Abstract
Recanalization of chronic occlusion of the common carotid artery (CCA) in patients with a history of neck irradiation is challenging, both for vascular surgeons and interventional neuroradiologists. We describe a case of successful stenting of radio induced chronic occlusion of the right CCA in a 41-year-old patient with neurological deterioration and minor stroke due to cerebral hypoperfusion caused by concomitant bilateral arterial occlusions. Direct surgery and surgical bypass were considered contraindicated. The endovascular approach was successful and required multiple precautions during the procedure. We describe particular solutions, not used in day to day practice, that allowed us to carry out the endovascular treatment in this unusual situation.
Keywords: Intervention, Balloon, Technique, Stent, Stenosis
Background
This case represents an extreme presentation of a well known pathology. We have no knowledge of reported cases in the literature of endovascular treatment in patients with long bilateral common carotid and vertebral occlusion. Large vascular steno-occlusive disease is a major sequela of head and neck radiation due to extensive endothelial damage followed by destruction of the internal elastic lamina and marked thickening of the endothelium. Carotid endarterectomy and surgical bypass are not recommended due to associated scarring of the vessel wall and tissue planes, involvement of the long segment, presence of both intracranial and extracranial stenosis, bilateral occlusion, inadequate wound healing and closure following the procedure, and the high rate of recurrent bypass stenosis.1
Case presentation
A 41-year-old man was admitted with acute onset of postural symptoms with right arm hemiparesis. The patient complained of chronic weakness and lack of appetite with progressive loss of weight. The patient had a history of neck irradiation for an oropharyngeal undifferentiated carcinoma 23 years before with complete healing.
Investigations
Brain MR imaging showed a bilateral linear pattern suggestive of significant hemodynamic impairment of the watershed area between the middle cerebral artery and anterior cerebral artery territory.
Selective diagnostic cerebral angiogram showed: (1) slow antegrade flow into the right internal carotid artery supplied by the external carotid artery re-inhabited from collaterals of the ipsilateral deep cervical artery; (2) inverted flow in the left carotid artery and collateral flow through the posterior communicating arteries bilaterally; (3) occlusion of the right vertebral artery and stenosis of the origin of the left vertebral artery; and (4) arterial flow to the brain supported mainly by the left vertebral artery and by low flow collateral branches to the right internal carotid (figure 1).
Figure 1.
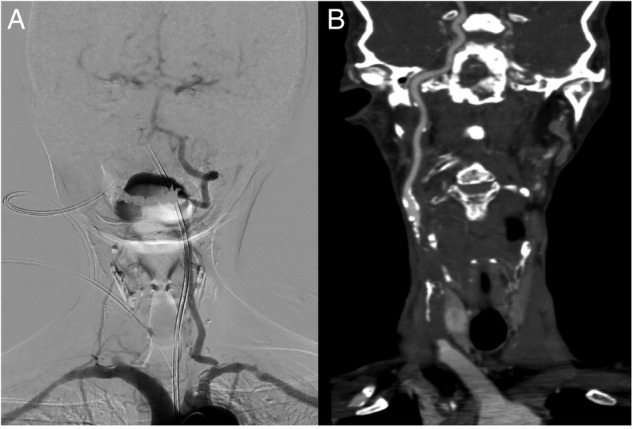
Preoperative DSA (A) and CT angiography (B) demonstrates three vessel chronic occlusion with residual supply by the left vertebral artery.
CT angiography demonstrated bilateral occlusion of the common carotid arteries and occlusion of the right vertebral artery, and 70% stenosis of the origin of the left vertebral artery (figure 1).
Ultrasound and color Doppler examinations of the neck confirmed very low flow in the carotid bulbs bilaterally and in the internal carotids.
Single photon emission CT (SPECT) scanning with 99mTc-ethyl cysteinate dimmer revealed decreased uptake in the cerebral parenchyma, especially in the frontoparietal lobe bilaterally. Carotid surgery was excluded due to the lack of soft tissue of the cervical region; extracranial–intracranial bypass was contraindicated due to highly calcified arterial walls in the neck region and of the superficial temporal artery.
Treatment
Following evaluation of symptoms, clinical status, and imaging studies, we decided that endovascular recanalization was required.
The patient was premedicated with clopidogrel (75 mg) and aspirin (100 mg) 3 days before the procedure. The procedure was performed under general anesthesia. Heparinization was performed during the intervention.
An 8 F guiding catheter (Merci; Stryker, Miami, USA) was placed into the residual limb of the right CCA with a co-assial 4 F catheter. A 0.018 inch guidewire (V-18 ControlWire; Boston Scientific Corporation, Massachusetts, USA) was used to cross the lesion with successive small penetrate and advance steps along the imaginary tract of the occluded vessel segment under roadmapping guidance. The tip of the 0.018 guidewire was advanced distally into the carotid artery.
In order to avoid the subintimal progression of the guidewire while entering the internal carotid at the end of the common carotid, we performed this phase under echographic control. A microcatheter was advanced along the guidewire in the internal carotid. The balloon of the Merci guiding catheter was inflated just at the origin of the common carotid. A 3×150 mm balloon (Savvy Long; Cordis, California, USA) was advanced and inflated to pre-dilate the CCA. The first balloon was exchanged with a 3.5×200 mm balloon (Savvy Long; Cordis) and a second pre-dilation was performed.
After balloon angioplasty, the angiogram showed a well dilated lumen of the CCA with regular flow in the internal carotid and intracranial branches. Two 5×30 mm and two 7×40 mm open cell self-expanding stents (Precise Pro Rx; Cordis) were placed partially overlapped to cover the entire CCA lumen. Post-dilation with a 5×220 mm balloon was then performed (Savvy Long; Cordis). Before the placement of the last stent at the origin of the CCA, we aspirated the lumen contents of the CCA to avoid debris migration. The final angiogram showed patency of the CCA (figure 2), with re-established flow to the brain. DSA two-dimensional perfusion performed at the end of the procedure confirmed the improvement in anterior cerebral parenchyma perfusion (figure 3).
Figure 2.
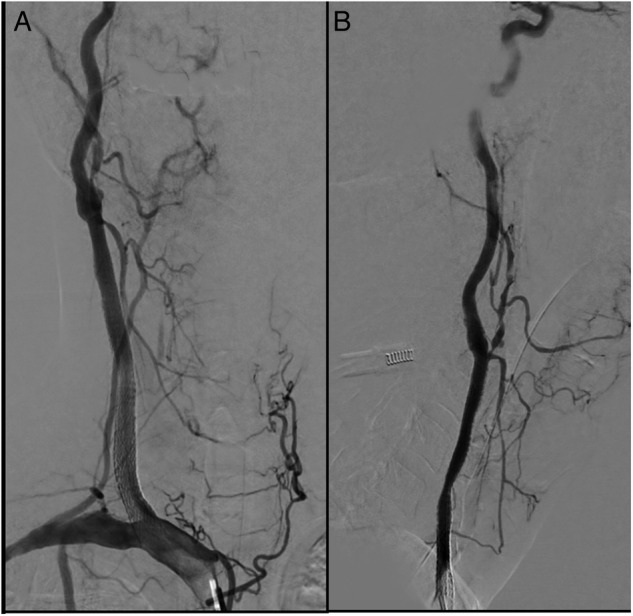
DSA images, anteroposterior (A) and lateral view (B), showed good apposition of the stents and restoration of the patency of the common carotid artery.
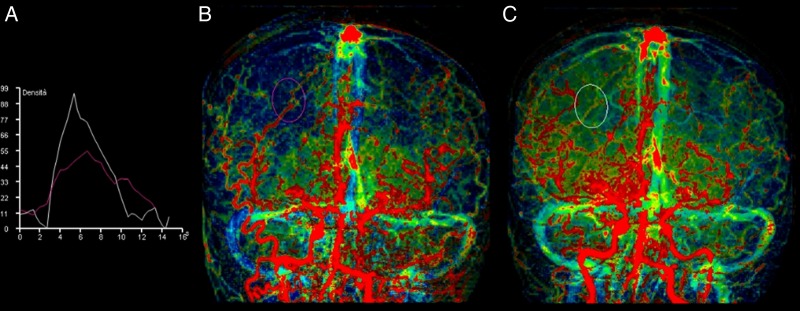
Figure 3.
DSA two-dimensional perfusion images performed with pigtail injection before (B) and after (C) treatment, providing time–density information (A), confirms the improvement (white slope) of hemispheric parenchyma perfusion with reduction in mean transit time from 4.0 to 2.7 s.
Outcome and follow-up
The days after the procedure the patient had a transitory and partial Horner's syndrome. The patient was commenced on aspirin (100 mg/day) indefinitely and clopidogrel (75 mg/day) for 6 weeks.
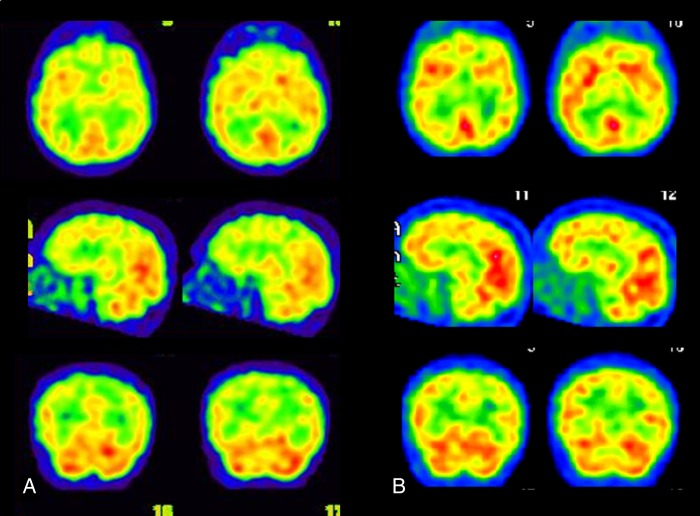
After 6 months, SPECT scanning with 99mTc-ethyl cysteinate dimmer showed a global improvement in cerebral parenchyma perfusion (figure 4). At the 1 year clinical examination, the patient complained of residual slight right arm hemiparesis with restoration of normal daily practice.
Figure 4.
Axial, sagittal, and coronal single photon emission CT images. (A) Preoperative images revealed decreased uptake. (B) Six months after treatment, the images confirmed global improvement in cerebral parenchyma perfusion.
Discussion
Guidelines for the management of patients with carotid stenosis define patients with neck irradiation as high risk for a surgical approach.2
In this type of scenario, the endovascular approach is preferred to surgery and fully indicated. Treatment of this type of patient requires multiple technical precautions to minimize the high risk associated with treatment.
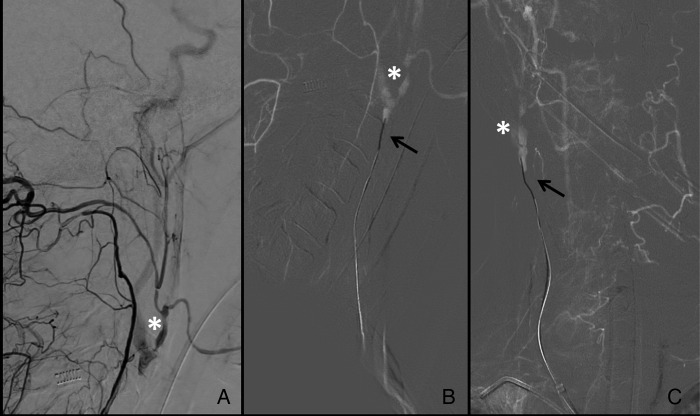
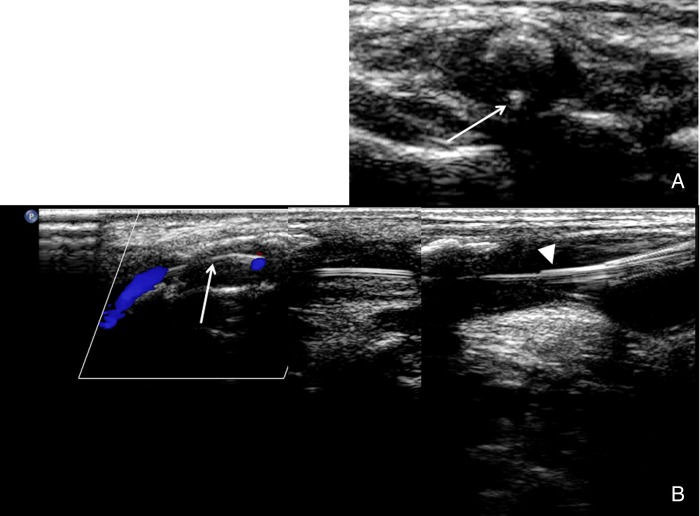
The first major risk is dissection of the carotid artery due to difficulty in catheterizing the true lumen of the vessel. The right CCA offers a safer approach because of its brachiocephalic origin and major stability for the guiding catheter. When crossing the lesion with a microwire, it is essential to be very delicate because of the high risk of damaging the intimal layer and perforating the vessel wall (figure 5). A very useful but uncommon tip is to perform an ultrasound check to visualize the position of the microwire in the true lumen and while entering the patent lumen of the internal carotid3 (figure 6). Possible dissection of the origin of the internal carotid could have caused occlusion of the lonely residual collateral supply to the brain.
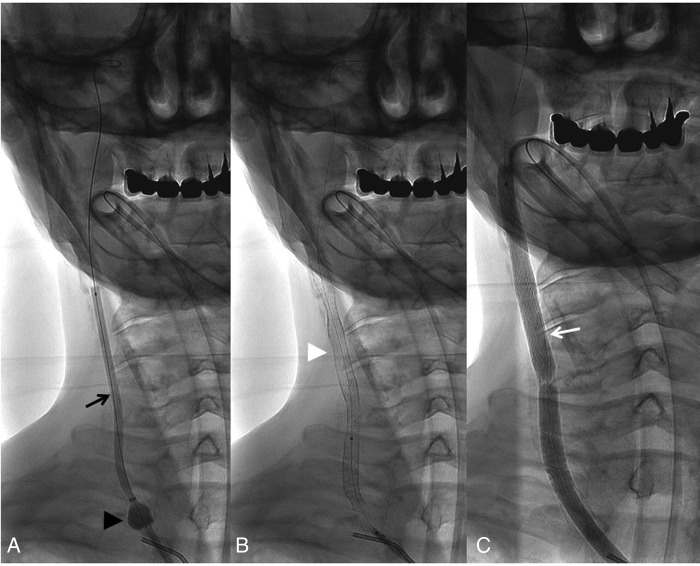
Figure 5.
DSA images. (A) lateral view before treatment, slow antegrade flow into the right internal carotid artery re-inhabited from collaterals of the ipsilateral deep cervical artery (asterisk=carotid bulb). (B, C) lateral view and anteroposterior projections, respectively: the tip of the 0.018 guidewire (black arrow) advanced distally in the right carotid artery.
Figure 6.
Ultrasound check of the catheter (white arrowhead) and the microwire tip (white arrow) in axial (A) and longitudinal (B) images.
Another significant risk is the possibility of an embolic event during the whole procedure but particularly during balloon dilatation. The proximal stop flow technique is a well known technique to avoid thromboembolic dissemination during recanalization of a stenotic carotid artery.4 This technique was preferred to the use of distal protection in order to have more options for catheters and devices during the whole procedure.
A particular and unusual technique in the head–neck area is the use of a unique long dilatation balloon. This technique is normally used in the peripheral endovascular procedure to perform a single inflation. This unusual technique was chosen because it was considered less traumatic to the arterial wall, it avoids multiple passages of different balloons, and homogeneous dilatation of the entire segment is obtained. To our knowledge, there is no description of the use of long balloons during carotid stenting. We find this option safe and extremely efficient (figure 7).
Figure 7.
Endovascular procedure. Pre-dilatation (black arrow) using a 3×150 mm balloon during the balloon stop flow (black arrowhead) technique (A), the conjoined self-expandable stent (white arrowhead) technique (B), and post-dilation with the peripheral 5×220 mm balloon (white arrow) (C).
Finally, in this type of patient a high risk of intra-stent stenosis should be considered. Therefore, closer follow-up, greater control of risk factors, and antiplatelet therapy are required.
Learning points.
In our experience of recanalizing a radio induced long chronic vessel occlusion, the following measures can be useful.
CT angiography to verify the existence of a persistent thrombosed lumen.
Ultrasound check of the microwire tip to verify the position in the lumen before the microcatheter is advanced.
Proximal balloon stop flow technique to avoid embolic dissemination.
Use of a peripheral long balloon to obtain a single homogenous inflation.
Conjoined stent technique to minimize kinking of the vessel after stenting.
Footnotes
Contributors: LN: substantial contributions to the intellectual content, conception and design of the study, and drafting of the manuscript; substantial contributions to the literature review; and critical revision of the manuscript. FC: critical revision of the manuscript for important intellectual content and final approval of the submitted manuscript for which he takes public responsibility for the whole content. GC, FV, and CB: acquisition of the data, and analysis and interpretation of the data. All authors read and approved the final manuscript.
Competing interests: None declared.
Patient consent: Obtained.
Provenance and peer review: Not commissioned; internally peer reviewed.
References
- 1.Hussain MA, Verma S, Gupta N et al. Carotid artery revascularization: what's the best strategy? Circulation 2015;131:2226–31. doi:10.1161/CIRCULATIONAHA.114.013017 [DOI] [PubMed] [Google Scholar]
- 2.Abbott AL, Paraskevas KI, Kakkos SK et al. Systematic review of guidelines for the management of asymptomatic and symptomatic carotid stenosis . Stroke 2015;46:3288–301. doi:10.1161/STROKEAHA.115.003390 [DOI] [PubMed] [Google Scholar]
- 3.Rostambeigi N, Khatri R, Hassan AE et al. Duplex ultrasound assisted endovascular revascularization of chronic internal carotid artery occlusion: technical note. Vasc Interv Neurol 2013;6:42–6. [PMC free article] [PubMed] [Google Scholar]
- 4.Lo CH, Doblas M, Criado EJ. Advantages and indications of transcervical carotid artery stenting with carotid flow reversal. Cardiovasc Surg 2005;46:229–39. [PubMed] [Google Scholar]