Abstract
In 2013, the Nutrition for Growth Summit called for a Global Nutrition Report (GNR) to strengthen accountability in nutrition so that progress in reducing malnutrition could be accelerated. This article summarizes the results of the first GNR. By focusing on undernutrition and overweight, the GNR puts malnutrition in a new light. Nearly every country in the world is affected by malnutrition, and multiple malnutrition burdens are the “new normal.” Unfortunately, the world is off track to meet the 2025 World Health Assembly (WHA) targets for nutrition. Many countries are, however, making good progress on WHA indicators, providing inspiration and guidance for others. Beyond the WHA goals, nutrition needs to be more strongly represented in the Sustainable Development Goal (SDG) framework. At present, it is only explicitly mentioned in 1 of 169 SDG targets despite the many contributions improved nutritional status will make to their attainment. To achieve improvements in nutrition status, it is vital to scale up nutrition programs. We identify bottlenecks in the scale-up of nutrition-specific and nutrition-sensitive approaches and highlight actions to accelerate coverage and reach. Holding stakeholders to account for delivery on nutrition actions requires a well-functioning accountability infrastructure, which is lacking in nutrition. New accountability mechanisms need piloting and evaluation, financial resource flows to nutrition need to be made explicit, nutrition spending targets should be established, and some key data gaps need to be filled. For example, many UN member states cannot report on their WHA progress and those that can often rely on data >5 y old. The world can accelerate malnutrition reduction substantially, but this will require stronger accountability mechanisms to hold all stakeholders to account.
Keywords: malnutrition, SDGs, accountability, progress, indicators
Introduction
Malnutrition, encompassing both undernutrition and overweight, is a problem facing virtually every country in the world. The consequences of malnutrition have fundamental implications throughout the life cycle: reduced chances of survival, increased risk of acute and chronic disease, impaired learning in school, and lower economic productivity. The consequences are transmitted across generations via maternal-child nutrition linkages (1–3).
Currently, political commitment to malnutrition reduction is high. For example, 54 countries have chosen to become members of the Scaling Up Nutrition (SUN)28 movement; the second International Conference on Nutrition in 2014 had a strong focus on all forms of malnutrition; resource allocation for the prevention and treatment of malnutrition is on the rise as indicated by the commitments made by many organizations at the Nutrition for Growth (N4G) summit in 2013; the Lancet nutrition series of 2008 and 2013 brought together what we know about preventing and reducing malnutrition; and, unlike the Millennium Development Goal framework, the 2013 High Level Panel on the Post 2015 Development Agenda (4) explicitly recommends nutrition as an explicit feature of one of its proposed goals.
The imperative now is to sustain and intensify this commitment and turn it into action that accelerates nutrition improvements. To this end, in 2013 the N4G stakeholders called for a Global Nutrition Report (GNR) to track the world’s progress in improving nutrition, to strengthen its accountability to meet commitments, and to identify actions to accelerate progress (5). The GNR is produced by an independent expert group empowered by the N4G stakeholder group [Governance details of the GNR are found on the GNR website (6)].
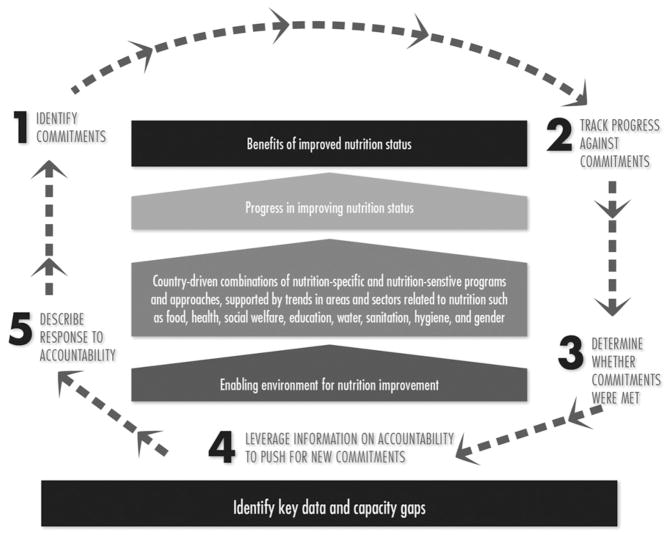
This article summarizes results and conclusions from the inaugural GNR. The GNR is global in nature, bringing together disparate data on 76 indicators of nutrition status, programs, policies, resources, legislation, and institutional arrangements, establishing a baseline for them to be tracked annually for the 193 UN member states. It draws on the data to describe progress in improving nutrition status, the coexisting burdens of malnutrition, the state of coverage of nutrition interventions and practices, trends in the sectors that support nutrition, nutrition spending trends, the state of data on nutrition policies, laws, and institutional arrangements. The GNR also collects data on progress toward the recent N4G commitments made in 2013 by a wide range of stakeholders. The GNR is action oriented. Drawing on original analyses and several highlighted country case studies of change, it identifies actions to accelerate progress in nutrition, suggests ways of filling key data gaps, and makes concrete recommendations on how nutrition accountability can be strengthened to better deliver action (Table 1). The report’s framework is summarized in Figure 1.
TABLE 1.
Key messages of the Global Nutrition Report1
| 1 | Multiple malnutrition burdens are the “new normal.” Countries are increasingly dealing with complex combinations of malnutrition problems. This strengthens the case for strategic whole-of-society approaches to addressing malnutrition. |
| 2 | Nearly every country in the world is affected by malnutrition. The potential for lesson learning is enormous but is not being exploited. |
| 3 | The world is off track to meet the 2025 WHA targets for nutrition. Nevertheless, many countries are making good progress on key WHA indicators. More needs to be understood about how this progress is being achieved. |
| 4 | Nutrition needs to be more strongly represented in the SDG framework. At present, it is only explicitly mentioned in 1 of 169 targets. |
| 5 | Nutrition-specific interventions have poor coverage. Countries and external funders need to invest in the capacity to scale up these interventions and their impact. |
| 6 | Nutrition-sensitive approaches are slow to take off. More guidance needs to be given to nutrition allies in sectors such as agriculture, social protection, water, sanitation, and hygiene about how and why their investments can become more nutrition sensitive. |
| 7 | Accountability in nutrition is in need of strengthening. New accountability mechanisms need piloting and evaluation. Financial resources to nutrition need to be made explicit. Nutrition spending targets need to be established to influence resource allocation norms. |
| 8 | Data gaps in nutrition need to be filled by governments. Forty percent of UN member states cannot report on the WHA progress. Of the countries that can, 40% of the data they are using are >5 y old. |
| 9 | Malnutrition rates can be reduced more quickly than they are now. Strengthening accountability is one way to build greater political commitment to do so. |
SDG, Sustainable Development Goal; WHA, World Health Assembly.
FIGURE 1.
The Global Nutrition Report’s conceptual framework.
Data Sources and Methods
The GNR presents 76 indicators from different data sources selected on the basis of their methodologic quality and global representativeness. Most data for child anthropometry, intervention coverage, and child feeding practices come from nationally representative household surveys, primarily the Demographic and Health Surveys and the Multiple Indicator Cluster Survey. The report uses databases provided by UNICEF, WHO, the World Bank, FAO, the UN Population Division, and the UN Educational, Scientific and Cultural Organization (UNESCO). The UNICEF/WHO/World Bank’s 2013 Joint Child Malnutrition Estimates form the backbone of analysis of child nutritional status and of tracking progress toward the World Health Assembly (WHA) targets (7).
The report uses some modeled estimates in the absence of adequate survey data. The WHO Global Health Observatory Data Repository is used for estimates of the prevalence of adult overweight and obesity and risk factors for noncommunicable diseases. Data on sanitation and safe water coverage are from WHO/UNICEF’s Joint Monitoring Program, and data on anemia in women of reproductive age are from a study by Stevens et al. (8).
Data on food supply are from FAO and data on severe acute malnutrition geographical coverage are from UNICEF/Coverage Monitoring Network/Action Against Hunger (ACF International). The GNR’s data for financial resources, policy and legislation, and institutional arrangements indicators are from UNICEF, WHO, the International Food Policy Research Institute, the Food Fortification Initiative, the International Labor Organization, the Institute of Development Studies, and the SUN Movement.
Data analysis was carried out by the GNR’s Secretariat based at the Institute of Development Studies, with additional technical input and assistance from partners at WHO and UNICEF. The report follows UN country and regional classification and naming conventions.
The summary measure for the prevalence of malnutrition and intervention coverage rates at the regional and subregional levels is the population-weighted mean, with the UN Development Program’s 2012 population estimates used as analytical weights. Rates are calculated when available data covered ≥50% of the regional or subregional population.
Trends in intervention coverage (nutrition-specific and nutrition-sensitive), underlying determinants (including food supply, water and sanitation, female education, and health worker density), and government expenditure in sectors related to nutrition (health, agriculture, education, and social protection) are calculated for milestone years: 1990, 2000, 2010, and for the most recent year when data are available.
Progress on WHA indicators at country levels, and summarized by regions, is assessed by presenting baseline (latest estimate in 2005–2012 for stunting, wasting, and overweight and 2011 for anemia) levels of malnutrition and current annual average rates of reduction or increase (AARRs or AARIs, respectively) compared with required rates when global targets apply. These on- and off-course rules are simply to allow global comparisons using a common denominator (9). Countries will need to set their own targets and assess whether they are on and off course on the basis of them.
Assessments of progress toward N4G commitments was made as follows: 1) identify the specific commitment in the N4G Compact document; 2) remind the signatory of this commitment asking them to report progress via a template, tailored to each group; 3) clarify issues with those who responded; 4) enter the final responses into a set of detailed online N4G Commitment Tracking tables; and 5) make an assessment of progress. Assessment consisted of 2 of the writing team reviewing the detailed online tables that show progress for each signatory, making independent assessments and then (twice) jointly reviewing each of the 2 independent assessments. All data sources are reported in full in the Global Nutrition Report 2014 (10).
Findings
Multiple malnutrition burdens are the “new normal”
To date, the worlds of undernutrition and of overweight (and obesity and diet-related noncommunicable disease) have operated largely independently of each other. However, once undernutrition and overweight data are brought together, the global picture of malnutrition changes dramatically.
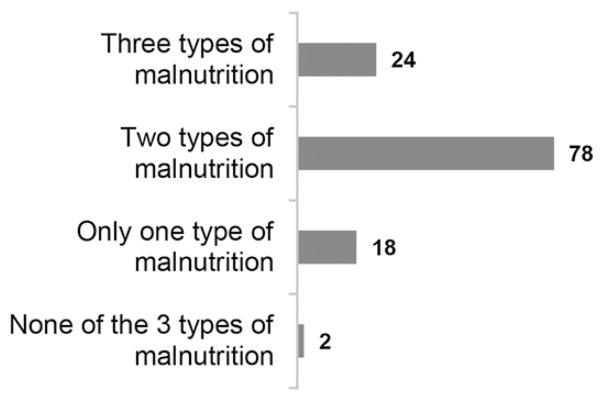
For example, of the 122 countries in the world with comparable data, all except 2 countries experience 1 of these 3 common forms of malnutrition: under-5 stunting, anemia in women of reproductive age, or adult overweight. Most countries experience multiple forms of malnutrition, and 24 countries show all 3 forms of malnutrition (Figure 2).
FIGURE 2.
Number of countries experiencing multiple burdens of malnutrition.
These different forms of malnutrition need to be considered holistically. They are connected at a political level because they compete for resources and attention (11) and at the programmatic level because the potential for unintended consequences is substantial (12). However, complexity is not an excuse for inaction. Rather, it is a call for more careful prioritizing of actions, with an enhanced understanding of potential trade-offs. The need for the development of tools and strategies for sequencing of nutrition-relevant actions in complex contexts is urgent. Multiple burdens and trends toward decentralization of nutrition programming [e.g., (13)] highlight the need for disaggregated data on nutrition outcomes. The realization that all countries face malnutrition opens the door for more cross-national collaboration and learning on what works to achieve good nutrition.
Although global progress in nutrition status outcomes is too slow, many countries are making good progress
Unfortunately, the world is not on course to meet any of the 6 nutrition WHA global targets for 2025. Table 2 lists the 6 WHA nutrition global targets and the extent of global progress toward them. For stunting and exclusive breastfeeding there is some progress, but for anemia, low birth weight, and wasting the global figures are static, and for under-5 overweight rates they are increasing. Countries make up the global numbers, and their progress can be assessed in 3 ways. First and foremost, individual nations will set their own targets and these are under development. Second, country rates of progress can be compared to the required global rates to meet the global targets, as shown in the last column of Table 2. Nearly one-fifth of countries are above the rate of reduction in stunting required to meet the global target. For under-5 overweight, half the countries show declining rates. For exclusive breastfeeding, over half of the countries are increasing their rates faster than the global required rate. And well over half of the countries that have data on wasting show declines. Amid the global picture, many countries are making good progress.
TABLE 2.
Progress toward the global WHA nutrition targets1
| WHA target | Baseline year(s) | Baseline status | Target for 2025 | Required global average annual rate of change | Globally on course? | Comments2 | Number of countries above and below required global rate of change |
|---|---|---|---|---|---|---|---|
| Stunting: 40% reduction in the number of children under 5 who are stunted3 | 2012 | 162 million | ~100 million (~15% prevalence) | 3.9% AARR | No | Current pace projects 130 million by 2025 (20% reduction) | AARR is above or equal to required rate: 21 countries; AARR is below required rate: 89 countries |
| Anemia: 50% reduction in anemia in women of reproductive age | 2011 | 29% | 15% | 5.2% AARR | No | Very little movement (was 32% in 2000) | — |
| Low birth weight: 30% reduction in low birth weight | 2008–2012 | 15% | 10% | 2.74% AARR | No | Little progress globally | — |
| Under-5 overweight: no increase in childhood overweight | 2012 | 7% | 7% | No | Upward trajectory is unchecked | AARR is constant or decreasing: 50 countries; AARR is increasing: 51 countries | |
| Exclusive breastfeeding: increase the rate of exclusive breastfeeding in the first 6 mo up to at least 50% | 2008–2012 | 38% | 50% | 2.11% AARI | No | 37% in 2000, 41% in 2012 | AARI is above or equal to required rate: 59 countries4; AARI is below required rate: 48 countries |
| Wasting: reduce and maintain childhood wasting to <5% | 2012 | 8% | <5% | No | No progress (was 8% globally in 2013)4 | Wasting rate is constant or decreasing: 73 countries; rate is increasing: 51 countries [see Table 3.2 in the GNR (10)] |
Data from reference 9. AARI, average annual rate of increase; AARR, average annual rate of reduction; GNR, Global Nutrition Report; WHA, World Health Assembly.
For more on the methods behind the WHA stunting target, see reference 14.
These are AARIs estimated by the writing team on the basis of the last 2 available estimates for exclusive breastfeeding in UNICEF (15). Formal AARIs from UNICEF/WHO are not available at this time.
These figures are from reference 7.
The third way of assessing country progress is to apply the global targets on a country-by-country basis. In other words, how many countries would be on course to make their proportionate contribution to the WHA global targets? By using data from the most recent UNICEF/WHO/World Bank joint global database (7) and estimates from WHO on the required rates of change in country-level indicators to meet the global target applied at the country level (9), we apply rules proposed by WHO (9) for determining whether a country is on or off course to meet the global WHA targets.29
Of the 99 countries that have data on all 4 WHA indicators for which rules exist (stunting, wasting, overweight, and anemia), only one—Colombia—is on course to meet all 4 targets by 2025. Thirty-one countries are not on course to meet any of the 4 targets. More encouragingly, more than two-thirds of all countries that have data on all 4 indicators will meet at least one goal. There is no regional pattern to whether or not countries are on or off course.
On an indicator-by-indicator basis, anemia is the indicator for which most countries are finding it difficult to make progress (Figure 3).30
FIGURE 3.
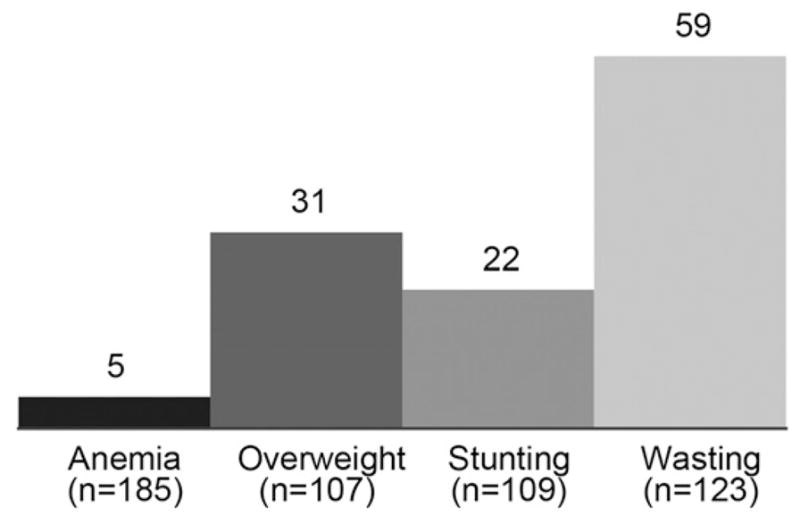
Number of countries that are on course to meet each World Health Assembly global target.
The 5 countries on course for anemia reduction are Burundi, Colombia, Kenya, Vanuatu, and Vietnam. Wasting is the indicator for which the largest number of countries are making progress. This result is based not on AARRs but rather on whether wasting is <5% (on course) or ≥5% (off course).31 The 59 countries on course for wasting reduction include Brazil, China, and the United States. These 59 countries represent 39% of all children under age 5 in the 123 countries with available data. For stunting reduction, 22 countries are on course, including China, Turkey, and Vietnam. These 22 countries represent 23% of all children under age 5 in the 109 countries with available data. Finally, 31 countries are on course for under-5 overweight reduction of the 107 with available data. The 31 countries, which include India, Nigeria, and the United States, represent 45% of all children under age 5 in these 107 countries.
Nutrition needs a stronger place within the Sustainable Development Goals
The WHA nutrition goals are a key accountability tool for nutrition. For development more generally, the Sustainable Development Goals (SDGs) will be the world’s post-2015 accountability mechanism. The UN’s Open Working Group has made an initial proposal for 17 SDGs and 169 accompanying targets (17). Improvements in nutrition status will make substantial contributions to the attainment of many of SDGs (Table 3) and, in turn, will benefit from improvements in them.
TABLE 3.
Contribution of nutrition to the SDGs1
| Proposed SDG | Contribution of nutrition to SDG |
|---|---|
| End poverty in all its forms everywhere | Preventing stunting in children <36 mo old makes it less likely that they will live in households below the poverty line (18) |
| End hunger, achieve food security and improved nutrition, and promote sustainable agriculture | Explicitly refers to 2 WHA indicators (stunting and wasting) Optimal breastfeeding and complementary feeding represent the best dietary start in life (3) A focus on pre-pregnancy and the first part of 1000 d reduces risk of low birth weight and improves women’s nutrition status (2) |
| Ensure healthy lives and promote well-being for all at all ages | Micronutrient malnutrition and women stunted in childhood, link to maternal mortality and low birth weight; 45% of all under-5 deaths linked to undernutrition (2) Link of stunting to later NCD onset (19) Reducing overweight and obesity for fewer NCDs (20) Reducing infectious diseases that are linked to nutrition-related morbidity and mortality |
| Ensure inclusive and equitable quality education and promote lifelong learning opportunities | Links between nutrition status in first 1000 d, early child development and school grade completion, and achievement, particularly for adolescent girls (1) |
| Achieve gender equality and empower all women and girls | Improving the nutrition status of girls, adolescents, and women increases their ability to perform well at school and in the workforce (18) |
| Ensure availability and sustainable management of water and sanitation for all | Improvements in nutrition outcomes help reinforce the need for action on water, sanitation, and hygiene as critical determinants of nutrition (21) |
| Promote sustained, inclusive, and sustainable economic growth; full and productive employment; and decent work for all | Undernutrition cuts GNP by at least 8–11% (22) Earned income is improved by stunting prevention (18) |
| Reduce inequality within and among countries | Stunting rates by wealth quintile demonstrate how current inequality perpetuates future inequality (2) |
| Ensure sustainable consumption and production | Research on sustainable food systems and sustainable diets can offer structure and indicators to this policy debate (23) |
GNP, gross national product; NCD, noncommunicable disease; SDG, Sustainable Development Goal; WHA, World Health Assembly.
Despite these contributions, nutrition is presently under-represented in the SDG framework. For example, 45% of global deaths of children under the age of 5 can be attributed jointly to fetal growth restriction, suboptimum breastfeeding, stunting, wasting, and deficiencies of vitamin A and zinc (2). In addition, the economic benefit-cost ratio of preventing undernutrition in Africa is 16:1 and the economic costs of obesity are estimated at 5% of gross national product in China. Despite the substantial burdens imposed on development by malnutrition, only 2 of the 6 WHA global nutrition goals are mentioned in the SDGs (stunting and wasting in children under 5 y of age) and nutrition is explicitly referred to in only 1 of the 169 targets. The GNR concludes that the remaining WHA nutrition indicators (under-5 overweight, anemia in women of reproductive age, exclusive breastfeeding, and low birth weight) need to be incorporated under the other remaining SDGs, subgoals, and targets. For example, low birth weight, exclusive breastfeeding, and anemia in women of reproductive age could be indicators for the stated subgoal (3.2) of “by 2030 end preventable deaths of newborns and under 5 children,” (17) and under-5 overweight rates could be an indicator for the stated subgoal (3.4) of “by 2030 reduce by one-third pre-mature morality from non-communicable diseases (NCDs) through prevention and treatment” (17).
In addition, other indicators that are important for a range of SDGs but also for nutrition improvement need to be identified and lobbied for. For example, coverage rates for nutrition-specific interventions could be indicators for the stated subgoal of “achieve universal health coverage” and there should be discussion and negotiation on the subgoals for hunger, water, sanitation, social protection, poverty and inequality, education, and women’s participation to determine if they can be framed in ways that are more helpful to nutrition.
As yet, no SDG nutrition targets have been set for 2030. The WHA targets are set for 2025. The GNR recommends that the 2030 targets should not be “business as usual” 5-y extrapolations of the WHA 2025 targets. The WHA targets are determined on the basis of historical trends as of 2012, based largely on data up to 2010. We should consider being more ambitious for the 2030 targets because of new data, new analysis, and new commitments. The new data are surveys for India (preliminary) and for the Indian state of Maharashtra. Both surveys show rates of decline in stunting that are far in excess of the rates assumed in 2012. Because India accounts for >40% of global stunting, this matters a great deal. By using a new analysis of the relation between 6 underlying drivers of nutrition (e.g., improved water and sanitation coverage, gender equity, and measures of the quantity and quality of food supply) and stunting rates (24), the GNR suggests that with challenging but realistic increases in the levels of these drivers the WHA targets can be met and even exceeded. Finally, the new pledges from the N4G in 2013, the expanding membership of SUN, and the commitments that will be embodied in the second International Conference on Nutrition all need to be taken into account when formulating the 2030 targets.
Nutrition interventions need to be scaled up much more quickly
Because a person’s nutritional status depends on a range of immediate, underlying, and basic determinants and their interactions, nutrition investments may take various forms to address these determinants (2). Nutrition-specific programs address the immediate determinants (e.g., inadequate diet and disease burden) of nutrition status and are found in a range of policy areas, such as health, humanitarian relief, and food processing (3). Nutrition-sensitive programs and approaches incorporate explicit nutritional goals or actions and address the underlying determinants of nutrition status (e.g., food security, health access, healthy household environment, and care practices) and are found in a wide range of policy areas such as the following: agriculture; education; water, sanitation, and hygiene; social protection; women’s empowerment; and health (25). Enabling environment investments address the basic determinants of nutrition status such as governance, income, and equity. These take the form of laws, regulations, policies, investments in economic growth, and improvements in governance capacity (26). Efforts to improve nutritional status can come from investments that address all 3 levels of determinants: immediate, underlying, and basic. The aim should be to find the most potent blend of determinants, at scale, given the need, capacities, and political opportunities in each context.
Nutrition-specific intervention coverage is too low
The scaled-up coverage of nutrition-specific interventions is crucial for undernutrition reduction (3). The GNR summarizes the state of coverage data for the 10 nutrition-specific interventions in Bhutta et al. (3), plus zinc treatment for diarrhea (27) and universal salt iodization (also a proven nutrition-specific intervention). Data are only readily available for more than a handful of countries for vitamin A supplementation for 6- to 59-mo-olds, universal salt iodization, and zinc treatment for diarrhea. This is because programs have not been scaled up (e.g., preventive zinc supplementation, multiple micronutrient supplementation, calcium supplementation in pregnancy) or because coverage data are missing (e.g., the treatment of moderate or severe acute malnutrition). Although expanded program coverage is vital, it is only valuable if it leads to expanded impact. It is thus important to focus on maintaining and improving program effectiveness. Implementation research is important here (28).
Trends in sectors that are important for nutrition are positive but too slow
The FAO’s estimate of hunger (what it terms “undernourishment”) is based on food supply data that are converted into the percentage of the population below a minimum energy cutoff. Undernourishment rates are declining, although the absolute numbers of hungry individuals in sub-Saharan Africa are increasing (29). At the same time, the GNR shows that the percentage of the population that is above an upper energy threshold is increasing steadily, leaving the share of the population in the healthy range between the 2 cutoffs static at 60%. Access to improved water and sanitation services is steadily improving, but there are large coverage gaps in Eastern, Western, and Middle Africa for water and in South and South East Asia for sanitation. Girls’ secondary education enrollment is increasing steadily and now exceeds 50% in Africa. Health worker population density remains very low in Africa and half the rate of Asia. Government expenditures on these broad categories—agriculture, education, health, and social protection—vary between and within regions. Social protection spending is increasing rapidly in many African and Asian countries, providing an opportunity to incorporate nutrition into those programs.
The evidence base is weak on how to make interventions that address underlying determinants more nutrition sensitive. Although the GNR offers some specific ideas for agriculture, social protection, education, health, water, sanitation, and hygiene, there are several actions that nutrition stakeholders need to take, whatever the sector. These include making the case to other sectors that they can further their own goals by using a nutrition lens; incorporating nutrition goals, indicators, and targets in sector strategies and log-frames; work with partners to use a nutrition lens to develop specific nutrition-enhancing practices and actions within their sector; deploy interventions in high malnutrition areas; engage women in design and implementation; focus on key stages in the life cycle; and incorporate nutrition-specific interventions within broader platforms (25, 30–33).
Investments in nutrition are probably increasing, but the picture is unclear
Most countries are unable, at present, to identify and track their financial commitments to nutrition (34). This is due to a combination of factors: lack of agreement on what to include and exclude, an absence of data that are sufficiently disaggregated to apportion spending to nutrition, and a lack of capacity to undertake a classification exercise. Several tools exist to accomplish this, and investments will need to be made to build the organizational capacity to use them.
Thirteen external funders provided data to the GNR on their nutrition investments. Between 2010 and 2012, commitments and disbursements to nutrition-specific interventions increased by 39% and 30%, respectively. Nutrition-sensitive commitments declined by 14%, but nutrition-sensitive disbursements for the 10 donors that reported such data increased by 19%. Although these changes are encouraging, the percentage of external funding to nutrition in total in 2012 was only marginally above 1% of all overseas development assistance. A nutrition spending target for governments and external funders would be a way of focusing more attention on financial resources to nutrition. It would need to be complemented by improved tracking of spending to ensure that the quality of spending is also improved.
The scope and quality of policies, laws, and institutions is important for scale-up
Policies, laws, and institutions are important for scaling up nutrition actions and impacts. The GNR reports on efforts to assess commitment to nutrition of governments [Hunger and Nutrition Commitment Index (35)], businesses [Access to Nutrition Index (36)], and the extent to which the food-health environment supports healthy choices [FOOD-INFO (37)]. The SUN process score approach is noteworthy for being a participatory measurement process that stimulates reflection and action by nutrition stakeholders on whether they are aligning their institutions to nutrition priorities (38).
Accountability in nutrition needs strengthening
The features of nutrition outcomes and actions—short- and long-term effects, invisibility of some consequences, and the need for alliances—make the process of identifying commitments, and then monitoring them for accountability, more complex than for many other development issues.
Reporting on N4G commitments: challenges and conclusions
As well as reporting on publicly available data, the GNR also sought primary, self-reported data on whether the 96 N4G signatories met their 2013 commitments. Reporting on the commitments was challenging for all groups of signatories. Nevertheless, 90% of them responded to requests for updates against their N4G commitments. Very few signatories were assessed by the GNR as “off course,” although there were many “not clear” assessments due to the vagueness of the initial commitment and of the response. In addition, financial tracking systems were not in place to distinguish between nutrition-specific and -sensitive spending and the infrequent implementation of national nutrition surveys made tracking nutrition status commitments difficult. In brief, the signatories were willing to be held to account, but the mechanisms to do so were weak. Notwithstanding these challenges, there were no obvious causes for concern from any group in terms of progress toward N4G targets at this stage in the 2013–2020 reporting period.
Ways to strengthen accountability in nutrition
The GNR outlines many ways in which nutrition accountability can be strengthened. The role of civil society actors is particularly important, although they need support if they are to be more effective. The reach and ability of civil society organizations to mobilize are invaluable and they are mostly credible in holding governments and others to account. There is potential for citizens to hold duty bearers to account via community scorecards, social audits, and other citizen-level accountability mechanisms (39, 40). National evaluation platforms (41) that bring together existing data and capacities are another promising set of interventions to be piloted and evaluated.
A data revolution is needed
Credible and timely data are the bedrock of accountability (42). Unfortunately, there are many data gaps in nutrition outcomes, outputs, and inputs. For example, 40% of the 193 UN member countries cannot track >2 of the 4 WHA indicators. For the countries that can report on WHA indicator progress, data are often outdated. For example, nearly 40% of the baseline surveys in Table 2 are from the period 2005–2009. It is challenging to make public policy on the basis of outdated data.
To identify data gaps beyond the WHA indicators, we asked, “Where are data gaps constraining attention to important issues and where are they holding back important actions?” We identified 4 indicators—anemia, overweight, wasting, and low birth weight—in which weak data (lack of detailed food consumption data, more accurate assessments of adult obesity, and outdated adjustments to birth weight) are likely to be holding back action. We also identified gaps—in program coverage data for nutrition-specific programs, financial tracking data, data on a system’s capacity to scale, program cost data, and disaggregated nutrition status data—that are likely holding back the scale-up of nutrition-specific and nutrition-sensitive interventions. A lack of broadly based but high-quality country case studies is also stifling learning about the effectiveness of different strategies, approaches, and combinations of interventions in reducing malnutrition at scale. Decisions about which data gaps are most important to fill need to be undertaken at the national level, based on nutrition policies, plans, and strategies.
Priority actions for the next 12 mo
Several actions are essential if current levels of commitment to nutrition are to be sustained, intensified, and more effectively converted into impact. First, influential nutrition stakeholders need to work hard to ensure that nutrition is embedded more firmly within the SDG framework. This entails 1) making the case for the inclusion of all 6 WHA indicators within the suite of SDGs, 2) identifying other indicators that are relevant for nutrition (e.g., improved water and sanitation coverage) and making sure they are included and defined in ways that are most useful to nutrition, and 3) establishing inspiring yet attainable 2030 targets for the WHA indicators.
Second, several countries need to demonstrate that it is feasible to track resource allocations to nutrition actions. The methods do not have to be exactly comparable across countries if this is likely to slow down the production of credible estimates. Without such estimates, it is impossible to hold governments to account for nutrition-specific or nutrition-sensitive investments. A target for spending on nutrition also needs to be developed, either in relation to health or total government expenditure. This will promote transparency and help shift norms about optimal nutrition spending levels.
Third, more analysis needs to be done on coverage levels of nutrition-specific interventions. What are they for different countries and regions and why are some countries doing better than others in scaling up? External funding figures suggest that investments in nutrition-sensitive interventions are only twice those of nutrition-specific interventions. If this is a reliable guide to country spending on nutrition sensitive actions—and given the large sectoral budgets that the nutrition-sensitive interventions are carved out of—the current levels of spending seem low. More guidance and examples are needed on what design features make an intervention at the underlying determinant level become “nutrition sensitive” (43). This will give confidence to those who are being asked to scale up spending in this area.
Fourth, innovations in improving stakeholder accountability in nutrition need to be encouraged, piloted, and evaluated. Can community feedback play a key role in signaling a lack of fidelity in program implementation and will this improve fidelity? Will the tracking of commitments at the national or business levels change the behavior of governments or businesses? Can mobile phones be used to highlight failures in implementation of nutrition programs and will this lead to improved implementation? These questions need to be answered with rigorous impact assessments.
Fifth, the data gaps that are holding back priority actions need to be addressed. We identify 5 ways to fill key gaps: 1) use existing data better, 2) strengthen existing data collection quality, 3) improve data comparability across countries, 4) improve the frequency of data collection, and 5) collect new data where there is not enough for good accountability. All of these approaches require complementary investments in capacity. Capacities at the individual, organization, and system level are needed if nutrition actions are to be scaled and deliver the expected impact, yet they are often overlooked by potential funders who often do not know where to begin investing. Better data on capacity needs and gaps will help mobilize and guide investments in this vital area (44).
Finally, we need more country-level analyses of what is facilitating and holding back nutrition improvements. It is at the national and subnational level where nutrition theory becomes practice. How do interventions fit together? How do stakeholders work together? Where are the weak links in the nutrition chain? How do political, capacity, and technical considerations interact? Documenting the different pathways to improved nutrition status provides inspiration and learning for all countries. Research funders and scientific journals need to encourage more high-quality country case studies.
Improving nutrition is a quintessential 21st century challenge
Malnutrition affects all countries and crosses generational boundaries. Confronting it requires collaborations across sectors and disciplines. It requires all groups in society—governments, civic organizations, and businesses—to come together to address it. These features are typical of other 21st century development challenges such as mitigating and adapting to climate change, managing resource scarcity, and building resilient societies. But the world does not have to wait until the end of the 21st century to see the demise of malnutrition. We know what works. Commitment levels have never been higher. Stronger accountability mechanisms can help convert this energy into impact. They can provide greater transparency in commitments and greater clarity on progress and can offer more accurate signposts to action. Critically, stronger accountability mechanisms empower all stakeholders to put pressure on those who are most responsible for accelerating the world’s nutrition status to actually do so.
Acknowledgments
We acknowledge the contributions of Catherine Gee of the International Food Policy Research Institute for her support in preparing this manuscript. LH, KB, KE, and JF analyzed the data, performed the statistical analysis, and generated the figures; MB, EB, and JK provided data and advice; LH wrote the manuscript and had primary responsibility for the final content; and EA, MAB, AA, ZB, EC, MdO, RF-A, PF, EK-M, ENK, HN, RN, SO, YM-P, J Randel, J Requejo, TS, EU, and KSR added revisions to the text. All authors read and approved the final manuscript.
Footnotes
Supported by 1000 Days, the Bill & Melinda Gates Foundation, the Children’s Investment Fund Foundation, the European Commission, the Government of Canada, Irish Aid, the UK Department for International Development, and the CGIAR Agriculture for Nutrition and Health Programme. This is a free access article, distributed under terms (http://www.nutrition.org/publications/guidelines-and-policies/license/) that permit unrestricted noncommercial use, distribution, and reproduction in any medium, provided the original work is properly cited.
Author disclosures: L Haddad, E Achadi, M Ag Bendech, A Ahuja, K Bhatia, Z Bhutta, M Blössner, E Borghi, E Colecraft, M de Onis, K Eriksen, J Fanzo, R Flores-Ayala, P Fracassi, E Kimani-Murage, E Nago Koukoubou, J Krasevec, H Newby, R Nugent, S Oenema, Y Martin-Prével, J Randel, J Requejo, T Shyam, E Udomkesmalee, and KS Reddy, no conflicts of interest.
The findings and conclusions in this report are those of the authors and do not necessarily represent the views or the official position of the CDC.
The full report, technical notes, and nutrition country profiles can be found at: www.globalnutritionreport.org. Statements of related interests of authors are available on the Global Nutrition Report website at: http://globalnutritionreport.org/governance/ieg/.
GNR, Global Nutrition Report; N4G, Nutrition for Growth; SDG, Sustainable Development Goal; SUN, Scaling Up Nutrition; WHA, World Health Assembly.
The Global Nutrition Report Independent Expert Group alone is responsible for the classification of countries in this report, which does not necessarily represent the views or assessments of WHO. WHO will report on progress made toward the achievement of the WHA global nutrition targets at its 68th WHA session in May 2015.
Mason et al. (16) argue that addressing anemia urgently requires scaling up effective intervention programs such as supplementation with iron and folic acid or multiple micronutrients, fortification of staple foods or condiments, and disease control measures such as malaria control and deworming. They suggest that the lack of attention to this issue stems from the lack of awareness of both its pervasiveness and the slow rate of progress in reducing it.
Wasting trends between surveys that are several years apart are not considered meaningful by WHO, and so AARR is not used as a rule for determining whether countries are on or off course.
References
- 1.Adair LS, Fall CHD, Osmond C, Stein AD, Martorell R, Ramirez-Zea M, Sachdev HS, Dahly DL, Bas I, Norris SA, et al. Associations of linear growth and relative weight gain during early life with adult health and human capital in countries of low and middle income: findings from five birth cohort studies. Lancet. 2013;382:525–34. doi: 10.1016/S0140-6736(13)60103-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Black RE, Victora CG, Walker SP, Bhutta ZA, Christian P, de Onis M, Ezzati M, Grantham-McGregor S, Katz J, Martorell R, et al. Maternal and child undernutrition and overweight in low-income and middle-income countries. Lancet. 2013;382:427–51. doi: 10.1016/S0140-6736(13)60937-X. [DOI] [PubMed] [Google Scholar]
- 3.Bhutta ZA, Das JK, Rizvi A, Gaffey MF, Walker N, Horton S, Webb P, Lartey A, Black RE. Evidence-based interventions for improvement of maternal and child nutrition: what can be done and at what cost? Lancet. 2013;382:452–77. doi: 10.1016/S0140-6736(13)60996-4. [DOI] [PubMed] [Google Scholar]
- 4.High Level Panel on the Post-2015 Development Agenda. Goal 5: ensure food security and good nutrition. Report of the High-Level Panel of Eminent Persons on the Post-2015 Development Agenda. [cited 2014 Sep 23]. Available from: http://report.post2015hlp.org/digital-report-goal-5-ensure-food-security-and-good-nutrition.html.
- 5.UK Government. Nutrition for Growth commitments: executive summary. 2013 [cited 2014 Nov 11]. Available from: https://www.gov.uk/government/uploads/system/uploads/attachment_data/file/207274/nutrition-for-growth-commitments.pdf.
- 6.International Food Policy Research Institute. Global Nutrition Report: governance. 2014 doi: 10.3945/an.115.008599. [cited 2014 Dec 12]. Available from: http://global-nutritionreport.org/governance/ [DOI] [PMC free article] [PubMed]
- 7.United Nations Children’s Fund; World Health Organization; The World Bank. UNICEF-WHO-World Bank 2013 Joint Child Malnutrition Estimates. 2014 [cited 2014 Nov 11]. Available from: http://www.who.int/nutgrowthdb/estimates2013.
- 8.Stevens GA, Finucane MM, De-Regil LM, Paciorek CJ, Flaxman SR, Branca F, Peña-Rosas JP, Bhutta ZA, Ezzati M. Global, regional, and national trends in haemoglobin concentration and prevalence of total and severe anemia in children and pregnant and non-pregnant women for 1995–2011: a systematic analysis of population-representative data. Lancet Glob Health. 2013;1:e16–25. doi: 10.1016/S2214-109X(13)70001-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.WHO. Global targets 2025: what is measured gets done. 2014 [cited 2014 Aug 26]. Available from: http://www.who.int/nutrition/globaltargets_indicators.
- 10.International Food Policy Research Institute. Global Nutrition Report 2014: actions and accountability to accelerate the world’s progress on nutrition. Washington (DC): International Food Policy Research Institute; 2014. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Nisbett N, Gillespie S, Haddad L, Harris J. Why worry about the politics of childhood undernutrition? World Dev. 2014;64:420–33. [Google Scholar]
- 12.Leroy JL, Gadsden P, González de Cossío T, Gertler P. Cash and in-kind transfers lead to excess weight gain in a population of women with a high prevalence of overweight in rural Mexico. J Nutr. 2013;143:378–83. doi: 10.3945/jn.112.167627. [DOI] [PubMed] [Google Scholar]
- 13.Lapping K, Frongillo EA, Nguyen PH, Coates J, Webb P, Menon P. Organizational factors, planning capacity, and integration challenges constrain provincial planning processes for nutrition in decentralizing Vietnam. Food Nutr Bull. 2014;35:382–91. doi: 10.1177/156482651403500310. [DOI] [PubMed] [Google Scholar]
- 14.de Onis M, Dewey KG, Borghi E, Onyango AW, Blossner M, Daelmans B, Piwoz E, Branca F. The World Health Organization’s global target for reducing childhood stunting by 2025: rationale and proposed actions. Matern Child Nutr. 2013;9:6–26. doi: 10.1111/mcn.12075. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.UNICEF Global Databases. Nutrition: infant and young child feeding. 2014 [cited 2014 Jun 1]. Available from: http://data.unicef.org/nutrition/iycf.
- 16.Mason JB, Shrimpton R, Saldanha LS, Ramakrishnan U, Victora CG, Girard AW, McFarland DA, Martorell R. The first 500 days of life: policies to support maternal nutrition. Glob Health Action. 2014;7:2362. doi: 10.3402/gha.v7.23623. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.UN Open Working Group. Open Working Group proposal for Sustainable Development Goals. 2014 [cited 2014 Nov 11]. Available from: http://sustainabledevelopment.un.org/focussdgs.html.
- 18.Hoddinott J, Alderman H, Behrman JR, Haddad L, Horton S. The economic rationale for investing in stunting reduction. Matern Child Nutr. 2013;9:69–82. doi: 10.1111/mcn.12080. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Uauy R, Kain J, Corvalan C. How can the Developmental Origins of Health and Disease (DOHaD) hypothesis contribute to improving health in developing countries? Am J Clin Nutr. 2011;94(6, Suppl):1759S–64S. doi: 10.3945/ajcn.110.000562. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Popkin BM, Adair LS, Ng SW. Global nutrition transition and the pandemic of obesity in developing countries. Nutr Rev. 2012;70:3–21. doi: 10.1111/j.1753-4887.2011.00456.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Spears D, Ghosh A, Cumming O. Open defecation and childhood stunting in India: an ecological analysis of new data from 112 districts. PLoS ONE. 2013;8:e73784. doi: 10.1371/journal.pone.0073784. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Horton S, Steckel RH. Malnutrition: global economic losses attributable to malnutrition 1900–2000 and projections to 2050. In: Lomborg B, editor. How much have global problems cost the earth? A scorecard from 1900 to 2050. New York: Cambridge University Press; 2013. pp. 247–72. [Google Scholar]
- 23.Macdiarmid JI, Kyle J, Horgan GW, Loe J, Fyfe C, Johnstone A, McNeill G. Sustainable diets for the future: can we contribute to reducing greenhouse gas emissions by eating a healthy diet? Am J Clin Nutr. 2012;96:632–9. doi: 10.3945/ajcn.112.038729. [DOI] [PubMed] [Google Scholar]
- 24.Smith L, Haddad L. Reducing child undernutrition: past drivers and priorities for the post-MDG Era. Brighton (United Kingdom): Institute of Development Studies; 2014. IDS Working Paper No. 441. [Google Scholar]
- 25.Ruel MT, Alderman H. Nutrition-sensitive interventions and programmes: how can they help to accelerate progress in improving maternal and child nutrition? Lancet. 2013;382:536–51. doi: 10.1016/S0140-6736(13)60843-0. [DOI] [PubMed] [Google Scholar]
- 26.Gillespie S, Haddad L, Mannar V, Menon P, Nisbett N. The politics of reducing malnutrition: building commitment and accelerating progress. Lancet. 2013;382:552–69. doi: 10.1016/S0140-6736(13)60842-9. [DOI] [PubMed] [Google Scholar]
- 27.Bhutta ZA, Das JK, Walker N, Rizvi A, Campbell H, Rudan I, Black RE. Interventions to address deaths from childhood pneumonia and diarrhoea equitably: what works and at what cost? Lancet. 2013;381:1417–29. doi: 10.1016/S0140-6736(13)60648-0. [DOI] [PubMed] [Google Scholar]
- 28.Menon P, Covic NM, Harrigan PB, Horton SE, Kazi NM, Lamstein S, Neufield L, Oakley E, Pelletier D. Strengthening implementation and utilization of nutrition interventions through research: a framework and research agenda. Ann N Y Acad Sci. 2014;1332:39–59. doi: 10.1111/nyas.12447. [DOI] [PubMed] [Google Scholar]
- 29.FAO. The state of food insecurity in the world. Rome (Italy): FAO; 2014. [Google Scholar]
- 30.World Bank. Improving nutrition through multisectoral approaches. Washington (DC): World Bank; 2013. [Google Scholar]
- 31.UN Standing Committee on Nutrition. The nutrition sensitivity of agriculture and food policies: a synthesis of eight country case studies. Geneva (Switzerland): UN Standing Committee on Nutrition; 2013. [Google Scholar]
- 32.World Vision International. Importance of nutrition-sensitive agriculture. 2014 [cited 2014 Jun 1]. Available from: www.wvi.org/nutrition/nutrition-sensitive-agriculture.
- 33.Fanzo J, Curran S, Remans R, Mara V, Briseño JS, Cisewski D, Denning G, Fracassi P. Simulating potential of nutrition-sensitive interventions. New York: Columbia University, Earth Institute, Center on Globalization and Sustainable Development; 2014. [cited 2014 Sep 1]. Available from: http://scalingupnutrition.org/wp-content/uploads/2014/07/SUN-Report-CU_Jan-21-2014.pdf. [Google Scholar]
- 34.Picanyol C. Working Paper—final. Geneva (Switzerland): SUN Movement; 2014. Tracking investments on nutrition. [cited 2014 Sep 1]. Available from: http://scalingupnutrition.org/wp-content/uploads/2013/02/140120-Tracking-Investments-on-Nutrition.pdf. [Google Scholar]
- 35.te Lintelo DJH, Haddad LJ, Lakshman R, Gatellier K. The Hunger and Nutrition Commitment Index (HANCI 2013): measuring the political commitment to reduce hunger and undernutrition in developing countries. Brighton (United Kingdom): Institute of Development Studies; 2014. IDS Evidence Report No. 78. [Google Scholar]
- 36.Access to Nutrition Foundation. Access to Nutrition Index: Global Index. 2013 [cited 2014 Dec 12]. Available from: http://www.accesstonutrition.org/global-index-2013.
- 37.Swinburn B, Sacks G, Vandevijvere S, Kumanyika S, Lobstein T, Neal B, Barquera S, Friel S, Hawkes C, Kelly B, et al. INFORMAS (International Network for Food and Obesity/Non-Communicable Diseases Research, Monitoring and Action Support): overview and key principles. Obes Rev. 2013;14:1–12. doi: 10.1111/obr.12087. [DOI] [PubMed] [Google Scholar]
- 38.Scaling Up Nutrition. Monitoring progress—SUN Monitoring Pilot Workshop. 2014 [cited 2014 Nov 11]. Available from: http://scalin-gupnutrition.org/news/monitoring-progress-sun-monitoring-evaluation-workshop-in-rwanda#.VC7RTTleflK.
- 39.Björkman M, Svenssonn J. Power to the people: evidence from a randomized field experiment on community-based monitoring in Uganda. Q J Econ. 2009;124:735–69. [Google Scholar]
- 40.Swain B, Sen PD. Bridging the malnutrition gap with social audits and community participation. IDS Bull. 2009;40:95–102. [Google Scholar]
- 41.Bryce J, Vitora CG. National Evaluation Platform Approach [policy brief] Baltimore (MD): Institute for International Programmes; 2011. Available from: http://www.jhsph.edu/departments/international-health/centers-and-institutes/institute-for-international-programs/projects/nep-docs/NEP-Policy-Brief-2011.pdf. [Google Scholar]
- 42.UNICEF; WHO. Fulfilling the health agenda for women and children: the 2014 report. Geneva (Switzerland): UNICEF/World Health Organization; 2014. Countdown to 2015. [Google Scholar]
- 43.Haddad L, Isenman P. Which aid spending categories have the greatest untapped potential to support the reduction of undernutrition? Some ideas on moving forward. Food Nutr Bull. 2014;35:266–76. doi: 10.1177/156482651403500213. [DOI] [PubMed] [Google Scholar]
- 44.Sodjinou R, Bosu WK, Fanou N, Déart L, Kupka R, Tchibindat F, Baker S. A systematic assessment of the current capacity to act in nutrition in West Africa: cross-country similarities and differences. Glob Health Action. 2014;7:24763. doi: 10.3402/gha.v7.24763. [DOI] [PMC free article] [PubMed] [Google Scholar]