Abstract
Background
Pre-exposure prophylaxis (PrEP) is efficacious in preventing HIV among men who have sex with men (MSM). We assessed PrEP uptake among MSM presenting for services at a sexually transmitted diseases (STD) clinic.
Methods
MSM presenting to the Rhode Island STD Clinic between October 2013 and November 2014 were educated about, and offered, PrEP. We categorized PrEP engagement using an implementation cascade to describe gaps in uptake which described MSM who: 1) were educated about PrEP, 2) indicated interest, 3) successfully received follow-up contact, 4) scheduled an appointment, 5) attended an appointment, and 6) initiated PrEP (i.e., received a prescription). Bivariate and multivariable logistic regression models were used to examine predictors of PrEP initiation.
Results
A total of 234 MSM were educated about PrEP; of these, 56% expressed interest. Common reasons for lack of interest were low HIV risk perception (37%), wanting more time to consider (10%), concern about side effects (7%), and financial barriers (3%). Among those interested, 53% followed up. Of those, 51% scheduled an appointment. The most common reason patients did not schedule an appointment was low HIV risk perception (38%). Seventy-seven percent of those with an appointment attended the appointment; of those, 93% initiated PrEP. Patients with higher HIV risk perception (aOR=2.17, 95% CI 1.29-3.64) and a history of sex with an HIV-positive partner (aOR=7.08, 95% CI 2.35-21.34) had significantly higher odds of initiating PrEP.
Conclusions
Low HIV risk perception was the most significant barrier to PrEP uptake among MSM attending a public STD clinic.
Keywords: pre-exposure prophylaxis, implementation, men who have sex with men, HIV, sexually transmitted diseases
Summary: Low perceived HIV risk was a significant barrier to pre-exposure prophylaxis uptake among high-risk men who have sex with men at a sexually transmitted disease clinic.
INTRODUCTION
Pre-exposure prophylaxis (PrEP) is a bio-behavioral HIV prevention intervention consisting of once-daily treatment with a fixed dose combination of tenofovir disoproxil fumarate (TDF) and emtricitabine (FTC), the only medication currently approved by the US Food and Drug Administration (FDA) for this purpose. TDF/FTC has demonstrated high efficacy in preventing HIV acquisition in MSM in multiple randomized controlled trials, with greater than 90% efficacy when individuals were adherent.1–3 The Centers for Disease Control and Prevention (CDC) estimate that approximately 1.2 million Americans are eligible for PrEP.4 However, PrEP implementation in clinical settings has been slow,5 consistent with diffusion of innovations in clinical practice.6 Engaging groups who would benefit most from PrEP, including MSM, persons of color, and others who are at high risk, has been difficult in the context of structural barriers such as limited healthcare access and stigma.7,8 Individual-level barriers to PrEP implementation include low HIV risk perception, limited knowledge about PrEP,9 prohibitive cost or lack of insurance coverage,10 and concerns about side effects.11 Some providers have also expressed concern that PrEP use may promote behavioral risk compensation such as reduced condom use, ultimately undermining HIV and STD prevention.12 Optimal settings and methodology to deliver PrEP to high risk populations outside of research settings, in the context of multiple structural and individual-level barriers, have not been clearly delineated.12,13
STD clinics, which provide safety net services to low-income and high-risk populations such as MSM, represent opportune venues for PrEP programs in the US.13,14 The US PrEP Demonstration Project has demonstrated the feasibility and acceptability of PrEP implementation in these settings.15,16 Though promising, these findings do not necessarily reflect PrEP uptake in “real-world” clinical settings, as TDF/FTC for PrEP was provided at no cost to research participants in this and other demonstration studies. In 2013, we implemented a clinical PrEP program at a publicly-funded STD clinic in Providence, Rhode Island. This paper describes predictors of interest in PrEP and uptake among MSM presenting for STD services at our clinic and presents an implementation cascade describing the number of MSM who were educated about, expressed interest in, and initiated PrEP.
MATERIALS AND METHODS
Setting
The Rhode Island STD Clinic, part of The Miriam Hospital Immunology Center in Providence, is a publicly-funded STD clinic supported by the Rhode Island Department of Health. The clinic was established in early 2012 in response to increasing STD incidence in Rhode Island.17,18 The Miriam Hospital Immunology Center provides care to 80% of HIV-positive patients in the state, and the STD Clinic currently reports a 2% annual rate of new HIV diagnoses.
PrEP Program
In 2013, we implemented a PrEP program at the Rhode Island STD Clinic in accordance with CDC guidelines for provision of PrEP.19 All MSM who presented to the clinic for STD testing and treatment were offered education about PrEP, irrespective of reported behavioral risk factors. We adopted this approach to raise community awareness about PrEP given that the majority of new HIV diagnoses in Rhode Island occur among MSM.20 PrEP educational services were fully integrated into existing HIV/STD educational and screening programs, rather than being implemented as a standalone PrEP intervention. Test counselors were trained to counsel patients about PrEP and performed brief (approximately five minutes) PrEP educational sessions. Educational sessions were guided by a one-page informational sheet (see Appendix).19 Educational material included clinical indications for PrEP, a description of TDF/FTC treatment, common side effects, and follow-up clinical care guidelines, followed by an opportunity to discuss any of the patient's questions or concerns regarding PrEP.
Post-PrEP Session
Following the educational session, patients completed a brief questionnaire regarding their interest in initiating PrEP. Patients were asked how well they understood PrEP and whether they had any concerns about taking the medication. Patients who expressed interest in PrEP provided contact information and received a follow-up phone call from clinic staff within one to two weeks of their educational session. Patients were called at least two times, and messages were left if patients did not answer the phone. Upon contact, we scheduled appointments for patients who continued to express interest in PrEP with a medical provider at the STD Clinic, who assumed responsibility for follow-up and ongoing PrEP care. If patients were interested in PrEP and uninsured, insurance was obtained through the guidance of onsite financial staff.
Measures
We reviewed data from all MSM who presented for HIV/STD testing and were educated about PrEP from October 2013 to November 2014. Demographic data reviewed included age, gender, race, ethnicity, and insurance coverage status. Behavioral data reviewed included lifetime history of HIV testing, number and gender of sex partners in the past 12 months (oral, vaginal, and anal sex), condom use, sex with anonymous partners, drug or alcohol use during sex, sex with partners of unknown or HIV-positive status, history of transactional sex, sex with a partner who engages in transactional sex, history of forced sex, and past-year and lifetime STD diagnoses. Perceived HIV risk was measured by the item, “How would you rate your risk for contracting HIV?” with response options on a Likert scale from 1 (extremely unlikely) to 5 (extremely likely).
Data Analysis
To describe gaps in PrEP uptake, we analyzed six PrEP implementation steps including MSM who: (1) received PrEP education, (2) expressed interest in taking PrEP, (3) successfully received follow-up contact, (4) scheduled an appointment with a PrEP provider, (5) attended an appointment with a PrEP provider, and (6) received a PrEP prescription. We evaluated outcomes among all MSM who were educated about PrEP and repeated analyses using the subsample of men reporting at least one condomless anal sex encounter. The latter criterion was based on CDC guidelines indicating PrEP for men who have condomless anal sex with other men.19
Bivariate logistic regression analyses were conducted using all demographic and behavioral variables to identify those significantly correlated with PrEP interest and uptake. Multivariable logistic regression analyses were then performed to determine the relationship between multiple predictors and the two primary outcomes of interest, interest in PrEP and being prescribed PrEP. Variables with a p-value of <0.05 in the bivariate models were retained in the final multivariable models. Age, race, and ethnicity were selected a priori to be included in the final models, regardless of their significance in the bivariate models. Results of regression models are reported as odds ratios (ORs) and adjusted odds ratios (aORs) with 95% confidence intervals (CIs). The alpha level for significance was set to 0.05 (two-tailed) for each analysis. All dichotomous variables were coded with the non-endorsing group serving as the referent. Analyses were performed using SPSS 22 (IBM Corp, Armonk, NY). Evaluation of the PrEP program, including retrospective review of patient data, was approved by the institutional review board at The Miriam Hospital.
RESULTS
A total of 1,806 visits to the Rhode Island STD Clinic took place from October 2013 to November 2014, 30% of which were visits by MSM (n=539); these figures denote the total number of visits, and not unique individuals given that clinic visits have limited identifying information. Of the total population of MSM presenting for STD services, 234 unique individuals were educated about PrEP and completed a post-evaluation form. Reasons eligible patients were not educated about PrEP included lack of patient or provider time (63%), previous PrEP discussion with a provider (15%), patient was HIV-positive (10%), patient refused (6%), patient was already taking PrEP (4%), or patient spoke a language other than English with no interpreter present (1%).
Demographics
The demographic characteristics and HIV risk behaviors of MSM who were educated about PrEP (n=234) are depicted in Table 1. Individuals ranged in age from 18 to 72 years (mean = 32.3, standard deviation [SD] = 12.2), with 75% of patients aged 37 years or younger. Seventy-seven percent of individuals identified as White, 9% Black/African American, 4% Asian, and 9% as mixed or other race, reflecting local community demographics. Eighteen percent of MSM during this period identified as Hispanic or Latino. Eighty-five percent were non-transgender men who reported having sex with only men, 15% were non-transgender men who reported having sex with both men and women, and one individual was a transgender woman who reported having sex with only men. The majority (62%) of individuals did not have health insurance of any kind, including through public payers (i.e., Medicaid, Medicare).
Table 1.
Characteristics and Binary Logistic Regressions Predicting Interest in PrEP and Being Prescribed PrEP
| Total Sample N=234 | Interested in PrEP n=130 | Prescribed PrEP n=25 | |||
|---|---|---|---|---|---|
|
| |||||
| n(%) or M(SD) | n(%) or M(SD) | OR [95% CI] | n(%) or M(SD) | OR [95% CI] | |
| Age | 32.3 (12.17) | 31.8 (12.3) | 0.99 [0.97, 1.01] | 31 (8) | 0.99 [0.95, 1.03] |
| Race | |||||
| Caucasian/White | 181 (77%) | 97 (75%) | REF | 21 (84%) | REF |
| AA/Black | 22 (9%) | 15 (12%) | 1.86 [0.72, 4.77] | 0 (0%) | 0.00 [0.00, -] |
| Asian | 10 (4%) | 8 (6%) | 3.46 [0.72, 16.76] | 1 (4%) | 0.85 [0.10, 7.02] |
| Mixed/Other | 20 (9%) | 9 (7%) | 0.71 [0.28, 1.79] | 3 (12%) | 1.35 [0.36, 4.98] |
| Hispanic | 42 (18%) | 23 (18%) | 0.96 [0.49, 1.88] | 3 (12%) | 0.59 [0.17, 2.06] |
| Insurance | 87 (37%) | 52 (40%) | 1.33 [0.78, 2.28] | 12 (50%) | 1.79 [0.77, 4.17] |
| Risk1 | |||||
| MSM | 198 (85%) | 111 (85%) | REF | 20 (80%) | REF |
| MSMW | 35 (15%) | 19 (15%) | 1.14 [0.56, 2.33] | 5 (20%) | 0.69 [0.24, 1.99] |
| TSM | 1 (0%) | 0 (0%) | - | 0 (0%) | - |
| Prior HIV Test | 201 (86%) | 112 (87%) | 1.04 [0.49, 2.22] | 23 (92%) | 1.87 [0.42, 8.37] |
| 10+ sexual partners | 57 (24%) | 33 (25%) | 1.13 [0.62, 2.07] | 8 (32%) | 1.54 [0.63, 3.78] |
| Any anonymous sexual partners | 135 (58%) | 77 (59%) | 1.15 [0.68, 1.94] | 17 (68%) | 1.64 [0.68, 3.97] |
| Substance use with sex | 69 (30%) | 37 (29%) | 0.90 [0.51, 1.57] | 7 (28%) | 0.92 [0.37, 2.32] |
| Sex w/ partner of unknown status | 137 (59%) | 50 (39%) | 0.76 [0.45, 1.28] | 6 (24%) | 0.41 [0.16, 1.7] |
| Exchanged sex | 9 (4%) | 5 (4%) | 1.00 [0.26, 3.82] | 0 (0%) | 0.00 [0.00, -] |
| Sex with exchanger | 13 (6%) | 9 (7%) | 1.86 [0.56, 6.22] | 1 (4%) | 0.68 [0.09, 5.50] |
| Ever forced to have sex | 16 (7%) | 8 (6%) | 0.79 [0.29, 2.19] | 0 (0%) | 0.00 [0.00, -] |
| STD last 12 months | 28 (12%) | 20 (15%) | 2.18 [0.92, 5.18] | 5 (20%) | 2.02 [0.69, 5.90] |
| Prior STD lifetime | 69 (30%) | 48 (37%) | 2.31 [1.27,4.20]** | 7 (28%) | 0.92 [0.37, 2.32] |
| Any current STD | 34 (15%) | 22 (17%) | 1.56 [0.73, 3.33] | 5 (20%) | 1.55 [0.54, 4.46] |
| Any condomless anal sex | 170 (73%) | 102 (79%) | 1.93 [1.08, 3.45]* | 21 (84%) | 2.11 [0.70, 6.42] |
| Sex with HIV-positive partner | 29 (12%) | 22 (17%) | 2.82 [1.16, 6.90]* | 9 (36%) | 5.32 [2.08, 13.58]*** |
| # Anal sex partners | 4.9 (6.20) | 5.4 (7.00) | 1.03 [0.98, 1.08] | 6.52 (7.35) | 1.04 [0.98, 1.09] |
| # Oral sex partners | 6.4 (8.10) | 6.9 (9.50) | 1.02 [0.98, 1.05] | 6.88 (10.05) | 1.01 [0.96, 1.06] |
| Self-perceived HIV risk2 | 2.4 (0.90) | 2.5 (0.88) | 1.72 [1.25, 2.39]*** | 2.88 (0.90) | 1.87 [1.22, 2.86]** |
p<.05;
p<.01;
p<.001
AA= African American; MSM = men who have sex with men; MSMW = men who have sex with men and women; PrEP=pre-exposure prophylaxis; TSM = transgender women who have sex with men; STD = sexually transmitted disease.
Collaposed into binary (0 = MSM, 1 = Non-MSM) for logistic regression analysis;
Likert scale from 1 (extremely unlikely) to 5 (extremely likely); dependent variable in this analysis was coded so that 0 = was not interested in PrEP or not prescribed PrEP and 1 = Interested in PrEP or Prescribed PrEP with model predicting 1 group; Referents (REF) are group not endorsing listed behavior unless otherwise noted.
Sexual Risk Behaviors
Eighty-seven percent of individuals reported more than one sexual partner in the last 12 months. Individuals had an average of 6.2 (SD=4.9) anal sex partners and 8.1 (SD=0.90) oral sex partners in the last year. The majority (73%, n =170) reported condomless anal sex, sex with a partner of unknown HIV status (59%, n=137), or sex with an anonymous partner (58%, n=135) in the past year. In bivariate regressions, sex with an HIV-positive partner in the past year was associated with PrEP interest and obtaining a PrEP prescription. Greater perceived HIV risk was significantly associated with higher odds of past-year use of “poppers” (amyl nitrates), sex while under the influence of substances, and higher number of partners, and was significantly associated with both PrEP interest and obtaining a prescription.
Cascade of PrEP Uptake: All MSM
A total of 234 MSM underwent the PrEP educational session (Figure 1). Following this initial session, 56% (n = 130) reported being interested in learning more about PrEP. Among those who reported lack of interest (n = 104), reasons included low HIV risk perception (37%), desire to think about or research PrEP more (10%), concern about medication regimen or side effects (7%), insurance or financial reasons (3%), and other reasons (11%, e.g., planning to “quit” risk behavior); 35% of patients did not specify a reason for lack of PrEP interest. Among individuals who expressed interest in learning more about PrEP, 53% (n = 69, 29% of total sample) were successfully contacted by clinic staff for follow-up to schedule an appointment for PrEP. Among individuals successfully contacted for follow-up, 51% (n = 35, 15% of total sample) made an appointment for a prescription. Reasons why individuals did not schedule an appointment (n = 34) included low HIV risk perception (38%), desire to think about or research PrEP more (12%), concern about medication regimen or side effects (15%) and insurance or financial reasons (6%). Among those who scheduled an appointment, 77% (n = 27, 12% of total sample) presented for the appointment. Among individuals who attended appointments, 93% (n = 25, 11% of total sample) were prescribed PrEP (Table 2). Two patients were not prescribed PrEP after discussion with a physician due to low HIV risk. Eighty percent (n = 20) of the 25 patients who received a prescription were confirmed to have started PrEP by self-report. Two individuals did not start PrEP (one person had high deductible and could not afford the medication, and the other was concerned about side effects). Three individuals who received a prescription were lost to follow-up.
Figure 1.
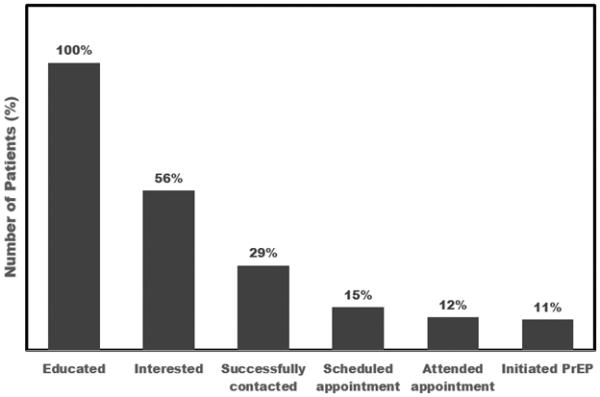
The PrEP implementation cascade among men who have sex with men presenting to the Rhode Island STD Clinic (N=234)
Table 2.
Implementation cascade describing frequencies in PrEP uptake among men who have sex with men at the Rhode Island STD Clinic (N=234)
| From full sample | |||
| Administered PrEP education session | 234 (100%) | 234 (100%) | |
|
|
|||
| Post PrEP education session | |||
| Interested | 130 (56%) | 130 (56%) | |
| Not interested | 104 (44%) | Of uninterested | |
| Perceived low risk | 38 (37%) | ||
| Desire to think about or research more | 10 (10%) | ||
| Concerned w/medication regimen/side effects | 7 (7%) | ||
| Insurance/Financial | 3 (3%) | ||
| Did not specify | 35 (34%) | ||
| Other | 11 (11%) | ||
|
|
|||
| Attempted to contact for follow-up | (Of those interested, N=130) | ||
| Successful | 69 (53%) | 69 (29%) | |
| Not contacted | 61 (47%) | ||
|
|
|||
| Attempted to schedule appointment | (Of those successfully contacted, N=69) | ||
| Scheduled | 35 (51%) | 35 (15%) | |
| Not scheduled | 34 (49%) | Of not scheduled | |
| Perceived low risk | 13 (38%) | ||
| Desire to think about or research more | 5 (15%) | ||
| Concerned w/medication regimen/side effects | 4 (12%) | ||
| Insurance/Financial | 2 (6%) | ||
| Other | 10 (29%) | ||
|
|
|||
| Came to appointment | (Of those scheduled, N=35) | ||
| Yes | 27 (77%) | 27 (12%) | |
| No | 8 (23%) | ||
|
|
|||
| Prescribed PrEP | (Of those who attended their appointment, N=27) | ||
| Yes | 25 (93%) | 25 (11%) | |
| No | 2 (7%) | ||
Cascade of PrEP Uptake: Men ≥ 1 Condomless Anal Sex Partner
A total of 170 individuals in the study sample reported at least one condomless anal sex encounter in the last 12 months at the time of presenting for STD services (Table 3). Following the initial educational session, 60% (n = 102) of these reported interest in learning more about PrEP. Reasons the remaining 40% (n = 68) were not interested included low HIV risk perception (32%), desire to think about or research PrEP more (10%), concern about medication regimen or side effects (9%) and other reasons (9%, e.g., not wanting female partner or others to see medication). Forty percent of those who were not interested did not specify a reason.
Table 3.
Implementation cascade describing frequencies in PrEP uptake among men who have sex with men with one or more condomless anal sex encounter (CASE) at the Rhode Island STD Clinic (N=170)
| From MSM ≥ 1 CASE | |||
| Administered PrEP education session | 170 (100%) | 170 (100%) | |
|
|
|||
| Post PrEP education session | |||
| Interested | 102 (60%) | 102 (60%) | |
| Not interested | 68 (40%) | Of uninterested | |
| Perceived low risk | 22 (32%) | ||
| Desire to think about or research more | 7 (10%) | ||
| Concerned w/medication regimen/side effects | 6 (9%) | ||
| Insurance/Financial | 0 (0%) | ||
| Did not specify | 27 (40%) | ||
| Other | 6 (9%) | ||
|
|
|||
| Attempted to contact for follow-up | (Of those interested, N=102) | ||
| Successful | 57 (56%) | 57 (36%) | |
| Not contacted | 45 (44%) | ||
|
|
|||
| Attempted to schedule appointment | (Of those successfully contacted, N=57) | ||
| Scheduled | 30(53%) | 30 (18%) | |
| Not scheduled | 27(47%) | Of not scheduled | |
| Perceived low risk | 10 (37%) | ||
| Desire to think about or research more | 5 (19%) | ||
| Concerned w/medication regimen/side effects | 2 (7%) | ||
| Insurance/Financial | 1 (4%) | ||
| Other | 9 (33%) | ||
|
|
|||
| Came to appointment | (Of those scheduled, N=30) | ||
| Yes | 22 (73%) | 22 (13%) | |
| No | 8 (27%) | ||
|
|
|||
| Prescribed PrEP | (Of those who made their appointment, N=22) | ||
| Yes | 21 (95%) | 21 (12%) | |
| No | 1 (5%) | ||
Among interested individuals, 56% (n = 57, 36% of total sample) were successfully contacted for follow-up, 53% (n = 30, 18% of total sample) of whom made an appointment for a prescription. Reasons individuals did not schedule an appointment (n = 27) included: low HIV risk perception (37%), desire to think more about PrEP (19%), concern about medication regimen or side-effects (7%), and insurance or other financial reasons (4%). Among individuals who scheduled an appointment, 73% (n = 22, 13% of total sample) attended the appointment. Of those who attended the appointment, 95% (n = 21, 12% of total sample) were prescribed PrEP. Of the 21 men reporting condomless anal sex who were prescribed PrEP, 81% (n=17) were confirmed to have started PrEP. One individual did not start PrEP due to concern about side effects and three individuals were lost to follow-up.
Predictors of PrEP Interest
In the bivariate analyses (Table 1), statistically significant variables that predicted interest in PrEP included: history of STD diagnosis (OR=2.31, 95% CI 1.27–4.20, p=0.006), sex with an HIV-infected partner (OR=2.82, 95% CI 1.16–6.90, p=0.023), engaging in condomless anal sex with at least one partner (OR=1.93, 95% CI 1.08–3.45, p=0.027), and greater HIV risk perception (OR=1.72, 95% CI 1.25–2.39, p=0.001). In the multivariable model (Table 4) adjusting for age, race, and ethnicity, HIV risk perception (aOR=1.58, 95% CI 1.13 to 2.22, p=0.008) was the only significant correlate of interest in PrEP (Table 4A).
Table 4.
| A Logistic regression results predicting being interested in PrEP† | ||
|---|---|---|
|
| ||
| AOR† | 95% CI | |
|
|
||
| HIV risk perception1 | 1.58** | 1.13, 2.22 |
| Any condomless anal sex2 | 1.81 | 0.96, 3.45 |
| Any sex w/HIV-positive partner2 | 2.53‡ | 0.98, 6.57 |
| Ever had an STD (lifetime)2 | 1.85§ | 0.98, 3.47 |
| Model: χ2 = 29.02 P= .000644 | ||
| B Logistic regression results predicting being prescribed PrEP† | ||
|---|---|---|
|
| ||
| AOR† | 95% CI | |
|
|
||
| HIV risk perception1 | 2.17** | 1.29, 3.64 |
| Any sex w/HIV-positive partner2 | 7.08*** | 2.35, 21.34 |
| Model: χ2 = 30.58 P= .000074 | ||
Model controls for age, race, and ethnicity. The dependent variable in this analysis is coded so that 0 = not interested in PrEP and 1 = Interested in PrEP;
Likert scale ranging from 1 (no risk) to 5 (high risk);
Reference group = No, AORs displayed for Yes group. PrEP=pre-exposure prophylaxis; STD=sexually transmitted disease; AOR=adjusted odds ratio; CI=confidence interval.
p ≤ .05;
p ≤ .01;
p≤ .001
approaching significance at p = 0.056
approaching significance at p = 0.057
Predictors of PrEP Uptake
In the bivariate analyses (Table 1), variables significantly associated with PrEP uptake included sex with an HIV-positive partner (OR=5.32, 95% CI 2.08–13.58, p<0.001) and HIV risk perception (OR=1.87, 95% CI 1.22–2.86, p=0.004). In the multivariable model (Table 4B) adjusting for age, race, and ethnicity, both predictors maintained significant associations with PrEP uptake. History of sex with an HIV-positive partner was associated with significantly greater odds (aOR=7.08, 95% CI 2.3-21.34, p<0.001) of being prescribed PrEP. Greater HIV risk perception was also associated with greater odds of being prescribed PrEP (aOR=2.17, 95% CI 1.29-3.64, p=0.003) (Table 4B).
DISCUSSION
This study describes significant barriers to PrEP uptake among MSM at a public STD clinic, a population with a 2% annual rate of new HIV diagnoses.21 CDC guidelines recommend considering PrEP in MSM who report condomless anal sex with men.19 To promote PrEP among MSM, PrEP education and counseling were integrated into standard care at our STD clinic. We found that acceptability of PrEP education was high among MSM, as most patients were amenable to receiving PrEP education. Nonetheless, the overall rate of PrEP uptake was low, similar to other reports in STD clinic settings.22,23 PrEP uptake was lower among racial and ethnic minorities, likely reflecting a combination of individual- and structural-level factors including insurance status. Among all MSM who were educated about PrEP, only half (56%) were initially interested in PrEP, despite reporting risk factors associated with HIV acquisition such as condomless anal sex. Only 53% of those who expressed interest were successfully contacted for follow-up. Of these, 51% scheduled an appointment; the majority of these individuals attended their appointment and were prescribed PrEP. The most common reason individuals were not interested in PrEP was low perceived HIV risk. Other concerns commonly cited by MSM included cost and side effects. In a multivariable regression analysis, HIV risk perception and history of sex with an HIV-positive partner were significant predictors of PrEP uptake. Cascade results were similar among MSM who reported at least one episode of condomless anal sex in the previous 12 months compared to the total MSM sample. Ultimately, 11% of all MSM and 12% of MSM reporting condomless sex initiated PrEP through our educational program. The results of this study provide insight for best practices in PrEP provision at STD clinics and add to the existing body of literature on PrEP implementation by introducing experiences from a STD clinic-based PrEP program.24
Among our clinic MSM population, low HIV risk perception was an important reason for declining PrEP, in contrast to findings from other studies indicating that concern about side effects was the major predictor of refusing PrEP.24,25 HIV risk perception and sex with an HIV-positive partner were the only significant predictors of PrEP uptake. These findings suggest that MSM who most accurately perceive their HIV acquisition risks are more likely to take up PrEP; however, even among those reporting high perceived HIV risk, PrEP uptake was suboptimal. Prior research demonstrates that individuals with low perceived HIV risk are less likely to undergo HIV testing and participate in other HIV prevention strategies.26–29 Similarly, we hypothesize that improved education about HIV risk should result in increased PrEP uptake.30 Addressing low HIV risk perception among at risk MSM should be a focus for future interventions to enhance PrEP uptake.
Prior to incorporating PrEP education into standard clinical care, only 25% of our clinic population reported any PrEP awareness. There are likely positive spillover effects of providing brief PrEP education sessions to all MSM presenting for care, such that educating some MSM helped raise awareness in the larger community. Indeed, anecdotal evidence from patients suggests that clients shared information about our PrEP program with friends, many of whom subsequently presented for PrEP care. In addition, we were able to successfully integrate this brief screening program into the clinic workflow, which allowed us to identify and prescribe PrEP to many MSM who otherwise might not have sought information regarding this important biomedical intervention elsewhere.
This study is subject to several limitations. Small sample size, particularly of the number of MSM who initiated PrEP, limited our power to detect associations between variables in regression analysis. The study evaluated PrEP initiation defined as receiving a prescription; subsequent retention in care and adherence were beyond the scope of this analysis but are reported elsewhere.31,32 Additionally, patients may have sought PrEP care elsewhere after the PrEP education session, which we were not able to measure or incorporate in our analysis. On the level of clinic operations, we lost a significant number of PrEP candidates during the follow-up period. One way to address this challenge would be to have a medical provider who is able to prescribe PrEP at the time of the initial STD testing appointment. Other potential interventions to minimize the number of PrEP-eligible patients lost to follow-up may include peer- or patient-navigators to help facilitate PrEP uptake. Availability of providers and staff to facilitate immediate referral and follow-up is currently limited by the funding and staffing constraints common among many publicly-funded, community clinics. Additionally, on busy clinic days, a small fraction of MSM presenting for care did not receive PrEP educational sessions; those men represented less than 10% of eligible participants and were not included in this analysis. Finally, our results may not be generalizable to all STD clinics in the US.
This study is among the first to evaluate PrEP implementation at an STD clinic outside a demonstration project or clinical trial. Results of this study highlight barriers to uptake and opportunities for enhancing STD clinic-based PrEP programs. Interventions that improve understanding of HIV risk perception may enhance uptake. In addition, future studies should also evaluate PrEP retention in care and adherence outside of research settings. From a programmatic perspective, low PrEP uptake in our clinic highlights opportunities for us to improve our approach to PrEP education; this is also fertile ground for intervention development and other research. These findings can inform development of other PrEP programs across the US.
Supplementary Material
Acknowledgments
Sources of Support: The study was supported by a research grant from Gilead Sciences, Inc. PAC is supported by the National Institute of Allergy and Infectious Diseases (1K23AI096923). CEO is supported by the National Institute of Drug Abuse (T32DA013911) and the National Institute of Mental Health (R25MH083620). JR is supported by the National Institute of Allergy and Infectious Diseases (T32AI102623) and the National Institute of Mental Health (R25MH083620). RP is supported by the National Center for Advancing Translational Sciences (KL2TR000450). Additional support was provided by the Lifespan/Tufts/Brown Center for AIDS Research (P30AI042853).
Footnotes
Conflicts of interest: The authors declare no conflicts of interest.
References
- 1.Grant RM, Lama JR, Anderson PL, McMahan V, Liu AY, Vargas L, et al. Preexposure chemoprophylaxis for HIV prevention in men who have sex with men. N Engl J Med. 2010 Dec 30;363(27):2587–99. doi: 10.1056/NEJMoa1011205. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Molina J-M, Capitant C, Spire B, Pialoux G, Cotte L, Charreau I, et al. On-demand preexposure prophylaxis in men at high risk for HIV-1 infection. N Engl J Med. 2015 Dec 3;373(23):2237–46. doi: 10.1056/NEJMoa1506273. [DOI] [PubMed] [Google Scholar]
- 3.McCormack S, Dunn DT, Desai M, Dolling DI, Gafos M, Gilson R, et al. Pre-exposure prophylaxis to prevent the acquisition of HIV-1 infection (PROUD): effectiveness results from the pilot phase of a pragmatic open-label randomised trial. Lancet. 2016 Jan 2;387(10013):53–60. doi: 10.1016/S0140-6736(15)00056-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Smith D, Van Handel M, Wolitski R, Stryker J, Hall H, Prejean J, et al. Vital Signs: estimated percentages and numbers of adults with indications for preexposure prophylaxis to prevent HIV acquisition - United States, 2015. Morb Mortal Wkly Rep. 2015 Nov 27;64(46):1291–5. doi: 10.15585/mmwr.mm6446a4. [DOI] [PubMed] [Google Scholar]
- 5.Flash C, Landovitz R, Giler RM, Ng L, Magnuson D, Wooley SB, et al. Two years of Truvada for pre-exposure prophylaxis utilization in the US. J Int AIDS Soc. 2014;17(4 Suppl 3):19730. doi: 10.7448/IAS.17.4.19730. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Berwick DM. Disseminating innovations in health care. JAMA. 2003 Apr 16;289(15):1969–75. doi: 10.1001/jama.289.15.1969. [DOI] [PubMed] [Google Scholar]
- 7.Herek GM, Gillis JR, Cogan JC. Internalized stigma among sexual minority adults: insights from a social psychological perspective. J Couns Psychol. 2009;56(1):32. [Google Scholar]
- 8.Calabrese SK, Underhill K. How stigma surrounding the use of HIV preexposure prophylaxis undermines prevention and pleasure: a call to destigmatize “Truvada whores.”. Am J Public Health. 2015 Aug 13;105(10):1960–4. doi: 10.2105/AJPH.2015.302816. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Mimiaga MJ, Case P, Johnson CV, Safren SA, Mayer KH. Preexposure antiretroviral prophylaxis attitudes in high-risk Boston area men who report having sex with men: limited knowledge and experience but potential for increased utilization after education. J Acquir Immune Defic Syndr 1999. 2009 Jan 1;50(1):77–83. doi: 10.1097/QAI.0b013e31818d5a27. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Horberg M, Raymond B. Financial policy issues for HIV pre-exposure prophylaxis: cost and access to insurance. Am J Prev Med. 2013 Jan;44(1 Suppl 2):S125–128. doi: 10.1016/j.amepre.2012.09.039. [DOI] [PubMed] [Google Scholar]
- 11.Krakower DS, Jain S, Mayer KH. Antiretrovirals for primary HIV prevention: the current status of pre- and post-exposure prophylaxis. Curr HIV/AIDS Rep. 2015 Mar;12(1):127–38. doi: 10.1007/s11904-014-0253-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Karris MY, Beekmann SE, Mehta SR, Anderson CM, Polgreen PM. Are we prepped for preexposure prophylaxis (PrEP)? Provider opinions on the real-world use of PrEP in the United States and Canada. Clin Infect Dis. 2014 Mar 1;58(5):704–12. doi: 10.1093/cid/cit796. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Krakower D, Ware N, Mitty JA, Maloney K, Mayer KH. HIV providers' perceived barriers and facilitators to implementing pre-exposure prophylaxis in care settings: a qualitative study. AIDS Behav. 2014 Sep;18(9):1712–21. doi: 10.1007/s10461-014-0839-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Marx GE, Bhatia R, Rietmeijer CA. An opportunity too good to miss: implementing human immunodeficiency virus preexposure prophylaxis in sexually transmitted diseases clinics. Sex Transm Dis. 2016 Apr;43(4):266–7. doi: 10.1097/OLQ.0000000000000439. [DOI] [PubMed] [Google Scholar]
- 15.Cohen SE, Vittinghoff E, Bacon O, Doblecki-Lewis S, Postle BS, Feaster DJ, et al. High interest in preexposure prophylaxis among men who have sex with men at risk for HIV infection: baseline data from the US PrEP Demonstration Project. J Acquir Immune Defic Syndr. 2015 Apr;68(4):439–48. doi: 10.1097/QAI.0000000000000479. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Liu AY, Cohen SE, Vittinghoff E, Anderson PL, Doblecki-Lewis S, Bacon O, et al. Preexposure prophylaxis for HIV infection integrated with municipal- and community-based sexual health services. JAMA Intern Med. 2015 Nov 16;:1–11. doi: 10.1001/jamainternmed.2015.4683. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.U.S. Census Bureau . State and County QuickFacts: Rhode Island. Oct, 2015. [Google Scholar]
- 18.RI Department of Health . 2014 Rhode Island HIV/AIDS epidemiologic profile with surrogate data. Providence, RI: Dec, 2015. [Google Scholar]
- 19.Smith DK, Koenig LJ, Martin M, Mansergh G, Heneine W, Ethridge SF, et al. Preexposure prophylaxis for the prevention of HIV infection in the United States – 2014: a clinical practice guideline. US Public Health Service; Centers for Disease Control and Prevention; Atlanta: 2014. [Google Scholar]
- 20.Rhode Island Department of Health . Rhode Island HIV/AIDS/Viral Hepatitis Epidemiologic Profile with Surrogate Data, 2012. Division of Infectious Disease and Epidemiology; Providence, RI: 2013. [Google Scholar]
- 21.Chan PA, Rose J, Maher J, Benben S, Pfeiffer K, Almonte A, et al. A latent class analysis of risk factors for acquiring HIV among men who have sex with men: implications for implementing pre-exposure prophylaxis programs. AIDS Patient Care STDs. 2015 Nov;29(11):597–605. doi: 10.1089/apc.2015.0113. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Mikati T, Bhatia R, Pohl D, Keglovitz K, Buatista-Gutierrez B. Pilot Implementation of PrEP: Active Referral Model in a Chicago Public STI Clinic. Atlanta, GA: 2015. [Google Scholar]
- 23.Coury-Doniger P, DiLaura S, Johnson V, McCaffery R, Scahill M, Schwartz A. Implementation of PrEP Services in an STD Clinic – Where to Start? 2015. [Google Scholar]
- 24.Cohen SE, Vittinghoff E, Bacon O, Doblecki-Lewis S, Postle BS, Feaster DJ, et al. High interest in preexposure prophylaxis among men who have sex with men at risk for HIV infection: baseline data from the US PrEP demonstration project. J Acquir Immune Defic Syndr 1999. 2015 Apr 1;68(4):439–48. doi: 10.1097/QAI.0000000000000479. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Liu A, Cohen S, Follansbee S, Cohan D, Weber S, Sachdev D, et al. Early experiences implementing pre-exposure prophylaxis (PrEP) for HIV prevention in San Francisco. PLoS Med. 2014 Mar;11(3):e1001613. doi: 10.1371/journal.pmed.1001613. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Takahashi TA, Johnson KM, Bradley KA. A population-based study of HIV testing practices and perceptions in 4 U.S. states. J Gen Intern Med. 2005 Jul;20(7):618–22. doi: 10.1111/j.1525-1497.2005.0112.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Kellerman SE, Lehman JS, Lansky A, Stevens MR, Hecht FM, Bindman AB, et al. HIV testing within at-risk populations in the United States and the reasons for seeking or avoiding HIV testing. J Acquir Immune Defic Syndr 1999. 2002 Oct 1;31(2):202–10. doi: 10.1097/00126334-200210010-00011. [DOI] [PubMed] [Google Scholar]
- 28.MacKellar DA, Valleroy LA, Secura GM, Behel S, Bingham T, Celentano DD, et al. Unrecognized HIV infection, risk behaviors, and perceptions of risk among young men who have sex with men: opportunities for advancing HIV prevention in the third decade of HIV/AIDS. J Acquir Immune Defic Syndr 1999. 2005 Apr 15;38(5):603–14. doi: 10.1097/01.qai.0000141481.48348.7e. [DOI] [PubMed] [Google Scholar]
- 29.MacKellar DA, Valleroy LA, Secura GM, Behel S, Bingham T, Celentano DD, et al. Perceptions of lifetime risk and actual risk for acquiring HIV among young men who have sex with men. AIDS Behav. 2007 Mar;11(2):263–70. doi: 10.1007/s10461-006-9136-0. [DOI] [PubMed] [Google Scholar]
- 30.Weinstein ND. Testing four competing theories of health-protective behavior. Health Psychol Off J Div Health Psychol Am Psychol Assoc. 1993 Jul;12(4):324–33. doi: 10.1037//0278-6133.12.4.324. [DOI] [PubMed] [Google Scholar]
- 31.Montgomery MC, Oldenburg CE, Nunn AS, Mena L, Anderson P, Liegler T, et al. Adherence to pre-exposure prophylaxis for HIV prevention in a clinical setting. PloS One. 2016;11(6):e0157742. doi: 10.1371/journal.pone.0157742. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Chan PA, Mena L, Patel R, Oldenburg CE, Beauchamps L, Perez-Brumer AG, et al. Retention in care outcomes for HIV pre-exposure prophylaxis implementation programmes among men who have sex with men in three US cities. J Int AIDS Soc. 2016;19(1):20903. doi: 10.7448/IAS.19.1.20903. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.


