Summary
Aim
To assess attitudes and beliefs towards benign prostatic hyperplasia (BPH)/ lower urinary tract symptoms (LUTS) and its treatment among patients and physicians in Latin America, Asia Pacific and the Commonwealth of Independent States (CIS).
Methods
Cross‐sectional, quantitative study conducted between December 2014 and September 2015. Separate questionnaires were administered to BPH/LUTS patients receiving drug treatment for their condition and to practising physicians who treat patients with BPH/LUTS.
Results
In total, 1094 patients and 202 physicians completed a questionnaire. Most patients (61%) felt very/fairly well informed about BPH/LUTS, and 60% of physicians perceived patients to be very/somewhat informed. Overall, 70% of physicians felt that it would be valuable to raise awareness of BPH/LUTS and encourage men to consult a physician. The first symptoms most commonly noticed by patients were need to urinate more frequently, slower/weaker stream and nocturia. At first consultation, 71% of patients recalled providing a urine sample, 57% having a blood test for prostate‐specific antigen and 56% a digital rectal examination being performed. Over two thirds of patients (69%) were satisfied with their current medication; highest satisfaction rates (among both patients and physicians) were reported for alpha blockers and 5ARIs, either as monotherapies or used in combination. Patients were prepared to wait longer for symptom relief in order to have a reduced risk of surgery. Most physicians (90%) thought that at least some patients believe BPH/LUTS to be a progressive condition. Most physicians thought that patients were very/fairly concerned about BPH surgery (92%) and acute urinary retention (72%); 52% of physicians thought treatment adherence was “extremely” important.
Conclusions
This study provides valuable insights into the attitudes and beliefs of patients and physicians in Asia Pacific, Latin America and CIS about BPH/LUTS and its management. It also highlights areas of discordance between patient/physician perceptions and beliefs about BPH/LUTS, and potential areas of focus to improve the experience of affected patients.
What's known
It is now recognised that patients have an important role in clinical decision making, and that it is important to take account of patient perceptions and preferences when choosing the most appropriate treatment.
Surveys in the United States and Europe have demonstrated significant differences in the beliefs and attitudes of patients and physicians towards BPH/LUTS, both in terms of the condition itself and its management.
What's new
This survey provides information on the views and beliefs of patients and physicians in Latin America, Asia Pacific and the Commonwealth of Independent States towards BPH/LUTS and its management.
This study confirms and extends the findings from the United States and Europe, and highlights important areas of discordance between patients’ and physicians’ perceptions and beliefs about BPH/LUTS, and potential areas of focus to improve the experience of affected patients.
1. Introduction
Benign prostatic hyperplasia (BPH) is common among older men, with 612 million cases predicted to occur by 2018.1, 2 Histologically, BPH is defined as the presence of stromal‐glandular hyperplasia within the prostate gland.3 Many patients with BPH present with bothersome lower urinary tract symptoms (LUTS), typically an increase in urinary urgency and frequency, nocturia, decreased and intermittent force of stream and a sense of incomplete bladder emptying3; these symptoms can have a substantial negative impact on quality of life (QoL).4 BPH/LUTS is a progressive condition that can lead to serious long‐term complications such as acute urinary retention (AUR) and BPH‐related surgery,5 and is associated with a considerable economic burden.6, 7, 8
Medical, rather than surgical, therapy is the main treatment option for most men who suffer from LUTS as a result of BPH.1 Several different classes of pharmacotherapy are now available; these include antimuscarinics and phosphodiesterase‐5 inhibitors, and longer‐established agents such as alpha blockers and 5‐alpha reductase inhibitors (5ARIs). Adherence to medical therapy for BPH/LUTS is associated with better clinical outcomes, however, several studies indicate that adherence rates are low and may vary according to the class of drug(s) used.9, 10, 11
Surveys conducted in the United States and Europe (PROBE) have demonstrated discrepancies between patients and physicians in their attitudes and beliefs towards BPH/LUTS and its treatment,12, 13 but there is limited knowledge of attitudes and beliefs among patients and physicians in other regions. Here, we report findings from the Prostate Research on Behaviour and Education (PROBE) II survey conducted in countries across Asia Pacific, Latin America and the Commonwealth of Independent States (CIS). The aims of this study were to explore attitudes of patients and physicians towards BPH, and investigate patient adherence with current BPH treatment.
2. Methods
PROBE II was a cross‐sectional, multinational, quantitative study conducted between December 2014 and September 2015 in 14 countries across Asia Pacific, Latin America, and the CIS: Argentina, Australia, China, Colombia, Indonesia, Japan, Kazakhstan, Malaysia, Mexico, Peru, Philippines, Russia, Ukraine and Venezuela. The survey consisted of two questionnaires that were structured in a similar way to those used in the first PROBE study, which assessed practices in Europe13: one for patients with BPH who were receiving drug treatment for their condition, and the second for practising physicians (urologists/general practitioners [GPs]).
The primary objectives of the survey were to explore and identify patient and healthcare provider (HCP) attitudes to BPH and to explore understanding of the BPH condition and treatment across Asia Pacific, Latin America and the CIS. Secondary objectives were to: identify the health‐seeking behaviour and treatment preferences of BPH patients; examine the role of physicians in diagnosing and managing BPH and factors driving prescribing; highlight attitudes towards the symptoms and complications of BPH among patients and physicians; assess current medication adherence and any differences in adherence between patients with different treatment options.
The sample size for each geographical region or country was based on several factors, including the relative size of each population, experience of conducting research with physicians and patients in the selected territories and comparison with the first PROBE study.13 For the patient sample, the target sample size also took account of the relative size of the predicted male population aged ≥50 years for 2014 published by the US Census Bureau (in the absence of epidemiological data for BPH in the territories to be included).
For data analysis, China, Japan and Australia were separated from the other Asia Pacific countries (hereafter referred to as APAC Other) because of significant differences in their health system structures, demographics and population size, in order to avoid data from this region being dominated by these large or characteristically different countries.
The protocol and questionnaires were approved by an ethics committee or Institutional Review Board for each market before subjects could participate in the study. All participants were required to sign an informed consent form before being given the questionnaire.
2.1. Patient questionnaire
Eligible patients were men aged 45–80 years who had the following: a self‐reported previous diagnosis of BPH, “enlarged prostate” or “prostate problems”; a self‐reported consultation with a physician for BPH, “enlarged prostate” or “prostate problems” during the last 12 months; and known current use of prescription medication for BPH, “enlarged prostate” or “prostate problems”. To ensure dutasteride users were not over‐ or underrepresented, recruitment of patients into the survey was quota controlled to reflect the market share of dutasteride in each country (data on dutasteride were provided by GlaxoSmithKline).
Data were collected using a paper questionnaire aided by a trained interviewer in most countries; computer‐assisted telephone interviewing (CATI) and online surveys were used in some countries (e.g. where respondents were more responsive to talking about the topic via telephone/online link). Questionnaires were made as country specific as possible, not only through appropriate language of the surveys but also by use of relevant treatments that were listed. Key questions asked of patients included: perception of how well informed they feel about health issues related to prostate problems/BPH; timing of first treatment from diagnosis and perceived reasons for being given that treatment; length of time on current treatment and dosing regimen; extent of patient agreement with a range of statements relating to perceived severity, general public understanding and impact of BPH on their life. The 8‐item version of Morisky Medication Adherence Scale (MMAS)14 was used for assessment of patient medication adherence (low adherence, score of 0 to <6; medium adherence, score of 6 to <8; high adherence, score of 8). The International Prostate Symptom Score was used to assess current prostate symptom score and associated QoL.
2.2. Physician questionnaire
Physicians eligible for inclusion were urologists (or GPs in Australia) who had been practising for more than 3 years but less than 31 years, and who have consultations with at least five patients per month presenting for the first time with symptomatic BPH. Physicians were excluded from participation if they had recently (within the last 3 months) participated in any market or clinical research study in prostate health, or if they (or a family member) had an existing paid affiliation with a healthcare or pharmaceutical organisation as a consultant or clinical researcher.
Physicians participated mostly via an online questionnaire; paper or CATI questionnaires could be utilised, depending on physician preference. Key questions asked of physicians included: perception of reasons why some men with BPH symptoms delay consulting their physician; perception of reasons why men with BPH symptoms visit their physicians (“triggers”); perception of awareness of BPH among male patients and level of importance of raising awareness; belief in progression of BPH and perception of patients’ belief in BPH progression.
3. Results
A total of 1094 patients and 202 physicians met the inclusion criteria and completed a questionnaire. The number of participants from each country in the study is shown in Table 1.
Table 1.
Patient and physician sample size from countries participating in the PROBE II survey
| Region | Country | Patient sample size (n) N=1094 | Physician sample size (n) N=203 |
|---|---|---|---|
| Asia Pacific | Australia | 109 | 36 |
| China | 214 | 47 | |
| Indonesia | 114 | 5 | |
| Japan | 200 | 30 | |
| Malaysia | 18 | 5 | |
| Philippines | 41 | 8 | |
| Latin America | Argentina | 43 | 12 |
| Columbia | 33 | 4 | |
| Mexico | 81 | 10 | |
| Peru | 22 | 4 | |
| Venezuela | 20 | 7 | |
| Commonwealth of Independent States | Kazakhstan | 11 | 2 |
| Russia | 140 | 25 | |
| Ukraine | 48 | 8 |
3.1. General awareness of BPH
The proportion of patients who felt that they were “very well” or “fairly well” informed about health issues related to BPH was 61%, whereas just under one fifth (19%) felt “not very well” or “not at all” informed (Table 2A). Among physicians, 60% perceived their patients to be “very” or “somewhat informed” about BPH, whereas almost two fifths (39%) believed their patients were “not very informed” about BPH (Table 2B). Variation was observed among countries/regions, among both patients and physicians. Patients in the CIS were the least likely, and those in Australia most likely, to feel adequately informed about BPH. Among physicians, those in the CIS and APAC Other regions were most likely to feel that their patients were poorly informed.
Table 2.
General awareness of BPH (A) level to which patients felt informed about BPH and (B) level to which physicians feel their patients are informed about BPH (data expressed as % of respondents)
| (A) | |||||
|---|---|---|---|---|---|
| Very/fairly well informed | Neither informed nor uninformed | Not very wellinformed | Not at allinformed | Don't know | |
| All countries | 61 | 19 | 17 | 2 | 0.2 |
| APAC Other | 69 | 8 | 13 | 10 | 0 |
| China | 71 | 19 | 10 | 0 | 0 |
| Australia | 77 | 10 | 9 | 4 | 0 |
| Japan | 63 | 13 | 24 | 1 | 0 |
| CIS | 40 | 33 | 25 | 2 | 1 |
| Latin America | 55 | 28 | 16 | 1 | 0 |
| (B) | ||||
|---|---|---|---|---|
| Very informed | Somewhat informed | Not very informed | Most have never heard of it | |
| All countries | 12 | 48 | 39 | 0 |
| APAC Other | 11 | 39 | 50 | 0 |
| China | 26 | 43 | 32 | 0 |
| Australia | 8 | 53 | 36 | 3 |
| Japan | 23 | 43 | 33 | 0 |
| CIS | 3 | 43 | 54 | 0 |
| Latin America | 0 | 62 | 38 | 0 |
APAC, Asia Pacific; BPH, benign prostatic hyperplasia; CIS, Commonwealth of Independent States.
3.2. Presenting symptoms of BPH
The majority of patients (60%) reported that their condition was discovered through reporting of symptoms rather than routine examination by a HCP (39%). The first symptoms of BPH most commonly noticed by patients were the need to urinate more frequently, a slower or weaker urinary stream and getting up at night to urinate (Fig. 1); urgent need to urinate was commonly noticed by patients from China. On noticing symptoms, over two thirds of patients (69%) visited the doctor first, 15% first searched the Internet for information, 5% first went to a pharmacist for advice and 5% first went to a pharmacist for a non‐prescription drug. Patients in China and APAC Other countries were the most likely to have gone straight to a doctor on first noticing symptoms (82% and 80%, respectively). On average, patients waited 3 weeks after first noticing symptoms before seeking the advice of a doctor. The main reason given by patients for waiting was to see if the condition would go away on its own (61%), although nearly one in five men (18%) admitted feeling embarrassed talking about the condition. On first noticing symptoms, 40% of patients had first visited a hospital‐based urologist, 29% had first visited their family doctor or GP and 22% had visited an office‐based urologist. There was considerable regional variation in this pattern (e.g. 98% of patients in China visited a hospital‐based urologist and 1% a family doctor/GP, whereas 1% of Australian patients visited a hospital‐based urologists and 98% a family doctor/GP), largely reflecting different regional health service structures.
Figure 1.
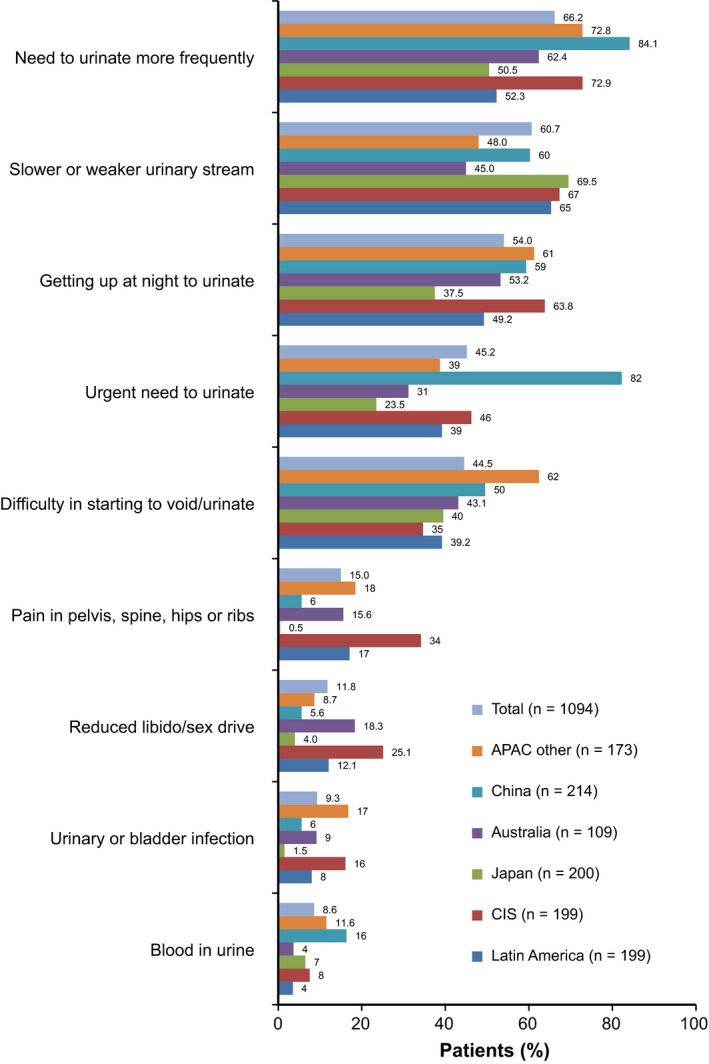
First symptoms of BPH most commonly noticed by patients. Responses of <3% of total group received for the following categories (data not shown): dribbling after urination, stinging/painful urination, high PSA level, burning sensation while urinating, routine exam/tests, other, none/nothing, decline to answer/no answer. APAC, Asia Pacific; BPH, benign prostatic hyperplasia; CIS, Commonwealth of Independent States; PSA prostate‐specific antigen
When physicians were asked why they thought men with urinary symptoms avoided or delayed visiting a physician, just over half (55%) thought it was because men believed it was an inevitable part of ageing. A further 12% thought the main reason was because patients did not like visiting physicians, and a similar proportion (12%) thought the reason was fear of surgery. On average, physicians estimated that half of men with BPH symptoms consulted a HCP about these, with some regional variation evident (Australia, 38%; Latin America 60%).
3.3. Healthcare‐seeking behaviour
Two thirds of patients (66%) first noticed symptoms of BPH between the ages of 51 and 70 years, with just over one quarter (27%) first noticing symptoms between 36 and 50 years (Table 3A). Approximately half of physicians (51%) stated that men were usually in their sixties when they first presented with symptomatic BPH (Table 3B), with little regional variation observed in responses.
Table 3.
Age at which patients first noticed BPH symptoms (A) and physicians report of the average age at which men first presented with symptomatic BPH (B) (data expressed as % of respondents)
| (A) | ||||
|---|---|---|---|---|
| <35 years | 36–50 years | 51–70 years | >71 years | |
| All countries | 0.4 | 27 | 66 | 7 |
| APAC Other | 0 | 5 | 73 | 22 |
| China | 0 | 39 | 58 | 2 |
| Australia | 0 | 31 | 63 | 6 |
| Japan | 0 | 11 | 82 | 7 |
| CIS | 2 | 41 | 54 | 4 |
| Latin America | 1 | 32 | 66 | 2 |
| (B) | |||||
|---|---|---|---|---|---|
| 30–39 years | 40–49 years | 50–59 years | 60–69 years | 70–79 years | |
| All countries | 0.5 | 2 | 35 | 51 | 10 |
| APAC Other | 0 | 0 | 44 | 56 | 0 |
| China | 2 | 9 | 28 | 47 | 15 |
| Australia | 0 | 0 | 36 | 56 | 8 |
| Japan | 0 | 0 | 10 | 53 | 37 |
| CIS | 0 | 3 | 46 | 51 | 0 |
| Latin America | 0 | 0 | 51 | 49 | 0 |
APAC, Asia Pacific; BPH, benign prostatic hyperplasia; CIS, Commonwealth of Independent States.
The majority of patients surveyed (80%) had spoken to a specialist doctor about their BPH or prostate problems, and over half (56%) had spoken to their spouses/partners. Patients from the CIS region (96%) were most likely to have consulted a specialist doctor, whereas patients from APAC Other countries were the most likely to have consulted Internet chat groups, social or church groups or telephone help lines (23%, 32% and 29%, respectively). Patients generally viewed specialist doctors as being more helpful than family doctors, and just under half of patients (45%) deemed their spouse/partner to be extremely or very helpful, although large regional variations were observed. Approximately half of patients (51%) had consulted the Internet about their BPH‐related problems, 48% had looked at leaflets from a healthcare professional, and approximately one third had consulted magazines or newspapers (35%), the television (33%) and books (31%). Almost two thirds of men (61%) who had sourced information about BPH on the Internet found this helpful, whereas only a third of men who had found information about BPH on the television/radio or in newspapers/magazines deemed it useful.
Overall, 70% of physicians thought it would be very valuable to raise awareness of BPH and to encourage men to consult a physician. However, this varied considerably across the different regions, with physicians in APAC Other and Latin America much more likely to think raising awareness would be very valuable (94% and 97% of physicians, respectively) than those in Japan, China and Australia (21%, 64% and 61%, respectively).
3.4. Severity of BPH symptoms and impact on QoL
Patient ratings of the severity of various symptoms of BPH when first experienced are shown in Fig. 2A, and physician ratings of these symptoms at a patient's first visit for BPH are shown in Fig. 2B. For most symptoms, at least 20% of patients rated them as severe; the exceptions were slower/weaker stream and blood in urine. Approximately one quarter of patients stated that many of the symptoms of BPH had a major impact on their QoL. Generally, physicians were less likely than patients to rate a symptom as severe, although almost 40% rated nocturia as severe.
Figure 2.
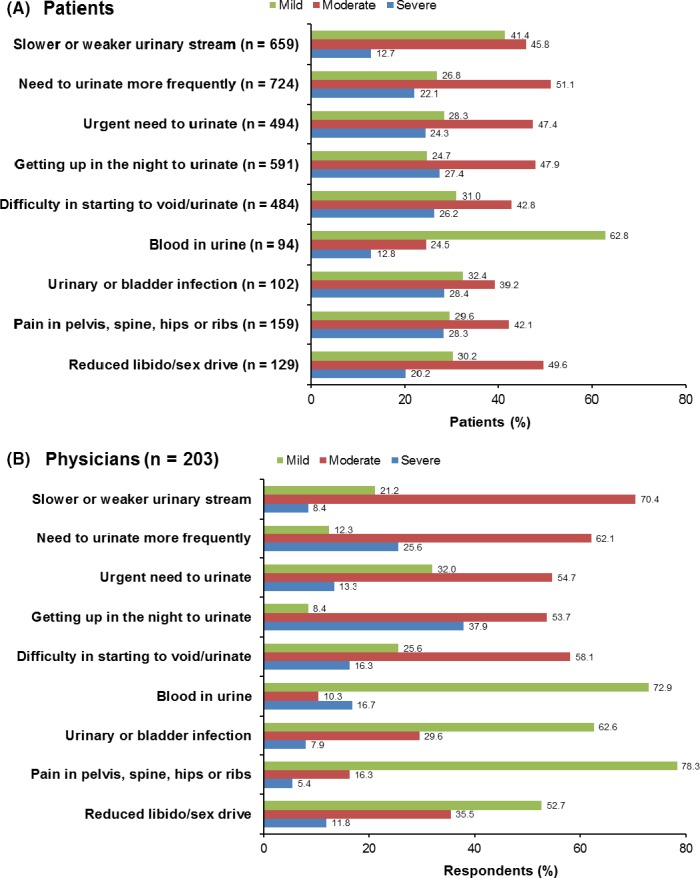
Patients (A) and physicians (B) ratings of severity of BPH symptoms at first presentation. BPH, benign prostatic hyperplasia
3.5. Main concerns about initial symptoms of BPH
Among patients whose BPH or prostate problem had been discovered during an examination by a doctor, the most common concern mentioned was discomfort (48%), followed by disturbed or interrupted sleep (44%) and the fear that it might be cancer (31%) (Fig. 3). Patients in APAC Other countries were more likely than those from other regions to mention concerns about discomfort and interrupted sleep, whereas fear of cancer was most common among patients in Japan, Australia and Latin America. Patients from China and the CIS region were the most likely to have reported frustration with their symptoms.
Figure 3.
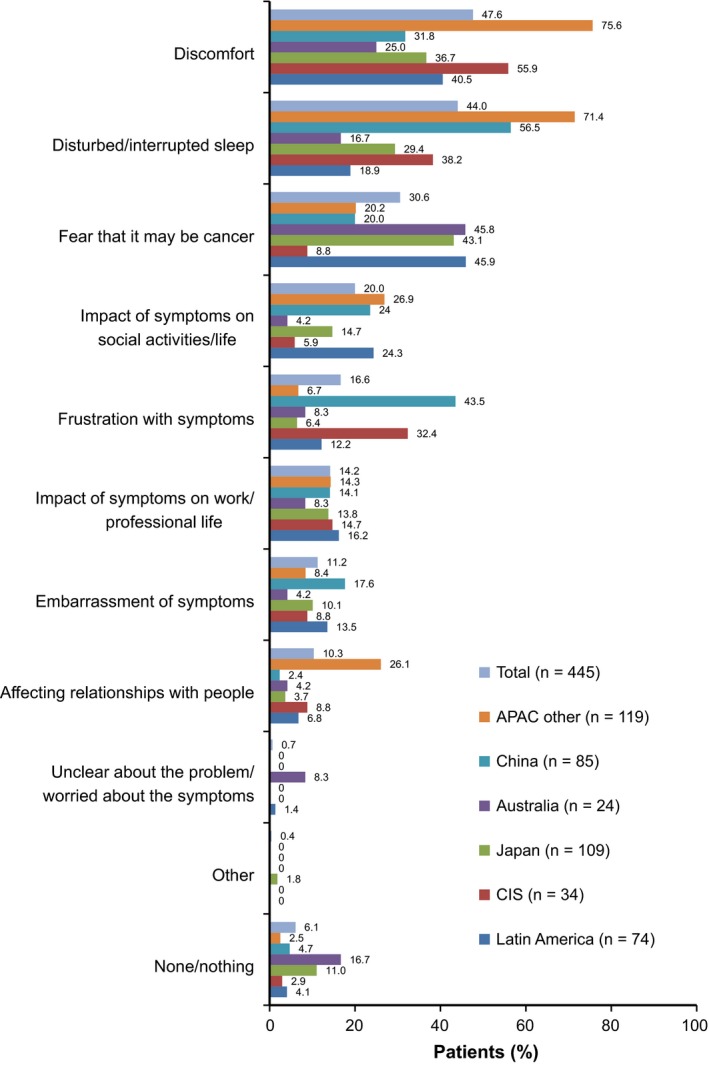
Main patient concerns about initial symptoms of BPH. APAC, Asia Pacific; BPH, benign prostatic hyperplasia; CIS, Commonwealth of Independent States
Among patients who had noticed their symptoms themselves, the main concerns at the time they first visited a doctor were discomfort (51%), followed by disturbed or interrupted sleep (45%) and frustration with symptoms (31%). Patients in China were less likely than others to have been concerned about discomfort, whereas those from Australia, China and the CIS region were more likely than others to have been concerned about embarrassing symptoms and the impact of symptoms on their social life.
About half of physicians surveyed (49%) believed “bother from irritating symptoms” to be the most common reason men with BPH visit their physician, whereas 36% selected “bother from obstructive symptoms” and 10% chose “fear of prostate cancer”. When physicians were asked for the top three symptoms that trigger men with BPH to first visit their doctor, getting up at night to urinate was the most commonly named (87% of physicians), followed by the need to urinate more frequently (69%), slower or weaker urinary stream (42%), urgent need to urinate (41%) and difficulty starting to urinate (39%).
3.6. Diagnosis of BPH
At first consultation, 71% of patients recalled the doctor taking a urine sample, 57% recalled a prostate‐specific antigen (PSA) blood test being conducted and 56% recalled a digital rectal examination being performed. Almost one third (31%) of respondents reported that they received their diagnosis of BPH after one visit to the physician, and 39% within two visits.
3.7. Treatment experience and satisfaction
Among patients, 71% stated they were first given a prescription for medicine to treat their BPH symptoms during their first or second consultation. In most regions, the majority of patients were given a prescription treatment; however, in Australia, fewer than three in ten BPH patients (27%) received such treatment. Across all regions, anticholinergic drugs had been taken by patients for the longest period of time (28.9 months). Other drug classes were taken for between 18 and 23 months (alpha blockers, 23 months; alpha blocker/5ARI combination, 20 months; 5ARI monotherapy, 19 months), whereas herbal remedies and ß‐agonists were taken on average for less than 18 months.
Approximately one fifth of patients (21%) had changed from one prescription medication for BPH to another. The main reasons given for changing medication were that the product did not work quickly enough (37%), the effect of the product wore off (17%) and because of side effects (16%).
3.7.1. Patient satisfaction with treatment
Over two thirds of patients (69%) were satisfied with the medications they were currently taking for their BPH or prostate problems (Table 4), although patients in Japan were considerably less likely than others to report satisfaction (46%). When stratified by class of medication, users of dutasteride or dutasteride plus tamsulosin (brand names were used in the questionnaire) were more likely to be satisfied with their current medicine (76%) than other patients (alpha blockers, 69%; 5ARIs, 70%; combination therapy [alpha blocker plus 5ARI], 74%; herbal, 64%; other, 58%). The main reasons given for being satisfied with current medication were that it worked well (64%), or had minimal or no side effects (4%).
Table 4.
Patient satisfaction with treatment (data expressed as % of responders)
| Very/fairly satisfied | Neutral | Not very satisfied | Not at all satisfied | Don't know | |
|---|---|---|---|---|---|
| All countries | 69 | 20 | 9 | 1 | 2 |
| APAC Other | 80 | 13 | 6 | 1 | 0 |
| China | 67 | 26 | 6 | 0 | 1 |
| Australia | 75 | 12 | 7 | 0 | 6 |
| Japan | 46 | 24 | 23 | 5 | 3 |
| CIS | 73 | 18 | 7 | 0 | 3 |
| Latin America | 75 | 21 | 3 | 1 | 0 |
APAC, Asia Pacific; CIS, Commonwealth of Independent States.
3.7.2. Physician satisfaction with treatment
Overall, physicians expressed most satisfaction with alpha blockers, 5ARIs and the combination of alpha blocker plus 5ARI (Fig. 4). Less than one fifth of physicians (19%) were satisfied with herbal remedies or vasopressin analogues.
Figure 4.
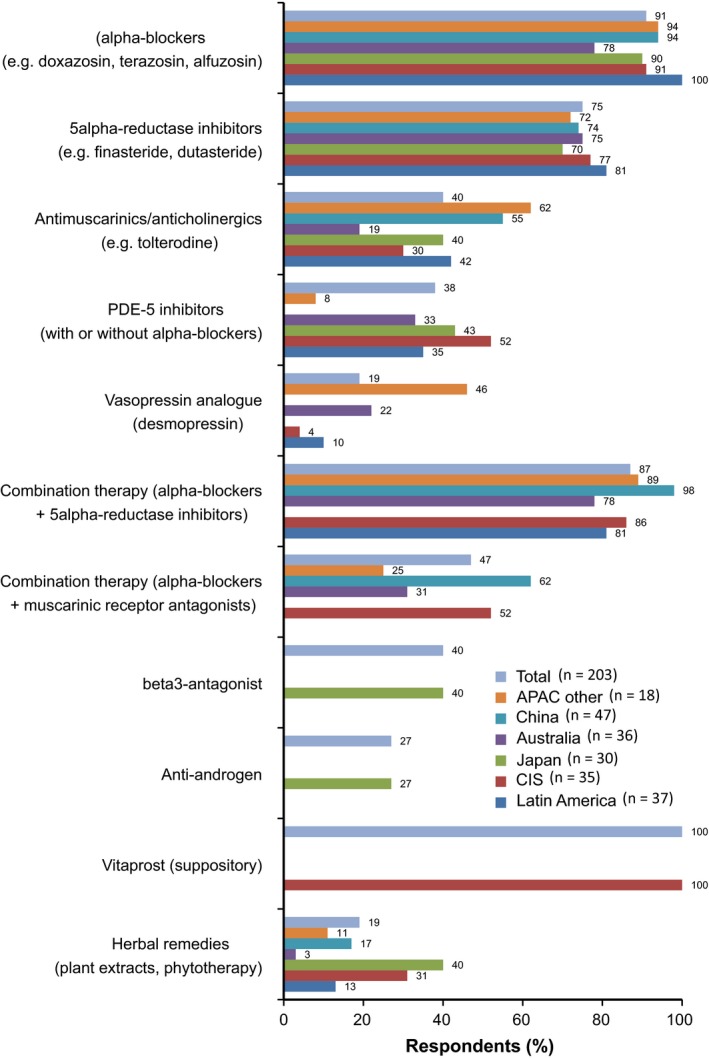
Physician satisfaction with BPH treatment. APAC, Asia Pacific; BPH, benign prostatic hyperplasia; CIS, Commonwealth of Independent States; PDE‐5, phosphodiesterase type 5
3.7.3. Treatment preference
When asked to rate attributes of a drug treatment for BPH on a scale of 1–8 (where 1 referred to a 50% reduction in the risk of surgery and onset of symptom relief within 6 months, and 8 referred to relief from symptoms within 2 weeks but no reduction in the risk of surgery), the average total score was 3.5, indicating that patients were slightly more in favour of waiting longer for symptom relief in order to benefit from a reduced risk of surgery. When patients were again given a scale of 1–8 (where 1 was an extremely strong preference for relief of symptoms within 6 months and 50% reduction in risk of surgery with a once weekly tablet, and 8 referred to symptom relief within 6 months and 50% reduction in risk of surgery with a once daily tablet), the mean scale score was 3.6, indicating that patients were slightly more in favour of a weekly tablet than a daily tablet. Some regional variation was noted, with patients in China showing a stronger preference for a weekly tablet than patients in other regions, and patients in Australia and Japan showing a slightly stronger preference for a daily tablet.
3.7.4. Adherence with treatment
Almost two fifths of patients (38%) were rated as having “low adherence” with treatment; one third (33%) were rated as “medium adherence” and the remaining 29% as “high adherence”. Patients in China and the CIS region were more likely than those from other regions to be rated as showing “low adherence”. Although patients in Australia were most likely to stop taking their medication before completing the course, they were also the most likely to be rated as “high adherence”, based on their current treatment behaviour. Dutasteride users (either as monotherapy or in combination with tamsulosin) were more likely than non‐dutasteride patients to be rated as having “high adherence” (40% vs 27%). Overall, approximately half of physicians surveyed (52%) thought adherence with treatment was “extremely” important.
3.8. Progression of BPH
Approximately one third of patients (32%) had discussed prostate‐related surgery with a HCP, and 28% had discussed AUR. Of those patients who had discussed surgery and AUR with their doctor, 70% and 76%, respectively, said they were “very” or “fairly” concerned about these issues.
Almost all physicians surveyed believed that BPH progresses in at least some patients, and just under half (46%) believed that it progresses in all patients. There was little regional variation, although Japanese physicians were the least likely to believe that BPH progresses in all patients (33%). Most (90%) physicians thought that at least some of their patients believe that BPH is a progressive condition. On average, physicians thought that 20% of their patients would progress to AUR and 30% would progress to BPH‐related surgery within 4 years of diagnosis. Overall, 92% of physicians believed that their patients were “very” or “fairly” concerned about surgery for BPH, whereas 72% believed that their patients were “very” or “fairly” concerned about AUR. Ninety per cent of physicians said that they always or usually took prevention of BPH progression into account when deciding how to treat a patient; 5ARIs and the combination of alpha blockers with 5ARI were most commonly identified by physicians as reducing the risk of BPH progression.
4. Discussion
PROBE II is the most comprehensive survey conducted to date of patient and physician perceptions of BPH in Asia Pacific, Latin America and the CIS region. Our data showed that there was agreement between patients and physicians in their perceptions of levels of awareness of BPH; almost two thirds of men felt “very well” or “fairly well” informed about health issues related to BPH, whereas a similar proportion of physicians perceived their patients to be “very well” or “fairly well” informed. However, almost one fifth of men, particularly those in the CIS region, did not feel well informed, highlighting the need for greater patient education. Regional differences were evident in information‐seeking behaviour; men in Australia were most likely to use the Internet, whereas men in China were most likely to consult leaflets from a healthcare professional, magazines/newspapers and the television. This suggests that educational initiatives should be tailored to suit regional preferences.
The main concerns of patients who sought medical advice for BPH were discomfort, disruption to sleep, fear of cancer and frustration with symptoms. These concerns were similar to those among men in Europe in the PROBE I study.13 There was a disconnect between patients and physicians in the reasons given for why men with urinary symptoms avoid or delay visiting a doctor. More than half (55%) of physicians thought it was because men believed it was just an inevitable part of ageing, compared with just 14% of patients who cited this as the reason. Physicians were also generally unaware that men may find it embarrassing to talk about their condition and often hoped it would go away on its own. This suggests that there is a need for HCPs to proactively raise the topic of BPH when patients present for other reasons, and to allay common misperceptions about BPH. The views of patients and physicians also differed in the perceived severity of BPH symptoms on initial presentation, which may impact the physician–patient relationship and lead to delays in starting the most appropriate treatment.
In this study, patients were slightly more in favour of waiting longer for symptom relief in order to benefit from a reduced risk of surgery. This is in agreement with previous research, which found that a slight majority of patients preferred therapies affecting long‐term disease progression over those that provide short‐term symptom improvement.15
Despite over half of physicians surveyed expressing the belief that treatment adherence is extremely important, 38% of patients were rated as showing low adherence to treatment. This is in line with findings from other studies demonstrating poor adherence with BPH treatments.9, 10 Further research into the reasons for poor adherence is needed, to inform strategies for improving adherence which could in turn improve clinical outcomes.
There were some similarities, but also some differences, between our findings and those from the first PROBE study.3 A similar proportion of patients felt well informed about BPH (61% in PROBE II and 56% in PROBE I). However, a greater proportion of physicians in PROBE II felt it would be valuable to raise awareness of BPH (70% vs 51% in PROBE I). Interestingly only six in ten patients in PROBE II said that they noticed BPH symptoms themselves, whereas in the previous study 85% discovered the symptoms on their own.3
In both PROBE studies, hoping that the condition would go away was the main reason for delaying a visit to a doctor. From a physician perspective, over half (55%) of those in PROBE II believed that men with urinary symptoms avoided or delayed visiting a doctor because they thought it was just an inevitable part of ageing, compared with just under half of physicians in PROBE I.3 In PROBE II, discomfort was the top patient concern, whereas in PROBE I fear of cancer was the most frequent concern raised by patients. In both studies, around three quarters of patients were prescribed medication on their first or second visit to their physician. Although a minority of patients (32%) surveyed for this study discussed prostate‐related surgery with their doctor, over half (54%) had done so in PROBE I. Possible explanations for differences between PROBE I and PROBE II include regional differences in practice patterns and attitudes and the fact that the studies were conducted more than 10 years apart.
There are some limitations to our study, including lack of longitudinal follow up and possible recall bias. In addition, physicians and patients were invited using market research databases, which may indicate potential bias related to their willingness to participate in the survey as they may be more proactive in their approach to managing the condition. There are also some potential limitations related to sampling of patients and physicians. For example, the number of patients included for large population countries such as China could be considered relatively low, and therefore may not be entirely representative of the population with BPH. However, for a survey among of patients with a specific condition such as BPH sample sizes are typically smaller than for more general consumer samples. Data are not available on the BPH patient universe to enable structuring of the sample so that it is representative of, for example, urban/rural areas. Nevertheless, we ensured a good regional distribution across the sample to capture any major regional differences. For physicians, no account was taken of academic status, or whether office or hospital based; different practice patterns across these categories may therefore not be entirely represented.
5. Conclusions
The PROBE II survey provides valuable insights into the attitudes and beliefs of patients and physicians in the Asia Pacific, Latin America and CIS regions about BPH and its management. It also highlights important areas of discordance between patients’ and physicians’ perceptions and beliefs about BPH. There is a need to raise awareness of BPH and its symptoms among older men, and for HCPs to adopt more proactive counselling approaches, to ensure that men with this condition receive a timely diagnosis and appropriate treatment.
Author contributions
All authors made substantial contributions to research design, or the acquisition, analysis or interpretation of data; were involved in drafting the manuscript or revising it critically and approved the submitted and final versions.
Acknowledgements
This study was funded by GlaxoSmithKline. Medical writing support was provided by Tony Reardon of Spirit Medical Communications Ltd, funded by GlaxoSmithKline.
Disclosures
BA, ID, PE and MM are employees of GlaxoSmithKline. BL is an employee of Ipsos Healthcare, who carried out the study on behalf of GlaxoSmithKline.
References
- 1. van Asseldonk B, Barkin J, Elterman DS. Medical therapy for benign prostatic hyperplasia: a review. Can J Urol. 2015;22(5 Suppl 1):7–17. [PubMed] [Google Scholar]
- 2. Lee HW, Kim SA, Nam JW, et al. The study about physical activity for subjects with prevention of benign prostate hyperplasia. Int Neurourol J. 2014;18:155–162. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3. Emberton M, Cornel EB, Bassi PF, et al. Benign prostatic hyperplasia as a progressive disease: a guide to the risk factors and options for medical management. Int J Clin Pract. 2008;62:1076–1086. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4. Gupta K, Yesdani M, Sotelo T, Aragon‐Ching JB. A synopsis of drugs currently in preclinical and early clinical development for the treatment of benign prostatic hyperplasia. Expert Opin Investig Drugs. 2015;24:1059–1073. [DOI] [PubMed] [Google Scholar]
- 5. Emberton M, Zinner N, Michel MC, et al. Managing the progression of lower urinary tract symptoms/benign prostatic hyperplasia: therapeutic options for the man at risk. BJU Int. 2007;100:249–253. [DOI] [PubMed] [Google Scholar]
- 6. Saigal CS, Joyce G. Economic costs of benign prostatic hyperplasia in the private sector. J Urol. 2005;173:1309–1313. [DOI] [PubMed] [Google Scholar]
- 7. Kirby RS, Kirby M, Fitzpatrick JM. Benign prostatic hyperplasia: counting the cost of its management. BJU Int. 2010;105:901–902. [DOI] [PubMed] [Google Scholar]
- 8. Speakman M, Kirby R, Doyle S, Ioannou C. Burden of male lower urinary tract symptoms (LUTS) suggestive of benign prostatic hyperplasia (BPH) – focus on the UK. BJU Int. 2015;115:508–519. [DOI] [PubMed] [Google Scholar]
- 9. Cindolo L, Pirozzi L, Fanizza C, et al. Drug adherence and clinical outcomes for patients under pharmacological therapy for lower urinary tract symptoms related to benign prostatic hyperplasia: population‐based cohort study. Eur Urol. 2015;68:418–425. [DOI] [PubMed] [Google Scholar]
- 10. Cindolo L, Pirozzi L, Sountoulides P, et al. Patient's adherence on pharmacological therapy for benign prostatic hyperplasia (BPH)‐associated lower urinary tract symptoms (LUTS) is different: is combination therapy better than monotherapy? BMC Urol. 2015;15:96. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11. Koh JS, Cho KJ, Kim HS, Kim JC. Twelve‐month medication persistence in men with lower urinary tract symptoms suggestive of benign prostatic hyperplasia. Int J Clin Pract. 2014;68:197–202. [DOI] [PubMed] [Google Scholar]
- 12. Kaplan S, Naslund M. Public, patient, and professional attitudes towards the diagnosis and treatment of enlarged prostate: a landmark national US survey. Int J Clin Pract. 2006;60:1157–1165. [DOI] [PubMed] [Google Scholar]
- 13. Emberton M, Marberger M, de la Rosette J. Understanding patient and physician perceptions of benign prostatic hyperplasia in Europe: the Prostate Research on Behaviour and Education (PROBE) Survey. Int J Clin Pract. 2008;62:18–26. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14. Morisky DE, Green LW, Levine DM. Concurrent and predictive validity of a self‐reported measure of medication adherence. Med Care. 1986;24:67–74. [DOI] [PubMed] [Google Scholar]
- 15. Emberton M. Medical treatment of benign prostatic hyperplasia: physician and patient preferences and satisfaction. Int J Clin Pract. 2010;64:1425–1435. [DOI] [PubMed] [Google Scholar]


