Abstract
Multivalvular disease (MVD) is a common condition with a complex pathophysiology, dependent on the specific combination of valve lesions. Diagnosis is challenging as several echocardiographic methods commonly used for the assessment of stenosis or regurgitation have been validated only in patients with single valve disease. Decisions about the timing and type of treatment should be made by a multidisciplinary heart valve team, on a case-by-case basis. Several factors should be considered, including the severity and consequences of the MVD, the patient’s life expectancy and comorbidities, the surgical risk associated with combined valve procedures, the long-term risk of morbidity and mortality associated with multiple valve prostheses, and the likelihood and risk of reoperation. The introduction of transcatheter valve therapies into clinical practice has provided new treatment options for patients with MVD, and decision-making algorithms on how to combine surgical and percutaneous treatment options are evolving rapidly. In this Review, we discuss the pathophysiology, diagnosis, and treatment of MVD, focussing on the combination of valve pathologies that are most often encountered in clinical practice.
Multivalvular disease (MVD), that is the combination of stenotic and / or regurgitant lesions of two or more cardiac valves is a highly prevalent clinical condition among patients with valvular heart disease. In the EuroHeart Survey, 20.2% of the patients with native valve disease, and 14.6% of the patients undergoing valvular surgery, had MVD1. Multiple valve surgery accounted for 10.9% of the 623,039 patients undergoing valve surgery and included in the Society of Thoracic Surgeons (STS) database between 1993 and 20072. Among these patients, 57.8% underwent surgery on the aortic and mitral valves, 31.0% on the mitral and tricuspid, 3.3% on the aortic and tricuspid, and 7.9% underwent triple-valve surgery3, 4. In the PARTNER trials5-7, the incidence of concomitant moderate-to-severe mitral regurgitation in patients with severe aortic stenosis was approximately 20%, and the incidence of moderate-to-severe tricuspid regurgitation was 27%. In the EuroHeart Survey, the mean age of patients presenting with MVD (N=712) was 64, and 83.6% of them were of male gender1.
Rheumatic heart disease has long been considered the main cause of primary (or organic) MVD8, but the incidence of this aetiology has dramatically declined over the past five decades9. However, no concomitant decline in the overall prevalence of valvular heart disease has occurred, because degenerative valve disease has become more prevalent in developed countries owing to aging of the population9. In the EuroHeart survey conducted in 2001, rheumatic heart disease was the most frequent aetiology (51.4%) of MVD, followed by degenerative valve disease (40.6%)1. Other, less frequent, causes of primary MVD include endocarditis, thoracic and mediastinal radiation therapy, and the adverse effects of drugs. Even less frequently, connective tissue disorders, aortic root and myxomatous mitral and tricuspid valve disease linked to genetic syndromes can be associated with MVD10. Mitral and tricuspid regurgitation can also develop in the presence of a structurally normal valve owing to malcoaptation. These common forms of mitral and tricuspid regurgitation, classified as secondary regurgitation, result from alterations of the geometry of the left or right ventricle, respectively 11. In a recent review, secondary mitral regurgitation accounted for approximately 50% of patients with mitral regurgitation undergoing transcatheter aortic valve implantation (TAVI) 12. Coronary artery disease and a history of myocardial infarction are highly prevalent in patients with degenerative valve disease, and ischaemic mitral regurgitation is, therefore, common in the ageing population13-16, and thus in elderly patients with degenerative valve disease. Aortic root dilatation can cause functional aortic regurgitation with anatomically normal aortic valve cusps17. Moreover, primary and secondary aetiologies can coexist.
Despite the prevalence of MVD, limited data exist in the literature to guide the management of patients with this disease. The large number of possible pathophysiological combinations contributes to the scarcity of studies. In this Review, we assess the available data on the pathophysiological complexity of MVD, discuss the diagnostic pitfalls and consider potential management strategies for these challenging clinical scenarios. We will not examine the specific problems of mixed heart valve disease, that is, the combination of stenosis and regurgitation of the same valve.
Pathophysiology
The clinical effect of MVD depends on a complex interplay of pathophysiological factors, including the severity of each individual valve lesion, which combination of valves are diseased, the type (primary versus secondary) and chronicity of the lesions, loading conditions, and ventricular compensation. The severity and clinical effect of one valve lesion can be altered if loading conditions changes or if another valve is repaired. These haemodynamic interactions can promote, exacerbate, or, in contrast, blunt the clinical expression of each singular lesion. For example, in some patients, a rapid decrease in mitral regurgitation severity occurs after mechanical correction of aortic stenosis. Similarly, one concomitant valve lesion can modify the clinical effect of another. For example, two patients with equally severe aortic regurgitation might experience the ventricular and clinical consequences of the aortic regurgitation at different time points if one patient has concomitant mitral stenosis (which can protect from the volume load of aortic regurgitation) and the other patient has concomitant mitral regurgitation (which exacerbates the volume load). The complex and dynamic pathophysiology of MVD makes the evaluation, diagnosis, and management of these patients challenging. Although each case of MVD is different and precludes generalization, we will review some general pathophysiological principles that ought to be considered with the following combinations of valve lesions.
Aortic stenosis and mitral regurgitation
Long-standing increased afterload resulting from aortic stenosis leads to hypertrophic remodelling of the left ventricle (LV). However, a substantial proportion of patients with aortic stenosis develops LV dilation and systolic dysfunction as a result of LV afterload mismatch, concomitant cardiomyopathy (frequently of ischaemic origin), or both. In turn, LV dilation and adverse remodelling can be accompanied by secondary mitral regurgitation owing to mitral annular dilation and leaflet tethering (FIGURE 1)18. Elderly patients (>70 years old) with aortic stenosis often also have coronary artery disease, thus explaining the high prevalence of concomitant secondary ischaemic mitral regurgitation in this population12, 19. Alternatively, patients with aortic stenosis can have concomitant primary mitral regurgitation. The systolic transmitral pressure gradient is inherently increased in the presence of aortic stenosis and, therefore, the regurgitant flow rate (and the regurgitant volume) will be increased for any given mitral regurgitant orifice area20.
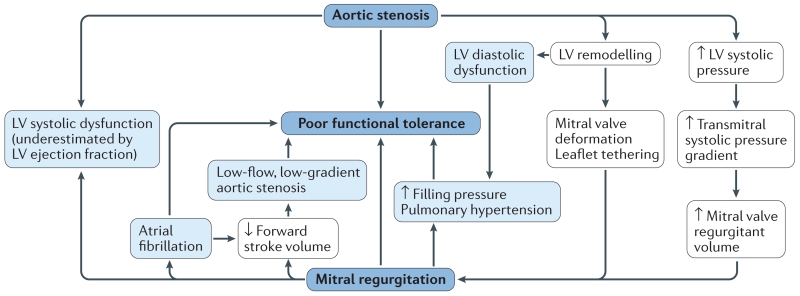
Figure 1. Pathophysiology of combined aortic stenosis and mitral regurgitation.
Mitral valve deformation and tethering, as well as an increase in transmitral pressure gradient caused by aortic stenosis, all contribute to mitral regurgitation. Increased left ventricular (LV) afterload related to aortic stenosis, combined with mitral regurgitation, result in a decrease in forward LV stroke volume and, therefore, often to a low-flow, low-gradient pattern. Both aortic stenosis and mitral regurgitation can, in the long-term, induce LV myocardial fibrosis and dysfunction. However, the extent of LV systolic dysfunction in such cases is underestimated by LV ejection fraction (LVEF) owing to the LV concentric remodelling related to aortic stenosis and the retrograde flow (mitral regurgitant volume) related to mitral regurgitation.
The presence of moderate or severe primary or secondary mitral regurgitation can alter the clinical presentation of patients with aortic stenosis. Mitral regurgitation contributes to a low-flow state, resulting in a low transaortic pressure gradient despite a small aortic valve area (FIGURE 1). Atrial fibrillation, which frequently results from mitral valve diseases, can exacerbate the clinical condition, as loss of the atrial kick is poorly tolerated in patients with aortic stenosis. Furthermore, atrial fibrillation is an independent risk factor for heart failure , stroke, and mortality in patients with aortic stenosis21, 22. In addition, aortic stenosis and mitral regurgitation have opposite effects on ejection phase indices of myocardial performance18. Therefore, unlike patients with isolated mitral regurgitation, those with aortic stenosis and mitral regurgitation and can experience an improvement in LV ejection fraction after mitral valve replacement if the stenotic aortic valve is concomitantly replaced (FIGURE 2). Conversely, the early detection of LV dysfunction in patients with aortic stenosis can be impeded by the presence of mitral regurgitation.
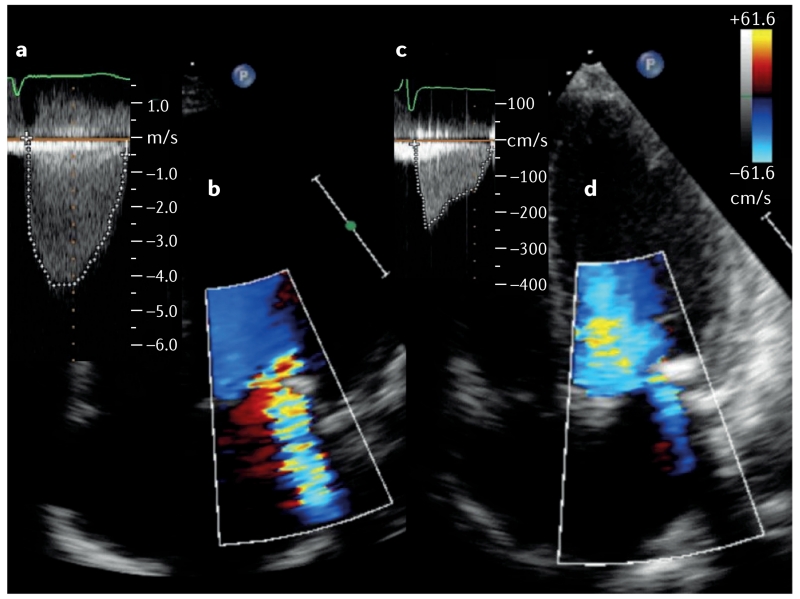
Figure 2. A patient with aortic stenosis and mitral regurgitation.
a | This patient has severe, symptomatic aortic stenosis with a mean transaortic gradient of 48 mmHg and an aortic valve area of 0.7 cm2 on Doppler-echocardiography. Left ventricular ejection fraction is 45%. b | Color Doppler shows that moderate-to-severe mitral regurgitation is also present (see also Supplementary video 1a online). c, d | The same patient, 6 months after transcatheter aortic valve implantation. The mean transaortic pressure gradient is 11 mmHg with only mild residual mitral regurgitation (see also Supplementary video 1b online). Left ventricular ejection fraction is 65%.
Aortic stenosis and mitral stenosis
The combination of severe aortic and mitral stenosis is infrequent in developed countries, as this condition is usually very poorly tolerated from a haemodynamic standpoint, and treatment is sought early during the course of the disease23. A greater than expected reduction in cardiac output can occur when both stenoses are severe, decreasing the flow rate and pressure gradients across both valves, which can lead to underestimation of the severity of both aortic and mitral stenosis (FIGURE 3)24. Whereas physical findings are mainly caused by the aortic stenosis, several clinical manifestations resulting from the mitral stenosis—including atrial fibrillation, haemoptysis, and peripheral embolization—can occur. If concomitant severe aortic stenosis is not recognized25, percutaneous balloon mitral valvuloplasty could impose a sudden preload increase to a small, hypertrophied, and stiff LV, resulting in pulmonary oedema26.
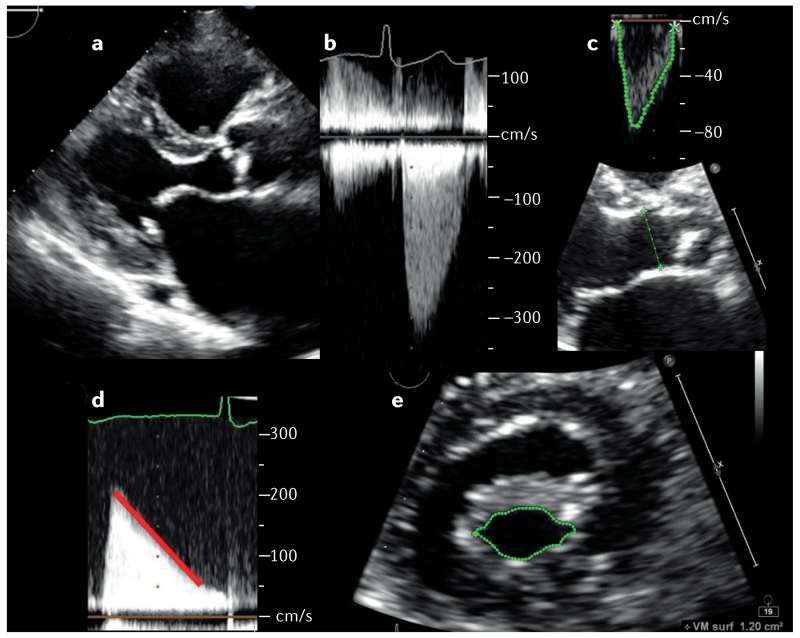
Figure 3. A patient with aortic and mitral stenosis.
a | Parasternal long-axis echocardiographic view of a patient with rheumatic aortic and mitral stenosis and severe symptoms (NYHA class III; see also Supplementary video 2 online). Left ventricular ejection fraction is 60%. b | The mean pressure gradient across the aortic valve is 21 mm Hg. c | Stroke volume, measured in the left ventricular outflow tract (velocity-time integral [green line tracing in top image] multiplied by the cross-sectional area [calculated from diameter: green line in bottom image]), is 42 ml (26 ml/m2 of body surface area). The aortic valve area is 0.62 cm2, consistent with a low-flow, low-gradient aortic stenosis. d | The mean pressure gradient across the mitral valve is 8 mmHg, and the mitral valve area estimated from the pressure half-time method (red diagonal line) is 1.65 cm2. e | Mitral anatomic orifice area (green outline) as measured by direct planimetry is 1.2 cm2. This case highlights the inaccuracy of the pressure half-time method to assess mitral valve effective area in the presence of severe aortic valve disease. Moreover, this patient exemplifies the frequent and challenging situation of low-flow, low-gradient stenosis, present here at both the aortic and the mitral valve. This situation can lead to underestimation of the severity of aortic and mitral stenoses.
As opposed to rheumatic mitral stenosis, degenerative mitral stenosis (or ‘calcific mitral stenosis’) is found in elderly individuals and is usually the result of progressive mitral annular calcification involving the base of the leaflets. Degenerative mitral stenosis causes progressive reduction in the functional valvular orifice, without commissural fusion27. The resulting valvular stenosis is generally less severe than in rheumatic valve disease, therefore decreasing the prevalence of combined critical aortic and mitral stenosis in this population23.
Aortic regurgitation and mitral stenosis
The combination of aortic regurgitation and mitral stenosis imposes opposite loading conditions on the LV. Both LV end-diastolic and end-systolic volume are lower than with isolated aortic regurgitation28. Therefore, the increase in stroke volume typically associated with aortic regurgitation might be blunted in the presence of mitral stenosis, and the clinical signs associated with increased pulse pressure might not be observed29.
Aortic regurgitation and mitral regurgitation
This condition, characterized by severe volume overload caused by the two regurgitations, and some pressure overload typically associated with aortic regurgitation, is usually poorly tolerated. LV dilatation can be severe and hypertrophic remodelling pattern is eccentric (that is lower wall thickness to cavity ratio). Furthermore, premature mitral valve closure—a protective mechanism limiting the amount of backward flow into the left atrium and the pulmonary veins in acute and severe aortic regurgitation—does not occur, which contributes to poor clinical tolerance in patients with concomitant aortic and mitral regurgitation. Patients with this combination of valve lesions who are symptomatic have worse LV performance than those with isolated aortic or mitral regurgitation30, resulting in a high incidence of postoperative LV dysfunction31. However, over long-term follow-up, LV function can eventually improve32. Nonetheless, patients with aortic and mitral regurgitation have significantly reduced postoperative survival and more frequently persistent symptoms after surgery than those with single valve disease30.
Tricuspid regurgitation and left-sided valvular disease
Secondary tricuspid regurgitation is highly prevalent in patients presenting with mitral valve disease (FIGURE 4),33, 34 and is also common in patients undergoing surgical or TAVI for aortic stenosis. Secondary tricuspid regurgitation is associated with reduced postoperative survival7, 35, 36. As with secondary mitral regurgitation, a complex interplay of factors—including free wall annular dilation, right ventricular enlargement and dysfunction, pulmonary hypertension, and right atrial enlargement—underlies the presence and severity of secondary tricuspid regurgitation in the setting of left-sided valve disease, but no single factor seems to be required. Importantly, the severity of tricuspid regurgitation is highly sensitive to changes in loading conditions, and the absence of regurgitation at the time of treatment of the left-sided valve lesion does not guarantee long-term freedom from tricuspid regurgitation (that is, annular dilation alone can be a harbinger of future tricuspid regurgitation). More studies are needed to elucidate the pathophysiology and determinants of secondary tricuspid regurgitation in the setting of left-sided valve disease and to identify predictors of development or progression of tricuspid regurgitation if the tricuspid valve is not treated.
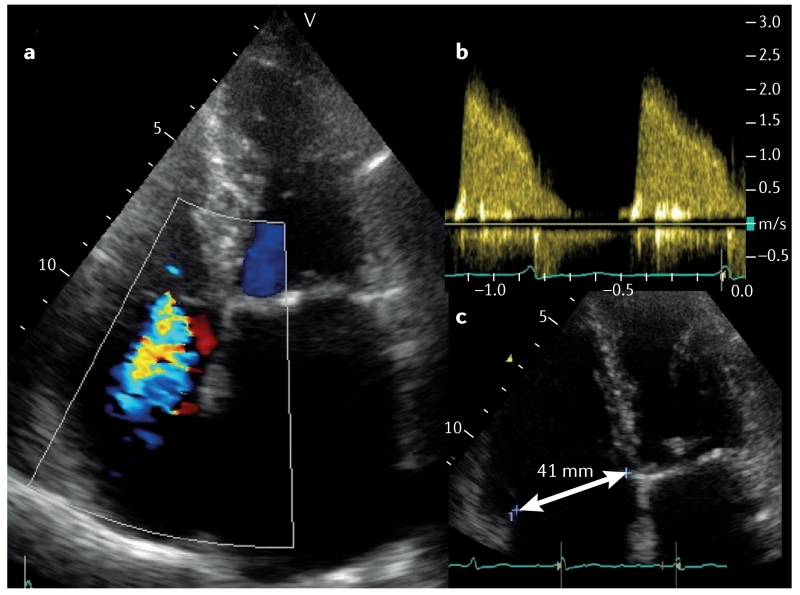
Figure 4. A patient with mitral stenosis and tricuspid regurgitation before surgery.
a | Color Doppler echocardiography shows moderate tricuspid regurgitation (see also Supplementary video 3 online). b | On Doppler-echocardiography, mitral valve area is 1.2 cm2, and the mean pressure gradient across the mitral valve is 12 mmHg. c | The tricuspid annulus, as measured from the apical four-chamber view in late diastole, is 41 mm. This clinical situation represents a class IIa indication for concomitant tricuspid annuloplasty according to both the AHA/ACC41 and ESC/EACTS54 guidelines.
Diagnosis
The haemodynamic consequences of MVD on blood flow, and on ventricular size, shape, and function, as well as the specific combination of valve lesions can influence the diagnostic process in many ways10. Physical examination can be misleading in terms of both the timing and intensity of murmurs heard during auscultation and of other signs, such as pulse pressure. Echocardiography is the cornerstone of the diagnosis of valvular heart disease. However, several Doppler methods commonly used for the assessment of stenosis or regurgitation have been validated only in patients with single valve disease and might not be valid in the setting of MVD. Echocardiographic assessment should include quantification of the stenosis or regurgitation and evaluation of valve anatomy and function, integrated in a multiparametric analysis37. Left and right ventricular volume and function and pulmonary pressure should also be assessed. As a general rule, measurements that are not dependent on loading conditions, such as direct planimetry of a stenotic valve or, for regurgitant lesions, assessment of the effective regurgitant orifice or the vena contracta, are preferred.
A low-flow, low-gradient stenosis is common in MVD (FIGURE 3). Indeed, any severe valve lesion can reduce flow and, therefore, the gradient across another stenotic valve. A low-flow, low-gradient pattern makes the accurate assessment of stenosis severity difficult. On the other hand, the presence of concomitant regurgitation on a stenotic valve (mixed lesion) will have the opposite effect; that is increase the transvalvular flow and, therefore, the pressure gradient. Mitral valve area should not be evaluated using the continuity equation method in the presence of aortic regurgitation, because the transmitral flow differs from the transaortic flow. Pressure half-time-derived echocardiographic methods is invalid in the presence of altered LV compliance or relaxation. Therefore, mitral pressure half-time in the presence of aortic valve disease should be interpreted with caution38, 39. These and other diagnostic echocardiographic caveats of MVD are summarized in TABLE 1.
Table 1. Echocardiographic caveats in the diagnosis of multivalvular disease.
| Combination of valve lesions |
Aortic stenosis | Aortic regurgitation |
Mitral stenosis | Mitral regurgitation |
|---|---|---|---|---|
|
| ||||
| Aortic stenosis | n/a | Pressure half-time method unreliable |
Pressure half-time method unreliable Low-flow, low- gradient mitral stenosis can occur |
High MRV Increased area of mitral regurgitant jet using colour- flow mapping ERO less affected than MRV and colour-flow mapping parameters |
|
| ||||
|
Aortic
regurgitation |
Simplified Bernoulli equation might not be applicable if LVOT velocity is elevated Gorlin formula using thermodilution is invalid Continuity equation is applicable Peak aortic jet velocity reflects severity of both aortic stenosis and aortic regurgitation |
n/a | Aortic regurgitant jet can be mistaken for MS jet Continuity equation is unreliable |
Doppler volumetric method invalid |
|
| ||||
| Mitral stenosis | Low-flow, low- gradient aortic stenosis is common |
Mitral stenosis can blunt the increase in pulse pressure associated with aortic regurgitation |
n/a | Not affected |
|
| ||||
|
Mitral
regurgitation |
Low-flow, low- gradient aortic stenosis is common Mitral regurgitant jet should not be mistaken for the aortic stenosis jet |
Doppler volumetric method inapplicable Pressure half-time method can be unreliable |
Continuity equation unreliable Pressure half-time method unreliable Gorlin formula using thermodilution invalid |
n/a |
This table presents the caveats in the echocardiographic diagnosis of a given valvular lesion (columns of the Table) in presence of concomitant valvular lesion (Lines of the Table). ERO, mitral effective regurgitant orifice; MRV, mitral regurgitant volume. Adapted with permission from Unger 2011 10.
Aortic or pulmonary valve disease can lead to remodelling of the left and right ventricles and thereby the respective atrioventricular valve and subvalvular apparatus. In turn, secondary mitral or tricuspid regurgitation can result. In addition, the increased driving pressure across the atrioventricular valve in the presence of aortic or pulmonary stenosis will increase the regurgitant volume. In this context, the regurgitant volume accurately reflects the haemodynamic burden of the regurgitation and correlates with symptoms, but will tend to be disproportionately elevated as compared with the effective regurgitant orifice. On the other hand, the effective regurgitant orifice area is more useful to guide decisions about whether to perform concomitant correction of the regurgitation of the atrioventricular valve if the patient undergoes replacement of the aortic or pulmonary valve.
Catheterization is recommended when discordant or inconclusive results are obtained on physical examination and with noninvasive testing40. In the EuroHeart survey, catheterization was performed in 30% of patients with MVD1. However, right-heart catheterization cannot be used accurately in this setting because the stroke volume obtained by this technique does not equal the stroke volume across the aortic or the mitral valve in the presence of mixed aortic or mitral valve disease, respectively.In addition, thermodilution can be misleading in the assessment of cardiac output and, therefore, valve area in patients with severe tricuspid regurgitation, very low cardiac output, or both—situations that are common in patients with MVD41, 42.
Multimodality imaging
Echocardiography is the primary imaging modality to establish the diagnosis and follow patients with MVD, but other imaging modalities can be helpful when the information obtained by echocardiography is not sufficient or is inconclusive to determine the severity of each individual valvular lesions.
Determination of the severity of stenotic lesions can be hampered by the frequent occurrence of low-flow states with resulting ‘pseudonormal’ low gradients or ‘pseudosevere’ valve stenosis. Yet, an accurate diagnosis is critical, often with implications for treatment decisions. The continuity equation, on which the estimation of aortic valve area is based, assumes a circular shape of the LV outflow tract. However, 3D analysis has demonstrated that the annulus often has an oval shape43. Therefore, LV outflow tract area, as measured by 3D echocardiography, MRI, or multidetector CT is often larger than the area calculated from a single LV outflow tact diameter obtained by transthoracic echocardiography44. This larger LV outflow tract area will translate into a different (and often larger) aortic valve area when 3D methods are used45. However, these measurements of aortic valve area by hybrid methods (for example, LV outflow tract area measured by multislice CT and flow velocities measured by Doppler echocardiography) have to be used with technique-specific validated thresholds that might be higher than 1 cm2 (the validated threshold for echocardiography) 46.
Dobutamine stress echocardiography should be performed in patients with low flow and a low transaortic gradient, but a small valve area, to exclude pseudosevere aortic stenosis47. In such difficult cases, particularly when the results of echocardiography are inconclusive, multislice CT can be used to assess the aortic valve calcium score (severe stenosis: >2,000 AU in men and >1,200 AU in women)48, 49.
Real-time 3D transoesophageal echocardiography can be valuable to measure mitral valve area in rheumatic mitral stenosis50, whereas real-time 3D echocardiography using colour-defined planimetry can be useful in selected patients with degenerative calcified mitral stenosis51. However, with the exception of interventional cardiology52, the role of multimodality imaging in the setting of MVD is currently limited.
Treatment
Evidence on medical, surgical, and interventional management of patients with MVD is scarce. Most recommendations from both American40, 53 and European54 guidelines are, therefore, given a level of evidence C (TABLE 2). Several factors should, however, be taken into account when determining the optimal management strategy. First, the increased surgical risk of combined procedures and the long-term increase in morbidity associated with multiple prosthetic valves. Second, the risk of eventual reoperation and the prognostic impact of not correcting a less-than-severe lesion. Third, the likelihood of spontaneous changes in mitral or tricuspid regurgitation after surgery on a downstream valvular lesion. Fourth, the choice of surgical technique. Fifth, the emerging role of percutaneous approaches, and sixth, the crucial role of a heart valve team. We will consider each of these factors in turn.
Table 2. Indications for concomitant valve surgery in patients undergoing surgery on another valve.
| Valve lesion | ESC/EACTS guidelines (2012)54 | AHA/ACC guidelines (2014)41 |
|---|---|---|
|
| ||
| Aortic stenosis | AVR is indicated in patients with severe aortic stenosis undergoing CABG surgery, or surgery on the ascending aorta or another valve (class I, LOE C) AVR should be considered in patients with moderate aortic stenosis undergoing surgery on the ascending aorta or another valve (class IIa, LOE C) |
AVR is indicated for patients with severe aortic stenosis undergoing other cardiac surgery (class I, LOE B) AVR is reasonable for patients with moderate aortic stenosis undergoing other cardiac surgery (class IIa, LOE C) |
|
| ||
|
Aortic
regurgitation |
Surgery is indicated in patients with severe aortic regurgitation undergoing surgery on another valve (class I, LOE C) |
AVR is indicated for patients with severe aortic regurgitation (stage C or D) undergoing cardiac surgery for other indications (class I, LOE C) AVR is reasonable in patients with moderate aortic regurgitation undergoing other cardiac surgery (class IIa, LOE C) |
|
| ||
| Mitral stenosis | Surgery is preferable to PMC in patients with severe mitral stenosis combined with severe aortic valve disease In patients with severe mitral stenosis and moderate aortic valve disease, PMC can be performed to postpone the surgical treatment of both valves Severe concomitant aortic valve disease is a contraindication to PMC |
Concomitant mitral valve surgery is indicated for patients with severe mitral stenosis undergoing other cardiac surgery (class I, LOE C) Concomitant mitral valve surgery may be considered for patients with moderate mitral stenosis (mitral valve area 1.6–2.0 cm2) undergoing other cardiac surgery (class IIb, LOE C) |
|
| ||
|
Mitral
regurgitation |
No clear position | Concomitant mitral valve repair or replacement is indicated in patients with chronic severe primary mitral regurgitation undergoing cardiac surgery for other indications (class I, LOE B) Concomitant mitral valve repair is reasonable in patients with chronic moderate primary mitral regurgitation (stage B) undergoing cardiac surgery for other indications (class IIa, LOE C) Mitral valve surgery is reasonable for patients with chronic severe secondary mitral regurgitation (stages C and D) undergoing AVR (class IIa, LOE C) Mitral valve repair may be considered for patients with chronic moderate secondary mitral regurgitation (stage B) undergoing other cardiac surgery (class IIb, LOE C) |
|
| ||
|
Tricuspid
stenosis |
Tricuspid valve surgery is indicated in patients with severe tricuspid stenosis undergoing left-sided valve intervention (class I, LOE C) PBV can be attempted if PMC can be performed on the mitral valve |
Tricuspid valve surgery is recommended for patients with severe_tricuspid stenosis at the time of operation for left-sided valve disease (class I, LOE C) |
|
| ||
|
Tricuspid
regurgitation |
Tricuspid valve surgery is indicated in patients with severe primary or secondary tricuspid regurgitation undergoing left- sided valve surgery (class I, LOE C) Surgery should be considered in patients with moderate primary tricuspid regurgitation undergoing left-sided valve surgery (class IIa, LOE C) Surgery should be considered in patients with mild or moderate secondary tricuspid regurgitation with annular dilation (≥40 mm or >21 mm/m2) undergoing left-sided valve surgery (class IIa, LOE C) |
Tricuspid valve surgery is recommended for patients with severe tricuspid regurgitation (stages C and D) undergoing left-sided valve surgery (class I, LOE C) Tricuspid valve repair can be beneficial for patients with mild, moderate, or greater functional tricuspid regurgitation (stage B) at the time of left-sided valve surgery with either tricuspid annular dilation or prior evidence of right-sided heart failure (class IIa, LOE B) Tricuspid valve repair may be considered for patients with moderate functional tricuspid regurgitation (stage B) and pulmonary artery hypertension at the time of left-sided valve surgery (class IIb, LOE C) |
AVR, aortic valve replacement; LOE, level of evidence; PBV, percutaneous balloon valvuloplasty; PMC, percutaneous mitral commissurotomy. Adapted with permission from Unger 2011 10.
Surgical risk and long-term morbidity
Combined surgical procedures on multiple valves are associated with increased operative risk. Patients with MVD included in the EuroHeart Survey had an hospital mortality of 6.5% as compared with 0.9% to 3.9% for single valve surgery1. In a series of 513 patients undergoing multiple valve surgery, overall hospital mortality was 12.5% and overall 5-year mortality was 32.9%.54 Postoperatively, 80% of the patients discharged from hospital improved to NYHA functional class I or II, with only 0.6% remaining in functional class IV. The 5-year rate of freedom from late combined valve-related morbidity and mortality was 71.7%.54 Pulmonary artery hypertension was one of the main risk factors for increased risk of postoperative mortality.54 Among the 623,039 patients undergoing valvular surgery between 1993 and 2007 included in the STS database, 10.9% had multiple valve procedures4, 55. Overall, operative mortality almost doubled as compared with single-valve procedures (10.7% vs 5.7%)4. However, a higher proportion of patients with NYHA class III/IV congestive heart failure and a higher incidence of nonelective surgery with multiple valve procedures might have contributed to the increased mortality in these patients4. In this large series, unadjusted operative mortality was 10.7% for the combination of aortic and mitral surgery, 13.2% for aortic plus tricuspid, 9.7% for mitral plus tricuspid, and 14.0% for triple valve surgery, whereas unadjusted operative mortality was 4.9%, 6.9%, and 10.0% for isolated aortic, mitral, and tricuspid surgery, respectively4. Noticeably, results are improving over time, with a decrease in mortality from 1993 through 2007, despite worsening in preoperative risk profiles time2. In another analysis, risk factors significantly associated with operative mortality included emergency presentation, older age, renal failure, reoperation, endocarditis, diabetes mellitus, severe chronic lung disease, peripheral vascular disease, coronary artery disease, and female sex56. In a series of 871 patients with rheumatic heart disease undergoing triple-valve surgery, 30-day hospital mortality was 8%57. NYHA class IV functional status, ascites, and reduced LV ejection fraction were identified as independent risk factors for in-hospital mortality. Overall long-term survival was 71% +/− 3% at 5 years, and 59% +/− 5% at 10 years, with 74% of surviving patients remaining in NYHA class I or II57.
Together, the results from these studies demonstrate that, at the price of an increased operative risk, acceptable clinical improvement and late survival can be expected after a multiple valve operation. In addition, these data also indicate that the risk of late mortality after multiple valve surgery can be reduced by early surgical treatment, before pulmonary hypertension, progression to NYHA class IV, or deterioration of LV ejection fraction occur.
Risk of reoperation
Treatment decisions for patients with MVD require knowledge of the natural history of each specific valvular lesion. The risk of eventual reoperation and the prognostic impact of not correcting a less-than-severe lesion should also be taken into account. Increased operative mortality and poor long-term survival are to be expected after a ‘redo’ valve procedure58. Patient age and the aetiology of the secondary valve lesion are the main factors influencing these estimates. Therefore, the likelihood and timing of reoperation for the secondary valve lesion should be considered when planning the initial surgical procedure.
Moderately severe valve lesions have variable rates of progression; some progress in severity more often and more quickly. In patients with mild-to-moderate aortic stenosis, the average yearly increase in transaortic velocity and mean gradient is 0.3 m/s and 7 mmHg, respectively, whereas the decrease in valve area is 0.1 cm2 per year59. However, the pattern of progression varies according to its aetiology; aortic stenosis progresses faster in patients with degenerative disease than in those with a rheumatic or congenital aetiology60, 61. A higher degree of valvular calcification is independently associated with faster stenosis progression and worse outcome62. Aortic regurgitation is slow to progress. Patients with aortic regurgitation and normal LV systolic function who are asymptomatic have a low likelihood of progression to asymptomatic LV systolic dysfunction (<3.5% per year)63. The risk of developing symptoms or LV dysfunction is <6.0% per year, and the risk of sudden death <0.2% per year63. In a series of 262 patients with moderate aortic regurgitation, the average rate of progression to severe aortic regurgitation was 1.9% per year, and only 0.3% of patients were referred for aortic valve replacement64. The rate of mitral valve narrowing in patients with rheumatic mitral stenosis is variable, with an average decline of 0.09 ± 0.21 cm2 per year65, 66. The rate of progression is, however, faster in patients with a greater mitral valve echocardiographic score and higher transmitral gradients.
Most recommendations on the management of less-than-severe valve lesions in patients undergoing surgery for another valve lesion have been extrapolated from data obtained with CABG surgery. After CABG surgery, the long-term mortality risk is more than two-fold higher in patients with moderate-to-severe aortic stenosis (aortic valve area 1.0–1.25 cm2) than patients with no aortic stenosis67. The available data indicate that, during CABG surgery, concomitant aortic valve replacement for moderate aortic stenosis should be recommended if surgical risk is not prohibitive68. The situation is less clear for mild aortic stenosis,69-71 but concomitant aortic valve replacement could be considered in patients who are expected to be ‘rapid progressors’ (that is, those with documented rapid increase in aortic velocity, moderate-to-severe valve calcification, or both), providing that reasonable life expectancy is anticipated. Patients with a high surgical risk could be treated conservatively with CABG surgery with a percutaneous valve replacement performed later if necessary.
Risk of mitral or tricuspid regurgitation
Spontaneous changes in mitral or tricuspid regurgitation can occur after surgery on a downstream valvular lesion. The severity of mitral regurgitation can be influenced by the presence of aortic valve disease12, 18, 72. After aortic valve replacement, the LV systolic pressure drops, thereby reducing the transmitral pressure gradient. In addition, reverse LV remodelling can be initiated as early as the postoperative period20, which contributes to reduced mitral regurgitation (FIGURE 2). However, the mitral valve response to aortic valve replacement is heterogeneous; whereas a favourable response has been described in a substantial number of patients, it may remain unchanged or even worsen in some patients12, 14. Primary mitral regurgitation is less likely than secondary regurgitation to improve after aortic valve replacement15, 73. In addition to a secondary aetiology, several factors have been associated with an improvement in the magnitude of mitral regurgitation after aortic valve replacement: poor LV ejection fraction and larger LV volumes (indicating a greater potential for reverse remodelling), smaller left atrial size, absence of atrial fibrillation or pulmonary hypertension (consistent with lesser chronic repercussions of mitral regurgitation), and higher preoperative transaortic pressure gradient and lesser postoperative prosthesis–patient mismatch (consistent with a greater postoperative reduction in systolic transmitral gradient)12, 18. In addition, the use of the self-expanding valves seems to be associated with less improvement in mitral regurgitation than the balloon expandable valves 74, 75. This finding could be explained by anatomical or functional interference with mitral leaflet excursion annulus geometry, or by the increased incidence of LV dyssynchrony resulting from left bundle branch block or pacemaker insertion. Balloon aortic valvuloplasty has been shown to reduce the severity of mitral regurgitation in nearly half of patients with severe aortic stenosis and coexistent mitral regurgitation,76 but no specific data exist to support the routine use of this procedure to select patients who should not receive an additional mitral procedure during aortic valve replacement.
Secondary tricuspid regurgitation is an independent predictor of long-term mortality7, 33-36, 77. Mitral and aortic valve replacement tend to decrease pulmonary vascular pressures and so reduce right ventricular overload, therefore, conservative management of moderate secondary tricuspid regurgitation has been postulated78. However, as discussed, the pathophysiological links between left-sided valve disease and secondary tricuspid regurgitation are not linear or predictable. Several studies have demonstrated that the presence of untreated moderate-to-severe tricuspid regurgitation at the time of aortic or mitral valve surgery is associated with reduced postoperative survival7, 33. Moreover, late onset of tricuspid regurgitation is associated with poor functional tolerance and reduced exercise capacity79. Redo surgery for secondary tricuspid regurgitation is associated with operative mortality of 10–25%80. Accordingly, patients with severe secondary tricuspid regurgitation, or those with mild-to-moderate secondary tricuspid regurgitation and evidence of right-sided heart failure or annular dilation (>40 mm when measured in end-diastole in the four-chamber view, or >70 mm when as assessed by the surgeon in the operating room) are generally recommended to undergo tricuspid valve surgery at the time the left-sided valve lesion is fixed (FIGURES 4, 5)40, 53, 81.
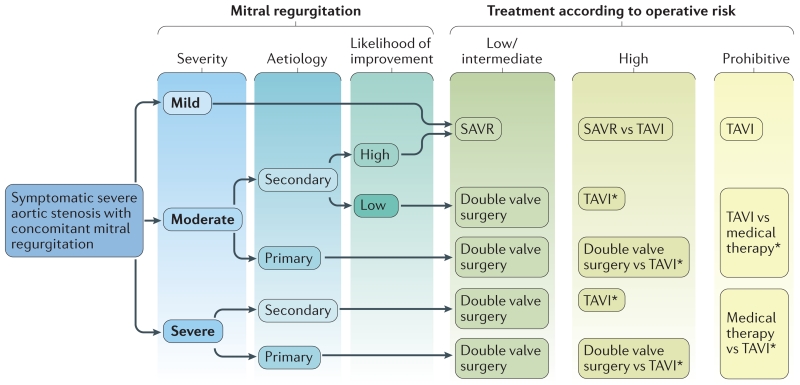
Figure 5. Management of severe aortic stenosis requiring surgery, with concomitant mitral regurgitation.
Mitral regurgitation is highly likely to improve with aortic valve replacement in the absence of atrial fibrillation, left atrial dilatation, or pulmonary hypertension. This algorithm requires validation by further studies. SAVR, surgical aortic valve replacement; TAVI, transcatheter aortic valve implantation. *A staged approach is possible, consisting of TAVI followed by implantation of a MitraClip® (Evalve, Inc., USA) if symptomatic mitral regurgitation persists. Adapted from Nombela-Franco 2014 12.
Choice of surgical technique
Whether valve repair or replacement is the optimal surgical strategy should be considered when making management decisions for patients with MVD. In a propensity-matched analysis of patients with aortic and mitral valve lesions, aortic valve replacement and mitral valve repair improved late survival when compared with replacement of both valves82. Similarly, in another study of patients with rheumatic heart disease, mitral valve repair plus aortic valve replacement improved event-free survival when compared with double valve replacement83. In the STS database, 23,404 patients underwent concomitant aortic valve replacement and mitral valve surgery between 1993 and 200784. Mitral valve repair was performed in 46% and these patients had a 39% reduction in the risk of operative mortality when compared with those undergoing mitral valve replacement, despite them being of older age, with a lower LV ejection fraction, and a higher incidence of concomitant CABG surgery84. Therefore, efforts should be directed towards improving rates of mitral valve repair, even if prosthetic valve replacement on another valve may decrease the desire to repair.
Controversy exists, however, as to whether repair or replacement of the mitral valve is preferred in patients who have significant secondary mitral regurgitation and are undergoing aortic valve replacement. One study reported reduced in-hospital mortality with mitral valve repair (11% versus 18% for replacement), but postdischarge survival did not differ significantly between the two strategies85. On the other hand, other studies that included patients with primary or secondary mitral regurgitation reported no survival benefit of mitral valve repair with aortic valve replacement over double valve replacement, and an increased long-term incidence of mitral valve failure in patients undergoing mitral repair was observed86, 87. In a propensity matched analysis88 and in the Cardiothoracic Surgery Network randomized trial89, mitral valve replacement was associated with better freedom from recurrent secondary ischaemic mitral regurgitation during follow-up compared with mitral valve repair.
When a patient is to undergo double valve replacement, using the same type of prosthesis in both locations (bioprosthesis or mechanical) has been recommended so as not to lose the advantages of each valvular substitute. That is, to avoid superimposing the risk of anticoagulation and the risk of bioprosthesis deterioration8.
For the surgical treatment of tricuspid regurgitation at the time of left-sided valve surgery, the preferred technique is tricuspid annuloplasty given that the tricuspid regurgitation is most often due to annulus dilation with ensuing lack of leaflet coaptation and that tricuspid valve replacement is associated with a higher rate of complications compared to annuloplasty 34, 81, 90, 91
Percutaneous approaches
Percutaneous treatment of aortic stenosis and mitral regurgitation is increasingly used in patients at high surgical risk. Limited series of combined transcatheter treatment of aortic stenosis and mitral regurgitation have been reported92, 93. In carefully selected patients, a staged approach has been proposed—the valve stenosis is treated first by TAVI, followed by subsequent implantation of a MitraClip® (Evalve, Inc., USA) if moderate-to-severe mitral regurgitation with symptoms persists. This strategy has been associated with good procedural success rates and, at 6 months, acceptable functional outcomes and survival93.
In patients with severe aortic stenosis undergoing transcatheter aortic valve replacement, the concomitant mitral stenosis is generally of degenerative aetiology (that is, mitral annulus calcification) with significant thickening and calcification of the subvalvular apparatus and absence of commissural fusion, and is, therefore, not suitable for percutaneous mitral commissurotomy94. However, in exceptional circumstances, circular mitral annular calcification is severe enough to cause hemodynamically significant mitral stenosis and may offer enough support to allow stable anchoring of a percutaneous mitral prosthesis95, 96.
Several percutaneous procedures have been recently developed and successfully applied to treat secondary tricuspid regurgitation 90, 97. These emerging less invasive techniques provide a valuable alternative to surgery to correct tricuspid regurgitation i) at the same time of other percutaneous intervention on the aortic or mitral valve or ii) as a staged procedure following previous surgical or percutaneous intervention on another valve.
More studies are needed to clarify these treatment pathways and to incorporate evolving transcatheter options for mitral valve replacement and tricuspid repair.
The heart valve team
The evaluation and treatment of patients with MVD can be incredibly complex. The numerous diagnostic pitfalls, emergence of innovative transcatheter therapies, and treatment of elderly high-risk patients with multiple morbidities require the expertise of a multidisciplinary heart valve team (BOX 1). Expertise in cardiac surgery, transcatheter interventions, cardiac imaging, haemodynamics, anaesthesia, and geriatrics are critical to making the best recommendations and tailoring treatment strategies to optimize outcomes for the individual patient98.
Box 1. Factors to be considered by the heart valve team.
Life expectancy of the patient
Nature and severity of symptoms
Which valve lesion is dominant
Aetiology and severity of each valve lesion
Size and function of the left and right ventricles
Presence and severity of pulmonary hypertension
Anticipated progression of a secondary valve lesion if left untreated
Transcatheter options
Staged procedures versus all-at-once treatment
Procedural risk
Local experience of the treatment team
Patient wishes
Clinical scenarios
Three main clinical scenarios are encountered in clinical practice—the patient with two or more severe lesions, the patient with one severe lesion plus at least one or nonsevere lesion, and the patient with two or more nonsevere lesions. The recommendations for concomitant valve surgery in patients undergoing surgery on another valve, as outlined in the AHA/ACC41 and ESC/EACTS54 guidelines, are presented in TABLE 2.
Two or more severe lesions
The general recommendation for patients with two or more severely stenotic or regurgitant lesions, and who are symptomatic or have ventricular dysfunction or dilatation, is for all lesions should be surgically corrected concomitantly40, 53. However, for patients at high or prohibitive risk for surgery, alternative treatment pathways have been proposed. In such cases, the staged percutaneous approach involving the Mitraclip® outlined above might be considered. This rapidly evolving area will only become more complex with the emergence of transcatheter options for tricuspid disease.
One severe lesion plus at least one nonsevere lesion
The decision to perform an intervention should be based on the recommendations for the predominant valvular lesion53. Whether an additional procedure on a coexistent nonsevere valvular lesion is required can be a difficult to determine. The surgical risk of a combined valve procedure and the long-term increase in morbidity associated with multiple valve prostheses should be balanced against the risk of eventual reoperation and the prognostic impact of not correcting the less-severe lesion during the initial procedure. In addition, life expectancy, comorbidities, and patient wishes should all be taken into account.
In the current AHA/ACC41 and ESC/EACTS54 guidelines, moderate aortic stenosis, moderate aortic regurgitation, moderate primary mitral regurgitation, and moderate primary or secondary tricuspid regurgitation (provided that tricuspid annulus is dilated) are all class IIa recommendations for performing a second surgical valve procedure in patients undergoing surgery for another valve lesion or other cardiac surgery. Moderate mitral stenosis, moderate secondary mitral regurgitation, and moderate tricuspid regurgitation (in the presence of pulmonary artery hypertension) are considered class IIb indications in the AHA/ACC guidelines40.
In patients with one severe and one moderately-severe valve lesion who are asymptomatic, the increased operative risk associated with a double valve procedure represents an incentive to postpone surgery until symptoms develop or another class I indication for surgery exists. Decisional algorithms for patients with aortic stenosis presenting with concomitant mitral regurgitation have been proposed. These algorithms take into account the severity and mechanism of mitral regurgitation, the likelihood of spontaneous improvement should isolated aortic valve replacement be performed, as well as the individual surgical risk (FIGURE 5)12, 18. In patients with severe mitral stenosis and concomitant moderate aortic valve disease, percutaneous mitral commissurotomy can be performed to postpone double-valve surgery. Indeed, only a minority of these patients will require subsequent aortic valve replacement on long-term follow-up, emphasizing the limited progression of aortic regurgitation in this setting 99.
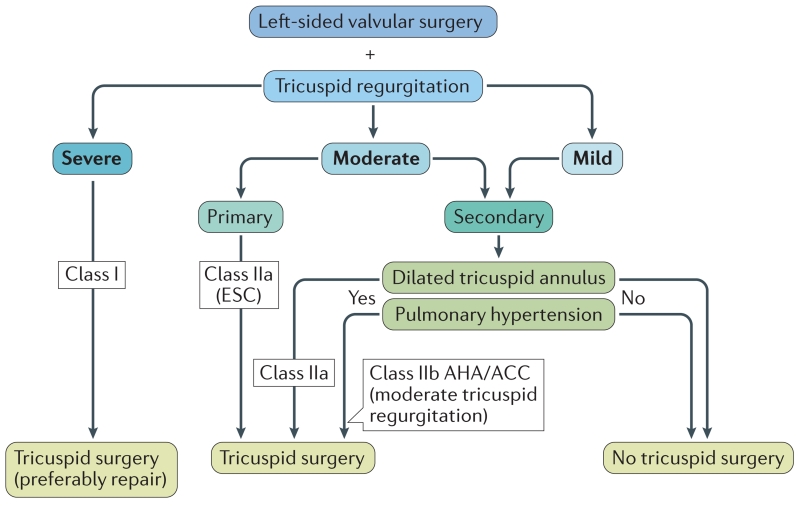
The management of tricuspid regurgitation in patients undergoing left-sided valve surgery as recommended in the AHA/ACC40 and ESC/ EACTS53 guidelines is depicted in FIGURE 6. Tricuspid valve repair or replacement is recommended (class I) in patients with severe tricuspid regurgitation undergoing surgery for aortic or mitral valve disease. Tricuspid valve repair should be considered in patients undergoing left-sided valve surgery if they have mild or moderate tricuspid regurgitation and tricuspid annulus dilation (class IIa) or pulmonary hypertension with tricuspid annulus dilation (class IIb).40,53
Figure 6. Management of tricuspid regurgitation in patients undergoing left-sided valve surgery.
Indications for surgery on the tricuspid valve according to the severity and aetiology (primary versus secondary) of tricuspid regurgitation, and to the presence of tricuspid annulus dilation or pulmonary hypertension40, 53.
Importantly, in some elderly patients, performing an intervention to improve quality of life can be more important than prolonging life. Procedures that are beneficial only after a long period of survival might be less suitable or appropriate for very elderly patients. Single valve procedures that are less demanding and carry a lower risk than double or triple valve procedures should be considered for these individuals, even at the cost of incomplete repair.
Two or more nonsevere lesions
In patients with nonsevere MVD, determining the global consequences of all lesions is of the utmost importance. Even moderate lesions , when combined, can lead to severe functional intolerance, symptoms, LV dilatation or dysfunction, and pulmonary hypertension. This combination of lesions is the most challenging in terms of therapeutic decision making. The consequences of the overall haemodynamic burden on the cardiac chambers, pulmonary circulation, and patient’s functional capacity should be assessed. Therefore, maximal exercise capacity and peak oxygen consumption, parameters of ventricular function (such as LV global longitudinal strain, RV tricuspid annulus plane excursion, or free-wall strain), as well as natriuretic peptide levels and pulmonary arterial pressure at rest and during exercise should be measured100, 101. Surgery might be appropriate for selected patients in whom the combination of moderate lesions has a meaningful effect on the functional parameters mentioned above. However, further studies are needed to identify and validate criteria for intervention in this subset of patients.
Conclusions
Degenerative aetiologies have replaced rheumatic heart disease as the predominant causes of MVD, the prevalence of which is increasing in developed countries owing to aging of the population. Clinicians must be aware of specific pitfalls associated with the evaluation of MVD; diagnosis and treatment of this condition MVD depend on the individual patient’s presentation and combination of valve pathologies. Patient-centred therapeutic decisions should be made by a multidisciplinary heart valve team, with integration of numerous factors to optimize clinical outcomes. Much work remains to be done to develop evidence to guide treatment decisions for these complex clinical cases. Several randomized trials are currently ongoing to assess the benefit of performing concomitant tricuspid annuloplasty at the time of mitral valve surgery in patients with mild or moderate tricuspid regurgitation. Similar studies will also be needed for patients undergoing aortic valve surgery. Randomized trials are also needed to determine if concomitant treatment of moderate mitral regurgitation at the time of surgical or percutaneous aortic valve procedure improve patients outcomes.
Supplementary Material
Key points.
Multivalvular disease (MVD) is a highly prevalent condition; rheumatic heart disease is the predominant aetiology in developing countries, whereas degenerative aetiologies are increasingly common in developed countries
Haemodynamic interactions between valve lesions can promote, exacerbate, or, in contrast, blunt the clinical expression of each singular lesion
Several diagnostic tools used for the assessment of valve stenosis or regurgitation have been validated in patients with single valve disease, but such tools might not be valid for MVD
Therapeutic decisions should be made by a heart valve team, considering the severity of MVD, the patient’s life expectancy and comorbidities, and the risks of multiple prostheses and eventual reoperation
The introduction of transcatheter valve therapies is changing the therapeutic paradigm, but further studies are needed to guide therapeutic decision-making
Acknowledgements
B.R.L. is supported by NIH K23 HL116660. P.P. holds the Canada Research Chair in Valvular Heart Disease and his research program is funded by the Canadian Institutes of Health Research (Grant numbers FDN-143225, MOP 126072, MOP 114997 and MOP 102737) (Ottawa, Ontario, Canada).
B.R.L. has received research support from and served on the scientific advisory board for Roche Diagnostics. P.P. has Core Lab contracts with Edwards Lifesciences, for which he receives no direct compensation, and is a speaker for St. Jude Medical.
Footnotes
Author contributions
P.U. prepared the first version of the manuscript. P.P., M.A.C., B.L., and P.M. made important revisions and contributed to preparation of the figures and tables..
Competing interests
The other authors declare no competing interests.
REFERENCES
- 1.Iung B, et al. A prospective survey of patients with valvular heart disease in Europe : The Euro Heart Survey on Valvular heart Disease. Eur. Heart J. 2003;24:1231–1243. doi: 10.1016/s0195-668x(03)00201-x. [DOI] [PubMed] [Google Scholar]
- 2.Lee R, et al. Fifteen-year outcome trends for valve surgery in North America. Ann Thorac Surg. 2011;91:677–684. doi: 10.1016/j.athoracsur.2010.11.009. [DOI] [PubMed] [Google Scholar]
- 3.Agarwal A, et al. Results of repeat balloon valvuloplasty for treatment of aortic stenosis in patients aged 59 to 104 years. Am J Cardiol. 2005;95:43–47. doi: 10.1016/j.amjcard.2004.08.061. [DOI] [PubMed] [Google Scholar]
- 4.Vassileva CM, et al. Outcome characteristics of multiple-valve surgery: comparison with single-valve procedures. Innovations. (Phila) 2014;9:27–32. doi: 10.1097/IMI.0000000000000028. [DOI] [PubMed] [Google Scholar]
- 5.Leon MB, et al. Transcatheter aortic-valve implantation for aortic stenosis in patients who cannot undergo surgery. N Eng J Med. 2010;363:1597–1607. doi: 10.1056/NEJMoa1008232. [DOI] [PubMed] [Google Scholar]
- 6.Smith CR, et al. Transcatheter versus surgical aortic-valve replacement in high-risk patients. N. Engl. J. Med. 2011;364:2187–2198. doi: 10.1056/NEJMoa1103510. [DOI] [PubMed] [Google Scholar]
- 7.Lindman BR, et al. Effect of tricuspid regurgitation and the right heart on survival after transcatheter aortic valve replacement: Insights from the placement of aortic transcatheter Valves II inoperable cohort. Circ. Cardiovasc Interv. 2015;8:1–10. doi: 10.1161/CIRCINTERVENTIONS.114.002073. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Roberts WC, Sullivan MF. Clinical and necropsy observations early after simultaneous replacement of the mitral and aortic valves. Am. J. Cardiol. 1986;58:1067–1084. doi: 10.1016/0002-9149(86)90116-5. [DOI] [PubMed] [Google Scholar]
- 9.Goldbarg SH, Elmariah S, Miller MA, Fuster V. Insights into degenerative aortic valve disease. J Am Coll Cardiol. 2007;50:1205–1213. doi: 10.1016/j.jacc.2007.06.024. [DOI] [PubMed] [Google Scholar]
- 10.Unger P, Rosenhek R, Dedobbeleer C, Berrebi A, Lancellotti P. Management of multiple valve disease. Heart. 2011;97:272–277. doi: 10.1136/hrt.2010.212282. [DOI] [PubMed] [Google Scholar]
- 11.DeBonis M, Maisano F, La CG, Alfieri O. Treatment and management of mitral regurgitation. Nat. Rev. Cardiol. 2012;9:133–146. doi: 10.1038/nrcardio.2011.169. [DOI] [PubMed] [Google Scholar]
- 12.Nombela-Franco L, et al. Significant mitral regurgitation left untreated at the time of aortic valve replacement: A comprehensive review of a frequent entity in the transcatheter aortic valve replacement era. J Am Coll Cardiol. 2014;63:2643–2658. doi: 10.1016/j.jacc.2014.02.573. [DOI] [PubMed] [Google Scholar]
- 13.Kodali SK, Moses JW. Coronary artery disease and aortic stenosis in the transcatheter aortic valve replacement era: old questions, new paradigms: the evolving role of percutaneous coronary intervention in the treatment of patients with aortic stenosis. Circulation. 2012;125:975–977. doi: 10.1161/CIRCULATIONAHA.111.087965. [DOI] [PubMed] [Google Scholar]
- 14.Barbanti M, et al. Impact of preoperative moderate/severe mitral regurgitation on 2-year outcome after transcatheter and surgical aortic valve replacement: insight from the Placement of Aortic Transcatheter Valve (PARTNER) Trial Cohort A. Circulation. 2013;128:2776–2784. doi: 10.1161/CIRCULATIONAHA.113.003885. [DOI] [PubMed] [Google Scholar]
- 15.Bedogni F, et al. Interplay between mitral regurgitation and transcatheter aortic valve replacement with the CoreValve Revalving System: a multicenter registry. Circulation. 2013;128:2145–2153. doi: 10.1161/CIRCULATIONAHA.113.001822. [DOI] [PubMed] [Google Scholar]
- 16.Barreiro CJ, et al. Aortic valve replacement and concomitant mitral valve regurgitation in the elderly: impact on survival and functional outcome. Circulation. 2005;112:I443–I447. doi: 10.1161/CIRCULATIONAHA.104.526046. [DOI] [PubMed] [Google Scholar]
- 17.Kim DH, et al. Aortic valve adaptation to aortic root dilatation: insights into the mechanism of functional aortic regurgitation from 3-dimensional cardiac computed tomography. Circ. Cardiovasc. Imaging. 2014;7:828–835. doi: 10.1161/CIRCIMAGING.113.001976. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Unger P, et al. Mitral regurgitation in patients with aortic stenosis undergoing valve replacement. Heart. 2009 doi: 10.1136/hrt.2009.165548. [DOI] [PubMed] [Google Scholar]
- 19.Paradis JM, et al. Aortic stenosis and coronary artery disease: What do we know? What don’t we know? A comprehensive review of the literature with proposed treatment algorithms. Eur. Heart J. 2014;35:2069–2082. doi: 10.1093/eurheartj/ehu247. [DOI] [PubMed] [Google Scholar]
- 20.Unger P, et al. Effects of valve replacement for aortic stenosis on mitral regurgitation. Am J Cardiol. 2008;102:1378–1382. doi: 10.1016/j.amjcard.2008.07.021. [DOI] [PubMed] [Google Scholar]
- 21.Greve AM, et al. Prognostic importance of atrial fibrillation in asymptomatic aortic stenosis: The Simvastatin and Ezetimibe in Aortic Stenosis study. Int. J Cardiol. 2013;166:72–76. doi: 10.1016/j.ijcard.2011.09.064. [DOI] [PubMed] [Google Scholar]
- 22.Kristensen CB, Jensen JS, Sogaard P, Carstensen HG, Mogelvang R. Atrial fibrillation in aortic stenosis--echocardiographic assessment and prognostic importance. Cardiovasc. Ultrasound. 2012;10:38. doi: 10.1186/1476-7120-10-38. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Unger P, Lancellotti P, de Canniere D. The clinical challenge of concomitant aortic and mitral valve stenosis. Acta Cardiol. 2016;71:3–6. doi: 10.2143/AC.71.1.3132091. [DOI] [PubMed] [Google Scholar]
- 24.Honey M. Clinical and haemodynamic observations on combined mitral and aortic stenosis. Br. Heart J. 1961;23:545–555. doi: 10.1136/hrt.23.5.545. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Zitnik RS, et al. The masking of aortic stenosis by mitral stenosis. Am. Heart J. 1965;69:22–30. doi: 10.1016/0002-8703(65)90212-7. [DOI] [PubMed] [Google Scholar]
- 26.Otto CM, Bonow RO. In: Braunwald’s Heart Disease. Libby P, Bonow RO, Mann DL, Zipes DP, editors. Saunders Elsevier; Philadelphia, PA: 2008. pp. 1625–1693. [Google Scholar]
- 27.Tyagi G, Dang P, Pasca I, Patel R, Pai RG. Progression of degenerative mitral stenosis: insights from a cohort of 254 patients. J Heart Valve Dis. 2014;23:707–712. [PubMed] [Google Scholar]
- 28.Gash AK, Carabello BA, Kent RL, Frazier JA, Spann JF. Left ventricular performance in patients with coexistent mitral stenosis and aortic insufficiency. J. Am. Coll. Cardiol. 1984;3:703–711. doi: 10.1016/s0735-1097(84)80246-6. [DOI] [PubMed] [Google Scholar]
- 29.Cohn LH, Mason DT, Ross J, Jr., Morrow AG, Braunwald E. Preoperative assessment of aortic regurgitation in patients with mitral valve disease. Am. J. Cardiol. 1967;19:177–182. doi: 10.1016/0002-9149(67)90530-9. [DOI] [PubMed] [Google Scholar]
- 30.Niles N, et al. Preoperative left and right ventricular performance in combined aortic and mitral regurgitation and comparison with isolated aortic or mitral regurgitation. Am J Cardiol. 1990;65:1372–1378. doi: 10.1016/0002-9149(90)91330-9. [DOI] [PubMed] [Google Scholar]
- 31.Gentles TL, Finucane AK, Remenyi B, Kerr AR, Wilson NJ. Ventricular Function Before and After Surgery for Isolated and Combined Regurgitation in the Young. Ann. Thorac. Surg. 2015;100:1383–1389. doi: 10.1016/j.athoracsur.2015.06.009. [DOI] [PubMed] [Google Scholar]
- 32.Skudicky D, Essop MR, Sareli P. Time-related changes in left ventricular function after double valve replacement for combined aortic and mitral regurgitation in a young rheumatic population. Predictors of postoperative left ventricular performance and role of chordal preservation. Circulation. 1997;95:899–904. doi: 10.1161/01.cir.95.4.899. [DOI] [PubMed] [Google Scholar]
- 33.Taramasso M, et al. The growing clinical importance of secondary tricuspid regurgitation. J. Am. Coll. Cardiol. 2012;59:703–710. doi: 10.1016/j.jacc.2011.09.069. [DOI] [PubMed] [Google Scholar]
- 34.Chikwe J, Itagaki S, Anyanwu A, Adams DH. Impact of concomitant tricuspid annuloplasty on tricuspid regurgitation, right ventricular function, and pulmonary artery hypertension after repair of mitral valve prolapse. J Am Coll Cardiol. 2015;65:1931–1938. doi: 10.1016/j.jacc.2015.01.059. [DOI] [PubMed] [Google Scholar]
- 35.Jeong DS, et al. Fate of functional tricuspid regurgitation in aortic stenosis after aortic valve replacement. J. Thorac. Cardiovasc. Surg. 2014;148:1328–1333. doi: 10.1016/j.jtcvs.2013.10.056. [DOI] [PubMed] [Google Scholar]
- 36.Dahou A, et al. Tricuspid regurgitation is associated with increased risk of mortality in patients with low-flow low-gradient aortic stenosis and reduced ejection fraction: results of the multicenter TOPAS study (True or pseudo-severe aortic stenosis) JACC Cardiovasc Interv. 2015;8:588–596. doi: 10.1016/j.jcin.2014.08.019. [DOI] [PubMed] [Google Scholar]
- 37.Lancellotti P, et al. Recommendations for the echocardiographic assessment of native valvular regurgitation: an executive summary from the European Association of Cardiovascular Imaging. Eur Heart J Cardiovasc Imaging. 2013;14:611–644. doi: 10.1093/ehjci/jet105. [DOI] [PubMed] [Google Scholar]
- 38.Moro E, Nicolosi GL, Zanuttini D, Cervesato E, Roelandt J. Influence of aortic regurgitation on the assessment of the pressure half-time and derived mitral-valve area in patients with mitral stenosis. Eur. Heart J. 1988;9:1010–1017. doi: 10.1093/oxfordjournals.eurheartj.a062592. [DOI] [PubMed] [Google Scholar]
- 39.Flachskampf FA, et al. Aortic regurgitation shortens Doppler pressure half-time in mitral stenosis: clinical evidence, in vitro simulation and theoretic analysis. J. Am. Coll. Cardiol. 1990;16:396–404. doi: 10.1016/0735-1097(90)90592-d. [DOI] [PubMed] [Google Scholar]
- 40.Nishimura RA, et al. 2014 AHA/ACC guideline for the management of patients with valvular heart disease: Executive summary. A report of the American College of Cardiology/American heart association task force on practice guidelines. J Am Coll Cardiol. 2014;63:2438–2488. doi: 10.1016/j.jacc.2014.02.537. [DOI] [PubMed] [Google Scholar]
- 41.Goldenheim PD, Kazemi H. Cardiopulmonary monitoring of critically ill patients (2) N. Engl. J. Med. 1984;311:776–780. doi: 10.1056/NEJM198409203111206. [DOI] [PubMed] [Google Scholar]
- 42.van GA, Ditchey RV, Groves BM, Wagner WW, Jr., Reeves JT. Thermodilution method overestimates low cardiac output in humans. Am. J. Physiol. 1983;245:H690–H692. doi: 10.1152/ajpheart.1983.245.4.H690. [DOI] [PubMed] [Google Scholar]
- 43.Tops LF, et al. Noninvasive evaluation of the aortic root with multislice computed tomography implications for transcatheter aortic valve replacement. JACC Cardiovasc Imaging. 2008;1:321–330. doi: 10.1016/j.jcmg.2007.12.006. [DOI] [PubMed] [Google Scholar]
- 44.O’Brien B, et al. Integration of 3D imaging data in the assessment of aortic stenosis: impact on classification of disease severity. Circ. Cardiovasc. Imaging. 2011;4:566–573. doi: 10.1161/CIRCIMAGING.111.964916. [DOI] [PubMed] [Google Scholar]
- 45.Ng AC, et al. Comparison of aortic root dimensions and geometries before and after transcatheter aortic valve implantation by 2- and 3-dimensional transesophageal echocardiography and multislice computed tomography. Circ. Cardiovasc Imaging. 2010;3:94–102. doi: 10.1161/CIRCIMAGING.109.885152. [DOI] [PubMed] [Google Scholar]
- 46.Clavel MA, et al. Aortic valve area calculation in aortic stenosis by CT and doppler echocardiography. JACC Cardiovasc Imaging. 2015;8:248–257. doi: 10.1016/j.jcmg.2015.01.009. [DOI] [PubMed] [Google Scholar]
- 47.Clavel MA, et al. Validation of conventional and simplified methods to calculate projected valve area at normal flow rate in patients with low flow, low gradient aortic stenosis: the multicenter TOPAS (True or Pseudo Severe Aortic Stenosis) study. J Am Soc Echocardiogr. 2010;23:380–386. doi: 10.1016/j.echo.2010.02.002. [DOI] [PubMed] [Google Scholar]
- 48.Clavel MA, et al. The complex nature of discordant severe calcified aortic valve disease grading: New insights from combined Doppler-echocardiographic and computed tomographic study. J Am Coll Cardiol. 2013;62:2329–2338. doi: 10.1016/j.jacc.2013.08.1621. [DOI] [PubMed] [Google Scholar]
- 49.Clavel MA, et al. Impact of aortic valve calcification, as measured by MDCT, on survival in patients with aortic stenosis: results of an international registry study. J Am. Coll Cardiol. 2014;64:1202–1213. doi: 10.1016/j.jacc.2014.05.066. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50.Schlosshan D, Aggarwal G, Mathur G, Allan R, Cranney G. Real-time 3D transesophageal echocardiography for the evaluation of rheumatic mitral stenosis. JACC. Cardiovasc. Imaging. 2011;4:580–588. doi: 10.1016/j.jcmg.2010.12.009. [DOI] [PubMed] [Google Scholar]
- 51.Chu JW, et al. Assessing mitral valve area and orifice geometry in calcific mitral stenosis: a new solution by real-time three-dimensional echocardiography. J. Am. Soc. Echocardiogr. 2008;21:1006–1009. doi: 10.1016/j.echo.2008.05.010. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 52.Delgado V, et al. Multimodality imaging before, during, and after percutaneous mitral valve repair. Heart. 2011;97:1704–1714. doi: 10.1136/hrt.2011.227785. [DOI] [PubMed] [Google Scholar]
- 53.Vahanian A, et al. Guidelines on the management of valvular heart disease (version 2012): Joint task force on the management of valvular heart disease of the European Society of Cardiology (ESC) and the European Association for Cardio-Thoracic Surgery (EACTS) Eur J Cardiothor Surg. 2012;42:S1–S44. doi: 10.1093/ejcts/ezs455. [DOI] [PubMed] [Google Scholar]
- 54.Galloway AC, et al. Multiple valve operation for advanced valvular heart disease: results and risk factors in 513 patients. J. Am. Coll. Cardiol. 1992;19:725–732. doi: 10.1016/0735-1097(92)90509-l. [DOI] [PubMed] [Google Scholar]
- 55.STS Database 2014 Online Source: http://www.sts.org/national-database.
- 56.Rankin JS, et al. The Society of Thoracic Surgeons risk model for operative mortality after multiple valve surgery. Ann. Thorac. Surg. 2013;95:1484–1490. doi: 10.1016/j.athoracsur.2012.11.077. [DOI] [PubMed] [Google Scholar]
- 57.Han QQ, et al. Primary triple valve surgery for advanced rheumatic heart disease in Mainland China: a single-center experience with 871 clinical cases. Eur. J. Cardiothorac. Surg. 2007;31:845–850. doi: 10.1016/j.ejcts.2007.02.005. [DOI] [PubMed] [Google Scholar]
- 58.Fukunaga N, et al. Clinical outcomes of redo valvular operations: a 20-year experience. Ann. Thorac. Surg. 2012;94:2011–2016. doi: 10.1016/j.athoracsur.2012.06.045. [DOI] [PubMed] [Google Scholar]
- 59.Otto CM, et al. Prospective study of asymptomatic valvular aortic stenosis. Clinical, echocardiographic, and exercise predictors of outcome. Circulation. 1997;95:2262–2270. doi: 10.1161/01.cir.95.9.2262. [DOI] [PubMed] [Google Scholar]
- 60.Wagner S, Selzer A. Patterns of progression of aortic stenosis: a longitudinal hemodynamic study. Circulation. 1982;65:709–712. doi: 10.1161/01.cir.65.4.709. [DOI] [PubMed] [Google Scholar]
- 61.Vaturi M, et al. The natural history of aortic valve disease after mitral valve surgery. J Am Coll Cardiol. 1999;33:2003–2008. doi: 10.1016/s0735-1097(99)00112-6. [DOI] [PubMed] [Google Scholar]
- 62.Rosenhek R, et al. Predictors of outcome in severe, asymptomatic aortic stenosis. N Engl J Med. 2000;343:611–617. doi: 10.1056/NEJM200008313430903. [DOI] [PubMed] [Google Scholar]
- 63.Borer JS, Bonow RO. Contemporary approach to aortic and mitral regurgitation. Circulation. 2003;108:2432–2438. doi: 10.1161/01.CIR.0000096400.00562.A3. [DOI] [PubMed] [Google Scholar]
- 64.Weisenberg D, et al. Mid-term echocardiographic progression of patients with moderate aortic regurgitation: implications for aortic valve surgery. J. Heart Valve Dis. 2013;22:192–194. [PubMed] [Google Scholar]
- 65.Gordon SPF, Douglas PS, Come PC, Manning WJ. Two-dimensional and Doppler echocardiographic determinants of the natural history of mitral valve narrowing in patients with rheumatic mitral stenosis: implications for follow-up. J Am Coll Cardiol. 1992;19:968–973. doi: 10.1016/0735-1097(92)90280-z. [DOI] [PubMed] [Google Scholar]
- 66.Sagie A, et al. Doppler echocardiographic assessment of long-term progression of mitral stenosis in 103 patients: valve area and right heart disease. J. Am. Coll. Cardiol. 1996;28:472–479. doi: 10.1016/0735-1097(96)00153-2. [DOI] [PubMed] [Google Scholar]
- 67.Thalji NM, et al. Untreated aortic valve stenosis identified at the time of coronary artery bypass grafting: thresholds associated with adverse prognosis. Eur. J. Cardiothorac. Surg. 2015;47:712–719. doi: 10.1093/ejcts/ezu231. [DOI] [PubMed] [Google Scholar]
- 68.Dagenais F, Mathieu P, Doyle D, Dumont E, Voisine P. Moderate aortic stenosis in coronary artery bypass grafting patients more than 70 years of age: to replace or not to replace? Ann. Thorac. Surg. 2010;90:1495–1499. doi: 10.1016/j.athoracsur.2010.06.036. [DOI] [PubMed] [Google Scholar]
- 69.Sareyyupoglu B, et al. Management of mild aortic stenosis at the time of coronary artery bypass surgery: should the valve be replaced? Ann Thorac Surg. 2009;88:1224–1231. doi: 10.1016/j.athoracsur.2009.05.085. [DOI] [PubMed] [Google Scholar]
- 70.Boning A, et al. Should the aortic valve be replaced in patients with mild aortic stenosis admitted for coronary surgery? Thorac Cardiovasc Surg. 2008;56:467–470. doi: 10.1055/s-2008-1038840. [DOI] [PubMed] [Google Scholar]
- 71.Pereira JJ, et al. Aortic valve replacement in patients with mild or moderate aortic stenosis and coronary bypass surgery. Am. J. Med. 2005;118:735–742. doi: 10.1016/j.amjmed.2005.01.072. [DOI] [PubMed] [Google Scholar]
- 72.Regeer MV, et al. Mitral valve geometry changes in patients with aortic regurgitation. J. Am. Soc. Echocardiogr. 2015;28:455–462. doi: 10.1016/j.echo.2015.01.009. [DOI] [PubMed] [Google Scholar]
- 73.Toggweiler S, et al. Transcatheter aortic valve replacement: outcomes of patients with moderate or severe mitral regurgitation. J Am Coll Cardiol. 2012;59:2068–2074. doi: 10.1016/j.jacc.2012.02.020. [DOI] [PubMed] [Google Scholar]
- 74.Unger P, Dedobbeleer C, Vanden Eynden F, Lancellotti P. Mitral regurgitation after transcatheter aortic valve replacement: does the prosthesis matter? Int. J. Cardiol. 2013;168:1706–1709. doi: 10.1016/j.ijcard.2013.03.055. [DOI] [PubMed] [Google Scholar]
- 75.Nombela-Franco L, et al. Clinical impact and evolution of mitral regurgitation following transcatheter aortic valve replacement: a meta-analysis. Heart. 2015;101:1395–1405. doi: 10.1136/heartjnl-2014-307120. [DOI] [PubMed] [Google Scholar]
- 76.Maluenda G, et al. Changes in mitral regurgitation after balloon aortic valvuloplasty. Am J Cardiol. 2011;108:1777–1782. doi: 10.1016/j.amjcard.2011.07.061. [DOI] [PubMed] [Google Scholar]
- 77.Nath J, Foster E, Heidenreich PA. Impact of tricuspid regurgitation on long-term survival. J Am Coll Cardiol. 2004;43:405–409. doi: 10.1016/j.jacc.2003.09.036. [DOI] [PubMed] [Google Scholar]
- 78.Braunwald NS, Ross J, Jr., Morrow AG. Conservative management of tricuspid regurgitation in patients undergoing mitral valve replacement. Circulation. 1967;35:I63–I69. doi: 10.1161/01.cir.35.4s1.i-63. [DOI] [PubMed] [Google Scholar]
- 79.Groves PH, Lewis NP, Ikram S, Maire R, Roger JCH. Reduced exercise capacity in patients with tricuspid regurgitation after successful mitral valve replacement for rheumatic mitral valve disease. Br Heart J. 1991;66:295–301. doi: 10.1136/hrt.66.4.295. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 80.King RM, et al. Surgery for tricuspid regurgitation late after mitral valve replacement. Circulation. 1984;70(suppl II):1193–1197. [PubMed] [Google Scholar]
- 81.Dreyfus GD, Corbi PJ, Chan KM, Bahrami T. Secondary tricuspid regurgitation or dilatation: which should be the criteria for surgical repair? Ann. Thorac. Surg. 2005;79:127–132. doi: 10.1016/j.athoracsur.2004.06.057. [DOI] [PubMed] [Google Scholar]
- 82.Gillinov AM, et al. Mitral valve repair with aortic valve replacement is superior to double valve replacement. J. Thorac. Cardiovasc. Surg. 2003;125:1372–1387. doi: 10.1016/s0022-5223(02)73225-x. [DOI] [PubMed] [Google Scholar]
- 83.Talwar S, Mathur A, Choudhary SK, Singh R, Kumar AS. Aortic valve replacement with mitral valve repair compared with combined aortic and mitral valve replacement. Ann. Thorac. Surg. 2007;84:1219–1225. doi: 10.1016/j.athoracsur.2007.04.115. [DOI] [PubMed] [Google Scholar]
- 84.Thourani VH, et al. Does mitral valve repair offer an advantage over replacement in patients undergoing aortic valve replacement? Ann Thorac. Surg. 2014;98:598–603. doi: 10.1016/j.athoracsur.2014.01.031. [DOI] [PubMed] [Google Scholar]
- 85.Leavitt BJ, et al. Outcomes of patients undergoing concomitant aortic and mitral valve surgery in northern new England. Circulation. 2009;120:S155–S162. doi: 10.1161/CIRCULATIONAHA.108.843573. [DOI] [PubMed] [Google Scholar]
- 86.Hamamoto M, et al. Durability and outcome of aortic valve replacement with mitral valve repair versus double valve replacement. Ann. Thorac. Surg. 2003;75:28–33. doi: 10.1016/s0003-4975(02)04405-3. [DOI] [PubMed] [Google Scholar]
- 87.Kuwaki K, et al. Mitral valve repair versus replacement in simultaneous mitral and aortic valve surgery for rheumatic disease. Ann. Thorac. Surg. 2007;83:558–563. doi: 10.1016/j.athoracsur.2006.08.015. [DOI] [PubMed] [Google Scholar]
- 88.Magne J, et al. Mitral repair versus replacement for ischemic mitral regurgitation: comparison of short-term and long-term survival. Circulation. 2009;120:S104–S111. doi: 10.1161/CIRCULATIONAHA.108.843995. [DOI] [PubMed] [Google Scholar]
- 89.Acker MA, et al. Mitral-valve repair versus replacement for severe ischemic mitral regurgitation. N Engl J Med. 2014;370:23–32. doi: 10.1056/NEJMoa1312808. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 90.Arsalan M, Walther T, Smith RL, Grayburn PA. Tricuspid regurgitation diagnosis and treatment. Eur Heart J. 2015 doi: 10.1093/eurheartj/ehv487. [DOI] [PubMed] [Google Scholar]
- 91.Gatti G, et al. Tricuspid annuloplasty for tricuspid regurgitation secondary to left-sided heart valve disease: immediate outcomes and risk factors for late failure. Can. J Cardiol. 2015 doi: 10.1016/j.cjca.2015.09.007. [DOI] [PubMed] [Google Scholar]
- 92.Rudolph V, et al. Bivalvular transcatheter treatment of high-surgical-risk patients with coexisting severe aortic stenosis and significant mitral regurgitation. Int. J. Cardiol. 2013;167:716–720. doi: 10.1016/j.ijcard.2012.03.060. [DOI] [PubMed] [Google Scholar]
- 93.Kische S, et al. Staged total percutaneous treatment of aortic valve pathology and mitral regurgitation: institutional experience. Catheter. Cardiovasc. Interv. 2013;82:E552–E563. doi: 10.1002/ccd.24809. [DOI] [PubMed] [Google Scholar]
- 94.Vahanian A, Himbert d., Brochet E. Multiple valve disease - assessment, strategy and intervention. EuroIntervention. 2015;11(Suppl W):W14–W16. doi: 10.4244/EIJV11SWA3. [DOI] [PubMed] [Google Scholar]
- 95.Himbert D, et al. Transvenous mitral valve replacement after failure of surgical ring annuloplasty. J Am Coll Cardiol. 2012;60:1205–1206. doi: 10.1016/j.jacc.2012.05.033. [DOI] [PubMed] [Google Scholar]
- 96.Himbert d., et al. Transcatheter valve replacement in patients with severe mitral valve disease and annular calcification. J Am Coll Cardiol. 2014;64:2557–2558. doi: 10.1016/j.jacc.2014.09.047. [DOI] [PubMed] [Google Scholar]
- 97.Campelo-Parada F, et al. First-in man experience of a novel transcatheter repair system for treating severe tricuspid regurgitation. J Am Coll Cardiol. 2015;66:2475–2483. doi: 10.1016/j.jacc.2015.09.068. [DOI] [PubMed] [Google Scholar]
- 98.Lancellotti P, et al. ESC working group on valvular heart disease position paper--heart valve clinics: organization, structure, and experiences. Eur Heart J. 2013;34:1597–1606. doi: 10.1093/eurheartj/ehs443. [DOI] [PubMed] [Google Scholar]
- 99.Sanchez-Ledesma M, et al. Impact of concomitant aortic regurgitation on percutaneous mitral valvuloplasty: Immediate results, short-term, and long-term outcome. Am. Heart J. 2008;156:361–366. doi: 10.1016/j.ahj.2008.03.009. [DOI] [PubMed] [Google Scholar]
- 100.Bissessor N, et al. The role of natriuretic peptides in patients with chronic complex (mixed or multiple) heart valve disease. Congest. Heart Fail. 2010;16:50–54. doi: 10.1111/j.1751-7133.2009.00132.x. [DOI] [PubMed] [Google Scholar]
- 101.Bissessor N, et al. Complex valve disease: pre-surgical functional capacity evaluation using peak oxygen consumption. J Heart Valve Dis. 2009;18:554–561. [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.