Abstract
Systemic sclerosis, or scleroderma, rarely involves the cervical spine. The disorder can induce dystrophic calcinosis that can cause spinal canal stenosis and spinal instability. An association between this pathology with acute traumatic central cord syndrome and dural erosion is rare. This case report highlights such an association and postulates the underlying mechanisms. A 57-year-old female, with a history of chronic obstructive pulmonary disease (COPD), schizophrenia and systemic sclerosis, presented with weakness in all extremities after a minor fall. Imaging demonstrated a calcified soft-tissue mass at C4/5 causing severe cord compression, cord edema spanning C3–C6, calcified soft-tissue masses at right C2/C3 facet joint and bilateral C4/5 facet joints, and significant subluxation at C4/5. Patient underwent C4–C7 laminectomies, and C3–T1 fixation and fusion. The calcinosis appeared to erode through the dura, which necessitated dura repair once the calcionsis was carefully debulked. The patient recovered well, and improved clinically with rehabilitation. Dystrophic calcinosis from underlying systemic sclerosis can cause significant chronic cervical stenosis, which may reduce the threshold for acute traumatic cervical cord syndrome under minor trauma. Moreover, dystrophic calcinosis may exhibit a propensity for dural erosion, possibly through chronic adhesions secondary to chronic inflammation. Aggressive removal of the calcinosis may breach the dura. Consequently, subtotal debulking may be reasonable if the spinal canal is adequately decompressed after laminectomies.
Subject terms: Chronic inflammation, Neuroscience
Systemic sclerosis, or scleroderma, is an idiopathic disease that affects the immune system, microvasculature and connective tissue.1,2 The disease distresses the skin, muscle, gastrointestinal tract, heart, lung and kidney.2 Infrequently, systemic sclerosis can affect the spine through dystrophic calcinosis of the spinal column.3–7 Several cases have documented destructive osteolysis of the posterior elements, causing spinal canal stenosis and spinal instability.8 An association between this pathology with acute traumatic central cord syndrome and dural erosion is rare. Surgical management, including findings and approaches, has been reported, but none have documented dural erosion of the calcinosis requiring dural repair.
The authors report a rare case where a patient with systemic sclerosis and spinal instability, secondary to calcinosis, suffered a hyperextension injury from a minor fall and developed acute central cord syndrome. During the operation, the calcinosis was observed to have eroded through the dura, necessitating dural repair. The authors conduct a brief literature review regarding systemic sclerosis, cervical calcinosis and surgical management.
A 57-year-old female, with a medical history of chronic obstructive pulmonary disease (COPD), schizophrenia and systemic sclerosis, presented to the emergency department with progressive weakness and numbness. Symptoms began after a minor fall 2 weeks ago; since that time, her gait and balance had declined where she suffered multiple falls. She also had episodes of urinary and bowel incontinence, which was partly attributed to her worsened mobility. On physical exam, her deltoids were 3/5, biceps 4/5, triceps 4/5, grips 4/5 and intrinsics 4/5. Her lower extremities were diffusely 4/5. Patient had bilateral Hoffman’s sign and elevated deep tendon reflexes.
Computed tomography cervical spine demonstrated calcified soft tissue, most significantly within the posterior elements at C4/5, with C4/5 subluxation (Figures 1a–c and 2). Magnetic resonance imaging cervical spine demonstrated epidural extension of the calcified soft tissue mass at C4/5 causing severe cord compression; cord edema spanned C3–C6; calcified soft tissue masses were seen along right C2/C3 facet joint and bilateral C4/5 facet joints (Figure 3). Her presentation was consistent with a central cord syndrome with hyperextension injury and spinal instability. Operative intervention was recommended. Following sub-periosteal dissection and calcinosis debulking, there was noted to be a dural rent where friable granulation tissue had indeed eroded through the dura laterally. This material was sent to pathology for frozen section along with necrotic bone. The dura was repaired primarily with 5-0 Prolene and no further cerebrospinal fluid leakage was observed. Laminectomies were completed from C4 to C7; the bone quality was extremely poor. Posterior lateral mass fixation was undertaken from C3 to T1. Subsequently, the patient underwent spinal cord injury rehabilitation, with improvement in strength, bowel and bladder function at 3 month follow-up. Final pathology was consistent with calcified debris, with no evidence of malignancy.
Figure 1.
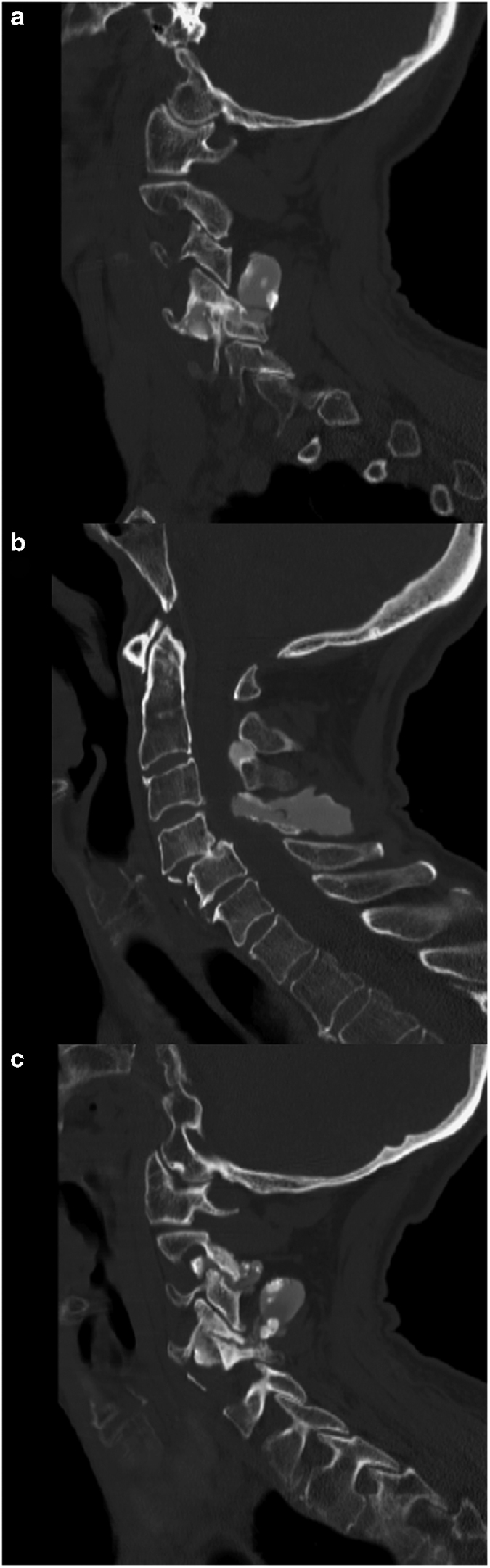
(a) left parasagittal, (b) sagittal and (c) right parasagittal computed tomography images that demonstrate calcinosis involvement of right C2/3 facet and bilateral C3/4 facets, along with C4/5 subluxation.
Figure 2.
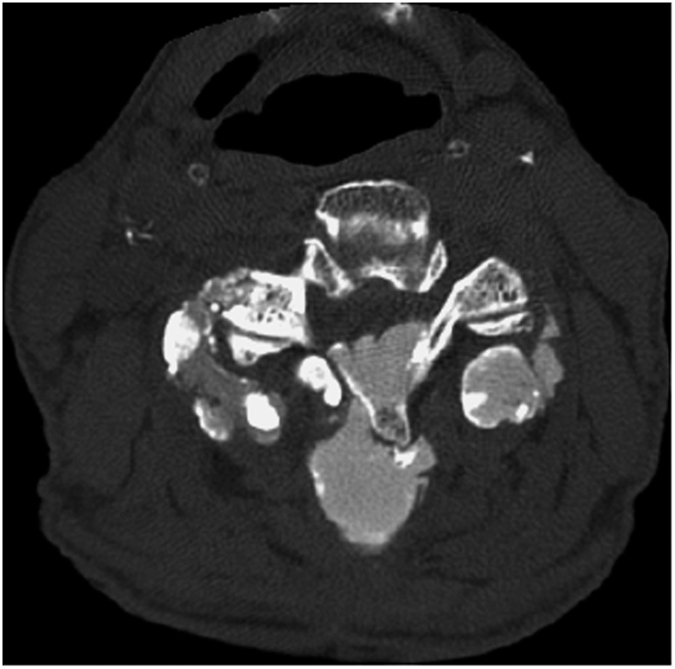
Axial computed tomography cervical spine demonstrates bilateral C3/4 facet calcinosis.
Figure 3.
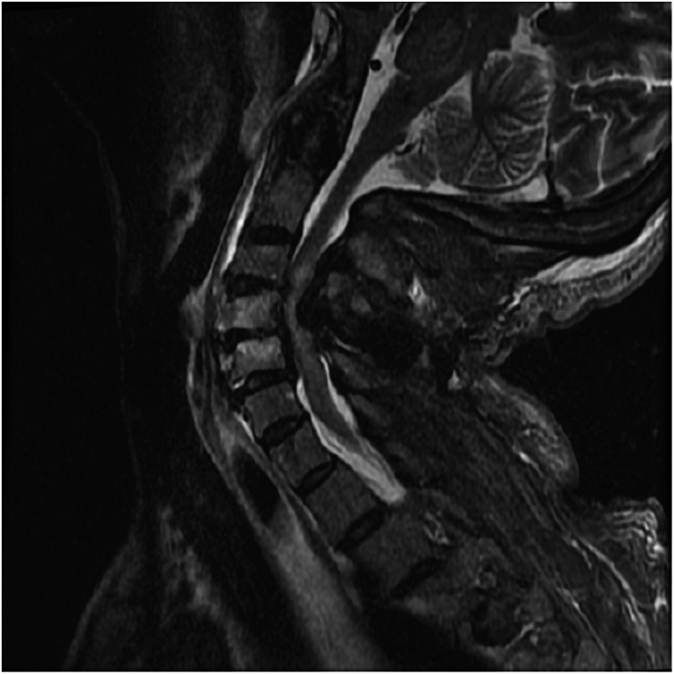
Magnetic resonance imaging T2 cervical spine demonstrates C3–C6 cord edema and stenosis.
For systemic sclerosis, soft tissue calcifications, or calcinosis, frequently involve the fingertips and the synovial joints in hands, knees and elbows.3,5,9 The disorder rarely inflicts the cervical spine; when it does, erosive, paraspinal, calcinosis may develop, which can produce spinal canal stenosis and instability.3–6,10,11 There is an association between anti-centromere antibodies and calcinosis.3,12 The calcinosis is generally dystrophic and is characterized by hydroxyapatite crystals.8 The pathology may be propagated by microvascular insufficiency, inflammation and local tissue damage.5,6,11
Table 1 presents previously reported cases where surgery was also discussed. Initial presentations included occipital headaches, axial neck pain, neck stiffness, cervical radiculopathy and cervical myelopathy.3,4,6,8,11,13 Our patient presented with an acute traumatic central cord syndrome after a hyperextension injury, precipitated by chronic stenosis from her dystrophic calcinosis.
Table 1. Literature review.
| Literature | Age | Gender | Symptoms | Imaging | Treatment | |
|---|---|---|---|---|---|---|
| Arginteanu et al. 3 | 1 | 65 | F | Neck pain, Lhermitte's sign | Calcified mass from occiput to C5 | Posterior occiput-C7 fusion |
| Bracard et al. 10 | 2 | 62 | F | Gait disturbance, pain in shoulders and elbows, | C3/4 subluxation | Surgery, posterior approach, no description of technique |
| Durant et al. 18 | 3 | 48 | M | a | C3/4 calcinosis | Decompression, laminectomy, fusion (unknown levels) |
| Haverbush et al. 11 | 4 | 55 | F | Neck pain, shoulder pain, arm pain | Marked kyphosis at C5/6 | Posterior cervical C1–C7 fusion, halo |
| Lima et al. 6 | 5 | 51 | F | Progressive weakness for months | Medullar compression, C4–T1 PLL calcification | Posterior cervico-thoracic laminectomies (unknown levels) |
| Shoji et al. 19 | 6 | 34 | F | Occipital headaches | Vertical atlanto-axial subluxation | Halo, occipitocervical fusion |
| Smucker et al. 8 | 7 | 60 | M | Progressive neck pain, hand dysfunction, stumbling gait | C2/3 subluxation | Halo, Lateral retropharyngeal approach with C3 corpectomy and anterior fusion followed by C1–C4 posterior onlay fusion |
| 8 | 59 | F | Neck pain | C4/5 destructive lesion | Posterior C3–C7 fusion | |
| 9 | 73 | F | Progressive neck pain, hand motor dysfunction | Multiple levels listhesis | Posterior C2–T2 fusion, Anterior C3–T1 fusion | |
| Present case | 10 | 57 | F | Central cord syndrome | C4/5 subluxation | Posterior C3–T1 fusion |
Abbreviation: PLL, posterior longitudinal ligament.
no data available.
Central cord syndrome is the most frequent form of incomplete spinal cord injury,14,15 where the pathology is directed toward the medial aspect of the lateral corticospinal tract in the cervical spine.15 No prior cases have noted acute spinal cord injury with underlying systemic sclerosis and cervical calcinosis. Central cord syndrome typically occurs in the older population with attendant cervical spondylosis who incur hyperextension injuries. The cervical calcinosis in our patient effectively induced chronic stenosis, not unlike cervical spondylosis, which leads to a lower threshold for central cord syndrome with minor trauma.
Prior surgical management for cervical calcinosis has predominantly employed the posterior approach for decompression, fixation and fusion (Table 1). This approach is appropriate given that much of the pathology is directed at the posterior elements, including the facet joints and the lamina. For significant listhesis, past cases have used cervical traction or halo for cervical reduction before surgical stabilization (Table 1, cases 4, 6, and 7). Circumferential stabilization has also been used in two cases (Table 1, cases 7 and 9); the authors recommended vigilance about dysphagia given underlying esophageal dysmotility with systemic sclerosis. Our patient received laminectomies from C4 to C7, with fixation at C3–T1. The calcinosis was significantly adherent to the dura, where debulking revealed a dural opening. In prior literature, this characteristic of the calcinosis has not been described. Dural erosion has been associated with disc herniation;16,17 a proposed mechanism suggests that chronic adhesions, secondary to chronic inflammation, may lead to rupture of the dura.17 A similar mechanism may be at play in this case, given that systemic sclerosis is a chronic inflammatory disease. The authors emphasize caution during removal of the calcinosis, as durotomies can be a significant complication. Subtotal debulking may be a reasonable mindset if the spinal canal is relaxed after laminectomies.
Dystrophic calcinosis from underlying systemic sclerosis can cause significant chronic cervical stenosis, which may reduce the threshold for acute traumatic cervical cord syndrome under minor trauma. Moreover, dystrophic calcinosis may have a propensity for dural erosion. Aggressive removal of the calcinosis may breach the dura. Consequently, subtotal debulking may be reasonable if the spinal canal is adequately decompressed after laminectomies.
The authors declare no conflict of interest.
References
- Elhai M , Avouac J , Kahan A , Allanore Y . Systemic sclerosis at the crossroad of polyautoimmunity. Autoimmun Rev 2013; 12, pp 1052–1057. [DOI] [PubMed] [Google Scholar]
- Allanore Y , Avouac J , Kahan A . Systemic sclerosis: an update in 2008. Joint Bone Spine 2008; 75, pp 650–655. [DOI] [PubMed] [Google Scholar]
- Arginteanu MS , Perin NI . Paraspinal calcinosis associated with progressive systemic sclerosis. Case report. J Neurosurg 1997; 87, pp 761–763. [DOI] [PubMed] [Google Scholar]
- Schweitzer ME , Cervilla V , Manaster BJ , Gerharter J , Dalinka M , Peck WW et al. Cervical paraspinal calcification in collagen vascular diseases. AJR Am J Roentgenol 1991; 157, pp 523–525. [DOI] [PubMed] [Google Scholar]
- Van de Perre S , Vanhoenacker FM , Op de Beeck B , Gielen JL , De Schepper AM . Paraspinal cervical calcifications associated with scleroderma. JBR-BTR 2003; 86, pp 80–82. [PubMed] [Google Scholar]
- Lima IV , Galrão LA , Maia TS , Santiago MB . Spinal cord compression by ectopic calcinosis in scleroderma. Clin Exp Rheumatol 2005; 23, pp 704–706. [PubMed] [Google Scholar]
- Ward M , Curé J , Schabel S , Smith EA , Schumacher HR Jr , Silver RM . Symptomatic spinal calcinosis in systemic sclerosis (scleroderma). Arthritis Rheum 1997; 40, pp 1892–1895. [DOI] [PubMed] [Google Scholar]
- Smucker JD , Heller JG , Bohlman HH , Whitesides TE Jr . Surgical treatment of destructive calcific lesions of the cervical spine in scleroderma: case series and review of the literature. Spine (Phila Pa 1976) 2006; 31, pp. 2002–2008. [DOI] [PubMed] [Google Scholar]
- Bassett LW , Blocka KL , Furst DE , Clements PJ , Gold RH . Skeletal findings in progressive systemic sclerosis (scleroderma). AJR Am J Roentgenol 1981; 136, pp 1121–1126. [DOI] [PubMed] [Google Scholar]
- Bracard S , Thomas E , Braun M , Renard M , Picard L . Cervical cord compression in scleroderma. One case. J Neuroradiol 1991; 18, pp 12–17. [PubMed] [Google Scholar]
- Haverbush TJ , Wilde AH , Hawk WA Jr , Scherbel AL . Osteolysis of the ribs and cervical spine in progressive systemic sclerosis (scleroderma). A case report. J Bone Joint Surg Am 1974; 56, pp 637–640. [PubMed] [Google Scholar]
- Nishikai M , Itoh K , Sato A . Calcinosis and the anticentromere antibody: its clinical, radiological and immunogenetic aspects. Br J Rheumatol 1992; 31, pp 9–12. [DOI] [PubMed] [Google Scholar]
- Teng AL , Robbin MR , Furey CG , Easley SE , Abdul-Karim FW , Bohlman HH . Tumoral calcinosis in the cervical spine in a patient with CREST syndrome. A case report. J Bone Joint Surg Am 2006; 88, pp 193–197. [DOI] [PubMed] [Google Scholar]
- McKinley W , Santos K , Meade M , Brooke K . Incidence and outcomes of spinal cord injury clinical syndromes. J Spinal Cord Med 2007; 30, pp 215–224. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Brodell DW , Jain A , Elfar JC , Mesfin A . National trends in the management of central cord syndrome: an analysis of 16 134 patients. Spine J 2015; 15, pp 435–442. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Floeth F , Herdmann J . Chronic dura erosion and intradural lumbar disc herniation: CT and MR imaging and intraoperative photographs of a transdural sequestrectomy. Eur Spine J 2012; 21 Suppl. 4, pp S453–S457. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Choi JY , Lee WS , Sung KH . Intradural lumbar disc herniation--is it predictable preoperatively? A report of two cases. Spine J 2007; 7, pp 111–117. [DOI] [PubMed] [Google Scholar]
- Durant DM , Riley LH 3rd , Burger PC , McCarthy EF . Tumoral calcinosis of the spine: a study of 21 cases. Spine (Phila Pa 1976) 2001; 26, pp. 1673–1679. [DOI] [PubMed] [Google Scholar]
- Shoji A , Tahara K , Hayashi H , Tsuji S , Kimura E , Yamamoto K et al. Severe headache complicated by vertical atlantoaxial subluxation in diffuse systemic sclerosis with crowned dens pattern calcification. Rheumatol Int 2011; 31, pp 1247–1250. [DOI] [PubMed] [Google Scholar]


