Abstract
Study design:
A retrospective study was performed.
Objectives:
To analyze the outcome of two neglected sacral fractures who presented late to us after 6 weeks of injury with main complaints of incontinence and numbness in sacral region. There are no guidelines for management of complex fractures of sacrum who present late, and available literature is equally perplexing.
Methods:
Patients were evaluated and radiological investigations were done. Anterior-displaced U-shaped fracture was found to be present between S2 and S3 with bony fragments encroaching the canal. Decompression with wide sacral laminectomies was done without any fixation.
Results:
Case 1 showed complete recovery of bladder and perineal sensations 6 months post surgery. Second patient (case 2) had partial recovery of bladder control but numbness persisted till last follow-up at 6 months.
Conclusion:
Neglected fractures of sacrum that present later than 6 weeks post injury with cauda equina syndrome could be given a chance for decompression if imaging shows canal encroachment with bony fragments. Fixation of fracture may not be required in all unstable sacral fractures after 6 weeks.
Subject terms: Surgery, Physiology
Introduction
Sacrum is relatively protected from injuries because of being placed deep in the pelvic ring. Injuries to sacrum can be missed frequently owing to difficulty in imaging this region. Sacral fractures are frequently associated with polytrauma, which also increases the chance of them being missed by an unwary physician. Around 30% of sacral injuries are missed in the initial diagnosis.1 Management of sacral fractures with neurological deficit has been controversial. Treatment with either operative or nonoperative approach, neurological recovery rate up to 80% has been reported in literature.2 In modern world with easy to access healthcare it is rare to find neglected injuries. This also translates to less-available literature. There are no guidelines on management of neglected sacral fractures to the best of author’s knowledge.
Materials and methods
Case 1
A 36-year-old lady presented to us in outpatient department 45 days after injury due to fall from height with pain and numbness in sacral region. Patient was on bed rest for the last 45 days and had taken symptomatic treatment for pain relief. She complained of saddle anesthesia with incontinence of bladder and bowel. Perianal sensation was absent and voluntary anal contraction was weak. There was no motor deficit. X-rays, computed tomography scan and magnetic resonance imaging were done, which showed anteriorly displaced fracture between S2 and S3 with vertical extensions (U-shaped fracture; Figures 1, 2, 3) and canal encroachment with bony fragments. Patient was operated and multiple wide sacral laminectomies of S2 S3 were done. Left S3, S4 sacral nerve roots were found to be contused but continuity of nerve roots was maintained (Figure 4). Intraoperative there was no mobility at fracture site and fracture fragments were found to be united. No fixation for fracture was done. Patient was mobilized immediately post surgery. Patient improved and recovered her sphincter control and sensations completely 6 months after surgery.
Figure 1.

Showing X-ray sacrum lateral view showing fracture sacrum (Case 1).
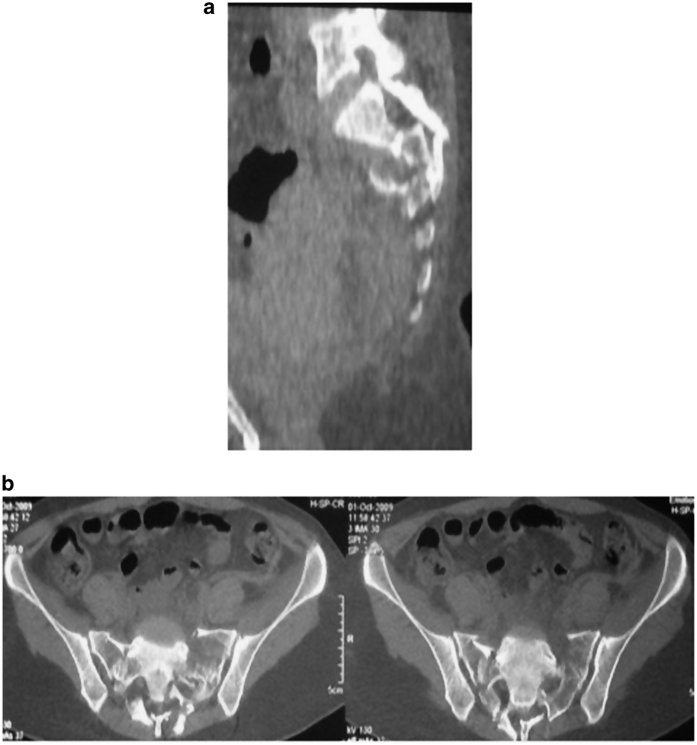
Figure 2.
(a, b) Showing CT scan of the fracture (Case 1).
Figure 3.
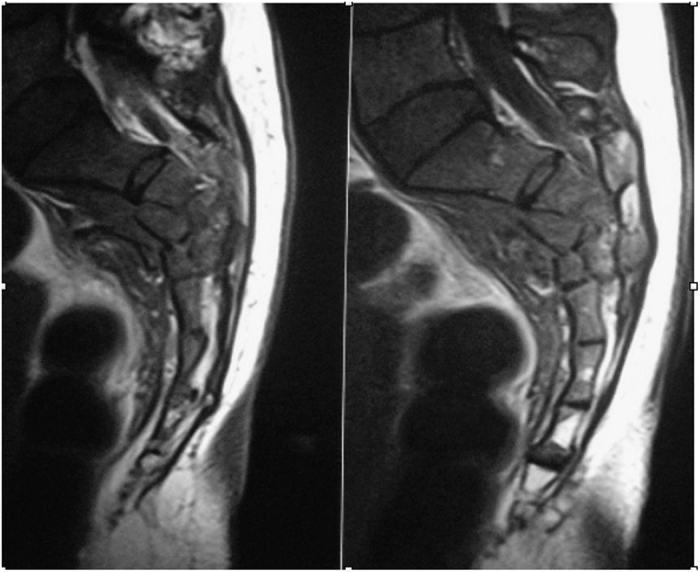
MRI showing sacral fracture (Case 1).
Figure 4.
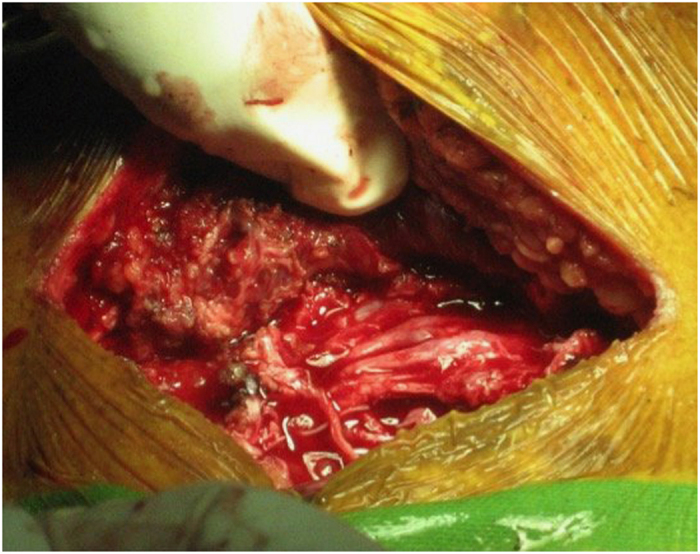
Intraoperative picture showing sacral nerve roots continuity after decompression (Case 1).
Case 2
A 64-year-old lady presented to us with complaint of pain in sacral region and incontinence of bladder for last 6 weeks. She had a history of fall on buttocks, following which she was on bed rest for 3 weeks. Radiological investigations in the form of X-rays were done at a primary health center where she was diagnosed as spondylolisthesis L5S1 with cauda equina syndrome and was advised surgery for the same. After 6 weeks of injury she reported to us where a magnetic resonance imaging and computed tomography scan of sacrum was done, which suggested sacral fracture through S2S3 with vertical extensions (Figures 5 and 6), which suggested the sacral fracture to be the cause for cauda equina symptoms that was missed initially. Patient was operated by sacral laminectomies of S2 and S3. Left S3 root was found to be lacerated intraoperatively. Patient was mobilized after surgery.
Figure 5.
Showing X-ray sacrum lateral view showing fracture sacrum with spondylolisthesis (Case 2).
Figure 6.
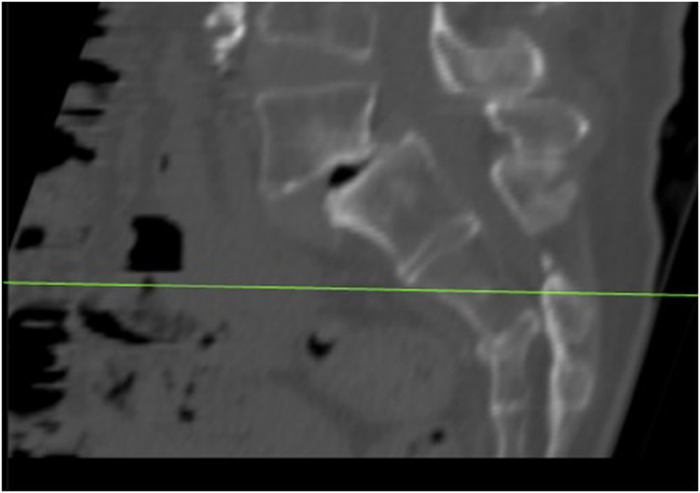
Showing CT scan of the fracture (Case 2).
Results
Case 1 patient showed complete recovery of her bladder control and also had complete recovery of her sensations in perineal region.
Case 2 patient had recovered her bladder partially after 6 months but urge incontinence still persisted. She had discontinued clean intermittent catheterization (CIC) but numbness in perineal region still persisted.
Discussion
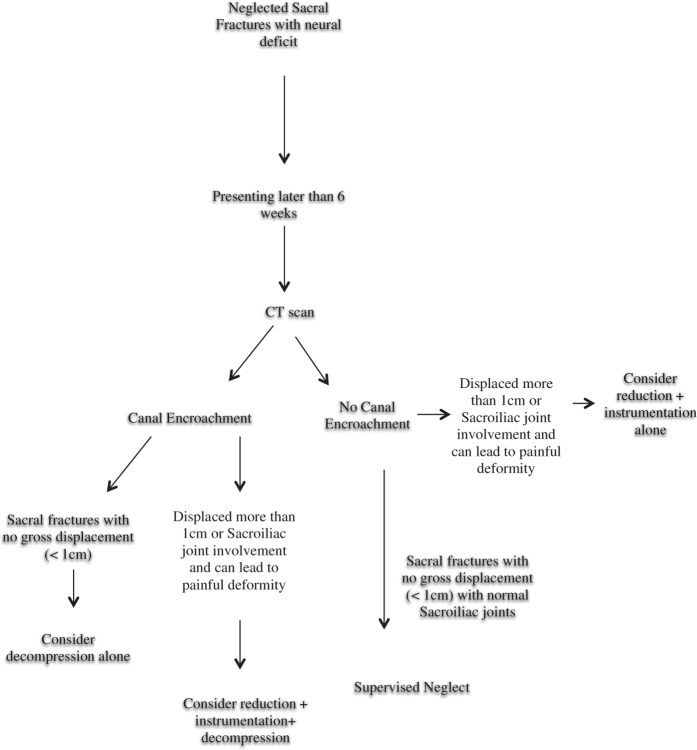
Schmidek et al.3 had classified transverse sacral fractures into low and high types depending on location of fracture in sacrum. High fractures usually occur at S1–S2 region and are due to fall from height on extended knee and flexed hips. Low sacral fractures are rare, occur from S3 to S5 and are caused owing to fall on buttocks. Our both cases had transverse fracture below S2 with vertical extensions and were so classified into low fractures category. Neglected spinal injuries are unusual in today’s modern health era. These injuries may result in serious medical and medico-legal problems. Sengupta4 defined neglected spinal injuries as those, which are not treated in timely fashion and are found late when options are limited. Rajasekaran et al.5 emphasized that in western world neglected spinal injuries are those, which are usually missed at initial presentation, whereas in developing countries late presentation with or without adequate treatment may also be a reason for neglected injuries. In our case 1 the reason of neglect was late presentation of patient to hospital, whereas in second case neglect was on the part of treating physician where spondylolisthesis was presumed to be cause of incontinence and sacral fracture was completely missed. Sacral fractures are commonly associated with multiple injuries, which is one of the main reasons for their neglect. Pohlemann et al.6 reported in a series of 377 patients with sacral fractures; 89.4% had at least one more injury. Sacral injuries can result in neurological injuries ranging from monoradiculopathies to cauda equina syndrome. Surgical indications and timing of surgery are controversial considering that 80% of patients will recover neurologically with either operative or nonoperative approach. Gibbons et al.7 reported neurological improvement in 11 of 15 patients treated nonoperatively compared with 7 of 8 patients managed surgically. Denis et al.8 reported no improvement of bowel or bladder control in three patients treated nonoperatively, whereas all five patients treated surgically had complete return of bladder and bowel control. Sabiston et al.9 recommended nonoperative care in all patients with a sacral fracture and found no recovery of bladder and bowel only in one patient. Neurological deficit in sacral fractures can be because of root contusion, laceration and stretching. It is difficult to predict whether neurological recovery will occur after decompression or not but most scholars agree that chances of recovery are more with contused roots rather than lacerated or torn rootlets. Unfortunately it is difficult to predict preoperatively whether the roots are contused or lacerated. Neurological decompression should preferably be performed early within first 24–72 h following injury.10 However, there is no literature, which suggests up to what time after injury there is a chance for neurological recovery in sacral fracture. Literature available suggests recovery of cauda equina in patients with prolapsed intervertebral disc (PIVD) when surgery is done within 48 h but whether the same can be applied in cases with sacral fractures is debatable. In our cases neurological recovery occurred complete in first case and partial in the second one. In cauda equina owing to disc prolapse chemical as well as mechanical components both may be responsible for neurological compromise. In neglected sacral fractures role of any other factor than mechanical compression is not clear. Therefore, contemplating results of timing of cauda equina syndrome due to disc propalse may not hold well for the patients with sacral fractures. Early surgery can be associated with better chances of neurological recovery but with more chances of further soft tissue injury and infection. Late surgery can have limited prospect for neurological recovery but is debatable. Authors advise decompression alone in undisplaced sacral fractures for neglected sacral fractures with cauda equina syndrome if there is any canal encroachment seen on computed tomography or magnetic resonance imaging. In patients with displacement >1 cm and potential for painful sacral deformity with canal encroachment authors advise open reduction and fixation along with decompression. In cases with no canal encroachment with neurological deficit, cause is nerve roots avulsion or stretch leading to neurological deficit. In this scenario conservative approach is probably the preferred modality in stable minimal displaced fractures (<1 cm). Stand-alone laminectomies of sacral fracture are rarely done in acute fractures of sacrum. Average healing time for sacral fracture is 6–8 weeks. In neglected fractures of sacrum when patient presents later than 6 weeks, fracture is usually sticky and uniting. So authors decided against fixation of fracture in these cases. Author suggests that the surgical treatment option should be tailored to the individual fracture pattern, patients’ symptoms, timing of presentation after fracture, radiological compression as evident on imaging, associated injuries and the surgeons' expertize (Figure 7).
Figure 7.
Showing flowchart of treatment in neglected sacral fractures.
Conclusion
Authors suggest operative treatment using decompression and sacral laminectomies to attain maximum neurological improvement and favorable clinical outcome with cauda equina in neglected low sacral fractures with canal encroachment on imaging. Fixation of fracture may not be required in unstable sacral fractures after 6 weeks.
Data archiving
There were no data to deposit.
Acknowledgments
We would like to acknowledge Ms Meenakshi for her contribution in preparation of Manuscript.
The authors declare no conflict of interest.
References
- Routt ML Jr , Simonian PT , Swiontkowski MF . Stabilization of pelvic ring disruptions. Orthop Clin North Am 1997; 28: 369–388. [DOI] [PubMed] [Google Scholar]
- Vaccaro AR , Kim DH , Brodke DS , Harris M , Chapman JR , Schildhauer T et al. Diagnosis and management of sacral spine fractures. Instr Course Lect 2004; 53: 375–385. [PubMed] [Google Scholar]
- Schmidek HH , Smith DA , Kristiansen TK . Sacral fractures. Neurosurgery 1984; 15: 735–746. [DOI] [PubMed] [Google Scholar]
- Sengupta DK . Neglected spinal injuries. Clin Orthop Relat Res 2005; 431: 93–103. [DOI] [PubMed] [Google Scholar]
- Rajasekaran S , Kamath V , Basu S , Gupta S . Neglected spinal trauma. In: Jain AK , Kumar S (eds). Neglected Musculoskeletal Injuries. 1st edn, Jaypee Brother Medical Publisher: Delhi, 2011, 142–159. [Google Scholar]
- Pohlemann T , Gänsslen A , Tscherne H . [The problem of the sacrum fracture. Clinical analysis of 377 cases]. Orthopade 1992; 21: 400–412. [PubMed] [Google Scholar]
- Gibbons JK , Soloniuk DS , Razack N . Neurological injury and pattern of sacral fractures. J Neurosurg 1990; 72: 889–893. [DOI] [PubMed] [Google Scholar]
- Denis F , Davis S , Comfort T . Sacral fractures: an important problem. Retrospective analysis of 236 cases. Clin Orthop Relat Res 1988; 227: 67–81. [PubMed] [Google Scholar]
- Sabiston CP , Wing PC . Classification and neurologic implications. J Trauma 1986; 26: 1113–1115. [DOI] [PubMed] [Google Scholar]
- Mehta S . Sacral fractures. J Am Acad Orthop Surg 2006; 14: 656–665. [DOI] [PubMed] [Google Scholar]