Abstract
Background
To evaluate the clinical outcomes after the implantation of a new trifocal diffractive intraocular lens (IOL) combined with Enhanced depth of focus (EDOF) technology.
Methods
The study enrolled 80 eyes of 40 patients who underwent cataract surgery with bilateral implantation of a diffractive trifocal IOL (Reviol Tri-ED) designed with a combination of enhanced depth of focus. Mean age was 52.09 ± 11.32 years (range from 45 to 70 years). Uncorrected distance visual acuity (UDVA), corrected distance visual acuity (CDVA), uncorrected intermediate visual acuity (UIVA), corrected intermediate visual acuity (CIVA), uncorrected near visual acuity (UNVA), corrected near visual acuity (CNVA), keratometry (K), and manifest refraction spherical equivalent (MRSE) were evaluated pre- and postoperatively. The contrast sensitivity, defocus curves, and a questionnaire evaluating individual satisfaction were also estimated.
Results
There was a significant improvement in UDVA, CDVA, UNVA, CNVA, CIVA postoperatively. The defocus curve confirmed good visual acuity also in the intermediate distance. The postoperative MRSE was ranged from −0.75 to 0.75 diopters. Contrast sensitivity also significantly improved postoperatively. The patient satisfaction was high.
Conclusion
The new trifocal EDOF IOL provides visual improvement for far, intermediate, and near distances with a high level of visual quality and patient satisfaction.
Keywords: Enhanced depth of focus, Intraocular lens, Trifocal
Background
Cataract, which is a treatable problem, is the leading cause of vision disorders and blindness all over the world [1]. Although aging is the primary cause of cataract, other factors associated with cataract formation include various diseases, trauma, medications and genetic predisposition. While the prevalence of visually significant cataract is about 2.5% at the age of 40–49 years, it increases with age and reaches to 68% before the age of 80 years [2]. The most frequent application in the surgical treatment of cataract is implantation of monofocal or multifocal intraocular lenses (IOLs) after removal of opacified lenses using phacoemulsification [2].
The use of IOLs aims at providing good and high-quality vision and reducing need for additional optical correction. Additionally, designs of monofocal IOLs allow either near or distance focus. In order to overcome this limitation, multifocal IOLs with refractive, diffractive, and the combination of both optical principles have been developed [3]. Multifocal IOLs can improve uncorrected near visual acuity (UNVA) and uncorrected distance visual acuity (UDVA). Nevertheless, different IOL models provide different levels of improvement for uncorrected intermediate visual acuity (UIVA). Various collateral effects such as halos, glare and loss of contrast sensitivity may be observed with the use of multifocal IOLs [4]. Many domestic and professional tasks including the use of computers require a good intermediate vision. While bifocal lenses cause difficulty in intermediate vision, trifocal lenses provide an increase in intermediate vision without compromising distance and near vision [3]. Trifocal IOL models have recently been introduced and clinical outcomes have been reported in the literature. Technical properties of a new lens (Acriva Reviol Tri-ED), particularly enhanced depth of focus property, seem encouraging; thus, we used it in a group of patients and wish the present the initial results, which may be followed by comparative studies in the future.
The present study aimed to evaluate visual acuities (distance, intermediate and near), refractive changes, contrast sensitivity, defocus curve, and postoperative satisfaction of a new diffractive trifocal IOL (Acriva Reviol Tri-ED).
Subjects and methods
This prospective study comprised of bilateral cataract or presbyopia/pre-presbyopia suitable for refractive lens exchange patients who underwent routine phacoemulcification with diffractive trifocal IOL implantation between the periods of August 2014 and July 2015 at the Haydarpasa Numune Education and Research Hospital, Ophthalmology Clinic, Istanbul, Turkey. Informed consents of the patients were obtained. The study adhered to the tenets of the Declaration of Helsinki and was approved by the local ethics committee. Inclusion criteria were patients with bilateral cataract or presbyopia/pre-presbyopia suitable for refractive lens exchange and seeking for spectacle independence. Exclusion criteria were a history of glaucoma or retinal detachment, corneal disease, regular corneal astigmatism greater 0.75D, irregular corneal astigmatism, abnormal iris, macular degeneration or retinopathy, neurophthalmic disease, history of ocular inflammation and previous ocular surgery.
In the preoperative period, the following evaluations were performed: Distance (6 m, Early Treatment of Diabetic Retinopathy Study [ETDRS]), intermediate (80 cm) and near (40 cm) VA with and without correction, slit lamp examination, applanation tonometry, corneal topography (Sirius 3D, CSO, Italy), dilated fundus examination, optical biometry (IOLMaster version 4.3, Carl Zeiss Meditec AG, Germany) using SRK/T formula. The cataracts were graded using the LOCS III classification by the same examiner after slit-lamp examination [5].
All surgeries were performed by the same experienced surgeon (BTA) using a standard technique of sutureless microcoaxial 1.8–2.2 mm phacoemulsification. All incisions were made at the steep axis of the cornea. A 1.8 mm incision was made and 1.8 mm injector was used. In case of difficulty, the incision was extended up to 2.2 mm. After capsulorhexis creation and phacoemulsification, the IOLs were inserted into the capsular bag using the Acrijet Blue injector (VSY Biotechnology, Amsterdam, Netherlands) through the main incision. Postoperatively, all patients received the same treatment: a combination of an antibiotic and steroid agent.
The tests used in the preoperative period were also performed at the1st, 3rd and 6th months, except contrast sensitivity. Contrast sensitivity was evaluated preoperatively and at month 6, and measurement was performed under photopic (85 candelas [cd]/m2) conditions (CSV-1000, VectorVision, Ohio, USA). For the evaluation of the defocus curve, patients wore the correction providing the distance visual acuity in both eyes and the ETDRS charts were used at a distance of 4 m. Different levels of defocus were introduced in 0.5 D steps from +1.50 D to 4.00 D, and visual acuity values were recorded.
In order to evaluate patient satisfaction, the VFQ-14 (14-item Visual Function Questionnaire) was administered to the patients via e-mail at the postoperative 6th month. VFQ-14 questionnaire was sent via e-mail and patients were asked to respond within one week. Patients that did not respond until the specified deadline were called by phone and reminded about the questionnaire. Finally, all patients responded. To avoid patients being influenced, they answered the questions on their own. The questionnaire consists of 14 questions covering 14 aspects of visual function [6]. Each item was scored between 0 and 4 points, highest total point being 56. The degree of difficulty experienced while performing activities related to vision was assessed as no difficulty (4 points), a little difficulty (3 points), a moderate amount of difficulty (2 points), a great deal of difficulty (1 point), and unable to do the activity (0 point). The average of the points was calculated; higher points indicate a less difficulty in performing activities. In addition, all patients were questioned on spectacle need and photic phenomena during the 6th month visit.
The Acriva Reviol Tri-ED is an IOL with a single piece diffractive trifocal EDOF design (Fig. 1). The characteristics of the IOL is presented on the Table 1.
Fig. 1.
The new model of trifocal diffractive intraocular lens, Acriva Reviol Tri-ED
Table 1.
General IOL parameters [7]
| Parameters | Reviol Tri-ED 611 |
|---|---|
| Material | Hydrophobic surface, acrylic with 25% water content, blue filter |
| Optic size | 6.00 mm |
| Optic design | Active-Diffractive Tri-ED |
| Haptic size | 11.00 mm |
| Haptic Design | Plate Haptic |
| Haptic Angle | 0° |
| Recommended Ac. A Constant | 118.0 |
| Recommended Op. A Constant | Srk-T: 118.3 – SRK-II: 118.5 |
| Diopter Power Range | From 0.0 D to +32.00 D (0.50 D increments) |
| Refractive Index Dry | 20 °C/35 °C 1.509/1.509 ± 0.002 |
| Refractive Index Wet | 20 °C/35 °C 1.462/1.462 ± 0.002 |
| Lightdistribution (far%/intermediate%/near%) | 44/28/28 |
| Transmission Value (%) | 89.1 |
| Chromatic Aberration Control (Abbe number) | 58 |
| PCO prevention | 360° sharp edge |
| Recommended Injector and Cartridge System | Acrijet |
IOL intraocular lens, D diopter, PCO posterior capsule opacification
Product features are defined in manufacturer’s documents [7]. The EDOF feature of the lens provides a different advantage from the other available trifocal IOLs. Trifocal EDOF combination was created by changing height, width, interval and number of the diffractive rings. It’s a semi-apodized active diffractive trifocal structure is designed to reduce unwanted diffraction to increase optical quality with enhanced depth of focus vision. The entire optic dimeter covers 25 diffractive rings. This IOL has a trifocal anterior surface and provides an addition of 3.00 D for near and 1.50 D for intermediate at the IOL plane. Its design allocates 44% of light to distance, 28% to intermediate, and 28% to near for photopic and mesopic light condition; its overall efficiency of global light transmittance is 89.1%. The IOL is fully pupil diameters independent and provides adequate visual performance under all lighting conditions. It has a plate-haptic design with no haptic angulation with all enhanced 360-degree square edge to prevent posterior capsule opacification formation. It has spherical powers of 0.00 D to C32.00 D in 0.50 D increments and is implanted with a single-use injector through 2.2 mm incision.
Statistical analysis
NCSS (Number Cruncher Statistical System) 2007&PASS (Power Analysis and Sample Size) 2008 Statistical Software (Utah, USA) programs were used for statistical analyses. In addition to the descriptive statistics (mean, standard deviation, median, frequency, ratio, minimum, maximum), quantitative data were evaluated also by Friedman Test for intragroup comparison and Wilcoxon signed-rank test for paired comparison of the parameters that were not distributed normally. Categorical variables were compared using chi-square test. The surgically induced astigmatism (SIA) was defined as the vector of change in corneal astigmatism between the preoperative and postoperative period. Corneal astigmatism data, obtained by corneal topography, were transformed into Cartesian (x and y) coordinates and surgically induced astigmatism (SIA) was calculated using a standard vector analysis. After the calculations were finished, the Cartesian coordinates were transformed back to the standard notation for astigmatism (cylinder and meridian). Statistical significance was evaluated at the levels of p < 0.01 and p < 0.05.
Results
The present study included 40 patients who underwent bilateral trifocal IOL implantation. Patient characteristics are summarized in Table 2. The mean nuclear opalescence grade was 3.2 (range 1.2 to 4.1) for the 35 patients operated for cataract.
Table 2.
Patient characteristics
| Parameters | |
|---|---|
| Number of eyes | 80 |
| Right | 40 |
| Left | 40 |
| Gender, male/female | 24/16 |
| Age, years, mean ± SD, (range) | 52.09 ± 11.32 (45–70) |
| Follow-up, months, mean ± SD | 9.2 ± 2.1 |
SD standard deviation
Visual acuity
Visual acuities over time are demonstrated in Table 3 and Fig. 2. Statistically significant difference was determined between preoperative values and postoperative 6th-month values of UDVA, UIVA and UNVA. Uncorrected variables showed significant improvement after surgery as compared to the preoperative values.
Table 3.
LogMar visual acuity changes over time
| Visual acuity | Preoperative | 1 M | 3 M | 6 M | P value* |
|---|---|---|---|---|---|
| UDVA | |||||
| Mean ± SD | 0,72 ± 0,20 | −0,03 ± 0,08 | −0,04 ± 0,08 | −0,04 ± 0,08 | 0.001 |
| Range | 0,4–0,9 | −0,2–0,2 | −0,2–0,2 | −0,2–0,2 | |
| CDVA | |||||
| Mean ± SD | 0,05 ± 0,18 | −0,05 ± 0,05 | −0,05 ± 0,05 | −0,05 ± 0,08 | 0,018 |
| Range | 0,0–0,5 | −0,2–0,2 | −0,2–0,2 | −0,2–0,2 | |
| UNVA | |||||
| Mean ± SD | 0,76 ± 0,16 | 0,22 ± 0,13 | 0,18 ± 0,13 | 0,15 ± 0,12 | 0,001 |
| Range | 0,4–1,4 | −0,1–0,5 | 0,0–0,5 | 0,0–0,5 | |
| CNVA | |||||
| Mean ± SD | 0,28 ± 0,18 | 0,21 ± 0,12 | 0,16 ± 0,11 | 0,13 ± 0,04 | 0,340 |
| Range | 0,0–0,8 | −0,1–0,5 | 0,0–0,3 | 0,0–0,4 | |
| UIVA | |||||
| Mean ± SD | 0,69 ± 0,18 | 0,08 ± 0,12 | 0,10 ± 0,10 | 0,08 ± 0,11 | 0,001 |
| Range | 0,1–1,2 | −0,1–0,5 | −0,1–0,4 | −0,1–0,4 | |
| CIVA | |||||
| Mean ± SD | 0,15 ± 0,2 | 0,06 ± 0,07 | 0,07 ± 0,08 | 0,06 ± 0,10 | 0,120 |
| Range | 0,0–0,5 | −0,1–0,4 | −0,1–0,4 | −0,1–0,4 | |
UDVA uncorrected distance visual acuity, CDVA corrected distance visual
UNVA uncorrected near visual acuity acuity, CNVA corrected near visual acuity
UIVA uncorrected intermediate visual acuity, CIVA corrected intermediate visual acuity, SD standard deviation, M month
*6 month vs. preoperative measurement
Fig. 2.
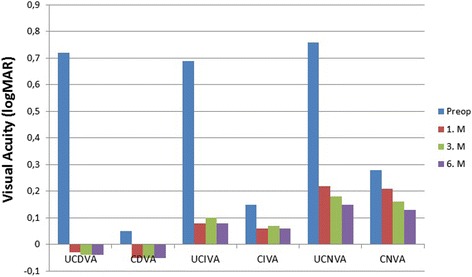
Visual acuity outcomes for distance (6 m), intermediate (80 cm), near (40 cm) distances during the whole period of follow up. (UDVA = uncorrected distance visual acuity; CDVA = corrected distance visual acuity; UIVA = uncorrected intermediate visual acuity; CIVA = corrected intermediate visual acuity; UNVA = uncorrected near visual acuity; CNVA = corrected near visual acuity)
Keratometry
The results of keratometry are demonstrated in Table 4. No significant difference was determined between preoperative values and postoperative 6th-month values in terms of the flattest meridian (Kf), steepest meridian (Ks) and keratometric astigmatism (Ks-Kf). According to vector analysis, the mean surgically induced astigmatism based on keratometry data was −0.23 ± 0.18 D (range, [−0.02]-[−1.00 D]).
Table 4.
Refractive and keratometric changes over time
| Parameters | Preoperative | 1 M | 3 M | 6 M | P value* |
|---|---|---|---|---|---|
| Sphere, D | |||||
| Mean ± SD | 0.40 ± 2.50 | −0.10 ± 0.45 | −0.00 ± 0.20 | −0.02 ± 0.28 | 0.001 |
| Range | −6.00, 3.50 | −0.75, 0.75 | −0.0, 0.50 | −0.75, 0.50 | |
| Cylinder, D | |||||
| Mean ± SD | −0.45 ± 0.36 | 0.35 ± 0.23 | 0.28 ± 0.13 | 0.28 ± 0.12 | 0.02 |
| Range | −0.75, 0.00 | −0.75, 0.0 | 0.50, 0.50 | 0.50, 0.00 | |
| MRSE, D | |||||
| Mean ± SD | 0.70 ± 2.28 | 0.24 ± 0.42 | 0.16 ± 0.35 | 0.12 ± 0.31 | 0.001 |
| Range | −5.50, 3.25 | −0.75, 0.75 | −0.75, 0.50 | −0.75, 0.75 | |
| K2, D | |||||
| Mean ± SD | 43.54 ± 1.52 | 43.46 ± 1.01 | 43.52 ± 1.12 | 43.48 ± 1.35 | 0.618 |
| Range | 40.43, 45.25 | 40.25, 45.48 | 40.21, 44.52 | 40.66, 45.51 | |
| K1, D | |||||
| Mean ± SD | 42.92 ± 1.28 | 42.86 ± 1.12 | 42.90 ± 1.34 | 42.88 ± 1.26 | 0,868 |
| Range | 39.75, 47.50 | 39.75, 45.00 | 39.75, 45.00 | 39.75, 45.00 | |
| K2-K1, D | |||||
| Mean ± SD | 0.62 ± 0.28 | 0.60 ± 0.25 | 0.62 ± 0.38 | 0.60 ± 0.38 | 0.612 |
| Range | −0.18, 0.14 | −0.15, 1.22 | −0.09, 1.15 | −0.05, 1.24 | |
MRSE manifest refraction spherical equivalent, D diopter, K1 flat keratometry reading, K2 steep keratometry reading, M month, K2-K1 corneal cylinder, SD standard deviation
*6 month vs. preoperative measurement
Refraction
Refractive changes of the patients over time are demonstrated in Table 4. Significant decrease was determined in the spherical and spherical equivalent values.
Contrast sensitivity
The results of contrast sensitivity over time at 4 different spatial frequencies are depicted in Fig. 3. From 1 month to 6 months postoperatively, there was a slight but significant improvement in contrast sensitivity at 3 cpd (spatial frequency). The mean contrast sensitivity changed from 1.78 ± 0.20 log units to 1.83 ± 0.11 log units (p = 0.023). There was no significant improvement in contrast sensitivity at 6 cpd, 12 cpd, and 18 cpd between 1 month and 6 months postoperatively.
Fig. 3.
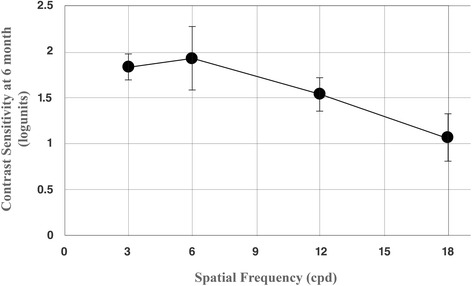
Mean contrast sensitivity outcomes under photopic conditions 6 months after the surgery with different spatial frequencies (cpd = cycles per degree)
Defocus curve
The mean visual acuities and their standard deviations for different defocus values are demonstrated in Fig. 4. In the present study, defocus curve obtained by trifocal IOL showed a tendency of flattening different from the typical M-shape observed by bifocal IOL. VA was preserved particularly in intermediate distances.
Fig. 4.

Defocus curve of Acriva Reviol Tri-ED intraocular lens
Patient satisfaction
The results of the questionnaire applied at the postoperative 6th month are summarized in Table 5. More than 90% of the patients reported no difficulty in performing the daily activities related to vision. The average total score (sum of all questions) was 54.6, 55.1, and 51.0 over maximum score of 56 for the whole study group (n = 40), patients operated for cataract (n = 35), and patients operated for presbyopia/pre-presbyopia (n = 5), respectively. When item-based responses are considered, 95% (464/490) of total questions were scored 4 (no difficulty) in the cataract group, whereas the corresponding figure was 74% (52/70) in the presbyopia/pre-presbyopia group (p < 0.001), indicating higher satisfaction in cataract patients. In addition, none of the patients complained of photic phenomena and were all spectacle-free at the 6th month visit.
Table 5.
The results of VFQ-14 Questionnaire performed to assess the patient satisfaction regarding the activities related to vision at the postoperative 6th month
| Questions | Score | No difficulty | A little of difficulty | Moderate amount of difficulty | A great deal of difficulty | Unable to do |
|---|---|---|---|---|---|---|
| Mean ± SD | n (%) | n (%) | n (%) | n (%) | n (%) | |
| Reading small print | 3.85 ± 042 | 35 (87.5) | 4 (10.0) | 1 (2.5) | 0 (0.0) | 0 (0.0) |
| Reading normal newsprint | 3.95 ± 0.22 | 38 (95.0) | 2 (5.0) | 0 (0.0) | 0 (0.0) | 0 (0.0) |
| Reading large newsprint | 3.97 ± 0.15 | 39 (97.5) | 1 (2.5) | 0 (0.0) | 0 (0.0) | 0 (0.0) |
| Recognizing faces at a distance | 3.85 ± 0.48 | 36 (90.0) | 2 (5.0) | 2 (5.0) | 0 (0.0) | 0 (0.0) |
| Going downstairs | 3.97 ± 0.15 | 39 (97.5) | 1 (2.5) | 0 (0.0) | 0 (0.0) | 0 (0.0) |
| Reading street signs | 3.95 ± 0.22 | 38 (95.0) | 2 (5.0) | 0 (0.0) | 0 (0.0) | 0 (0.0) |
| Sewing, doing delicate manual work | 3.80 ± 0.51 | 34 (85.0) | 4 (10.0) | 2 (5.0) | 0 (0.0) | 0 (0.0) |
| Reading mail, bills accurately | 3.90 ± 0.37 | 37 (92.5) | 2 (5.0) | 1 (2.5) | 0 (0.0) | 0 (0.0) |
| Playing cards | 3.95 ± 0.22 | 38 (95.0) | 2 (5.0) | 0 (0.0) | 0 (0.0) | 0 (0.0) |
| Going out to movies, plays, sporting events | 3.95 ± 0.22 | 38 (95.0) | 2 (5.0) | 0 (0.0) | 0 (0.0) | 0 (0.0) |
| Cooking | 3.90 ± 0.30 | 36 (90.0) | 4 (10.0) | 0 (0.0) | 0 (0.0) | 0 (0.0) |
| Watching television | 3.95 ± 0.22 | 38 (95.0) | 2 (5.0) | 0 (0.0) | 0 (0.0) | 0 (0.0) |
| Driving on day | 3.87 ± 0.40 | 36 (90.0) | 3 (7.5) | 1 (2.5) | 0 (0.0) | 0 (0.0) |
| Driving at night | 3.75 ± 0.66 | 34 (85.0) | 3 (7.5) | 2 (5.0) | 1 (2.5) | 0 (0.0) |
SD standard deviation
(no difficulty - 4 points; a little of difficulty - 3 points; moderate amount of difficulty – 2 points; a great deal of difficulty - 1 point; unable to do - 0)
Complications
No serious complication (iridodialysis, posterior capsule perforation, etc.) occurred during the surgery; refractive surprise, postoperative macular edema and posterior capsule opacity (PCO) were encountered during follow-up period.
Discussion
Recently, it is possible to obtain more successful outcomes in the treatment of patients with cataract with the developments in phacoemulsification techniques and IOL technology. Providing high-quality VA and best levels of spectacle independence for near, intermediate and distance vision has been the primary aim after multifocal IOL implantation [8, 9]. With the use of bifocal IOL implantation, successful outcomes have been obtained in distance and near vision along with increased quality of life and patient satisfaction; however, intended level of improvement could not be achieved in intermediate VA or different outcomes have been obtained depending on characteristics of lens or on patient selection [10–19]. In addition, some of the patients having bifocal IOL implantation complain about certain functional disorders such as haloes or rings around lights, glare and photopsia [20, 21].
Trifocal IOLs, which have three focal spots, have been introduced into use to overcome the problems experienced with bifocal lenses. It has been reported that the use of trifocal IOLs significantly improves intermediate VA without impairing near and distance vision [22, 23]. This also enhances patient satisfaction with its favorable effects on quality of life [22, 23].
Studies conducted on different commercial models of trifocal IOLs have reported good distance, intermediate and near VAs. In their study, Carballo-Alvarez et al. [24] performed FineVision trifocal IOL implantation in 44 eyes of 22 patients with cataract and reported that a full range of adequate vision was achieved, contrast sensitivity was satisfactory, and there were no significant adverse photic phenomena after implantation. Sheppard et al. [25] obtained good distance VA and near and intermediate visual function with the use of FineVision trifocal IOL. In the patients (54 eyes of 27 patients) who underwent AT LISA trifocal IOL implantation following phacoemulsification, Kohnen et al. [26] reported good distance, intermediate and near VAs (0.10 logMAR or better), a high patient satisfaction, and a high spectacle independence at the postoperative 3rd month. Kretz et al. [27] reported significant improvements in UDVA, UIVA, UNVA, and CDVA and better binocular outcomes as compared with monocular outcomes in 100 eyes of 50 patients who underwent AT LISA IOL implantation following cataract surgery.
In the present study, Acriva Reviol Tri-ED IOL was implanted in 80 eyes of 40 patients. The UDVA, UIVA and UNVA logMAR values were determined as 0.72 ± 0.20, 0.69 ± 0.18 and 0.76 ± 0.16, respectively, in the preoperative period and as −0.04 ± 0.08, 0.08 ± 0.11 and 0.15 ± 0.12, respectively, at the postoperative 6th month. These improvements in distance, intermediate and near VAs were found to be significant (p = 0.001 for each). The preoperative spherical equivalent refraction was 0.70 ± 2.28 D and a significant decrease to a value of 0.12 ± 0.31 D occurred at the postoperative 6th month. These results suggested that the trifocal IOL used in the present study was very effective. In their study, Vryghem and Heireman [28] implanted FineVision trifocal IOL in 50 eyes of 25 patients and reported binocular UDVA, UIVA and UNVA to be −0.04 ± 0.09, −010 ± 0.15 and 0.02 ± 0.06 logMAR, respectively, at the postoperative 6th month. In their study performed on 94 eyes of 47 patients, Cochener et al. [29] reported binocular UDVA, UIVA and UNVA as 0.02 ± 0.09, 005 ± 0.08 and 0.00 ± 0.04 logMAR, respectively at the 6th month following FineVision trifocal IOL implantation. Jonker et al. [30] compared the Finevision Micro F trifocal IOL with the Acrysof Restor IQ C3.0 D bifocal IOL in their randomized prospective study and indicated that better defocus curve was obtained by trifocal IOL in the intermediate distance. They also reported that the mean binocular UDVA, UIVA, and UNVA were 0.01 ± 0.11 logMAR, 0.32 ± 0.15 logMAR, and 0.15 ± 0.13 logMAR, respectively, in the patients implanted with trifocal IOL (30 eyes of 15 patients) at the postoperative 6th month. Kretz et al. [31] reported a binocular UDVA of 0.00 logMAR or better and a binocular UIVA of 0.10 logMAR or better in all patients undergoing AT LISA trifocal IOL implantation (76 eyes of 38 patients), and a binocular UNVA of 0.10 logMAR or better in 85% of the patients at the postoperative 3 months. Mojzis et al. [32] conducted a study in the patients (120 eyes of 60 patients) who underwent cataract surgery with trifocal AT LISA IOL implantation; and followed the patients for a postoperative period of 12- month. They reported that a complete and stable visual restoration and good levels of visual quality were achieved with the use of trifocal IOL during the follow-up period.
In the present study, acceptable changes were observed postoperatively in the keratometric parameters as compared with the preoperative period. This finding was consistent with the results of other studies performed with trifocal IOLs [22, 27]. It seems that steep meridian incision may not have clinically relevant flattening effects and small incision size may account for this outcome.
In the present study, the best levels of contrast sensitivity were achieved at lower (3 cpd) spatial frequencies. Likewise, Vryghem and Heireman [28] and Kretz et al. [31] also achieved the highest level of contrast sensitivity at 3 cpd. In the studies conducted by Mojzis et al. [22] and Sheppard et al. [25], the contrast sensitivity curve revealed that the patients had high sensitivity to medium (6 cpd) spatial frequencies. However, in this study, no change was observed at other spatial frequencies. Probably absence of a negative change at 6, 12 and 18 cpd may also be interpreted as clinically relevant, possibly indicating the absence of posterior capsular opacification.
In the present study, evaluation of the defocus curve obtained at the postoperative 6th month revealed that intermediate VA was also effectively improved in addition to near and distance VAs. According to the results of the questionnaire performed during the follow-up period, most of the patients had no difficulty in performing many activities related to vision and thus were satisfied with the results.
We believe that the outcomes we achieved support the idea that EDOF elements can be valuable option to be used as IOLs to restore the imaging ability of the pseudophakic eyes. Using this new design concept of IOLs promises an expanded depth of field without the drawbacks associated with a multifocal visual system. All our patients achieved spectacle independence without an incidence of photic phenomena, such as halos and glare at 6 month-follow up.
Several EDOF-related technical features of Reviol Tri-ED seem to provide some potential advantages: i) real trifocal structure at both center and periphery in contrast to other available trifocal IOLs (e.g. Finevision is a combination of two bifocal patterns and ATLisa has trifocal structure at the center but bifocal at the outer zone); ii) high modular transfer function (MTF) values for transitions, aiding seamless continuous vision; iii) the amount of light reaching retina is high and the ratios of light distributed to far, near and intermediate sights are similar resulting in better light utilization (other IOLs send more light for far vision); iv) intermediate and near sight additions are different thus potentially providing better intermediate sight (80 cm); v) pupil-independent due to semi-apodization feature; vi) higher Abbe value than other IOLs thus providing better chromatic aberration control to prevent halo glare [33], vii) diffractive surface transitions zones are smooth, possibly preventing halo-glare and low contrast sensitivity. However, although these features and findings of this study are encouraging, further comparative studies with other trifocal IOLs are warranted to examine whether these characteristics translate into better clinical outcomes.
The limitations of our study are small number of eyes included, also a reading speed is an important indicator of near visual performance which was not estimated in the current study. This might be also a limitation in terms of assessing the functional vision.
Conclusions
Acriva Reviol Tri-ED used in the present study, a novel trifocal IOL, appears to be a new option in overcoming the problems experienced with bifocal lenses owing to its maximum light energy transmission, and tolerability. It is able to provide an effective distance, intermediate, and near visual acuities after cataract surgery, with high level of visual improvement, and patient satisfaction.
Acknowledgements
None.
Funding
This study was not funded.
Availability of data and materials
Dataset supporting the findings of this study is available upon request from Banu Tırun Acar, MD (e-mail: torunbanu@yahoo.com).
Authors’ contributions
All authors contributed to the conception and design of the work. BTA collected and analyzed data, ED and SS contributed to the interpretation of data. BTA wrote the first draft of the manuscript; ED and SS reviewed and revised the manuscript. All authors have read and approve the final version of the manuscript.
Competing interests
The authors declare that they have no competing interests.
Consent for publication
Not applicable.
Ethics approval and consent to participate
This study adhered to the tenets of the Helsinki Declaration and was approved by the Ethics Committee for Clinical Studies of Haydarpasa Numune Research and Training Hospital (no: HNEAH KAEK 2015/KK/104). Written informed consent was obtained from all subjects prior to study entry.
Presentation
A part of this study was presented at XXXIII. Congress of the European Society of Cataract and Refractive Surgeons, September 5–9, Barcelona, Spain as a poster presentation.
Authors’ financial or proprietary interest
None of the authors has a financial or proprietary interest in any of the products, methods, or materials used in the study.
Sources of public and private financial support
There was no public or private financial support.
References
- 1.Bourne RR, Stevens GA, White RA, Smith JL, Flaxman SR, Price H, Jonas JB, Keeffe J, Leasher J, Naidoo K, Pesudovs K, Resnikoff S, Taylor HR, Vision Loss Expert Group Causes of vision loss worldwide, 1990–2010: a systematic analysis. Lancet Glob Health. 2013;1:e339-49. doi: 10.1016/S2214-109X(13)70113-X. [DOI] [PubMed] [Google Scholar]
- 2.Thompson J, Lakhani N. Cataracts. Prim Care. 2015;42:409–23. doi: 10.1016/j.pop.2015.05.012. [DOI] [PubMed] [Google Scholar]
- 3.Agresta B, Knorz MC, Kohnen T, Donatti C, Jackson D. Distance and near visual acuity improvement after implantation of multifocal intraocular lenses in cataract patients with presbyopia: a systematic review. J Refract Surg. 2012;28:426–35. doi: 10.3928/1081597X-20120518-06. [DOI] [PubMed] [Google Scholar]
- 4.Steinert RF. Visual outcomes with multifocal intraocular lenses. Curr Opin Ophthalmol. 2000;11:12–21. doi: 10.1097/00055735-200002000-00004. [DOI] [PubMed] [Google Scholar]
- 5.Chylack LT, Jr, Wolfe JK, Singer DM, Leske MC, Bullimore MA, Bailey IL, Friend J, McCarthy D, Wu SY. The Lens Opacities Classification System III. The Longitudinal Study of Cataract Study Group. Arch Ophthalmol. 1993;111:831–6. doi: 10.1001/archopht.1993.01090060119035. [DOI] [PubMed] [Google Scholar]
- 6.Steinberg EP, Tielsch JM, Schein OD, Javitt JC, Sharkey P, Cassard SD, Legro MW, Diener-West M, Bass EB, Damiano AM, et al. The VF-14. An index of functional impairment in patients with cataract. Arch Ophthalmol. 1994;112:630–8. doi: 10.1001/archopht.1994.01090170074026. [DOI] [PubMed] [Google Scholar]
- 7.Acriva Reviol Tri-ED IOL Product Brochure: VSY Biotechnology; Available from: http://www.vsybiotechnology.com/media/2016/08/Reviol_Tri-ED.pdf?v = 0.0.1. Cited 25 Aug 2016.
- 8.Lichtinger A, Rootman DS. Intraocular lenses for presbyopia correction: past, present, and future. Curr Opin Ophthalmol. 2012;23:40–6. doi: 10.1097/ICU.0b013e32834cd5be. [DOI] [PubMed] [Google Scholar]
- 9.Liu JW, Haw WW. Optimizing outcomes of multifocal intraocular lenses. Curr Opin Ophthalmol. 2014;25:44–8. doi: 10.1097/ICU.0000000000000012. [DOI] [PubMed] [Google Scholar]
- 10.Bellucci R. Multifocal intraocular lenses. Curr Opin Ophthalmol. 2005;16:33–7. doi: 10.1097/00055735-200502000-00006. [DOI] [PubMed] [Google Scholar]
- 11.Cillino S, Casuccio A, Di Pace F, Morreale R, Pillitteri F, Cillino G, Lodato G. One-year outcomes with new-generation multifocal intraocular lenses. Ophthalmology. 2008;115:1508–16. doi: 10.1016/j.ophtha.2008.04.017. [DOI] [PubMed] [Google Scholar]
- 12.Alio JL, Pinero DP, Plaza-Puche AB, Chan MJ. Visual outcomes and optical performance of a monofocal intraocular lens and a new-generation multifocal intraocular lens. J Cataract Refract Surg. 2011;37:241–50. doi: 10.1016/j.jcrs.2010.08.043. [DOI] [PubMed] [Google Scholar]
- 13.Alio JL, Plaza-Puche AB, Pinero DP, Amparo F, Jimenez R, Rodriguez-Prats JL, Javaloy J, Pongo V. Optical analysis, reading performance, and quality-of-life evaluation after implantation of a diffractive multifocal intraocular lens. J Cataract Refract Surg. 2011;37:27–37. doi: 10.1016/j.jcrs.2010.07.035. [DOI] [PubMed] [Google Scholar]
- 14.Ang R, Martinez G, Cruz E, Tiongson A, Dela CA. Prospective evaluation of visual outcomes with three presbyopia-correcting intraocular lenses following cataract surgery. Clin Ophthalmol. 2013;7:1811–23. doi: 10.2147/OPTH.S49848. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Gundersen KG, Potvin R. Comparative visual performance with monofocal and multifocal intraocular lenses. Clin Ophthalmol. 2013;7:1979–85. doi: 10.2147/OPTH.S52922. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Braga-Mele R, Chang D, Dewey S, Foster G, Henderson BA, Hill W, Hoffman R, Little B, Mamalis N, Oetting T, Serafano D, Talley-Rostov A, Vasavada A, Yoo S, Committee ACC. Multifocal intraocular lenses: relative indications and contraindications for implantation. J Cataract Refract Surg. 2014;40:313–22. doi: 10.1016/j.jcrs.2013.12.011. [DOI] [PubMed] [Google Scholar]
- 17.Kretz FT, Gerl M, Gerl R, Muller M, Auffarth GU, Group ZKBS. Clinical evaluation of a new pupil independent diffractive multifocal intraocular lens with a +2.75 D near addition: a European multicentre study. Br J Ophthalmol. 2015;99:1655–9. doi: 10.1136/bjophthalmol-2015-306811. [DOI] [PubMed] [Google Scholar]
- 18.Shah S, Peris-Martinez C, Reinhard T, Vinciguerra P. Visual Outcomes After Cataract Surgery: Multifocal Versus Monofocal Intraocular Lenses. J Refract Surg. 2015;31:658–66. doi: 10.3928/1081597X-20150611-01. [DOI] [PubMed] [Google Scholar]
- 19.Wang M, Corpuz CC, Fujiwara M, Tomita M. Visual and optical performances of multifocal intraocular lenses with three different near additions: 6-month follow-up. Open Ophthalmol J. 2015;9:1–7. doi: 10.2174/1874364101509010001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Calladine D, Evans JR, Shah S, Leyland M. Multifocal versus monofocal intraocular lenses after cataract extraction. Sao Paulo Med J. 2015;133:68. doi: 10.1590/1516-3180.20151331T2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Maurino V, Allan BD, Rubin GS, Bunce C, Xing W, Findl O, Moorfields IOLSG. Quality of vision after bilateral multifocal intraocular lens implantation: a randomized trial--AT LISA 809 M versus AcrySof ReSTOR SN6AD1. Ophthalmology. 2015;122:700–10. doi: 10.1016/j.ophtha.2014.10.002. [DOI] [PubMed] [Google Scholar]
- 22.Mojzis P, Pena-Garcia P, Liehneova I, Ziak P, Alio JL. Outcomes of a new diffractive trifocal intraocular lens. J Cataract Refract Surg. 2014;40:60–9. doi: 10.1016/j.jcrs.2013.06.025. [DOI] [PubMed] [Google Scholar]
- 23.Voskresenskaya A, Pozdeyeva N, Pashtaev N, Batkov Y, Treushnicov V, Cherednik V. Initial results of trifocal diffractive IOL implantation. Graefes Arch Clin Exp Ophthalmol. 2010;248:1299–306. doi: 10.1007/s00417-010-1424-8. [DOI] [PubMed] [Google Scholar]
- 24.Carballo-Alvarez J, Vazquez-Molini JM, Sanz-Fernandez JC, Garcia-Bella J, Polo V, Garcia-Feijoo J, Martinez-de-la-Casa JM. Visual outcomes after bilateral trifocal diffractive intraocular lens implantation. BMC Ophthalmol. 2015;15:26. doi: 10.1186/s12886-015-0012-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Sheppard AL, Shah S, Bhatt U, Bhogal G, Wolffsohn JS. Visual outcomes and subjective experience after bilateral implantation of a new diffractive trifocal intraocular lens. J Cataract Refract Surg. 2013;39:343–9. doi: 10.1016/j.jcrs.2012.09.017. [DOI] [PubMed] [Google Scholar]
- 26.Kohnen T, Titke C, Bohm M. Trifocal Intraocular Lens Implantation to Treat Visual Demands in Various Distances Following Lens Removal. Am J Ophthalmol. 2016;161:71–7. doi: 10.1016/j.ajo.2015.09.030. [DOI] [PubMed] [Google Scholar]
- 27.Kretz FT, Muller M, Gerl M, Gerl RH, Auffarth GU. Binocular function to increase visual outcome in patients implanted with a diffractive trifocal intraocular lens. BMC Ophthalmol. 2015;15:110. doi: 10.1186/s12886-015-0089-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Vryghem JC, Heireman S. Visual performance after the implantation of a new trifocal intraocular lens. Clin Ophthalmol. 2013;7:1957–65. doi: 10.2147/OPTH.S44415. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Cochener B, Vryghem J, Rozot P, Lesieur G, Heireman S, Blanckaert JA, Van Acker E, Ghekiere S. Visual and refractive outcomes after implantation of a fully diffractive trifocal lens. Clin Ophthalmol. 2012;6:1421–7. doi: 10.2147/OPTH.S32343. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Jonker SM, Bauer NJ, Makhotkina NY, Berendschot TT, van den Biggelaar FJ, Nuijts RM. Comparison of a trifocal intraocular lens with a +3.0 D bifocal IOL: results of a prospective randomized clinical trial. J Cataract Refract Surg. 2015;41:1631–40. doi: 10.1016/j.jcrs.2015.08.011. [DOI] [PubMed] [Google Scholar]
- 31.Kretz FT, Breyer D, Diakonis VF, Klabe K, Henke F, Auffarth GU, Kaymak H. Clinical Outcomes after Binocular Implantation of a New Trifocal Diffractive Intraocular Lens. J Ophthalmol. 2015;2015:962891. doi: 10.1155/2015/962891. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Mojzis P, Majerova K, Hrckova L, Pinero DP. Implantation of a diffractive trifocal intraocular lens: one-year follow-up. J Cataract Refract Surg. 2015;41:1623–30. doi: 10.1016/j.jcrs.2014.11.050. [DOI] [PubMed] [Google Scholar]
- 33.Zhao H, Mainster MA. The effect of chromatic dispersion on pseudophakic optical performance. Br J Ophthalmol. 2007;91:1225–9. doi: 10.1136/bjo.2007.118745. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Data Availability Statement
Dataset supporting the findings of this study is available upon request from Banu Tırun Acar, MD (e-mail: torunbanu@yahoo.com).


