Abstract
Objective: We aimed to perform a meta-analysis from eligible studies to analyze the true impact of QL when compared with BL with regard to post-procedural outcomes including lead deactivation, revision or replacement.
Background: Many observational and retrospective studies showed that quadripolar left ventricular leads (QL) are associated with better outcomes and fewer complications when compared with bipolar leads (BL).
Methods: We performed a comprehensive literature search through June 30, 2015 using: quadripolar, bipolar, left ventricular lead and CRT in Pubmed, Ebsco and google scholar databases.
Results: The analysis included 8 studies comparing QL and BL implantation. Post-procedural outcomes such as lead deactivation, revision or replacement were used as primary outcome and assessed with Mantel–Haenszel risk ratio (RR). Secondary outcomes included total fluoroscopy/procedure time, occurrence of phrenic nerve stimulation (PNS) and all-cause mortality on follow up. Follow-up duration for the studies ranged from 3 to 60 months. Compared with BL, the use of QL is associated with 52 % reduction (relative risk 0.48; 95% CI: 0.36-0.64, p=0.00001) in the risk of deactivation, revision or replacement of the LV lead. QL had significantly lower fluoroscopy/procedure time, PNS and all-cause mortality when compared with BL.
Conclusion:Our meta-analysis shows that QL implantation was associated with decreased risk of LV lead deactivation, revision or replacement when compared with BL.
Keywords: Cardiac Resynchronization Therapy, Quadripolar Lead, Bipolar Lead, Meta-Analysis, Congestive Heart Failure
Introduction
Cardiac resynchronization therapy (CRT) is shown to prolong survival, decrease hospitalizations and improve symptoms in patients with left ventricular ejection fraction (LVEF) of ≤35% and evidence of ventricular dysynchrony demonstrated by prolonged QRS duration on an electrocardiogram.[1-3] Despite, the effectiveness of CRT, there are several challenges associated with implantation of the left ventricular (LV) lead such as inability to cannulate the target cardiac vein, lead instability, high pacing thresholds, excessive phrenic nerve stimulation (PNS) and lead deactivation, lead revision or replacement.[4-6]
Recently, quadripolar LV lead (QL) has been a new innovation in pacing lead technology. The QL, by using 4-electrodes offers greater flexibility and programmability in LV lead placement and CRT by offering ten possible unipolar and bipolar pacing configurations and is designed to improve ease of implantation, decrease short-term and long term complications.[7,8]
Several recent studies have demonstrated that CRT using a QL was associated with lower PNS, procedure and fluoroscopy times and fewer lead related complications including lead deactivation, lead revision or replacement.[7-18] We aimed to conduct a meta-analysis from eligible randomized controlled trials (RCTs) and observational studies comparing QL versus bipolar LV leads (BL) performance and its impact on post-procedural CRT outcomes.
Methods
Search Strategy
We searched MEDLINE, the Web of Science, EBSCO database, Cochrane Central Register of Controlled Trials, Google Scholar, scientific conference sessions and the reference lists of retrieved reports from inception to June 30, 2015 using the search terms ‘cardiac resynchronization therapy’; ‘quadripolar lead’; ‘bipolar lead’ and ‘left ventricular lead’ to identify all RCT’s and observational studies comparing the effects of QL with BL lead on outcomes of CRT. A hand search was also performed in major search databases to identify potentially relevant literature on QL with regard to CRT.
Study Selection
The inclusion criteria of our meta-analysis consisted of RCTs and observational studies of patients undergoing biventricular device implantation in age ≥18 years’ assigned to QL or BL which reported post-procedural outcomes including lead deactivation, revision or replacement at any time during follow-up. Our literature search was limited to studies published in peer-review journals in English. We excluded studies having no reported procedural outcomes. Studies published in animal models and foreign languages were excluded. A search for unpublished literature was not performed.
Data Extraction
Two investigators independently performed a search strategy for eligible studies. All items were initially reviewed at the title and abstract level. Potential eligible manuscripts were reviewed in full text. The data was extracted using a standardized form.
Primary Outcome
The primary endpoint was post-procedural outcomes including lead deactivation, lead revision or replacement.
Secondary Outcome
Total duration of the procedure/fluoroscopy, PNS and all-cause mortality were assessed as secondary outcomes with random effect meta-analysis.
Quality Assessment
We followed the criteria established by Juni et al in the quality assessment of the included RCTs in the meta-analysis.[19]
Statistical Analysis
After the data elements were verified for accuracy, systematic and statistical analyses were conducted using Cochrane RevMan version 5.3, and results were expressed as risk ratio (RR) for dichotomous outcomes and mean difference for continuous variables with 95% confidence intervals (CIs). The difference between the QL and BL were estimated by weighted mean difference (WMD) with a two-tailed 95% CI in a DerSimonian-Laird random-effects model for heterogeneous studies. Statistic value I2 was used to quantify the degree of inconsistency. P < 0.05 was considered statistically significant. For the I2 statistic, heterogeneity was defined as low (25%–50%), moderate (50%–75%), or high (>75%). A fixed-effects model was only used if heterogeneity was low.
Results
Search Results
The original search strategy retrieved 29 clinical studies. The title and abstract were reviewed and after applying the inclusion and exclusion criteria, 20 articles were selected for further detailed assessment. After the exclusion of review articles, duplicates and studies with irrelevant outcomes, we found a total of 8 studies comparing QL and BL implantation in CRT outcomes for inclusion in the final analysis (Figure 1). Follow-up duration for the studies ranged from 3 to 60 months. The years of publication ranged from 2012 to 2015 (Table 1).
Figure 1. Flow diagram for the included studies.
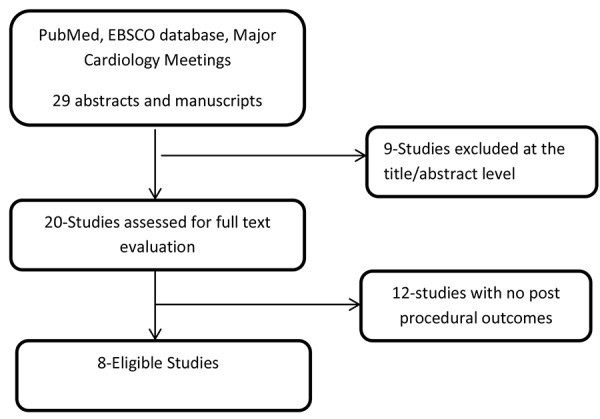
Table 1.
| Study ID | Type of Study | Age Mean±SD | Sample Size | Longest follow up | Risk difference between QL versus BL (95% CI) |
|---|---|---|---|---|---|
| Arias et al 2012 | Prospective Observational | 65.6 ± 9.9 | 42 | 9 months | -0.05 [-0.20, 0.11] |
| Forleo et al 2012 | Retrospective | 68.3±10.7 | 45 | 6 months | -0.23 [-0.43, -0.03] |
| Corbisiero et al 2014 | Retrospective | No data | 79 | 3 months | -0.02 [-0.09, 0.04] |
| Dhillion et al 2014 | Retrospective | 71±8 | 29 | 6 months | 0.00 [-0.12, 0.12] |
| MORE-CRT 2014 | Prospective randomized | 68±10 | 1,068 | 6 month | -0.03 [-0.06, 0.01] |
| Turakhia et al 2014 | Prospective Observational | 69.8±11.3 | 24,293 | 12 months | -0.01 [-0.02, -0.01] |
| Forleo et al 2015 | Prospective Observational | 70.3±9.2 | 418 | 39 months | -0.05 [-0.10, -0.01] |
| Behar et al 2015 | Prospective Observational | 68.4 ± 0.55 | 721 | 60 months | -0.08 [-0.12, -0.05] |
Study Characteristics
Table 1 summarizes the characteristics of included studies. The meta-analysis includes a total of 8 studies (one randomized control study, four prospective observational and three retrospective studies). Baseline characteristics, procedural details and patient’s follow up were similar across all studies. A total of 5,763 patients with QL and 20,894 patients with BL were found. The median follow-up duration was 7.5 months (range 3 months to 60 months), and the median sample size was 248 patients (range 29 to 24,293 patients).
Quadripolar Leads Last Longer Than Bipolar Leads
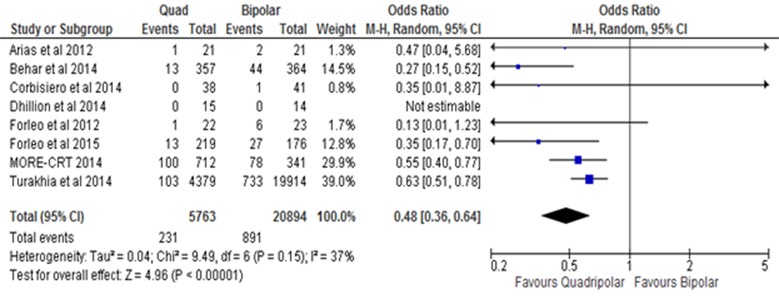
Compared with BL, the use of QL is associated with 52 % reduction (relative risk 0.48; 95% CI: 0.36-0.64, p=0.00001) in the risk of deactivation, lead revision or replacement of the LV lead (Figure 2).
Figure 2. Forest plot showing relative risk (RR) of lead deactivation, revision or replacement with quadripolar lead (QL) and bipolar lead (BL) at follow-up. The use of QL results in a 52% reduction (relative risk 0.48; 95% confidence interval [CI]: 0.36-0.64, p=0.00001) when compared with BL. M-H: Mentel-Haenszel.
QL Leads Require Reduced Fluoroscopic Exposure And Procedure Time For Optimal Placement
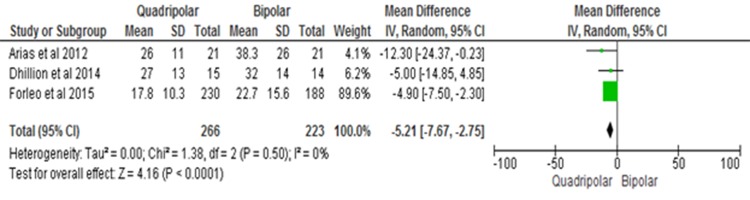
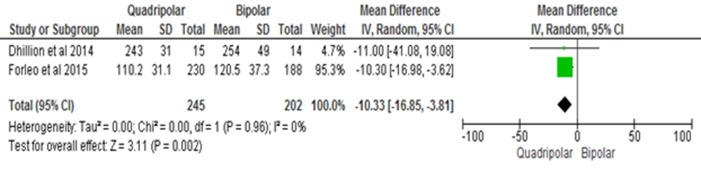
Compared with BL, the use of QL reduced fluoroscopy by a mean duration of 5.21 minutes (95% CI: -7.67 to -2.75, P<0.0001) and mean procedure time by 10.33 minutes (95% CI: -16.85 to -3.81, P=0.002) (Figure 3A, 3B).
Figure 3A. Reduction in fluoroscopy duration. Forest plot showing unadjusted difference in mean (95% confidence interval [CI]) fluoroscopy duration with quadripolar lead (QL) and bipolar lead (BL). QL results a reduction in mean fluoroscopy duration of 5.21 minutes (95% CI: -7.67 to -2.75, P<0.0001) when compared with BL. IV: inverse variance.
Figure 3B. Reduction in procedure duration. Forest plot showing unadjusted difference in mean (95% confidence interval [CI]) procedure duration with quadripolar lead (QL) and bipolar lead (BL). QL results a reduction in mean procedure duration of 10.33 minutes (95% CI: -16.85 to -3.81, P=0.002) when compared with BL. IV: inverse variance.
QL Leads Are Associated With Decreased Phrenic Nerve Stimulation
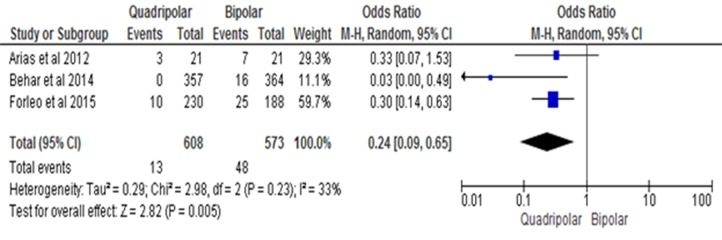
Compared with BL, the use of QL is associated with 76 % reduction (relative risk 0.24; 95% CI: 0.09-0.65, p=0.005) in risk of PNS due to the LV lead (Figure 4).
Figure 4. Forest plot showing relative risk (RR) of phrenic nerve stimulation (PNS) with quadripolar lead (QL) and bipolar lead (BL) at follow-up. The use of QL results in a 76 % reduction (relative risk 0.24; 95% CI: 0.09-0.65, p=0.005) of PNS when compared with BL. M-H: Mentel-Haenszel.
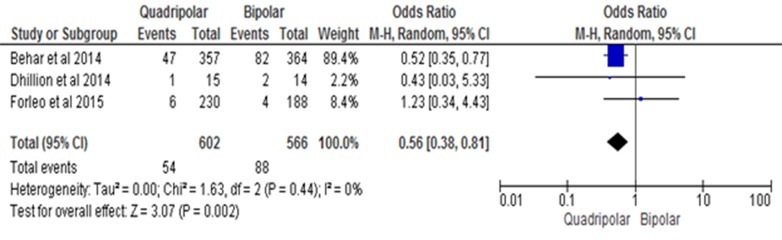
Placement Of QL Leads Improves Survival
Compared with BL, the use of QL is associated with 44 % reduction (relative risk 0.56; 95% CI: 0.38-0.81, p=0.002) in the risk of all-cause mortality at follow up (Figure 5).
Figure 5. Forest plot showing relative risk (RR) of all-cause mortality with quadripolar lead (QL) and bipolar lead (BL) at follow-up. The use of QL results in a 44 % reduction (relative risk 0.56; 95% CI: 0.38-0.81, p=0.002) in all-cause mortality when compared with BL. M-H: Mentel-Haenszel.
Discussion
Major Findings
The principal finding of this meta-analysis of RCTs and observational studies is that QL had lower post-procedural complications including lead deactivation, lead revision or replacement when compared with BL. To our knowledge, this is so far the first comprehensive meta-analysis comparing post procedural CRT lead outcome of QL and BL.
Impact On Lead Longevity
The current meta-analysis confirms the findings of several recent studies showing that QL are more durable. The most plausible explanation for the decreased need for lead revision or lead replacement with QL is the flexibility in programming in the presence of multiple poles.
Impact On The Procedure Duration
The current meta-analysis results are consistent with the findings of prior studies demonstrating superiority of QL when compared with BL.[12,13,20] Our meta-analysis including 26,657 patients demonstrated that QL was associated with a 52% reduction in post procedural complications in a median follow up of 7.5 months when compared with BL placement. Our data supports and extends the current notion that optimal lead implantation using QL is easier than BL. A significantly lower fluoroscopy and procedure time was noted with QL when compared with BL with a mean difference -5.21 minutes and -10.33 minutes respectively. The lower rate of lead revision and total procedure/fluoroscopy time in the QL versus BL was most likely due to ease of implantation from the programming flexibility due to multiple pacing vectors the lead has offered. The alternative pacing vectors with the QL can also overcome other commonly encountered challenges commonly seen with BL such as PNS, higher pacing thresholds and micro-dislodgement of the LV lead without the need for another surgical procedure. Furthermore, QL are reported to have lower impedance and use lower energy to capture the left ventricle that promotes longevity of the device and lowers the need for replacement.[11,12]
Impact Of QL Leads On The PNS
While implanting a CRT, it is of paramount importance to locate a suitable coronary sinus vein or tributary which is associated with low PNS and pacing thresholds. Prior studies have reported post-implantation PNS rates with bipolar leads ranged from 7.4-14% and were more commonly associated with the LV lead location.[21-24] PNS was more commonly seen with the LV lead in the mid-apical, posterior and lateral sites and less common with the LV lead in the anterior or basal site. Our meta-analysis demonstrates that compared with BL, the use of QL is associated with 76 % reduction in PNS. The QL has low PNS as it offers LV pacing from any of the four electrodes as cathode, and RV coil and LV electrodes as anode when compared with BL that offer LV pacing from the ring or the tip as cathode with various anode options. Furthermore, PNS can be posture-dependent and is usually detected post-implantation rather than during implantation. Post-procedural lead re-intervention including CRT termination due to PNS with BL was reported to be 2-13%.[21-25] A QL due to its multiple electrodes and pacing options overcomes the necessity for re-intervention by physically moving the LV lead to another location or CRT termination.
Improved Survival With QL
Our meta-analysis also demonstrates that compared with BL, the use of QL is associated with 44 % reduction in risk of all-cause mortality. These finding can be attributed to the ease of implantation and identification of optimal pacing site with QL which could have resulted in reverse myocardial remodeling and hemodynamic benefit when compared with BL. Implantation of LV lead at the site of a myocardial scar in patients with ischemic cardiomyopathy and presence of atrial arrhythmias has been associated with non-CRT responders.[6,26,27] QL with their multiple programming and pacing vectors can avoid such areas of myocardial scar improving outcomes in patients when compared with BL.
Strengths Of The Current Meta-Analysis
The potential strengths of this meta-analysis are that it is large and includes 26,657 patients. There was no heterogeneity or publication bias among individual studies as noted from our analysis. There is no previous meta-analysis comparing the effectiveness of QL when compared with BL with respect to post procedural complications. The current meta-analysis is the first attempt to explore the beneficial effects of QL over BL in regards to post procedural complications.
Study Limitations
The study has some potential limitations.
Most of the studies performed on QL have been from prospective registries. Only one study was a RCT. We cannot exclude the existence of potential unmeasured confounding factors in the included studies.
There were more patients in the BL (N=20,894) than compared to the QL (N=5,763) which can lead to some discrepancy in interpretation of results and the sample size may be not large enough to draw firm conclusions.
The type of lead implanted in the studies was at the discretion of the invasive cardiac electrophysiologist that could result in a selection bias.
Median follow- up in our study was limited to 7.5 months, so we cannot exclude the possibility of lead complications arising over a longer follow-up period.
Our meta-analysis does not include data regarding number of patients with ischemic cardiomyopathy and atrial arrhythmias in each individual group as it may impact CRT response and mortality.
We are unable to perform additional analysis due to limited number of studies and unpublished data.
Conclusions
Overall, this meta-analysis confirms and extends the findings of most clinical trials by demonstrating that QL have lower post procedural complications including lead deactivation, revision or replacement than BL in patients referred for CRT implantation. This meta-analysis encourages the use of QL and also highlights the need for large-scale multicenter trials to further validate the effectives of this LV lead technology.
Disclosures
None.
References
- 1.Cleland John G F, Daubert Jean-Claude, Erdmann Erland, Freemantle Nick, Gras Daniel, Kappenberger Lukas, Tavazzi Luigi. The effect of cardiac resynchronization on morbidity and mortality in heart failure. N. Engl. J. Med. 2005 Apr 14;352 (15):1539–49. doi: 10.1056/NEJMoa050496. [DOI] [PubMed] [Google Scholar]
- 2.Moss Arthur J, Hall W Jackson, Cannom David S, Klein Helmut, Brown Mary W, Daubert James P, Estes N A Mark, Foster Elyse, Greenberg Henry, Higgins Steven L, Pfeffer Marc A, Solomon Scott D, Wilber David, Zareba Wojciech. Cardiac-resynchronization therapy for the prevention of heart-failure events. N. Engl. J. Med. 2009 Oct 1;361 (14):1329–38. doi: 10.1056/NEJMoa0906431. [DOI] [PubMed] [Google Scholar]
- 3.Daubert Claude, Gold Michael R, Abraham William T, Ghio Stefano, Hassager Christian, Goode Grahame, Szili-Török Tamás, Linde Cecilia. Prevention of disease progression by cardiac resynchronization therapy in patients with asymptomatic or mildly symptomatic left ventricular dysfunction: insights from the European cohort of the REVERSE (Resynchronization Reverses Remodeling in Systolic Left Ventricular Dysfunction) trial. J. Am. Coll. Cardiol. 2009 Nov 10;54 (20):1837–46. doi: 10.1016/j.jacc.2009.08.011. [DOI] [PubMed] [Google Scholar]
- 4.Biffi Mauro, Exner Derek V, Crossley George H, Ramza Brian, Coutu Benoit, Tomassoni Gery, Kranig Wolfgang, Li Shelby, Kristiansen Nina, Voss Frederik. Occurrence of phrenic nerve stimulation in cardiac resynchronization therapy patients: the role of left ventricular lead type and placement site. Europace. 2013 Jan;15 (1):77–82. doi: 10.1093/europace/eus237. [DOI] [PubMed] [Google Scholar]
- 5.Gras D, Böcker D, Lunati M, Wellens H J J, Calvert M, Freemantle N, Gervais R, Kappenberger L, Tavazzi L, Erdmann E, Cleland J G F, Daubert J-C. Implantation of cardiac resynchronization therapy systems in the CARE-HF trial: procedural success rate and safety. Europace. 2007 Jul;9 (7):516–22. doi: 10.1093/europace/eum080. [DOI] [PubMed] [Google Scholar]
- 6.Ypenburg Claudia, van Bommel Rutger J, Delgado Victoria, Mollema Sjoerd A, Bleeker Gabe B, Boersma Eric, Schalij Martin J, Bax Jeroen J. Optimal left ventricular lead position predicts reverse remodeling and survival after cardiac resynchronization therapy. J. Am. Coll. Cardiol. 2008 Oct 21;52 (17):1402–9. doi: 10.1016/j.jacc.2008.06.046. [DOI] [PubMed] [Google Scholar]
- 7.Behar Jonathan M, Bostock Julian, Zhu Li Adrian Po, Chin Hui Men Selina, Jubb Stephen, Lent Edward, Gamble James, Foley Paul W X, Betts Tim R, Rinaldi Christopher Aldo, Herring Neil. Cardiac Resynchronization Therapy Delivered Via a Multipolar Left Ventricular Lead is Associated with Reduced Mortality and Elimination of Phrenic Nerve Stimulation: Long-Term Follow-Up from a Multicenter Registry. J. Cardiovasc. Electrophysiol. 2015 May;26 (5):540–6. doi: 10.1111/jce.12625. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Arias Miguel A, Pachón Marta, Puchol Alberto, Jiménez-López Jesús, Rodríguez-Padial Luis. Acute and mid-term outcomes of transvenous implant of a new left ventricular quadripolar lead versus bipolar leads for cardiac resynchronization therapy: results from a single-center prospective database. Cardiol J. 2012;19 (5):470–8. doi: 10.5603/cj.2012.0087. [DOI] [PubMed] [Google Scholar]
- 9.Forleo Giovanni B, Della Rocca Domenico G, Papavasileiou Lida P, Molfetta Arianna Di, Santini Luca, Romeo Francesco. Left ventricular pacing with a new quadripolar transvenous lead for CRT: early results of a prospective comparison with conventional implant outcomes. Heart Rhythm. 2011 Jan;8 (1):31–7. doi: 10.1016/j.hrthm.2010.09.076. [DOI] [PubMed] [Google Scholar]
- 10.Shetty Anoop K, Duckett Simon G, Bostock Julian, Roy Debashis, Ginks Matthew, Hamid Shoaib, Rosenthal Eric, Razavi Reza, Rinaldi Christopher Aldo. Initial single-center experience of a quadripolar pacing lead for cardiac resynchronization therapy. Pacing Clin Electrophysiol. 2011 Apr;34 (4):484–9. doi: 10.1111/j.1540-8159.2010.03003.x. [DOI] [PubMed] [Google Scholar]
- 11.Sperzel Johannes, Dänschel Wilfried, Gutleben Klaus-Jürgen, Kranig Wolfgang, Mortensen Peter, Connelly Derek, Trappe Hans-Joachim, Seidl Karlheinz, Duray Gabor, Pieske Burkert, Stockinger Jochem, Boriani Giuseppe, Jung Werner, Schilling Richard, Saberi Linda, Hallier Benoit, Simon Marcus, Rinaldi Christopher A. First prospective, multi-centre clinical experience with a novel left ventricular quadripolar lead. Europace. 2012 Mar;14 (3):365–72. doi: 10.1093/europace/eur322. [DOI] [PubMed] [Google Scholar]
- 12.Forleo Giovanni B, Mantica Massimo, Di Biase Luigi, Panattoni Germana, Della Rocca Domenico G, Papavasileiou Lida P, Santamaria Matteo, Santangeli Pasquale, Avella Andrea, Sergi Domenico, Santini Luca, Tondo Claudio, Natale Andrea, Romeo Francesco. Clinical and procedural outcome of patients implanted with a quadripolar left ventricular lead: early results of a prospective multicenter study. Heart Rhythm. 2012 Nov;9 (11):1822–8. doi: 10.1016/j.hrthm.2012.07.021. [DOI] [PubMed] [Google Scholar]
- 13.Forleo Giovanni B, Di Biase Luigi, Panattoni Germana, Mantica Massimo, Parisi Quintino, Martino Annamaria, Pappalardo Augusto, Sergi Domenico, Tesauro Manfredi, Papavasileiou Lida P, Santini Luca, Calò Leonardo, Tondo Claudio, Natale Andrea, Romeo Francesco. Improved implant and postoperative lead performance in CRT-D patients implanted with a quadripolar left ventricular lead. A 6-month follow-up analysis from a multicenter prospective comparative study. J Interv Card Electrophysiol. 2015 Jan;42 (1):59–66. doi: 10.1007/s10840-014-9956-1. [DOI] [PubMed] [Google Scholar]
- 14.Corbisiero Raffaele, Muller David. Profile of St. Jude Medical's Allure Quadra quadripolar pacemaker system for cardiac resynchronization therapy. Expert Rev Med Devices. 2015 Jan;12 (1):41–8. doi: 10.1586/17434440.2015.984686. [DOI] [PubMed] [Google Scholar]
- 15.Turakhia M. Decreased rate of left ventricular lead deactivation and replacement associated with use of quadripolar LV leads. Presented at Europace. 2013;Abstract 451 [Google Scholar]
- 16.Boriani G, Connors S, Lemke B. Chronic performance of 10 pacing vectors available with a novel quadripolar left ventricular lead compared to bipolar leads in the MORE CRT trial. Europace Abstracts Supplement. 2015;17:Supplement 3 [Google Scholar]
- 17.Dhillon O. Do quadripolar left ventricular leads offer any benefit over bipolar leads in cardiac resynchronisation therapy? The QUAD-CRT randomised controlled trial. Heart rhythm : the official journal of the Heart Rhythm Society. 2014 [Google Scholar]
- 18.Turakhia M. Decreased rate of left ventricular lead deactivation and replacement associated with use of a quadripolar LV lead. Presented at Europace 2013, Athens, Greece. 2013;Abstract 451 [Google Scholar]
- 19.Jüni P, Altman D G, Egger M. Systematic reviews in health care: Assessing the quality of controlled clinical trials. BMJ. 2001 Jul 7;323 (7303):42–6. doi: 10.1136/bmj.323.7303.42. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Tomassoni Gery, Baker James, Corbisiero Raffaele, Love Charles, Martin David, Niazi Imran, Sheppard Robert, Worley Seth, Beau Scott, Greer G Stephen, Aryana Arash, Cao Michael, Harbert Nicole, Zhang Suhong. Postoperative performance of the Quartet® left ventricular heart lead. J. Cardiovasc. Electrophysiol. 2013 Apr;24 (4):449–56. doi: 10.1111/jce.12065. [DOI] [PubMed] [Google Scholar]
- 21.Biffi Mauro, Moschini Carlotta, Bertini Matteo, Saporito Davide, Ziacchi Matteo, Diemberger Igor, Valzania Cinzia, Domenichini Giulia, Cervi Elena, Martignani Cristian, Sangiorgi Diego, Branzi Angelo, Boriani Giuseppe. Phrenic stimulation: a challenge for cardiac resynchronization therapy. Circ Arrhythm Electrophysiol. 2009 Aug;2 (4):402–10. doi: 10.1161/CIRCEP.108.836254. [DOI] [PubMed] [Google Scholar]
- 22.Seifert Martin, Schau Thomas, Moeller Viviane, Neuss Michael, Meyhoefer Juergen, Butter Christian. Influence of pacing configurations, body mass index, and position of coronary sinus lead on frequency of phrenic nerve stimulation and pacing thresholds under cardiac resynchronization therapy. Europace. 2010 Jul;12 (7):961–7. doi: 10.1093/europace/euq119. [DOI] [PubMed] [Google Scholar]
- 23.Gurevitz Osnat, Nof Eyal, Carasso Shemy, Luria David, Bar-Lev David, Tanami Nechemya, Eldar Michael, Glikson Michael. Programmable multiple pacing configurations help to overcome high left ventricular pacing thresholds and avoid phrenic nerve stimulation. Pacing Clin Electrophysiol. 2005 Dec;28 (12):1255–9. doi: 10.1111/j.1540-8159.2005.00265.x. [DOI] [PubMed] [Google Scholar]
- 24.Champagne Jean, Healey Jeffrey S, Krahn Andrew D, Philippon Francois, Gurevitz Osnat, Swearingen Anne, Glikson Michael. The effect of electronic repositioning on left ventricular pacing and phrenic nerve stimulation. Europace. 2011 Mar;13 (3):409–15. doi: 10.1093/europace/euq499. [DOI] [PubMed] [Google Scholar]
- 25.Jastrzebski Marek, Bacior Bogumila, Wojciechowska Wiktoria, Czarnecka Danuta. Left ventricular lead implantation at a phrenic stimulation site is safe and effective. Europace. 2011 Apr;13 (4):520–5. doi: 10.1093/europace/euq505. [DOI] [PubMed] [Google Scholar]
- 26.Forleo Giovanni B, Di Biase Luigi, Della Rocca Domenico G, Panattoni Germana, Mantica Massimo, Santamaria Matteo, Pappalardo Augusto, Panigada Stefania, Santini Luca, Natale Andrea, Romeo Francesco. Impact of previous myocardial infarction on outcomes of CRT patients implanted with a quadripolar left ventricular lead. Results from a multicentric prospective study. Int. J. Cardiol. 2012 Oct 4;160 (2):145–6. doi: 10.1016/j.ijcard.2012.05.077. [DOI] [PubMed] [Google Scholar]
- 27.Rivero-Ayerza Maximo, Scholte Op Reimer Wilma, Lenzen Mattie, Theuns Dominic A M J, Jordaens Luc, Komajda Michel, Follath Ferenc, Swedberg Karl, Cleland John G F. New-onset atrial fibrillation is an independent predictor of in-hospital mortality in hospitalized heart failure patients: results of the EuroHeart Failure Survey. Eur. Heart J. 2008 Jul;29 (13):1618–24. doi: 10.1093/eurheartj/ehn217. [DOI] [PubMed] [Google Scholar]