chairman of the Executive Board), Adrian Spoerri and Marcel Zwahlen (all Bern), Milo Puhan (Chairman of the Scientific Board), Matthias Bopp (both Zurich), Nino Künzli (Basel), Fred Paccaud (Lausanne) and Michel Oris (Geneva).
Footnotes
Contributors: CB conducted the data processing, the analyses and wrote the first draft of the paper. MZ developed the study design and supervised the statistical analyses. RH provided information regarding the interpretation of the results from the emergency medicine perspective and RP helped conduct the analyses using GIS. All authors critically revised the first draft and approved the final manuscript submitted for publication. The authors thank Christopher Ritter for his editorial assistance.
Funding: This work was supported by the Swiss National Science Foundation (grant numbers to be found on http://p3.snf.ch: 138056, 108806, 134273 and 148415).
Competing interests: None declared.
Ethics approval: Approval for the Swiss National Cohort study was obtained from the Ethics Committees of the Cantons of Zurich and Bern and a data centre was established at ISPM Bern. For this type of study, formal consent is not required.
Provenance and peer review: Not commissioned; externally peer reviewed.
Data sharing statement: Individual data from different data sets were used for the construction of the SNC. All these data are the property of the Swiss Federal Statistical Office (SFSO) and can only be made available by legal agreements with the SFSO. This also applies to derivatives such as the analysis files used for this study. However, after approval of the SNC Scientific Board, a specific SNC module contract with SFSO would allow researchers to receive analysis files for replication of the analysis. Data requests should be sent to Professor Milo Puhan (chairman of the SNC Scientific Board, miloalan.puhan@uzh.ch).
References
- 1.Windecker S, Kolh P, Alfonso F et al. 2014 ESC/EACTS Guidelines on myocardial revascularization: the Task Force on Myocardial Revascularization of the European Society of Cardiology (ESC) and the European Association for Cardio-Thoracic Surgery (EACTS) developed with the special contribution. Eur Heart J 2014;35:2541–619. 10.1093/eurheartj/ehu278 [DOI] [PubMed] [Google Scholar]
- 2.Terkelsen CJ, Sorensen JT, Michael M et al. System delay and mortality among patients with STEMI treated with primary percutaneous coronary intervention. JAMA 2010;304: 763–71. 10.1001/jama.2010.1139 [DOI] [PubMed] [Google Scholar]
- 3.Ferrante M, De Luca G, Fantaci G et al. [Distance from the nearest hospital and mortality for acute miocardial infarction (AMI) in Sicily Region (Southern Italy)]. Epidemiol Prev 2014;38:373–8. http://www.ncbi.nlm.nih.gov/pubmed/25651769 [PubMed] [Google Scholar]
- 4.Balamurugan A, Delongchamp R, Intramuscular L et al. Neighborhood and acute myocardial infarction mortality as related to the driving time to percutaneous coronary intervention-capable hospital. J Am Heart Assoc 2016;5:pii: e002378 10.1161/JAHA.115.002378 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Brokalaki H, Giakoumidakis K, Fotos NV et al. Factors associated with delayed hospital arrival among patients with acute myocardial infarction: a cross-sectional study in Greece. Int Nurs Rev 2011;58:470–6. 10.1111/j.1466-7657.2011.00914.x [DOI] [PubMed] [Google Scholar]
- 6.Postma S, Dambrink JHE, de Boer MJ et al. The influence of residential distance on time to treatment in ST-elevation myocardial infarction patients. Neth Heart J 2014;22:513–9. 10.1007/s12471-014-0599-8 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Sørensen JT, Terkelsen CJ, Nørgaard BL et al. Urban and rural implementation of pre-hospital diagnosis and direct referral for primary percutaneous coronary intervention in patients with acute ST-elevation myocardial infarction. Eur Heart J 2011;32:430–6. 10.1093/eurheartj/ehq437 [DOI] [PubMed] [Google Scholar]
- 8.Navarese EP, De Servi S, Politi A et al. Impact of primary PCI volume on hospital mortality in STEMI patients: does time-to-presentation matter? J Thromb Thrombolysis 2011;32:223–31. 10.1007/s11239-011-0598-1 [DOI] [PubMed] [Google Scholar]
- 9.Giuliani E, Lazzerotti S, Fantini G et al. Acute myocardial infarction—from territory to definitive treatment in an Italian province. J Eval Clin Pract 2010;16:1071–5. 10.1111/j.1365-2753.2009.01254.x [DOI] [PubMed] [Google Scholar]
- 10.European Stroke Organisation (ESO) Executive Committee; ESO Writing Committee. Guidelines for management of ischaemic stroke and transient ischaemic attack 2008. Cerebrovasc Dis 2008;25:457–507. 10.1159/000131083 [DOI] [PubMed] [Google Scholar]
- 11.European Stroke Organisation Executive Committee E. ESO GC Statement on revised guidelines for intravenous thrombolysis 2009. http://www.congrex-switzerland.com/fileadmin/files/2013/eso-stroke/pdf/ESO_Guideline_Update_Jan_2009.pdf
- 12.Powers WJ, Derdeyn CP, Biller J et al. 2015 American Heart Association/American Stroke Association focused update of the 2013 guidelines for the early management of patients with acute ischemic stroke regarding endovascular treatment. Stroke 2015;46:3020–35. 10.1161/STR.0000000000000074 [DOI] [PubMed] [Google Scholar]
- 13.Ogbu UC, Slobbe LCJ, Arah OA et al. Hospital stroke volume and case-fatality revisited. Med Care 2010;48:149–56. 10.1097/MLR.0b013e3181bd4df1 [DOI] [PubMed] [Google Scholar]
- 14.Tung YC, Jeng JS, Chang GM et al. Processes and outcomes of ischemic stroke care: the influence of hospital level of care. Int J Qual Healthcare 2015;27:260–6. 10.1093/intqhc/mzv038 [DOI] [PubMed] [Google Scholar]
- 15.Bekelis K, Marth NJ, Wong K et al. Primary stroke center hospitalization for elderly patients with stroke. JAMA Intern Med 2016;61:379–82. 10.1001/jamainternmed.2016.3919 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Biller-Andorno N, Zeltner T. Individual responsibility and community solidarity—the Swiss Healthcare System. N Engl J Med 2015;373:2193–7. 10.1056/NEJMp1508256 [DOI] [PubMed] [Google Scholar]
- 17.OECD/WHO. OECD reviews of health systems. Switzerland: OECD Publishing, 2011. 10.1787/9789264120914-en [DOI] [Google Scholar]
- 18.Bopp M, Spoerri A, Zwahlen M et al. Cohort profile: the Swiss National Cohort—a longitudinal study of 6.8 million people. Int J Epidemiol 2009;38:379–84. 10.1093/ije/dyn042 [DOI] [PubMed] [Google Scholar]
- 19.Spoerri A, Zwahlen M, Egger M et al. The Swiss National Cohort: a unique database for national and international researchers. Int J Public Health 2010;55:239–42. 10.1007/s00038-010-0160-5 [DOI] [PubMed] [Google Scholar]
- 20.Schmidlin K, Clough-Gorr KM, Spoerri A et al. Impact of unlinked deaths and coding changes on mortality trends in the Swiss National Cohort. BMC Med Inform Decis Mak 2013;13:1 10.1186/1472-6947-13-1 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Panczak R, Galobardes B, Voorpostel M et al. A Swiss neighbourhood index of socioeconomic position: development and association with mortality. J Epidemiol Community Health 2012;66:1129–36. 10.1136/jech-2011-200699 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Steck N, Junker C, Maessen M et al. Suicide assisted by right-to-die associations: a population based cohort study. Int J Epidemiol 2014;43:614–22. 10.1093/ije/dyu010 [DOI] [PubMed] [Google Scholar]
- 23.Spoerri A, Zwahlen M, Bopp M et al. Religion and assisted and non-assisted suicide in Switzerland: National Cohort Study. Int J Epidemiol 2010;39:1486–94. 10.1093/ije/dyq141 [DOI] [PubMed] [Google Scholar]
- 24.Mathisen SM, Dalen I, Larsen JP et al. Long-term mortality and its risk factors in stroke survivors. J Stroke Cerebrovasc Dis 2016;25:635–41. 10.1016/j.jstrokecerebrovasdis.2015.11.039 [DOI] [PubMed] [Google Scholar]
- 25.Hsia RY, Wang E, Saynina O et al. Factors associated with trauma center use for elderly patients with trauma: a statewide analysis, 1999-2008. Arch Surg 2011;146:585–92. 10.1001/archsurg.2010.311 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Roussot A, Cottenet J, Gadreau M et al. The use of national administrative data to describe the spatial distribution of in-hospital mortality following stroke in France, 2008–2011. Int J Health Geogr 2016;15:2 10.1186/s12942-015-0028-2 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Jordan H, Roderick P, Martin D et al. Distance, rurality and the need for care: access to health services in South West England. Int J Health Geogr 2004;3:21 10.1186/1476-072X-3-21 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Murata A, Matsuda S. Association between ambulance distance to hospitals and mortality from acute diseases in Japan: national database analysis. J Public Health Manag Pract 2013;19:E23–8. 10.1097/PHH.0b013e31828b7150 [DOI] [PubMed] [Google Scholar]
- 29.Wei L, Lang CC, Sullivan FM et al. Impact on mortality following first acute myocardial infarction of distance between home and hospital: cohort study. Heart 2008;94:1141–6. 10.1136/hrt.2007.123612 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Busingye D, Pedigo A, Odoi A. Temporal changes in geographic disparities in access to emergency heart attack and stroke care: are we any better today? Spat Spatiotemporal Epidemiol 2011;2:247–63. 10.1016/j.sste.2011.07.010 [DOI] [PubMed] [Google Scholar]
- 31.Magliano DJ, Cohen K, Harding JL et al. Residential distance from major urban areas, diabetes and cardiovascular mortality in Australia. Diabetes Res Clin Pract 2015;109:271–8. 10.1016/j.diabres.2015.05.029 [DOI] [PubMed] [Google Scholar]
- 32.Buchmueller TC, Jacobson M, Wold C. How far to the hospital? The effect of hospital closures on access to care. J Health Econ 2006;25:740–61. 10.1016/j.jhealeco.2005.10.006 [DOI] [PubMed] [Google Scholar]
- 33.Yamashita T, Kunkel SR. The association between heart disease mortality and geographic access to hospitals: county level comparisons in Ohio, USA. Soc Sci Med 2010;70:1211–8. 10.1016/j.socscimed.2009.12.028 [DOI] [PubMed] [Google Scholar]
- 34.Matsui H, Fushimi K, Yasunaga H. Variation in risk-standardized mortality of stroke among hospitals in Japan. PLoS ONE 2015;10:e0139216 10.1371/journal.pone.0139216 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Hsia RY, Kanzaria HK, Srebotnjak T et al. Is emergency department closure resulting in increased distance to the nearest emergency department associated with increased inpatient mortality? Ann Emerg Med 2012;60:707–715.e4. 10.1016/j.annemergmed.2012.08.025 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Alexandrescu R, Bottle A, Jarman B et al. Impact of transfer for angioplasty and distance on AMI in-hospital mortality. Acute Card Care 2012;14:5–12. 10.3109/17482941.2012.655291 [DOI] [PubMed] [Google Scholar]
- 37.Brual J, Gravely-Witte S, Suskin N et al. Drive time to cardiac rehabilitation: at what point does it affect utilization? Int J Health Geogr 2010;9:27 10.1186/1476-072X-9-27 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Nicholl J, West J, Goodacre S et al. The relationship between distance to hospital and patient mortality in emergencies: an observational study. Emerg Med J 2007;24:665–8. 10.1136/emj.2007.047654 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Evenson KR, Foraker RE, Morris DL et al. A comprehensive review of prehospital and in-hospital delay times in acute stroke care. Int J Stroke 2009;4:187–99. 10.1111/j.1747-4949.2009.00276.x [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
bmjopen-2016-013090supp_appendix1.pdf (37.7KB, pdf)
bmjopen-2016-013090supp_appendix2.pdf (38.6KB, pdf)
bmjopen-2016-013090supp_appendix3.pdf (4.4MB, pdf)
bmjopen-2016-013090supp_appendix4.pdf (68.1KB, pdf)
bmjopen-2016-013090supp_appendix5.pdf (68.6KB, pdf)
bmjopen-2016-013090supp_appendix6.pdf (46.1KB, pdf)
bmjopen-2016-013090supp_appendix7.pdf (46.2KB, pdf)
bmjopen-2016-013090supp_appendix8.pdf (46.3KB, pdf)
bmjopen-2016-013090supp_appendix9.pdf (46KB, pdf)
bmjopen-2016-013090supp_appendix10.pdf (46.1KB, pdf)
bmjopen-2016-013090supp_appendix11.pdf (46.1KB, pdf)
bmjopen-2016-013090supp_appendix12.pdf (46KB, pdf)
bmjopen-2016-013090supp_appendix13.pdf (45.8KB, pdf)
bmjopen-2016-013090supp_appendix14.pdf (46.1KB, pdf)
bmjopen-2016-013090supp_appendix15.pdf (46.3KB, pdf)
bmjopen-2016-013090supp_appendix16.pdf (46KB, pdf)
bmjopen-2016-013090supp_appendix17.pdf (46KB, pdf)
bmjopen-2016-013090supp_appendix18.pdf (46.4KB, pdf)
bmjopen-2016-013090supp_appendix19.pdf (46.2KB, pdf)
bmjopen-2016-013090supp_appendix20.pdf (46.2KB, pdf)
bmjopen-2016-013090supp_appendix21.pdf (46.1KB, pdf)