Abstract
We report the case of a patient who, ∼3 weeks after multiple bee stings, developed a prolonged heart block, syncope and cardiac arrest. This required a temporary pacemaker to be implanted, which was later replaced with a permanent pacemaker. An ECG taken following surgery for a fractured humerus 6 years earlier was reportedly normal. The patient had been a rubber tapper who walked ∼1.5 km/day, but after the bee attack he was no longer able to walk or get up from the bed without experiencing syncope. We presume that the bee venom caused these signs, as well as the resulting heart block, which persisted long after the bee sting had subsided. Since his coronary angiogram was normal we believe he had a Kounis type involvement of the cardiovascular system, namely profound coronary spasm that caused complete heart block that did not recover. Another probable reason for the complete heart block could have been that the bees had consumed the pollen of a rhododendron flower, causing ‘grayanotoxin’ poisoning and severe heart block. The other effects of bee sting are discussed briefly.
Background
Bumblebee and honeybee stings cause pain and allergic reactions in susceptible humans. Bee venom can also directly cause adverse reactions.1–6 Here we report the case of a patient who, ∼3 weeks after multiple bee stings, developed a prolonged heart block, syncope and cardiac arrest. This required a temporary pacemaker to be implanted, which was later replaced with a permanent pacemaker. An ECG taken following surgery for a fractured humerus 6 years earlier was reportedly normal. The patient had been a rubber tapper who walked ∼1.5 km/day, but after the bee attack he was no longer able to walk or get up from the bed without experiencing syncope. We presume that the bee venom caused these signs. Until now most of the bee sting mediated heart blocks have been associated with myocardial infarction. This case is of particular importance because earlier accounts of massive bee stings have not reported significant bradycardia. Hence we were unaware of this complication, and hesitated to implant a temporary pacemaker. The patient had almost died, when we saved him in the nick of time by inserting a temporary pacemaker. Hence this report highlights the need for urgent action even in patients after bee sting in order to prevent death, by implanting a temporary pacemaker. This patient presented later without any symptoms of myocardial infarction. We discuss the possibilities below.
Case presentation
A 55-year-old man suffered more than 50 bee stings. A relative reported that the patient was doused with water to stop the bees from stinging him further, and each sting was removed from his body. After the attack, the patient developed facial puffiness, breathlessness and sudden tiredness; the patient then fell down and hit his head, injuring his scalp in the occipital region. He was admitted to Sree Gokulam Medical College where he was given epinephrine, hydrocortisone, dipheneramine maleate, intravenous fluids and tetanus toxoid. The lacerated wound on his scalp was sutured. At that time, his face was still puffy and red, and he had developed bilateral pedal oedema. The following parameters were recorded: total leucocyte (TLC) count 12 500/mm3; polymorphonuclear leucocyte (P) count: 0.90%; lymphocyte (L) count: 10%; platelet count 180 000/mm3; erythrocyte sedimentation rate (ESR) −13 m/hour; haemoglobin (Hb) 14.8 g/dL. A CT scan of brain revealed a left basal ganglion lacunar infarct; he was given aspirin, clopidogrel, and 100 mg injection of hydrocortisone every 8 hours. On improvement of his condition he was discharged with a prescription of oral prednisolone (10 mg once each morning for 5 days).
The patient was then referred to our hospital after two presyncopal episodes during the previous week, the most recent occurring 3 days before he presented to our hospital. Although the patient had a history of acute nephrotic syndrome in his childhood, he had been otherwise asymptomatic until the recent series of episodes of dizziness.
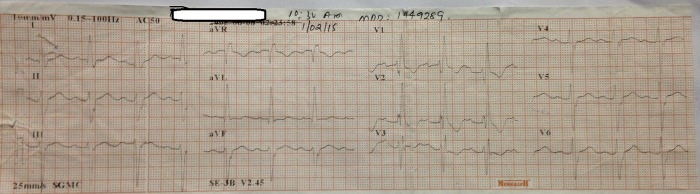
On initial examination, the following parameters were recorded: height 179 cm; weight 79 kg; pulse rate 48 bpm regularly irregular; blood pressure 104/80 mm Hg; jugular venous pressure, normal. He had no obvious cardiomegaly. His S1 heart sound was normal; S2 was widely split but moving with respiration. He had a 2/6 pansystolic murmur in the mitral area. ECG revealed a right bundle branch block (RBBB) with left anterior hemiblock (LAHB), a 3:2 type 2 Mobitz block and a ventricular rate of 50 bpm (figure 1).
Figure 1.
The patient's ECG showing a right bundle branch block (RBBB) with left anterior hemiblock (LAHB); a 3:2 type 2 Mobitz block; ventricular rate of 50 bpm.
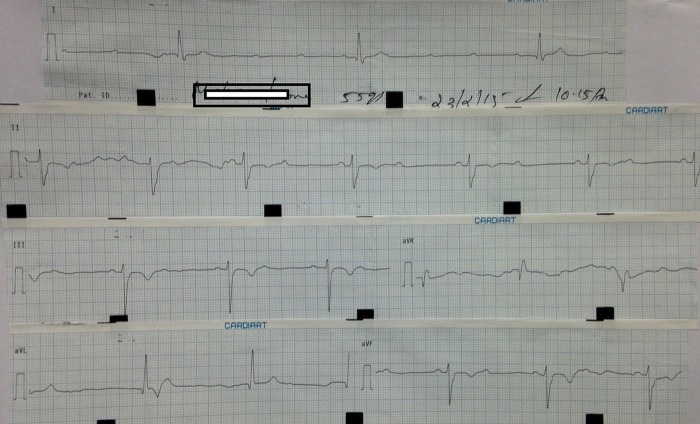
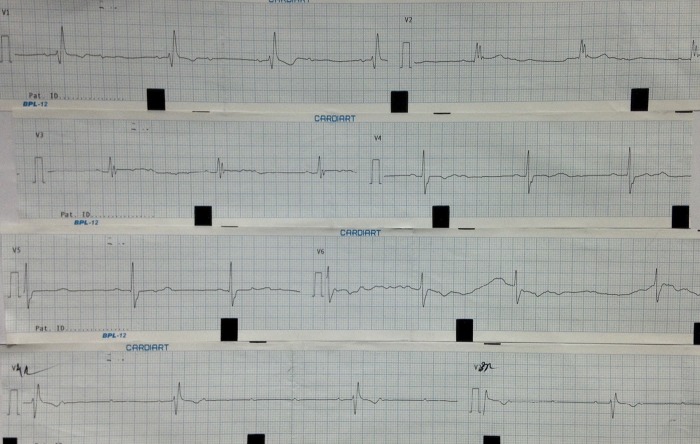
The second ECG showed a ventricular rate of 50 bpm, sinus rhythm with an axis of −50°, PR interval of 200 ms and QRS duration of 120 ms. LAHB with RBBB and partial trifasicular block were present, with occasional complete heart block (figure 2) and (figure 3). The rhythm strip shows a ventricular rate of 27 bpm.
Figure 2.
The patient's second ECG showing a slow heart rate and left axis deviation with varying 2:1 and complete heart block.
Figure 3.
The remaining half of the ECG of the patient showing a ventricular rate of 27 bpm, right bundle branch block and complete heart block.
Patient history before admission
In 2009 the patient had been admitted to a hospital for a fracture of his left humerus. Cardiac evaluation and an ECG carried out at that time were reportedly normal.
Investigations
Other parameters were recorded as follows: troponin T (trop T) 0.02 ng/dL (normal trop T values are 0.01–0.1 ng/dL); fasting blood sugar (FBS) level 86 mg/dL; blood urea −29 mg/dL; TLC 9730/mm3; Hb −13.1 g/dL; P 42%; L 38%; eosinophil count (E) 20; His IGE level was 2500 IU/mL (normal range: 0–100 IU/mL); C3 complement −164 mg/dL (normal range: 90–180 mg/dL); antinuclear antibody (ANA) ratio −0.3; and ANA-ELISA was negative. The patient's lipid profile, serum bilirubin, serum electrolytes, echocardiogram, coronary angiogram, liver function tests and serum protein levels were all normal. His thyroid function was also normal.
Differential diagnosis
The heart block appeared to be directly related to the bee stings as he was reported to be totally asymptomatic prior to this.
So the possibilities:
This was a type 1 Kounis syndrome, where severe coronary spasm of the right coronary artery occurs and causes complete heart block, and no residual myocardial infarction.
This was a late phase reaction to elevated IgE causing immune-mediated heart block due to bee stings.
This was because of the action of tertiapine on the potassium channels in the heart.
This was an apamine-mediated heart block.
It was due to the bees consuming pollen from a Rhododendron plant causing ‘grayanotoxin’ poisoning. (This has not yet been reported after bee stings, all prior reports are due to consuming wild honey or ‘mad honey’.)
We feel the most likely cause of the heart block was Kounis type 1 syndrome where only coronary spasm occurs, and then patients recover. In the literature the coronary angiograms in such cases are reportedly normal like in our case.
Treatment
Despite a regimen of 10 mg orciprenaline and 100 mg deriphylline three times daily, the patient's heart rate fell to 24 bpm and the patient fainted. He was moved to the intensive cardiac care unit (ICCU). Here he experienced one episode of decerebrate rigidity and a short convulsion, so, 8 days after admission and more than 28 days after the bee attack, a temporary pacemaker was implanted. He remained dependent on the pacemaker, which was then replaced with a permanent pacemaker. The patient's condition improved and he was discharged home.
As soon as the patient was admitted to our hospital we conducted an extensive literature search. Until Dr Sanjai gave us the reference as there were no reports of bee stings causing a slow heart rate without myocardial infarction.7 Even the search for the bee venom components did not seem to show any evidence that patients could develop bradycardia (most of the stimulants that can cause bradycardia are norepinephrine, dopamine, melittin, etc). We erred in our judgement and did not put a temporary pacemaker until it was quite late. He had a cardiac arrest and a seizure, when we decided implant a temporary pacemaker. We are apologetic, but we publish this report to prevent similar errors.
Bee stings can cause bradycardia, and need temporary pacing early if persons with bee stings do not recover within a day or two.
Outcome and follow-up
The patient's condition had improved and he was discharged home.
He came for follow-up almost 1-year later.
His latest pacing parameters were:
| 23-6-15, | ||
| AS-VP-81.9% | ||
| Ap-Vp-18.1% | ||
| Threshold | Atrium | Ventricle |
| 0.75 V | 0.7 V | |
| Pulse amplitude | 3.5 V | 3.5 V |
| pulse width | 0.4 ms | 0.4ms |
| P/R wave mV | 4.1 | – |
| Sensitivity | 0.3 mV | 0.9 mV |
| Pace polarity | Bipolar | Bipolar |
| Sense polarity | Bipolar | Bipolar |
| Lead impedance | 741 Ω | 665 Ω |
| Pace average 180 ms | ||
| Sensed average 150 ms | ||
| PVARP—auto | ||
| PVAB 150 ms | ||
| Mode switch—on | ||
| Upper tracking rate 120 bpm | ||
| Upper sensing rate 120 bpm |
AP is the atrial paced; AS is the atrial sensed; PVAB is the postventricular atrial blanking period in miliseconds; PVARP is the postventricular atrial refractory period and VP is the ventricular paced.
He also came for follow-up once again in June 2016. He was in good health. His ECG showed that all beats were AS and VP but we did not preserve the ECG.
Discussion
The present report describes a previously asymptomatic patient in whom it was necessary to implant a permanent pacemaker following multiple bee stings. Bee stings have previously been implicated in myocardial infarction1–3 We believe that the partial trifasicular block observed, which developed into a complete heart block that required pacing, was probably caused by a Kounis type 1 reaction as described below.
A relative of our patient reported that the patient was near a forest area when he was stung by a swarm of Indian rock bees (Apis dorsata, a species of honey bee). It is possible that the bees became aggressive because their territory was being invaded. To the best of our knowledge this is the first case report of its kind—and bee sting fatalities usually occur within 30 min of the attack—tribal people report that this territorial bee species was migrating from its natural forest habitat to abandoned homes.4
Why is this report important?
(a) This is a forewarning of an increased threat of bee aggression, and hence their stings are more potentially fatal to humans. The general physician should have sufficient knowledge of all the possible effects of bee stings, and have access to emergent state-of-the-art care.
(b) The cardiac effects of bee venom have been previously reported
A review by Santhosh et al1 described all cardiac events that have occurred after bee stings. These include myocardial infarction, Kounis syndrome, ventricular fibrillation, acute myocardial infarction with RBBB, myocardial infarction with atrioventricular block, atrial flutter and ventricular ectopics.
The composition of bee venom
Bee venom causes acute pain because it is acidic. The components of bee venom are proteins, polypeptides and low molecular-weight components.5 There are five enzymes in bee venom: phospholipase A2, phospholipase, hyaluronidase, phosphatase and α-glucosidase. The main peptides in bee venom are melittin (40–50% of the dry weight), apamine, MCD peptide, secapine, pamine, minimine, adolapine, procamine A, procamine B, a protease inhibitor, tertiapine, cardiopep and melittin F. Other components of bee venom are phospholipids, three biogenic amines (histamine, dopamine and norepinephrine), amino butyric acid, α amino acid, phosphorus, calcium, magnesium and complex ether pheromones. Different bees have different pheromones. It is believed that if a bee stings or is crushed, the release of pheromones may attract more bees. Therefore, if a person has these chemicals on their skin, they might be stung by another bee or the bees may become more aggressive.
A review by Weisel-Eichler reveals how bee stings might affect human beings.6 The histamine in bee venom causes pain as a line of defence to keep vertebrates away from the bees. Bee venom also induces mast cell release of histamine. This is aided by phospholipase A and melittin, which both cause mast cell lysis and further release of histamine. The norepinephrine and epinephrine in hymenoptera venom cause vasoconstriction and further prolongs the local pain.
Bee and wasp venoms contain dopamine to prevent other insects from entering the hive. Dopamine causes acceleration of encroaching insects' heartbeat and circulation in a similar fashion to the ‘catecholamine storm’ caused by scorpion venom.
A study by Hussein et al7 showed that infusing isolated toad hearts with low doses of bee venom (0.5, 1 or 2 µg/mL) caused an increase in the PR interval and severe bradycardia. The amplitude of the R wave also increased with increasing doses of bee venom. Atrial ectopic and junctional escape beats were also observed with bee venom. The commonest responses to bee venom were first-degree and second-degree heart block. Very high doses of the venom cause cardiac asystole.
It is also possible that the late-occurring bradycardia was a ‘late phase’ reaction caused by elevated levels of IgE. This has been described to last ∼3 to 10 days after bee sting, but bradycardia has not been described. In our patient the IgE levels were elevated.
It is also possible that bradycardia was caused by an apamine-mediated block of Ca2+-activated potassium channels normally described in the central nervous system, though this has not been reported to affect the cardiovascular system yet.
To the best of our knowledge this is the first reported case of a partial trifasicular block occurring after a bee sting, without concomitant myocardial infarction and the first case where an implantation of a permanent pacemaker was required after multiple bee stings.
Bee stings and myocardial infarction
Myocardial infarction is not unknown after a bee sting.3 4 Puvanalingam3 reports a 60-year-old farmer who was stung by multiple bees in the afternoon, and who, by evening, developed acute chest pain. His ECG and echocardiogram revealed an acute inferior wall myocardial infarction. His CPK-MB, troponin T and NT-proBNP levels were elevated. Like our in patient, his coronary angiography was normal. Myocardial infarction may also have been caused either by extreme vasospasm, the extraneous epinephrine administered or anaphylaxis in response to bee venom as mentioned above. Our patient had no evidence of myocardial infarction as assessed by either by echocardiography or by a rise in enzyme levels.
Rhythm disturbances following bee stings
Fisher and Antonios reported a case of atrial flutter after a wasp sting that developed within 10 min of the patient being stung.8
Beestings and heart block
Gangadharan et al9 have described a very dramatic case of complete heart block and myocardial infarction occurring within 60 min of bee sting. The patient described in his presented with rashes and wheezing and hypotension. He underwent primary angioplasty to his right coronary artery, left anterior descending coronary arteries within 20 min. He had been put on an intra-aortic balloon in counter-pulsation mode, and was ventilated. The patient later developed pulmonary embolism and HIT. All these findings were attributed to Kounis syndrome. Our patient had normal coronary arteries. Santosh also describes various cases of heart block with myocardial infarction, but our patient did not develop myocardial infarction (as shown by the enzymes and serial ECGs, not described here).
Wasp stings and heart block
Mukta and colleagues have described a case of myocardial infarction and heart block in a 30-year-old man who was stung by wasps.10 These episodes also occurred just 3 hours after the wasp stings. He had inferior wall myocardial infarction and was thrombolysed with intravenous streptokinase. A later coronary angiogram showed that the coronary arteries were all normal. They have called it an ‘allergic myocardial infarction’. They were unsure whether the angina and myocardial infarction were due to Kounis syndrome. They describe a type 1 Kounis syndrome where the patient develops myocardial infarction due to coronary spasm and the coronary arteries are normal. They also describe a type 2 Kounis syndrome where there is plaque rupture, regional wall motion abnormalities and myocardial infarction occurs due to allergic mechanisms. Surprisingly the right coronary artery is involved in type I Kounis syndrome.
What might have happened in our patient?
So what might have happened in our patient? He might have developed an allergic reaction due to the bee venom, and a type I Kounis syndrome, had an involvement of the right coronary artery that led to complete heart block; the Kounis syndrome might have reverted before the patient reached our hospital, leaving normal coronaries, no myocardial infarction and only persistent heart block at 3 weeks after the bee stings.10
Mass envenomations
Our patient must have had massive envenomation. He was stung by at least 50 bees. Vetter has described the effects of massive envenomation by bees and wasps.11 Most of the deaths described have been due to <10 stings per patient.
There is one more report of myocardial infarction and rhabdomyolysis from Vellore.12 Here a patient with more than 50 beestings, who was stung while picking flowers, came with angioedema of the face 12 hours after being stung. She developed ST elevation in the anterior leads that reverted later. She had elevated cardiac enzymes and troponin T suggestive of myocardial infarction. However, the patient later recovered after treatment with epinephrine, steroids and antihistamines.
Tertiapine
Recently researchers from Pennsylvania have reported that tertiapine in bee venom may cure systemic hypertension.13 Professor of Physiology, Zho Lu, of the School of Medicine, found that tertiapine, a honey bee toxin affects some channels in the kidney. These are potassium channels responsible for the conservation of salt in the human body. Tertiapine affects some Kir channels in the kidney but the heart also has these channels. There are no studies on the effects of tertiapine on the heart channels yet.
c) Bee stings have been implicated in adverse effects on other body systems
Infections
There are reports of septicaemia occurring after bee stings, caused by pathogens entering the human body via the pores when stingers are left in the skin.14
On a recent visit, our patient also had some papular lesions at the sting sites. These were treated with a local antibiotic ointment, but he had no fever.
IgE-mediated anaphylaxis can cause stent thrombosis and lead to myocardial infarction.15
Table 1 summarises the reported effects of bee stings on human body systems.
Table 1.
A review of the recently reported effects of bee stings in all systems
| Effects of bee stings | References |
|---|---|
| Myocardial infarction | 1–3 |
| Bradycardia | This paper |
| Partial trifasicular block | This paper |
| Atrial flutter | 8 |
| Myocardial infarction with both anterior and inferior wall infarction and heart block | 9 |
| Kounis syndrome type 1 | 10 |
| Fatal infection secondary to a bee sting episode | 14 |
| HIT and Kounis syndrome | 15 |
| Subarachnoid haemorrhage | 16 |
| Stroke | 16 |
| Intravascular coagulation | 17 |
| Rash due to bee venom transmitted by breast milk | 18 |
| Rhabdomyolysis | 19 |
| Acute tubular necrosis | 20 |
| Renal failure | 20 |
| Corneal ulcer not affecting vision | 21 |
| Acute polyneuropathy | 22 |
| Acute brachial plexopathy | 23 |
Consuming wild honey ‘Mad Honey’ or is it relevant here?
It has been observed that some bees use the nectar from a rhododendron flower. The honey of these bees contains ‘grayanotoxin’, a natural sodium channel blocker. There are various reports of heart block after consuming this type of honey in humans.24–26 So, since bees that stung our patients were forest bees this could have been the cause of complete heart block in our patient. The bees mentioned in our paper may have sucked nectar from a rhododendron flower’.
“Grayanotoxin is found in the following plants—plants of the Ericaceae family, Rhododendron, Pieris, Agarista and Kalmia. This has been shown to cause hypotension and atrioventricular block.24 The neural Na channels are continuously stimulated (inability to inactive the neural Na channels leads to continuous vagal stimulation that causes bradycardia). Honey containing grayanotoxin is called ‘mad honey’. Generally ingestion of mad honey by humans causes only a temporary heart block vomiting and dizziness. The symptoms usually improve within a few days. Depending on the continent different forms of grayanotoxin are found. Other names for grayanotoxin are andromedotoxin, acetylandromedol or rhodotoxin. Most of the patients affected by various forms of grayanotoxin responded well to an injection of intravenous atropine. Unfortunately we did not try intravenous atropine as we were not aware of this entity as being relevant to multiple bee stings.
Oguzturk et al25 have reported a case of atrioventricular block in a woman who consumed some ‘mad honey’ that had been given to her as a gift.
Another man developed severe bradycardia with just 30 mL of wild honey (oral ingestion).26 Other authors have reviewed the effects of ‘mad honey’ consumption and quoted the findings in 69 cases from 11 studies.27 Around 87% had bradycardia and 100% had hypotension. Four cases had complete heart block and all but one improved with intravenous atropine. One patient needed a temporary pacemaker. However, not even a single patient required a permanent pacemaker implantation.
Rhododendron is the national flower of Nepal. Bees feeding on this produce honey that causes intoxication when consumed.28 However, it is possible these flowers were found in the forests close to the home of our patient and the bees of the region produced contaminated honey and the multiple bee stings caused the bradycardia in our patient (this has not been reported after beestings).
Ozhan et al29 have described wild honey intoxication after ingestion of honey from a single center. They had 4 cases of complete heart block out of 15 cases in their report.
In this series, four patients suddenly collapsed and developed trauma to the head and three had haematomas. The reported heart rate was below 45 bpm in all the cases. All the patients developed bradycardia and hypotension. This report is from Turkey. None of the patients died and all had recovered with only intravenous atropine and intravenous saline treatment.
Prevention of bee stings
Bumblebees sting only when provoked, therefore when working with these bees one should remain calm and avoid provocation.30
When near bees, avoid drinking or smelling of alcohol or perspiration, soap, aftershaves or perfume. Rings, watches and bangles can cause aggressive behaviour in bees because oxidised materials react with the skin and emit a scent. Blue colour provokes bees to sting. This colour should be avoided.
Treatment of bee stings
Dutta and Mukta31 have described ‘Mueller's grading’ of bee sting responses in detail. The patient in our case probably presented to the hospital with a grade 2 reaction to his stings.
Test for IgE levels should be performed in all massive bee sting victims.32
Additionally the sting site should be inspected and any residual sting particles should be removed as they can form a portal for entry of germs and bacteria.32 Mortality from anaphylaxis usually occurs within 30 min and should be treated as an emergency. The local reaction should be treated with ice or cold packs. Antihistamines and epinephrine should be given if the patient has a known allergy to bee stings. If oxygen is available this should be given. Intravenous steroids can be life-saving. Intravenous fluids should be given to prevent shock and hypotension. If patients have respiratory symptoms or distress, they may be ventilated.32
If a patient has bradycardia, a temporary pacemaker should perhaps be implanted. In view of the possibility of ‘mad honey’ intoxication by multiple bites (not yet reported) intravenous atropine should be tried. If the heart block persists, a permanent pacemaker should be implanted.
There are a variety of causes of persistent heart block like sarcoidosis, hypothyroidism and acute rheumatic fever. These should be excluded one by one. Our patient had a normal ESR and no joint pains so we did not think of these at the time he presented to our hospital. He had normal thyroid functions and a normal echocardiogram.
Learning points.
Bee stings can cause long-term effects such as bradycardia, asystole and prolongation of PR interval. These effects may persist long after the effects of stimulants such as norepinephrine and dopamine in the bee venom may gradually ebb away.
When a bee sting victim has hypotension or shock, the physician should explore the possibility of bee venom-induced vasospasm, which can cause myocardial infarction in people with normal coronary arteries.
Given that bee venom can cause cerebral infarcts, all bee sting victims with syncope should have both a CT scan and an ECG.
Kounis syndrome can cause two types of myocardial reactions, type 1 and type 2. Type 1 presents only with coronary spasm, type 2 presents with plaque rupture and myocardial infarction.
If the location of the bee stings are known a search for possible Rhododendron plants in the vicinity should be made. These products can cause ‘mad honey’ intoxication due to bee stings. Thus patients with bradycardia following bee stings may recover with only intravenous atropine.
Acknowledgments
The authors acknowledge the help of Sanjay PV who provided the article on toad hearts.
Footnotes
Contributors: PNG wrote the article, treated the patient. BKK treated the patient. PV performed the permanent pacemaker implantation. SMD retrieved the ECG records and performed the emergency temporary pacemaker implantation. BKK followed up the patient. PNG and PV performed the permanent pacemaker implantation.
Competing interests: None declared.
Patient consent: Obtained.
Provenance and peer review: Not commissioned; externally peer reviewed.
References
- 1.Santhosh M Sr, Viswanathan S, Kumar S. The bee sting related Wolff-Parkinson-White Syndrome. J Clin Diagn Res. 2012;6:1541–3. 10.7860/JCDR/2012/4604.2554 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Bindu CB, Manuprakash SK, Srinivasa BS. Acute myocardial injury in multiple bee stings—a case report. Int J Med Sci Public Health 2013;2:1107–9E. 10.5455/ijmsph.2013.200620132 [DOI] [Google Scholar]
- 3.Puvanalingam A, Karpagam P, Sundar C et al. Myocardial infarction following bee sting. J Assoc Physicians India 2014;62:738–40. [PubMed] [Google Scholar]
- 4.Raman GK. Rock bees taste the bitter fruits of man's greed. The Hindu. http://www.thehindu.com/news/national/kerala/rock-bees-taste-the-bitter-fruits-of-mans-greed/article4574199.ece (accessed 11 Apr 2016).
- 5.Bogdanov S. Bee venom: composition, health, medicine: a review. Bee Product Science. http://www.bee-hexagon.net/files/file/fileE/Health/VenomBookReview.pdf (accessed 11 Apr 16).
- 6.Weisel-Eichler A, Libersat F. Venom effects on monoaminergic systems. J Comp Physiolol A Neuroethol Sens Neural Behav Physiol 2004;190:683–90. [DOI] [PubMed] [Google Scholar]
- 7.Hussein A, Nabil Z, Zalat S et al. Effect of the bumblebee Bombus morrisoni venom on cardiac, skeletal and smooth muscle activity. Egypt J Biology 1999;1:45–56. [Google Scholar]
- 8.Fisher BA, Antonios TF. Atrial flutter following a wasp sting. J Postgrad Med 2003;49:254–5. [PubMed] [Google Scholar]
- 9.Gangadharan V, Bhatheja S, Al Balbissi K. Kounis syndrome—an atopic monster for the heart. Cardiovasc Diagn Ther 2013;3:47–51. 10.3978/j.issn.2223-3652.2013.02.04 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Mukta V, Chandragiri S, Das AK. Allergic myocardial infarction. N Am J Med Sci 2013;5:157–8. 10.4103/1947-2714.10754 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Vetter RS, Visscher PK, Camazine S. Mass envenomations by honey bees and wasps. West J Med 1999;170:223–7. [PMC free article] [PubMed] [Google Scholar]
- 12.Mathew A, Chrispal A, David T. Acute myocardial injury and rhabdomyolysis caused by multiple bee stings. J Assoc Physicians India 2011;59:518–20. [PubMed] [Google Scholar]
- 13.Richards E. Don't Bee Alarmed: That Sting May Cure Hypertension By Erin Richards|September 19th 2008 01:38 PM “ Accessed on 4-5-16 Ramu ,Y ,Xu,Y and Zhe Lu “ Engineered specific and high-affinity inhibitor for a subtype of inward-rectifier K+channels “ PNAS 2008 105:10774-10778; published ahead of print July 31, 2008, doi:10.1073/pnas.0802850105. [Google Scholar]
- 14.Truskinovsky AM, Dick JD, Hutchins GM. Fatal infection after a bee sting. Clin Infect Dis 2001;32:E36–8. 10.1086/318451 [DOI] [PubMed] [Google Scholar]
- 15.Kounis NG. Kounis syndrome: a monster for the atopic patient. Cardiovasc Diagn Ther 2013;3:1–4. 10.3978/j.issn.2223-3652.2013.02.05 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Dikici S, Aydin LY, Saritas A et al. An unusual presentation of bee sting: subarachnoid haemorrhage. Am J Emerg Med 2012;30:1663.e5–6. 10.1016/j.ajem.2011.09.012 [DOI] [PubMed] [Google Scholar]
- 17.Gawlik R, Rymarczyk B, Rogala B. A rare case of intravascular coagulation after honey bee sting. J Invest Allergol Clin Immunol 2004;14:250–2. [PubMed] [Google Scholar]
- 18.Kaya A, Okur M. Bee sting in mother and urticarial rash in her baby. Indian Pediatr 2012;49:499 10.1007/s13312-012-0065-x [DOI] [PubMed] [Google Scholar]
- 19.Akdur O, Can S, Afacan G. Rhabdomyolysis secondary to bee sting. Case Rep Emerg Med 2013;2013:258421 10.1155/2013/258421 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Deshpande PR, Farooq AK, Bairy M et al. Acute renal failure and/or rhabdomyolysis due to multiple bee stings: a retrospective study. N Am J Med Sci 2013;5:235–9. 10.4103/1947-2714.109202 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Yuen KS, Lai JS, Law RW et al. Confocal microscopy in bee sting corneal injury. Eye (Lond) 2003;17:845–7. 10.1038/sj.eye.6700425 [DOI] [PubMed] [Google Scholar]
- 22.Poddar K, Poddar SK, Singh A. Acute polyradiculoneuropathy following honey bee sting. Ann Indian Acad Neurol 2012;15:137–8. 10.4103/0972-2327.95000 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Fan Kee H, Hassan S, Aliaa Ws W. A case report of an unusual complication from bee sting: acute brachial plexopathy. Pak J Med Sci 2014;30:455–6. 10.12669/pjms.302.4891 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Jansen SA, Kleerekooper I, Hofman ZLM et al. Grayanotoxin poisoning: ‘mad honey disease’ and beyond. Cardiovasc Toxicol 2012;12:208–15. 10.1007/s12012-012-9162-2 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Oguzturk H, Ciftci O, Turtay MG et al. Complete atrioventricular block caused by mad honey intoxication. Eur Rev Med Pharmacol Sci 2012;16:1748–50. [PubMed] [Google Scholar]
- 26.Dubey L, Maskey A, Regmi S. Bradycardia and severe hypotension caused by wild honey poisoning. Hellenic J Cardiol 2009;50:426–8. [PubMed] [Google Scholar]
- 27.Gunduz A, Turedi S, Russell RM et al. Clinical review of grayanotoxin/mad honey poisoning, past and present. Clin Toxicol (Phila) 2008;46:437–42. 10.1080/15563650701666306 [DOI] [PubMed] [Google Scholar]
- 28.Rawat B, Rajbhandari S, Bhatta Y et al. Honey Intoxication: a Unique Cause of Sudden Cardiac Collapse. World Academy of Science, Engineering and Technology. International Journal of Medical and Health Sciences 2015:2 Abstract no: International Science Index Vol:2, No:12, 2015 waset.org/abstracts/31998.
- 29.Ozhan H, Akdemir R, Yazici MK et al. Cardiac emergencies caused by honey ingestion: a single centre experience. Emerg Med J 2004;21:742–4. 10.1136/emj.2003.009324 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Koppert Biological Systems. Treatment of bumble bee stings and allergies. https://www.koppert.com/pollination/bumblebee-stings-and-allergies/ (accessed 11 Apr 16).
- 31.Dutta TK, Mukta V. Section 12 Toxicology, Chapter 92: Indian guidelines and protocols: bee sting. In: Muruganathan A, ed. Medicine update, Volume 23. New Delhi, India: Jaypee Brothers, 2013. http://www.apiindia.org/medicine_update_2013/chap92.pdf (11 Apr 2016). [Google Scholar]
- 32.Vankawala HH. Hymenoptera stings: background, pathophysiology, epidemiology. Medscape. http://emedicine.medscape.com/article/768764-overview (accessed 11 Apr 16).