Abstract
The purpose of this study is to examine what factors contributing to the variability in chronic obstructive pulmonary disorder (COPD) and asthma hospitalization rates when the influence of patient characteristics is being simultaneously considered by applying a risk adjustment method. A longitudinal analysis of COPD and asthma hospitalization of rural Medicare beneficiaries in 427 rural health clinics (RHCs) was conducted utilizing administrative data and inpatient and outpatient claims from Region 4. The repeated measures of risk-adjusted COPD and asthma admission rate were analyzed by growth curve modeling. A generalized estimating equation (GEE) method was used to identify the relevance of selected predictors in accounting for the variability in risk-adjusted admission rates for COPD and asthma. Both adjusted and unadjusted rates of COPD admission showed a slight decline from 2010 to 2013. The growth curve modeling showed the annual rates of change were gradually accentuated through time. GEE revealed that a moderate amount of variance (marginal R2 = 0.66) in the risk-adjusted hospital admission rates for COPD and asthma was accounted for by contextual, ecological, and organizational variables. The contextual, ecological, and organizational factors are those associated with RHCs, not hospitals. We cannot infer how the variability in hospital practices in RHC service areas may have contributed to the disparities in admissions. Identification of RHCs with substantially higher rates than an average rate can portray the need for further enhancement of needed ambulatory or primary care services for the specific groups of RHCs. Because the risk-adjusted rates of hospitalization do not very by classification of rural area, future research should address the variation in a specific COPD and asthma condition of RHC patients. Risk-adjusted admission rates for COPD and asthma are influenced by the synergism of multiple contextual, ecological, and organizational factors instead of a single factor.
Keywords: Rural health clinics, Affordable Care Act, COPD and asthma hospitalization, rurality
INTRODUCTION
Chronic obstructive pulmonary disorder (COPD) takes a heavy toll on costs of care, amounting to the projected annual cost for $49.9 billion in the United States (American Lung Association, 2013; Centers for Disease Control and Prevention, 2012; Kabir, Connolly, Koh, & Clancy, 2010). COPD is a major contributing factor to morbidity, disability and mortality in the older adult population. Hospitalizations associated with COPD and asthma are often cited as an ambulatory care sensitive condition or potentially avoidable hospitalization. Empirical research suggests that personal attributes (Kabir et al., 2010; Ong, Earnest, & Lu, 2005), socioeconomic status (Trachtenberg, Dik, Chateau, & Katz, 2014), health care system or provider factors (Casalino et al., 2014; O’Malley, Pham, Schrag, Wu, & Bach, 2015;), health education for self-care management (Gadoury et al., 2005), and access to primary care (Caminal, Starfield, Sanchez, Casanova, & Morales, 2005) are potential predictor variables for COPD hospitalizations. However, little is known about how these factors contribute to the variability in COPD hospitalization rates when the influence of patient characteristics is being simultaneously considered by applying a risk adjustment method.
The Centers for Medicare and Medicaid Services (CMS) has started monitoring the avoidable hospitalizations by implementing a financial sanction plan to eliminate this hospital quality problem. Beginning October 2012, Medicare payments decreased by 1- 2% in 2013 and 3% in 2014. Beginning in October 2014, the readmission rate for Medicare patients with chronic obstructive pulmonary conditions were included. Concomitantly, the enactment of the Patient Protection and Affordable Care Act (abbreviated as the ACA) in March 23, 2010, is expected to enhance patient-centered care, particularly related to an emphasis on the improved delivery of ambulatory care and prevention by expanding health insurance coverage for the uninsured (Wan, Ortiz, Berzon, & Lin, 2015).
Our construction of a unique database for Rural Health Clinics (RHCs) for a period of seven years from 2007 through 2013 (including the pre-ACA period and the post-ACA period) offers a unique opportunity to examine trends and patterns of rural disparities in COPD and asthma hospitalizations in eight states of Region 4 (Alabama, Florida, Georgia, Kentucky, Mississippi, North Carolina, South Carolina, and Tennessee).
Research literature suggests that the severity of illness and other personal characteristics may explain differential rates in COPD and asthma hospitalizations (Quintana et al., 2015). However, high hospital admission rates have been attributable to the lack of transitional care (Gold, Ortiz, & Wan, 2013; Jackson, Trygstad, DeWalt, & DuBard, 2013; Mor & Besdine, 2011), inadequate or poor access to primary care (Caminal et al., 2005; Joynt, Harris, Orav, & Jha, 2011; McCall, Brody, Mobley, & Subramenian, 2004), racial or socioeconomic inequalities (Biello, Rawlings, Carroll-Scott, Browne, & Ickovics, 2010; Chang, Mirvis, & Waters, 2008; Gottlieb, Beiser, & O’Connor, 1995; Laditka, Laditka, & Masanduno, 2003), and the provision of poor quality of hospital care (Jencks, Williams, & Coleman, 2009; The Official U.S. Government Site for Medicare, 2014).
The purpose of this investigation is to explore how contextual, ecological and organizational factors of RHCs may influence variations in COPD and asthma hospitalization rates after having risk-adjusted pertinent patient factors among Medicare beneficiaries who have access to RHCs in the eight states. More specifically, following research questions relevant to the patterns and trends of risk-adjusted COPD and asthma hospitalization rates of rural Medicare patients are addressed in this empirical study:
What are the risk-adjusted COPD and asthma hospitalization rates (per clinic) in varying categories of rural areas for 2007 through 2013?
Have the rates changed over the past seven years (2007 through 2013)? Can the change be reflected by the period effect attributable to the Affordable Care Act when other influencing factors are simultaneously considered?
Is there a difference in risk-adjusted COPD and asthma hospitalization rates between low- and high-socioeconomic status areas served by RHCs?
The present study uses time-series data aggregated into RHC years (472 RHCs observed for seven years) as the unit of analysis, using multivariate modeling analytics to identify statistically significant factors influencing the disparities in risk-adjusted COPD and asthma hospitalization rates. The identification of contributing factors to the high prevalence of COPD and asthma hospital admissions may shed some light on potential policy development or organizational interventions targeting the mutable contextual (e.g., policy, socioeconomic development, rurality, health and professional resources, etc.), ecological factors (e.g., aggregated indicators of population distribution, racial composition, patient mix, dual eligibility status, etc. in areas served by RHCs), and organizational factors (e.g., affiliation with accountable care organizations, years in operation, size, staffing mix, ownership, and other RHC characteristics).
RELATED RESEARCH
Avoidable hospitalizations are considered an important measure of sentinel health events and community health performance. Brennan (2014) reported findings from CMS research on Medicare and suggested that high avoidable hospitalization rates represent quality problems. Using 2003-2004 data Jencks et al. (2009) showed that hospitalization rates across Region 4 vary by state from 18.1% in South Carolina to 21.9% in Mississippi. In the United States, morbidity caused by COPD accounts for 4% - the fourth leading cause of mortality ranked after heart attacks, cancer and stroke (Hurd, 2000). Furthermore, air pollution and smoking may have contributed directly the increase of COPD hospitalization.
According to a recent report by the University of Washington Population Health Institute (2014) on county variations in health and health care in the U.S., the four contributing factors to the improvement of health care and health care outcomes by the percentage distribution include: 1) 10% attributed to physical environment and policy, 2) 20% to clinical care and technology, 3) 30% to personal behavioral factors, and 4) 40% to social and economic factors. This report points out strategic priorities for achieving population health by reducing health care disparities attributable to the contextual, ecological, and health delivery system factors. The potential avoidable COPD hospitalizations can be further identified if the determinants of risk-adjusted rates are made. The present study explores how the availability of RHCs, the ACA period effect, rurality, numbers of dual eligible, and many aggregated organizational characteristics at the RHC level, may influence the patterns and trends of risk-adjusted rates of COPD and asthma hospitalizations for the period of 2007 through 2013.
METHODS
Design and Data Sources
We conducted a longitudinal analysis of COPD and asthma hospitalization of rural Medicare beneficiaries based on administrative and claims data gathered from a variety of data sources compiled for CMS. The presence of hospital billing codes for admissions was coded as a hospitalized case (coded 1) or not-hospitalized case (coded 0). The detailed calculation for COPD and asthma hospitalization is described as follows.
Denominator
Patients should have at least one international classification of disease (ICD-9) diagnosis code for COPD or asthma in the Medicare Outpatient claims during the calendar year. These codes are as follows: 4910, 4911, 49120, 49121, 4918, 4919, 4920, 4928, 494, 4940, 4941, 496, 49300, 49301, 49302, 49310, 49311, 49312, 49320, 49321, 49322, 49381, 49382, 49390, 49391, and 49392. The exceptions and exclusions in the denominator were patterned after the measure ACO #9 version 9 (Centers for Medicare & Medicaid Services, 2012). In other words, the end-stage-renal disorder (ESRD) patients and patients transferring from a hospital, skilled nursing facility or intermediate care facility, or another health care facility were excluded from the analysis.
Numerator
Patients should have one principal ICD-9 diagnosis of COPD or asthma in Medicare Inpatient claims. The details of codes are as follows:
-
1)
A diagnosis code indicating COPD or asthma 4910, 4911, 49120, 49121, 4918, 4919, 4920, 4928, 494, 4940, 4941, 496, 49300, 49301, 49302, 49310, 49311, 49312, 49320, 49321, 49322, 49381, 49382, 49390, 49391, 49392; or (2) a principal diagnosis code of 4660 or 490 and a secondary diagnosis of one or more of the codes 4910, 4911, 49120, 49121, 4918, 4919, 4920, 4928, 494, 4940, 4941, or 496.
The COPD and asthma hospitalization rate is computed as the total number of Medicare inpatient claims for hospital admissions divided by the total number of outpatient claims of COPD and asthma patients served by each RHC per year. The formula used was as follows:
Using logistic regression analysis of the Medicare claims file, we created a Charlson Index (Deyo, Cherkin, & Ciol, 1992), age, gender, race, and other personal factors as risk adjusters, to arrive at an expected number of COPD and asthma admissions for each RHC per year. The risk-adjusted COPD and asthma admission rate, a dependent variable in this analysis, was then calculated using the expected number of COPD and asthma admissions (numerator) divided by the total COPD and asthma outpatients treated by each RHC (denominator). The formula is as follows:
Our analysis of variation in the adjusted COPD and asthma hospitalization rate may be accounted for by the contextual, ecological, and organizational factors. Analyses present major characteristics of RHCs serving Medicare beneficiaries in varying degrees of rural areas: RHCs located in an urbanized area, large rural area, small rural area, and isolated rural area. The total rural older adults studied, ranged from 202,707 patients in 2007 to 225,344 patients in 2013. Excluding missing cases for not having the total number of patients documented in the Medicare claims file, we retained only 472 RHCs for this research.
Measurements
The contextual variables, derived from the Health Resources and Services Administration (HRSA) Area Health Resource File (AHRF), include: the percentage of poverty population, rurality (in four levels), racial composition, state, etc. In addition, a dichotomized predictor variable showing the potential period effect of the ACA on RHC performance was created: before 2010 (2007 through 2009) coded as 0 and after 2010 (2010 through 2013) coded as 1. Personal attributes of Medicare beneficiaries such as size of patient population served, average age, % female patients, % Hispanic users, % White patients, % dually eligible, and diagnostic mix indicators are considered as aggregated indicators or ecological factors in this analysis. The organizational factors include years of RHC operation, staff mix (a ratio of primary care provider visits by the total number of health clinic visits), staff size, provider-based practice, ownership, etc.
Disparity in Adjusted COPD and Asthma Admission Rates between a Given Year and a Reference Year for Medicare Beneficiaries Accessing each RHC
The formula for computing the disparity ratio is as follows: (the deviation of an annual rate from the reference average rate in 2009 divided by this reference average rate) × 100. The deviation from an average rate or a norm is used to compare the changes in adjusted COPD and asthma admission rates of RHCs. For the purpose of this research, an average rate in 2009 of all study RHCs was used as a reference value so that the percentage deviation from an average rate of admissions per year refers to the disparity: a positive value refers to poorer performance (higher COPD and asthma hospitalization rate) than an average RHC rate in 2009 and a negative value (lower rate) indicates better performance.
Because of the problematic issue of missing values in the claims file, longitudinal data from 2007 to 2013 were pooled together in the analysis. Thus, the unit of analysis for a dependent variable is referred to as “RHC-year,” and the risk-adjusted COPD and asthma admission rate deviation from that of the 2009 rate was determined for all 472 RHCs.
Analytical methods
Three statistical methods were used to analyze the data pooled from 2007 to 2013, similar to a time-series without using a panel group of RHCs in the longitudinal analysis. Descriptive statistics are presented to illustrate the general characteristics of the RHCs in Region 4. Significance tests, at the alpha level of 0.05, were performed when the analysis of variance for eight states for a given attribute or variable was appropriate. The repeated measures of risk-adjusted COPD and asthma admission rate were analyzed by growth curve modeling for 2007 through 2013. This enabled us to ascertain if any autocorrelations of the variables exist (Wan, 2002). Regression of the dependent variable on selected predictors clustered into contextual, organizational, and ecological variables was analyzed by a generalized estimating equation (GEE) method, using the pooled data for the 472 RHCs with complete information for COPD and asthma admissions (N= 2,910 RHC years) and analyzed by the SAS Institute’s GENMOD procedure.
Both time constant and time-varying predictors were included. The reasons for performing GEE to identify the relevance of selected predictors in accounting for the variability in adjusted admission rates for COPD and asthma are: 1) a repeated measure of the risk-adjusted hospitalization rate of RHCs in seven years as the dependent variable; 2) some missing values found for the predictor variables; 3) robust standard estimates available for performing more consistent and accurate tests of statistical significance; and 4) the availability of the Quasi-likelihood Information Criterion [QIC] to reflect the relative quality of the proposed model in fitting the data.
RESULTS
Descriptive Statistical Analysis
Comparing Crude and Risk-Adjusted COPD and Asthma Hospitalization Rates of RHCs by State
For the crude hospitalization rates for COPD and asthma at the RHC level, all eight states located in Region 4 tend to have varying levels of admissions (Table 1). Lower average rates were found in Mississippi and South Carolina as compared to the other states. Kentucky had the highest rate (13.11%) for all seven years. Statistically significant yearly variations by state were further identified, using analysis of variance of average rates: only Kentucky and Georgia showed a statistically significant yearly variation. For the risk-adjusted hospitalization rates of COPD and asthma, lower averages were found for Mississippi and South Carolina than for other states. Kentucky had the highest average adjusted rate (10.29%) as compared to other states. Yearly fluctuations in the adjusted rate were observed for each state. However, the rates for 2013 appeared to decline in the seven states, except for North Carolina (where there was no change).
Table 1.
Crude and Risk-Adjusted Rates of COPD and Asthma Hospitalization Per Hundred COPD and Asthma Outpatients Served by RHCs in Eight States by Year
| State | Year | 2007 | 2008 | 2009 | 2010 | 2011 | 2012 | 2013 | Average |
|---|---|---|---|---|---|---|---|---|---|
| AL | Crude | 9.27 | 10.19 | 10.09 | 9.83 | 9.40 | 9.64 | 9.35 | 9.7 |
| Adjusted | 8.24 | 9.93 | 9.84 | 9.54 | 9.56 | 9.55 | 9.48 | 9.45 | |
| FL | Crude | 9.75 | 11.91 | 12.25 | 11.42 | 11.58 | 11.40 | 12.04 | 11.46 |
| Adjusted | 8.55 | 10.27 | 10.30 | 9.98 | 10.06 | 10.01 | 9.77 | 9.84 | |
| GA | Crude | 7.8 | 10.34 | 10.64 | 10.33 | 10.44 | 10.58 | 10.05 | 10.01 |
| Adjusted | 7.85 | 9.54 | 9.59 | 9.33 | 9.33 | 9.27 | 9.04 | 9.13 | |
| KY | Crude | 10.99 | 14.21 | 13.74 | 12.33 | 13.27 | 13.44 | 13.91 | 13.11 |
| Adjusted | 8.95 | 10.73 | 10.75 | 10.47 | 10.57 | 10.39 | 10.15 | 10.29 | |
| MS | Crude | 6.25 | 7.57 | 7.65 | 7.51 | 7.11 | 7.15 | 6.92 | 7.18 |
| Adjusted | 7.51 | 9.06 | 8.96 | 8.71 | 8.69 | 8.65 | 8.43 | 8.58 | |
| NC | Crude | 7.61 | 8.88 | 9.00 | 8.96 | 8.71 | 8.44 | 8.08 | 8.54 |
| Adjusted | 7.90 | 9.51 | 9.38 | 9.29 | 9.31 | 9.22 | 9.22 | 9.11 | |
| SC | Crude | 6.53 | 7.50 | 7.55 | 8.14 | 7.42 | 7.16 | 7.15 | 7.36 |
| Adjusted | 7.44 | 8.97 | 9.13 | 8.92 | 8.90 | 8.86 | 8.70 | 8.71 | |
| TN | Crude | 9.34 | 12.05 | 12.66 | 12.37 | 12.87 | 12.34 | 9.73 | 11.65 |
| Adjusted | 8.67 | 10.32 | 10.33 | 10.01 | 9.97 | 9.92 | 9.66 | 9.84 |
Graphic Trend in Risk-Adjusted Rates of Hospitalization in Rural Medicare Beneficiaries with COPD and Asthma
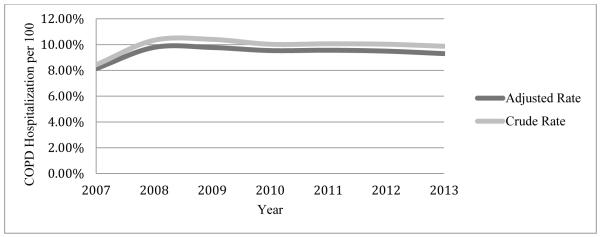
A steady increase in risk-adjusted rates for hospitalization for COPD and asthma patients has been observed from 2007 through 2009 (Fig. 1). The rates in 2010 through 2013 showed a slight decline. A similar pattern was observed for both crude and risk-adjusted rates for COPD and asthma hospitalization although risk-adjusted rates were slightly lower than crude rates.
Fig. 1.
Crude and Risk Adjusted COPD and Asthma Hospitalization Rates in 472 RHCs by Year 2007 through 2013
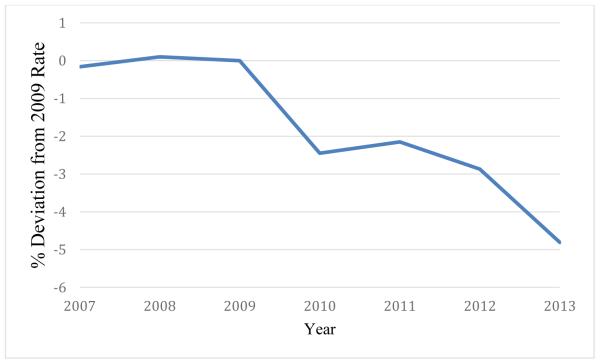
Graphic Trend in Disparity Ratio of COPD and Asthma Hospital Admissions
The risk-adjusted admission rates of each RHC were compared to an average rate of 2009 in the pre-ACA period. The percentage deviations from this mean were calculated: the higher the positive value, the poorer the care of COPD and asthma patients in the ambulatory care setting is observed. The disparity trend is shown in Fig. 2: the average rate of 2013 is 5 percentage points lower than that of 2009.
Fig. 2.
Trend for Disparities in Risk Adjusted COPD and Asthma Hospitalization Rates Compared to 2009 in 472 RHCs by Year 2007 through 2013
Multivariate Analysis
Correlations of Annual Risk-Adjusted Admission Rates for COPD and Asthma (2007 through 2013)
Serial-correlations are considered to be an important methodological problem that has to be addressed in longitudinal analysis of RHC data. The correlation analysis shows that the rates for risk adjusted COPD and asthma admissions among the seven years studied were strongly and positively associated. The potential threat of auto-regression of the rates in longitudinal analysis was further examined using latent growth curve modeling to detect the change trajectories of COPD and asthma rates.
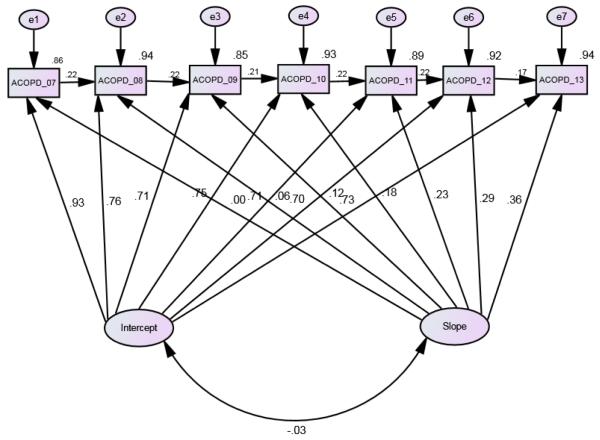
Latent Growth Curve Modeling of Risk-Adjusted COPD and Asthma Hospitalization Rates (2007 through 2013)
Fig. 3 shows that a latent growth curve model of seven waves the observations for 472 RHCs formulated to examine the relationship between the two latent growth components, the intercept reflecting the initial status and the slope of yearly rates showing the trajectories of rate change. This latent growth curve model fits the data very well (with a Chi-square value of 4.921, 12 degrees of freedom; NFI= 0.991, TLI = 0.983, CFI = 0.993, and RMSEA = 0.075). A negative and statistically insignificant association between the two growth factors (intercept and slope) was found (−0.030) as autoregressions of the rates were simultaneously considered in the model. The relationship between each annual rate and the intercept is 0.928, 0.763, 0.705, 0.751, 0.705, 0.701, and 0.733 from 2007 through 2013, respectively. The relationship between each annual rate and the slope is 0.00, 0.062, 0.115, 0.184, 0.230, 0.286 and 0.359 for the respective years. This suggests that the rates of change were gradually accentuated through time.
Fig. 3.
An Autoregressive Latent Growth Curve Model of Risk-Adjusted COPD and Asthma Admission (ACOPD) Rates: 2007 through 2013.
GEE analysis of predictors
GEE offers a unique perspective in the examination of repeated measures such as risk-adjusted hospital admission rates for COPD and asthma for the 2,910 RHC years. The analysis follows a two-step hierarchical regression: 1) the average adjusted rate of 2009 as a continuous dependent variable was regressed on each group of predictors such as the contextual, organizational and aggregated patient attributes independently; and 2) statistically significant predictors from each group of predictors, using a backward selection method, were combined in the second step of regression analysis. Rurality was categorized into three dummy variables (large rural, small rural, and isolated rural areas with RHC located in an urbanized area as a reference group) in the final regression equation. The results of substantively meaningful and statistically significant predictors for the risk-adjusted hospitalization rate for COPD and asthma are presented in Table 2. For the purpose of illustrating the relative importance of each predictor included in the analysis, we present standardized regression coefficients (parameter estimates) and relevant statistics in the table. A positive regression coefficient indicates that a higher risk-adjusted hospital admission rate of RHC years is observed. Similarly, a negative coefficient suggests that a lower average adjusted admission rate for COPD and asthma is observed for a given predictor variable. A marginal R2 for the estimating equation is also computed to show the total variance in the dependent variable explained by all predictors included.
Table 2.
Analysis of GEE Parameter Estimates for Predictors of Hospital Admission Rates for COPD and Asthma in RHCs (N = 2,910 RHC Years)
| Variable | Estimate | Standard Error |
95 % Confidence | Z | P- value | |
|---|---|---|---|---|---|---|
| Lower | Upper | |||||
| Contextual | ||||||
| ACA Period Effect | 0.096 | 0.008 | 0.081 | 0.111 | 12.76 | <.0001 |
| Rurality | ||||||
| Remote
and Isolated Rural Area |
−0.028 | 0.020 | −0.067 | 0.011 | −1.42 | 0.1570 |
| Small Rural Area | −0.016 | 0.020 | −0.055 | 0.024 | −0.77 | 0.4392 |
| Large Rural Area | −0.028 | 0.019 | −0.064 | 0.009 | −1.49 | 0.1355 |
| Ecological | ||||||
| State | ||||||
| Alabama | 0.037 | 0.014 | 0.010 | 0.064 | 2.72 | 0.0066 |
| Florida | 0.039 | 0.024 | −0.007 | 0.085 | 1.67 | 0.0940 |
| Georgia | 0.039 | 0.014 | 0.012 | 0.065 | 2.86 | 0.0043 |
| Kentucky | 0.080 | 0.021 | 0.038 | 0.122 | 3.74 | 0.0002 |
| North Carolina | 0.030 | 0.015 | 0.0004 | 0.059 | 1.99 | 0.0471 |
| South Carolina | 0.061 | 0.014 | 0.033 | 0.088 | 4.31 | <.0001 |
| Tennessee | 0.045 | 0.014 | 0.018 | 0.072 | 3.32 | 0.0009 |
| Females in
A County |
−0.034 | 0.014 | −0.060 | −0.008 | −2.53 | 0.0116 |
| African
Americans in A County |
−0.057 | 0.028 | −0.111 | −0.002 | −2.03 | 0.0419 |
| Older Adults in
a County |
0.034 | 0.019 | −0.002 | 0.071 | 1.86 | 0.0628 |
| Poverty
Population in A County |
0.103 | 0.020 | 0.064 | 0.142 | 5.16 | <.0001 |
| % Dually Eligible | 0.115 | 0.023 | 0.070 | 0.160 | 4.99 | <.0001 |
| Organizational | ||||||
| Years in operation | −0.028 | 0.013 | −0.053 | −0.003 | −2.22 | 0.0267 |
| Number of
Patients Treated |
0.086 | 0.022 | 0.042 | 0.130 | 3.83 | 0.0001 |
| % White Patients | 0.733 | 0.027 | 0.679 | 0.786 | 26.97 | <.0001 |
| % Female Patients | −0.148 | 0.020 | −0.187 | −0.109 | −7.41 | <.0001 |
| %Other Users | 0.119 | 0.015 | 0.090 | 0.148 | 8.15 | <.0001 |
Notes: R-squared: 0.663.
QIC = 2943.05 and QICu = 2931.00.
Z- statistics greater or equal to ∣ 1.96 ∣ are statistically significant at 0.05 level.
Table 2 reveals several interesting findings as follows: 1) the variable “ACA period” had a positive relationship to COPD and asthma admissions; 2) no apparent differences by rurality were found; 3) Alabama, Georgia, Kentucky, North Carolina, South Carolina and Tennessee had a higher rates than Florida and Mississippi; 4) RHCs that treated more patients had a higher admission rate; and 5) the percentage of the dually eligible and White patients treated at RHCs was positively related to the rates. Lower rates were more likely to be related to the percentage of African Americans, females, poverty population where RHCs were located, years of operation, and the percentage of female patients treated at RHCs. The total variance explained by the 21 predictors shown by the marginal R-squared value is 66.3%.
DISCUSSION
The analysis of RHC-related data with multiple years of observation enables us to shed some light on the variability in both crude and risk-adjusted admission rates for COPD and asthma. The findings of this empirical study offer specific answers to the research questions noted earlier. First, there was little variation in admission rates for COPD and asthma by rurality or rural classification. This finding is confirmed by multivariate analysis, holding other predictor variables constant. Second, there was a positive relationship between the average number of RHC patients treated and the COPD and asthma admission rate. Thus, increasing the total number of RHC patients may lead to the increase in COPD and asthma admissions to hospitals.
Third, both adjusted and unadjusted rates of COPD and asthma admission showed a slight decline from 2010 to 2013 although the speed of change was relatively small. The latent growth curve model offered more substantive explanations in regard to the nature of hospital admission rates for COPD and asthma. Because of the interdependence of the yearly rates, the change trajectories of admissions had to be considered in a thorough analysis of the contextual, ecological, and organizational predictors of the COPD and asthma admission rates. Careful analysis of the 21 predictor variables with a GEE method revealed that a moderate amount of variance (marginal R2 = 0.66) in the risk-adjusted hospital admission rates for COPD and asthma was accounted for by contextual, ecological, and organizational variables.
Fourth, the percentage of dually eligible beneficiaries reflects the relative socioeconomic and health status of Medicare patients served by RHCs. This variable was positively and statistically significantly associated with the COPD and asthma hospitalization rates: the higher percentage of the dually eligible served by RHCs, the higher the rate of admissions. Similarly, the greater the number of impoverished and White population in a county where RHCs were located, the higher the hospitalization rate for COPD and asthma. It is interesting to note that other aggregated demographic characteristics such as the percentage of female patients treated at RHCs were negatively associated with the COPD and asthma admission rate.
These empirical findings are relatively robust since our analyses are based on GEE analysis of longitudinal data with a risk adjustment method to remove patient differences. However, this study may subject to a few methodological limitations. First, the unit of analysis based on RHC year was measured by hospital admission claims for COPD and asthma of Medicare patients. The measurement was based on episodes or events of the interest. We cannot infer how the variability in hospital practices in RHC service areas may have contributed to the disparities in admissions. Second, the contextual, ecological, and organizational factors are those associated with RHCs, not hospitals. Our interest is to determine how the RHC and community area characteristics, reflecting the contextual, ecological, and organizational attributes, may account for the variability in COPD and asthma admissions in RHC years. Third, because the purpose of this investigation was to focus on the variability in the COPD admission rates, identification of RHCs with substantially higher rates than an average rate can portray the need for further enhancement of needed ambulatory or primary care services for the specific groups of RHCs. Lastly, we were unable to explore the full picture of regional variation in hospital admissions for COPD and asthma among RHCs in the United States because our data were restricted to eight southeastern states in Region 4.
Notwithstanding the limitations just described, this investigation has enlightened us about the lack of variability in hospital admission rates for COPD and asthma by rurality; the risk-adjusted rates of hospitalization do not vary by classification of rural area. Future studies should address the variation in a specific COPD and asthma condition of RHC patients. In addition, the effectiveness in detecting the underlying causes or mechanisms, such as the severity of COPD or chronicity of the illness, for the variations in hospital admissions for COPD and asthma and in implementing feasible organizational or community interventions, should be explored in future rural health research.
CONCLUSIONS
Our study offers new evidence showing the relevance of contextual, ecological, and organizational factors in influencing the disparities in hospital admission rates for COPD and asthma. The admission rates of rural Medicare beneficiaries were much lower in Region 4 than the U.S. average. No apparent ACA effect on hospital admissions for COPD and asthma was observed. The CMS Hospital Readmissions Reduction Program and other quality improvement initiatives may account for the rate decline in 2013, however. In order to disentangle the co-variations or synergistic effects of both ACA and Readmissions Reduction Program, researchers have to design and conduct thorough studies to investigate hospital practice variations in rural areas for multiple years.
This study contributes to the literature in social epidemiological research from the contextual, ecological, and organizational perspectives in the analysis of longitudinal data. The results reveal that it is not a single operative factor alone that influences risk-adjusted admission rates for COPD and asthma. The disparities, portrayed by race coupled with socioeconomic status, are influenced by access to primary care and practice patterns (Pappa, Hadden, & Fisher, 1997; Roos, Walld, Vhanova, & Bond, 2005). It is the synergism of multiple contextual, ecological, and organizational factors, as shown in this study, that should be considered in the design and implementation of intervention studies such as using proper incentive plans or penalties to address the problem of potentially avoidable hospital admissions for COPD and asthma through prevention and enhancement of disease management of rural Medicare beneficiaries. Furthermore, an evidence-based approach to guiding effective and efficient changes in admission practices coupled with the use of community-based care modalities, such as transitional care, mobile health care management technologies and a comprehensive care program for COPD (Fan, et al., 2012) should be formulated.
ACKNOWLEDGEMENTS
The analysis for this chapter was supported by the National Institute on Minority Health and Health Disparities of the National Institute of Health under Award Number U24MD006954. The content is solely the responsibility of the authors and does not necessarily represent the official views of the National Institute of Health.
Sources of Funding
Research for this chapter was funded by the National Institute on Minority Health and Health Disparities of the National Institute of Health.
Footnotes
Conflicts of Interest
None of the authors declare having any conflicts of interest.
Contributor Information
Thomas T. H. Wan, College of Health and Public Affairs, Doctoral Program in Public Affairs, University of Central Florida, Orlando, FL.
Yi-Ling Lin, College of Health and Public Affairs, University of Central Florida, Orlando, FL, Address: P.O. Box 162369, Orlando, FL 32816, yllin@knights.ucf.edu.
Judith Ortiz, College of Health and Public Affairs, University of Central Florida, Orlando, FL, Address: P.O. Box 162369, Orlando, FL 32816, Judith.Ortiz@ucf.edu.
REFERENCES
- American Lung Association . Trends in COPD morbidity and mortality. Epidemiology and Statistics Unit, Research and Health Education Division; 2013. [Google Scholar]
- Biello KB, Rawlings J, Carroll-Scott A, Browne R, Ickovics JR. American Journal of Preventive Medicine. 2010;38(1):54–60. doi: 10.1016/j.amepre.2009.08.027. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Brennan N. Real-time Reporting of Medicare Readmissions Data. Centers for Medicare and Medicaid Services; Washington, D.C.: 2014. [Google Scholar]
- Caminal J, Starfield B, Sanchez E, Casanova C, Morales M. The role of primary care in preventing ambulatory care sensitive conditions. European Journal of Public Health. 2005;14(3):246–251. doi: 10.1093/eurpub/14.3.246. [DOI] [PubMed] [Google Scholar]
- Casalino LP, Pesko MF, Ryan AM, Mendelsohn JL, Copeland KR, Ramsay PP, Shortell SM. Small primary care physician practices have low rates of preventable hospital admissions. Health Affairs. 2014;33(9):1680–1688. doi: 10.1377/hlthaff.2014.0434. [DOI] [PubMed] [Google Scholar]
- Centers for Disease Control and Prevention Chronic Obstructive Pulmonary Disease Among Adulst—US 2011. MMWR. 2012;61(46):938–943. [Google Scholar]
- Centers of Disease Control and Prevention Chronic obstructive pulmonary disease among adults—US 2011. MMWR. 2012;61(46):936–943. [Google Scholar]
- Centers for Medicare & Medicaid Services ACO #9 – Prevention Quality Indicator (PQI): Ambulatory Sensitive Conditions Admissions for Chronic Obsructive Pulmonary Disease (COPD) or Asthma in Older Adults, Version 9. 2012 Aug; Retrieved from http://www.cms.gov/Medicare/Medicare-Fee-for-Service-Payment/sharedsavingsprogram/Downloads/Measure-ACO-9-Asthma.pdf.
- Chang CF, Mirvis DM, Waters TM. The effects of race and insurance on potentially avoidable hospitalization in Tennessee. Medical Care. 2008;65(5):596–616. doi: 10.1177/1077558708318283. [DOI] [PubMed] [Google Scholar]
- Deyo RA, Cherkin DC, Ciol MA. Adapting a clinical comorbidity index for use with ICD-9-CM administrative databases. Journal of Clinical Epidemiology. 1992;45(6):613–619. doi: 10.1016/0895-4356(92)90133-8. [DOI] [PubMed] [Google Scholar]
- Fan VS, Gaziano JM, Lew R, Bourbeau J, Adams SG, Leatherman S, Niewoehner DE. A comprehensive care management program to prevent chronic obstructive pulmonary disease hospitalizations: A randomized controlled trial. Annals of internal Medicine. 2012;156(10):673–683. doi: 10.7326/0003-4819-156-10-201205150-00003. [DOI] [PubMed] [Google Scholar]
- Gadoury MA, Schwartzman K, Rouleau M, Maltais F, Julien M, Beaupré A, et al. Self-management reduces both short- and long-term hospitalization in COPD. European Respiratory Journal. 2005;26(5):853–857. doi: 10.1183/09031936.05.00093204. [DOI] [PubMed] [Google Scholar]
- Gold A, Ortiz J, Wan TTH. Transitional care: Looking for the right shoes to fit elderly patients. Care Management Journals. 2013;14(2):1–6. doi: 10.1891/1521-0987.14.2.78. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Gottlieb DJ, Beiser AS, O’Connor GT. Poverty, race, and medication use are correlates of asth ma hospitalization rates: A small area analysis in Boston. Chest. 1995;108(1):28–35. doi: 10.1378/chest.108.1.28. [DOI] [PubMed] [Google Scholar]
- Hurd S. The impact of COPD on long health worldwide: epidemiology and incidence. Chest. 2000;117(2_suppl):1s–4s. doi: 10.1378/chest.117.2_suppl.1s. [DOI] [PubMed] [Google Scholar]
- Jackson CT, Trygstad TK, DeWalt DA, DuBard CA. Transitional carecut hospital readmissions for North Carolina Medicaid patients with complex chronic conditions. Health Affairs. 2013;32(8):407–415. doi: 10.1377/hlthaff.2013.0047. [DOI] [PubMed] [Google Scholar]; Kabir Z, Connolly GN, Koh HK, Clancy L. Chronic obstructive pulmonary disease hospitalization rates in Massachusetts: A trend analysis. Q. Journal of Medicine. 2010;103(3):163–168. doi: 10.1093/qjmed/hcp190. [2] [DOI] [PMC free article] [PubMed] [Google Scholar]
- Jencks SF, Williams V, Coleman EA. Rehospitalizations among patients in the Medicare fee-for-services program. New England Journal of Medicine. 2009;360(14):1418–1428. doi: 10.1056/NEJMsa0803563. [DOI] [PubMed] [Google Scholar]
- Joynt KE, Harris Y, Orav EJ, Jha A. Quality of care and patient outcomes in critical access rural hospitals. Journal of American Medical Association. 2011;306(1):45–52. doi: 10.1001/jama.2011.902. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kabir Z, Connolly GN, Koh HK, Clancy L. Chronic obstructive pulmonary disease hospitalization rates in Massachusetts: A trend analysis. Q. Journal of Medicine. 2010;103(3):163–168. doi: 10.1093/qjmed/hcp190. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Laditka JN, Laditka SB, Mastanduno MP. Hospital utilization for ambulatory care sensitive conditions: Health outcome disparities associated with race and ethnicity. Social Science and Medicine. 2003;57(8):1429–1441. doi: 10.1016/s0277-9536(02)00539-7. [DOI] [PubMed] [Google Scholar]
- McCall NT, Brody E, Mobley L, Subramenian S. Investigation of Increasing Rates of Hospitalization for Ambulatory Care Sensitive Conditions among Medicare Fee-for-Services Beneficiaries. RTI International. A contract report submitted to the Centers for Medicare and Medicaid Services; Durham, NC: 2004. [Google Scholar]
- Mor V, Besdine RW. Policy options to improve discharge planning and reduce hospitalization. Journal of American Medical Association. 2011;305(3):302–303. doi: 10.1001/jama.2010.2006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- O’Malley AS, Pham HH, Schrag D, Wu B, Bach PB. Potentially avoidable hospitalization for COPD and pneumonia: The role of physician and practice characteristics. Medical Care. 2015;45(6):562–570. doi: 10.1097/MLR.0b013e3180408df8. [DOI] [PubMed] [Google Scholar]
- Ong K, Earnest A, Lu S. A multidimensional grading system as predictor of hospitalization for COPD. Chest. 2005;128(6):3810–3816. doi: 10.1378/chest.128.6.3810. [DOI] [PubMed] [Google Scholar]
- Pappas G, Hadden WC, Fisher GF. Potentially avoidable hospitalizations: Inequalities in rates between US socioeconomic groups. American Journal of Public Health. 1997;87(5):811–816. doi: 10.2105/ajph.87.5.811. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Quintana JM, Unzurrunzaga A, Garcia-Gutierrez S, Gonzalez, Lafuente I, Bare M, Fernandez de Larrea N, Rivas F, Esteban C, IRYSS-COPD Group Predictors of hospital length of stay in patients with exacerbations of COPD: A cohort study. Journal of General Internal Medicine. 2015;30(6):824–831. doi: 10.1007/s11606-014-3129-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Roos LL, Walld R, Vhanova J, Bond R. Physician visits, hospitalizations, and socioeconomic status: ambulatory care sensitive conditions in a Canadian setting. Health Services Research. 2005;40(4):1167–1185. doi: 10.1111/j.1475-6773.2005.00407.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- The Official U.S. Government Site for Medicare 30-day death and readmission measures. 2014 Retrieved from http://www.medicare.gov/hospitalcompare/data/30-day-measures.html.
- The University of Wisconsin Population Health Institute County Health Rankings and Roadmap: 2014 Rankings—Key Findings Report. 2014 Retrieved from http://www.countyhealthrankings.org.
- Trachtenberg AJ, Dik N, Chateau D, Katz A. Inequalities in ambulatory care and the relationship between socioeconomic status and respiratory hospitalization: A population-based study of a Canadian City. Annals of Family Medicine. 2014;12(5):402–407. doi: 10.1370/afm.1683. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wan TTH. Evidence-Based Health Care Management: Multivariate Modeling Approaches. Kluwer Academic Publishers; Boston: 2002. [Google Scholar]
- Wan TTH, Ortiz J, Berzon R, Lin YL. Variations in colorectal cancer screening of Medicare beneficiaries served by rural health clinics. Health Services Research and Managerial Epidemiology. 2015 doi: 10.1177/2333392815597221. published July 22, 2015. [DOI] [PMC free article] [PubMed] [Google Scholar]