Abstract
Although the vast majority of patients with a myelodysplastic syndrome (MDS) suffer from cytopenias, the bone marrow is usually normocellular or hypercellular. Apoptosis of hematopoietic cells in the bone marrow has been implicated in this phenomenon. However, in MDS it remains only partially elucidated which genes are involved in this process and which hematopoietic cells are mainly affected. We employed sensitive real-time PCR technology to study 93 apoptosis-related genes and gene families in sorted immature CD34+ and the differentiating erythroid (CD71+) and monomyeloid (CD13/33+) bone marrow cells. Unsupervised cluster analysis of the expression signature readily distinguished the different cellular bone marrow fractions (CD34+, CD71+ and CD13/33+) from each other, but did not discriminate patients from healthy controls. When individual genes were regarded, several were found to be differentially expressed between patients and controls. Particularly, strong over-expression of BIK (BCL2-interacting killer) was observed in erythroid progenitor cells of low- and high-risk MDS patients (both p = 0.001) and TNFRSF4 (tumor necrosis factor receptor superfamily 4) was down-regulated in immature hematopoietic cells (p = 0.0023) of low-risk MDS patients compared to healthy bone marrow.
Introduction
Myelodysplastic syndromes (MDS) represent a heterogeneous group of malignant hematopoietic disorders that are characterized by dysplasia in the myeloid, megakaryocytic and/or erythroid cell lineages. The clinical course of MDS is highly variable. Whereas some patients suffer from smoldering cytopenias, others rapidly develop a more aggressive disease eventually resulting in acute myeloid leukemia (AML). The WHO classification and International Prognostic Scoring systems (IPSS and IPSS-R) recognize the heterogeneity of MDS and divide patients into subgroups based on characteristics such as the amount of blasts in the bone marrow and the number of cytopenias [1–4].
Although cytopenias are present in the peripheral blood of the vast majority of MDS patients, the bone marrow is usually normocellular or hypercellular. Apoptosis of hematopoietic cells in the bone marrow has been implicated in this phenomenon. Several studies have shown signs of increased apoptosis in bone marrow of MDS patients, using techniques such as in situ end labeling (ISEL) of fragmented DNA/ TUNEL assay [5–7], electron microscopy [8, 9], flowcytometry using annexin V staining [10–12] and measurement of mitochondrial membrane potential [11]. The percentage of cells affected by apoptosis differs between studies, possibly due to the use of different techniques and the heterogeneity of the clinical samples studied. In most, but not all studies apoptosis markers are particularly elevated in the more indolent cases of MDS, whereas apoptosis is reduced or at normal levels in the more aggressive cases. This led to the hypothesis that apoptosis is initially increased in MDS due to either primary defects of the apoptotic pathway or in response to oncogenic stress. During the advanced stages of MDS, this response may be lost as a result of further transformation of the malignant cells. The presence of apoptosis has been studied in whole bone marrow and in several bone marrow fractions, such as CD34+ cells. Depending on the study, increased apoptosis parameters were found in the CD34+ cell fraction of all MDS patients [11, 12] or only in patients with the more indolent phenotype [10]. Others described that apoptosis is mainly increased in the more committed myeloid, erythroid and/or megakaryocytic lineages [8, 12, 13].
Apoptosis is a tightly regulated process that involves many proteins. The differential regulation of some of these proteins, such as Fas [12, 14], FLIP [13, 15], BCL-2 and BCL-2-related proteins [10, 16–21], TNF proteins and their receptors [22–25], IAPs [7, 26–28] and caspases [19, 29–32] has been the subject of studies in MDS patients. Most of these studies focused on only one or a few apoptosis-related genes and were performed in either whole bone marrow or the CD34+ cell fraction. Based on the results of these previous studies, we hypothesized that a distinct apoptotic gene expression signature might be present in specific hematopoietic stem and progenitor fractions from healthy individuals compared to MDS patients. To gain insight into the expression patterns of apoptosis-related genes, we have employed sensitive real-time PCR technology to study 93 apoptosis-related genes and gene families in both CD34+ immature hematopoietic cells as well as differentiated erythroid (CD71+) and monomyeloid (CD13/33+) cells.
Results
Isolation of hematopoietic cell fractions
Hematopoietic cell fractions were isolated from the bone marrow of 23 patients and 10 healthy controls (S1 Table). Three different hematopoietic cell fractions were sorted, CD34+ cells (immature hematopoietic cells), CD71+ erythroid precursors and CD13/33+ mono-myeloid precursors. According to the IPSS score 4 low, 11 int-1, 4 int-2 and 4 high risk patients were included. In most cases we were able to isolate all three subfractions from the same patient (S1 Table). As a control, the expression of several genes related to erythroid differentiation (TFRC, GYPA, GYPB, GYPC, SPTB, SPTA1, EBP41, EBP42 and HBB) was measured in all fractions and shown to be highly upregulated in CD71+ cells (data not shown).
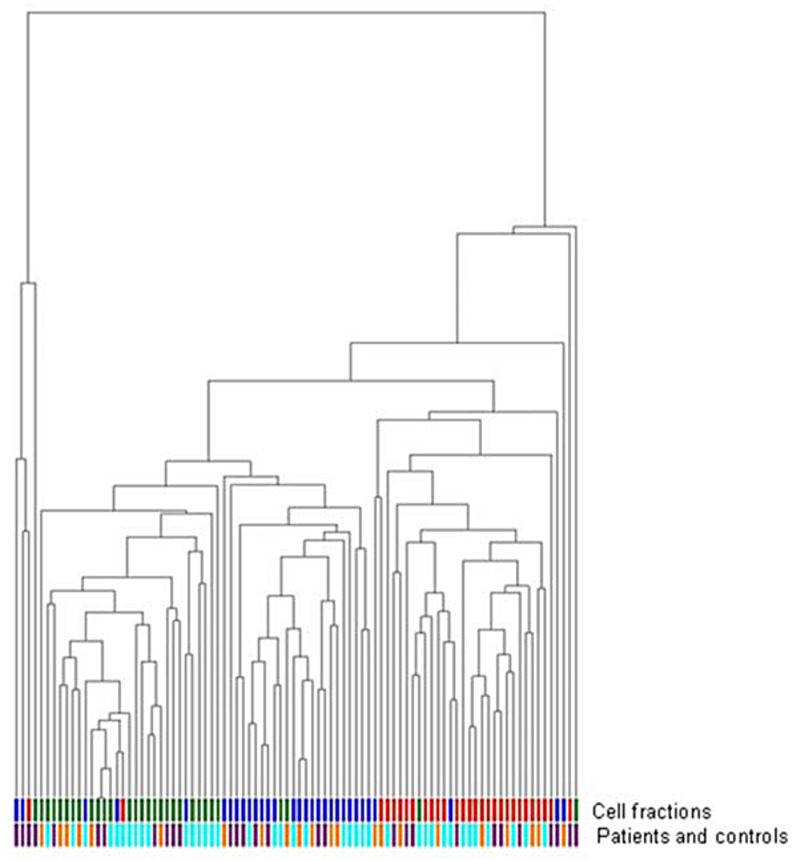
Unsupervised cluster analysis separates different bone marrow fractions but does not differentiate MDS patients and controls
Unsupervised hierarchical cluster analysis was performed based on the expression of 93 apoptosis-related genes. These included members of the TNF (Receptor) Family, BCL-2 Family, IAPs, Caspases, CARD Family, TRAF family and others (S2 Table). The analysis showed a clear clustering of the three hematopoietic cell fractions, indicating different patterns of apoptosis-related gene activity in these cell fractions (Fig 1). Unexpectedly, within each cell fraction, patients and healthy controls could not be distinguished based on the global expression pattern of these apoptosis-related genes (Fig 1). Also low-risk MDS and high-risk MDS patient groups could not be distinguished using this approach.
Fig 1. Unsupervised hierarchical cluster analysis of all samples based on apoptosis-related gene expression profile.
Cell fractions are shown in the first column: CD34+ cells (blue), CD71+ cells (green), CD13/33+ cells (red). The second column shows patients and controls: controls (purple), low risk MDS (light blue), high risk MDS (orange).
Differential expression of apoptosis-related genes in MDS patients and controls
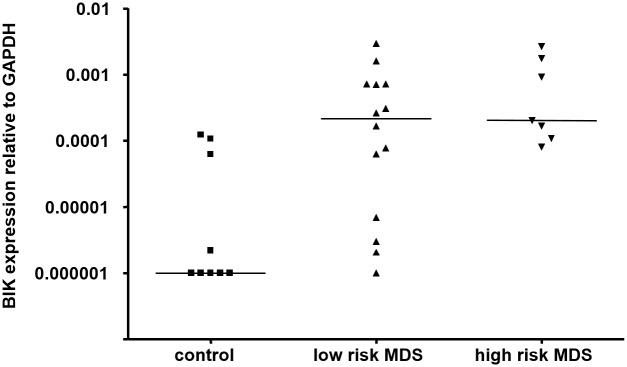
Analysis of individual genes revealed several genes that were differentially expressed between patients and controls in more than one cell fraction: BIK, TNFRSF19 and TNFRSF7 (CD34+ and CD71+ fractions) and MDM2 (CD71+ and CD13/33+ fractions) (Tables 1, 2 and 3, Fig 2). Of these genes, only the pro-apoptotic BIK gene showed a significantly increased expression after correction of p-values for multiple testing. The analyses were repeated after the MDS patients were divided into low-risk and high-risk groups. As was the case for the comparison between all patients and controls, differential expression was detected of TNFRSF4, TNFRSF19, RALBP1 and TNFRSF7 in the CD34+ fraction, BIK, DAPK1, DAPK2, BNIPL, TNFSRF10A, and CARD9 in the CD71+ group and TNFSRF13B, MDM2, DAPK2, TNFRSF10C, and CARD6 in the CD13/33+ fraction. In addition, several other genes mainly showed differences in expression between the low-risk and high-risk MDS patients and not between patients and controls (S3 Table). TNFRSF4 and BIK showed the most prominent differences in expression between the different patient groups and controls. BIK was expressed more than 200-fold higher in CD71+ cells of both low-risk MDS and high-risk MDS compared to healthy controls (p = 0.003). TNFRSF4 displayed a marked down-regulation in CD34+ cells of low-risk MDS patients compared to controls, and a significant increase of expression in high-risk MDS CD71+ cells compared to low-risk MDS CD71+ (p = 0.0023).
Table 1. Differentially expressed genes in the CD34+ cell fraction in MDS patients versus controls.
| Gene | p-value | effect on apoptosis | Ratio of median expression in patients/ controls |
|---|---|---|---|
| TNFRSF19 | 0.006 | pro | 0.2 |
| TNFRSF7 | 0.013 | pro | 0.1 |
| BIK | 0.016 | pro | 0.6 |
| RIPK2 | 0.020 | pro | 1.5 |
| CARD11 | 0.035 | pro | 0.6 |
| RALBP1 | 0.047 | anti | 2.9 |
Table 2. Differentially expressed genes in the CD71+ cell fraction in MDS patients versus controls.
| Gene | p-value | effect on apoptosis | Ratio of median expression in patients/ controls |
|---|---|---|---|
| BIK | 0.001* | pro | 203 |
| BNIPL | 0.004 | pro | 0.1 |
| DAPK1 | 0.020 | pro | 3.6 |
| BBC3 | 0.015 | pro | 3.0 |
| EDA2R | 0.015 | pro | 49 |
| TNFRSF10A | 0.015 | pro | 3.9 |
| CARD9 | 0.018 | pro | 1.6 |
| CASP9 | 0.018 | pro | 7.0 |
| DAPK1 | 0.012 | pro | 3.3 |
| MDM2 | 0.020 | anti | 1.8 |
| TNFSRF19 | 0.020 | pro | 0.2 |
| TNFRSF7 | 0.022 | pro | 0.2 |
| TNFRSF10B | 0.028 | pro | 6.2 |
| BCL2L10 | 0.032 | anti | 2.1 |
| BAG3 | 0.035 | anti | 3.1 |
| TNFRSF10D | 0.044 | anti | 2.9 |
*indicates significant difference (p<0.05) using p-value for multiple testing
Table 3. Differentially expressed genes in the CD13/33+ cell fraction in MDS patients versus controls.
| Gene | p-value | effect on apoptosis | Ratio of median expression in patients/ controls |
|---|---|---|---|
| MDM2 | 0.004 | anti | 1.7 |
| TNFRSF13B | 0.005 | - | 0.01 |
| FADD | 0.035 | pro | 1.7 |
Fig 2. Expression of BIK in MDS patients and controls.
BIK expression in ‘low risk’ patients, ‘high risk’ patients and controls. The expression of BIK is depicted relative to the housekeeping gene GAPDH. Median level of expression is indicated.
Discussion
We have studied the expression of a large set of genes and gene families that have been associated with apoptosis in three different FACS isolated hematopoietic cell fractions from MDS patients and healthy controls. Using sensitive real-time PCR analysis followed by unsupervised clustering analysis of the measured gene expression levels, we were able to distinguish the CD34+, CD71+ and CD13/33+ cell fractions. Unexpectedly, global patterns of gene expression could not distinguish healthy controls and low risk and high risk MDS patients, but consistently clustered the different cellular subsets. Gene expression analysis has been shown to be a powerful tool for patient stratification, discovery of cancer subtypes, and prediction of survival [33–40]. Although our cohort is relatively small, our results suggest that the apoptotic pathway is not grossly deregulated at the transcriptional level in MDS. Analysis of the expression of single genes identified a limited number of genes that were differentially expressed between these groups. Deregulation of the expression of some of these genes has been implicated in MDS before. Increased expression of TNFRSF10A (TRAIL-R1) in MDS has been described, though not specifically in the CD71+ population [23]. Differential expression of other genes, such as TP53 and BCL2, that have previously been implicated in MDS, could not be confirmed in our study. Differences between our study and those of others could be due to the bone marrow fractions studied and the selection of patients. The BIK (BCL-2 interacting killer) gene showed the most prominent increased expression in CD71+ in MDS patients compared to controls. BIK is a pro-apoptotic BH3-only member of the Bcl-2 family [41]. Its binding to Bcl-2 promotes apoptosis [42] and such binding is elicited through several pathways, most notably TP53 [43], E2F1 [44], Smad [45], and miR608 [46]. BIK is normally undetectable or expressed at low levels in cancers [47–50] but specific tumors that were marked with high BIK expression have been targeted for induction of apoptosis leading to tumor reduction [51–54]. BIK has been found to be over-expressed in 14 out of 15 breast cancer samples [47], and was also present in a gene expression signature consisting of 64 genes that correlated with long-term survival in non-small cell lung cancer patients [55]. Although mutations in BIK have been found in B-cell lymphomas [56], little is known about the role of BIK in hematopoietic malignancies. In acute myeloid leukemia, BIK was found to be upregulated in the leukemic cells compared to controls [57]. In addition, it has recently been observed that BIK is involved in autophagy in cancer cells [58, 59]. Although the role of autophagy in myeloid malignancies is still largely unclear [60], autophagy inhibitors are currently being tested in clinical trials [61, 62]. The outstanding over-expression of BIK in MDS CD71+ cells is a novel finding, and since BIK is pro-apoptotic, its overexpression in MDS CD71+ cells might be involved in increased cell death, particularly in the CD71+ erythroid cells in MDS.
The only other gene that maintained significance after correction for multiple testing was TNFRSF4, which we found to be down-regulated in CD34+ cells of low risk MDS patients. TNFRSF4, also known as OX40 or CD134, is mainly known for its role in T-cells. Upon activation it promotes cell survival and clonal expansion [63], and the secretion of pro-inflammatory cytokines, mainly IL-2 [64]. TNFRSF4 has been suggested as a potential target for immunotherapy [65–67] [68]. Little is known of its direct involvement in tumorigenesis or cancer maintenance. It has been shown that the TNFRSF4 gene is hypomethylated in MDS CD34+ cells [69] and a murine study has shown that expression of TNFRSF4 increases upon progression from MDS to AML [70].
In conclusion, we show that unsupervised clustering of the gene expression level of a large set of apoptosis regulating genes does not identify gene signatures that are specific for MDS. Moreover, when single genes were regarded, only a limited number of apoptosis-regulating genes (BIK and TNFRSF4) were differentially expressed between normal and MDS derived cell fractions. This does however not exclude a role for (dysregulated) apoptosis in the pathogenesis of MDS, as we did not measure protein levels.
Methods
Patients and controls
We confirm that the study has been reviewed and approved by the Commissie Mensgebonden Onderzoek (CMO), the institutional review board (IRB) at the Radboudumc (NL), with the IRB file number CMO 2013/64 before the beginning of the study. For further details, contact the CMO at commissiemensgebondenonderzoek@radboudumc.nl or at the phone number 0031-24-3613154. Bone marrow from MDS patients (n = 23) and healthy controls (n = 10) was collected after informed consent. Written informed consent for the use of surplus diagnostic patient material was obtained in compliance with institutional regulations. Patients diagnosed at the Radboudumc belonging to all different WHO and IPSS categories were included. Patient characteristics are shown in S1 Table. Patient 11 had an exceedingly high granulocyte count. Nonetheless, the diagnosis of MDS RAEB1 was confirmed for this patient. All patient samples were collected before treatment was administered. Mononuclear cells were isolated from the bone marrow by density gradient centrifugation using Ficoll 1.077 g/mL (Pharmacia Biotech, Uppsala, Sweden) and viably frozen in liquid nitrogen until further use.
Cell sorting and RNA isolation
After thawing, hematopoietic cell subtypes were isolated by fluorescence activated cell sorting (FACS) using monoclonal antibodies directed against CD45 and the side scatter profile. In addition, monoclonal antibodies directed against CD34, CD13, CD33 and CD71 were used. Gating on forward and side scatter was used to exclude dead cells and debris. RNA was isolated from three subfractions, the CD34+ stem/progenitor cells, the CD13/33+ mono/myeloid cells and the CD71+ erythroid cells.
Gene expression analysis
In a first set of patients and controls, the expression of 180 different apoptosis-related genes was measured simultaneously by real-time PCR employing a 384 Microfluidic Card (Applied Biosystems). The genes measured and the corresponding assay numbers are shown in S2 Table. cDNA obtained from the CD34+ (patients n = 13, controls n = 5), CD71+ (patients n = 12, controls n = 4) and CD13/33+ (patients n = 11, controls n = 5) cell fractions was analyzed. Based on the expression pattern of these genes, a selection of 93 genes was used to perform a similar expression analysis in an additional group of CD34+ (patients n = 8, controls n = 5), CD71+ (patients n = 9, controls n = 5) and CD13/33+ cells (patients n = 8, controls n = 5). The relative expression of the apoptosis-related genes was calculated by measuring the housekeeping gene GAPDH. Relative expression values less than 1x10-6 were set to 1x10-6 to avoid bias introduced by including values reaching the limit of detection of the real-time PCR assay. In addition to the apoptosis-related genes, the expression of several genes implicated in erythroid differentiation (TFRC, GYPA, GYPB, GYPC, SPTB, SPTA1, EBP41, EBP42 and HBB) was determined to check whether these genes indeed showed highest expression in the CD71+ cell fraction. The erythroid genes were only used as controls and not included in subsequent statistical analyses. Complete data are retrievable on Gene Expression Omnibus with the accession number GSE89579.
Statistical analysis
Microfluidic card log-scale values were imported into Partek (Partek Genomic Suite software, version 6.5; Partek Inc., St. Louis, MO). Principle Component Analysis (PCA) showed a clear distinction between the three different tissues and thus the dataset was split accordingly into three separate groups. In each group expression differences between donors and patients was calculated using the non-parametric Mann-Whitney U-test. For statistical analysis, patients from the IPSS low and int-1 risk groups were combined in a ‘low risk MDS’ group and patients from the IPSS int-2 and high-risk groups in a ‘high-risk MDS’ group. Corresponding P-values were corrected for multiple testing by random permutations. The Kruskall-Wallis-test was used to identify differences between the ‘low risk MDS’, ‘high-risk MDS’ and control groups. In case of a p-value< 0.05, posthoc analysis was performed using non-parametric Mann-Whitney U test.
Supporting Information
Patient characteristics: n/a = not available; * Normal Hemoglobin (Hb) range in adults = 2.0–2.7 mmol/L in males, 1.8–2.5 mmol/L in females; ** Normal granulocyte absolute count range in adults = 1.3–8.0 x10^9. Depending on material availability and quantity, it was possible to sort CD34+, CD71+, and CD13/33+ cell fractions from each patient.
(DOCX)
Complete list of 384 apoptosis-related genes with Gene symbols, RefSeq record, assay number, and assay replicate
(DOCX)
Genes with notable expression differences of patients versus low-risk MDS versus high-risk MDS in A) in the CD34+, B) in the CD71+, and C) in the CD13/33+ cell fraction. * indicates significant difference (p<0.05) in expression after posthoc analysis. ** indicates significant difference (p<0.05) using p-value for multiple testing.
(DOCX)
Data Availability
Complete data are retrievable on Gene Expression Omnibus with the accession number GSE89579.
Funding Statement
This work was supported by grants from the "Dutch Organization for Scientific Research" (NWO, 92003420) to SMCL and the "Dutch Cancer Society" (KWF) to NM. The funders had no role in study design, data collection and analysis, decision to publish, or preparation of the manuscript.
References
- 1.Germing U, Kobbe G, Haas R, Gattermann N. Myelodysplastic syndromes: diagnosis, prognosis, and treatment. Deutsches Arzteblatt international. 2013;110(46):783–90. 10.3238/arztebl.2013.0783 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Greenberg P, Cox C, LeBeau MM, Fenaux P, Morel P, Sanz G, et al. International scoring system for evaluating prognosis in myelodysplastic syndromes. Blood. 1997;89(6):2079–88. [PubMed] [Google Scholar]
- 3.Greenberg PL, Tuechler H, Schanz J, Sanz G, Garcia-Manero G, Sole F, et al. Revised international prognostic scoring system for myelodysplastic syndromes. Blood. 2012;120(12):2454–65. 10.1182/blood-2012-03-420489 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Tefferi A, Skoda R, Vardiman JW. Myeloproliferative neoplasms: contemporary diagnosis using histology and genetics. Nature reviews Clinical oncology. 2009;6(11):627–37. 10.1038/nrclinonc.2009.149 [DOI] [PubMed] [Google Scholar]
- 5.Tsoplou P, Kouraklis-Symeonidis A, Thanopoulou E, Zikos P, Orphanos V, Zoumbos NC. Apoptosis in patients with myelodysplastic syndromes: differential involvement of marrow cells in 'good' versus 'poor' prognosis patients and correlation with apoptosis-related genes. Leukemia. 1999;13(10):1554–63. [DOI] [PubMed] [Google Scholar]
- 6.Pecci A, Travaglino E, Klersy C, Invernizzi R. Apoptosis in relation to CD34 antigen expression in normal and myelodysplastic bone marrow. Acta haematologica. 2003;109(1):29–34. [DOI] [PubMed] [Google Scholar]
- 7.Invernizzi R, Travaglino E, Lunghi M, Klersy C, Bernasconi P, Cazzola M, et al. Survivin expression in acute leukemias and myelodysplastic syndromes. Leukemia & lymphoma. 2004;45(11):2229–37. [DOI] [PubMed] [Google Scholar]
- 8.Bogdanovic AD, Trpinac DP, Jankovic GM, Bumbasirevic VZ, Obradovic M, Colovic MD. Incidence and role of apoptosis in myelodysplastic syndrome: morphological and ultrastructural assessment. Leukemia. 1997;11(5):656–9. [DOI] [PubMed] [Google Scholar]
- 9.Shetty V, Hussaini S, Alvi S, Joshi L, Shaher A, Dangerfield B, et al. Excessive apoptosis, increased phagocytosis, nuclear inclusion bodies and cylindrical confronting cisternae in bone marrow biopsies of myelodysplastic syndrome patients. British journal of haematology. 2002;116(4):817–25. [DOI] [PubMed] [Google Scholar]
- 10.Parker JE, Mufti GJ, Rasool F, Mijovic A, Devereux S, Pagliuca A. The role of apoptosis, proliferation, and the Bcl-2-related proteins in the myelodysplastic syndromes and acute myeloid leukemia secondary to MDS. Blood. 2000;96(12):3932–8. [PubMed] [Google Scholar]
- 11.Huh YO, Jilani I, Estey E, Giles F, Kantarjian H, Freireich E, et al. More cell death in refractory anemia with excess blasts in transformation than in acute myeloid leukemia. Leukemia. 2002;16(11):2249–52. 10.1038/sj.leu.2402704 [DOI] [PubMed] [Google Scholar]
- 12.Pang WW, Pluvinage JV, Price EA, Sridhar K, Arber DA, Greenberg PL, et al. Hematopoietic stem cell and progenitor cell mechanisms in myelodysplastic syndromes. Proceedings of the National Academy of Sciences of the United States of America. 2013;110(8):3011–6. 10.1073/pnas.1222861110 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Raza A, Mundle S, Iftikhar A, Gregory S, Marcus B, Khan Z, et al. Simultaneous assessment of cell kinetics and programmed cell death in bone marrow biopsies of myelodysplastics reveals extensive apoptosis as the probable basis for ineffective hematopoiesis. American journal of hematology. 1995;48(3):143–54. [DOI] [PubMed] [Google Scholar]
- 14.Lin CW, Manshouri T, Jilani I, Neuberg D, Patel K, Kantarjian H, et al. Proliferation and apoptosis in acute and chronic leukemias and myelodysplastic syndrome. Leukemia research. 2002;26(6):551–9. [DOI] [PubMed] [Google Scholar]
- 15.Bouscary D, De Vos J, Guesnu M, Jondeau K, Viguier F, Melle J, et al. Fas/Apo-1 (CD95) expression and apoptosis in patients with myelodysplastic syndromes. Leukemia. 1997;11(6):839–45. [DOI] [PubMed] [Google Scholar]
- 16.Rajapaksa R, Ginzton N, Rott LS, Greenberg PL. Altered oncoprotein expression and apoptosis in myelodysplastic syndrome marrow cells. Blood. 1996;88(11):4275–87. [PubMed] [Google Scholar]
- 17.Parker JE, Fishlock KL, Mijovic A, Czepulkowski B, Pagliuca A, Mufti GJ. 'Low-risk' myelodysplastic syndrome is associated with excessive apoptosis and an increased ratio of pro- versus anti-apoptotic bcl-2-related proteins. British journal of haematology. 1998;103(4):1075–82. [DOI] [PubMed] [Google Scholar]
- 18.Suarez L, Vidriales MB, Sanz G, Lopez A, Lopez-Berges MC, de Santiago M, et al. Expression of APO2.7, bcl-2 and bax apoptosis-associated proteins in CD34- bone marrow cell compartments from patients with myelodysplastic syndromes. Leukemia. 2004;18(7):1311–3. 10.1038/sj.leu.2403386 [DOI] [PubMed] [Google Scholar]
- 19.Economopoulou C, Pappa V, Kontsioti F, Papageorgiou S, Kapsimali V, Papasteriadi C, et al. Analysis of apoptosis regulatory genes expression in the bone marrow (BM) of adult de novo myelodysplastic syndromes (MDS). Leukemia research. 2008;32(1):61–9. 10.1016/j.leukres.2007.04.012 [DOI] [PubMed] [Google Scholar]
- 20.Bogenberger JM, Kornblau SM, Pierceall WE, Lena R, Chow D, Shi CX, et al. BCL-2 family proteins as 5-Azacytidine-sensitizing targets and determinants of response in myeloid malignancies. Leukemia. 2014;28(8):1657–65. 10.1038/leu.2014.44 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Jilg S, Reidel V, Muller-Thomas C, Konig J, Schauwecker J, Hockendorf U, et al. Blockade of BCL-2 proteins efficiently induces apoptosis in progenitor cells of high-risk myelodysplastic syndromes patients. Leukemia. 2016;30(1):112–23. 10.1038/leu.2015.179 [DOI] [PubMed] [Google Scholar]
- 22.Kitagawa M, Saito I, Kuwata T, Yoshida S, Yamaguchi S, Takahashi M, et al. Overexpression of tumor necrosis factor (TNF)-alpha and interferon (IFN)-gamma by bone marrow cells from patients with myelodysplastic syndromes. Leukemia. 1997;11(12):2049–54. [DOI] [PubMed] [Google Scholar]
- 23.Zang DY, Goodwin RG, Loken MR, Bryant E, Deeg HJ. Expression of tumor necrosis factor-related apoptosis-inducing ligand, Apo2L, and its receptors in myelodysplastic syndrome: effects on in vitro hemopoiesis. Blood. 2001;98(10):3058–65. [DOI] [PubMed] [Google Scholar]
- 24.Sawanobori M, Yamaguchi S, Hasegawa M, Inoue M, Suzuki K, Kamiyama R, et al. Expression of TNF receptors and related signaling molecules in the bone marrow from patients with myelodysplastic syndromes. Leukemia research. 2003;27(7):583–91. [DOI] [PubMed] [Google Scholar]
- 25.Tsimberidou AM, Estey E, Wen S, Pierce S, Kantarjian H, Albitar M, et al. The prognostic significance of cytokine levels in newly diagnosed acute myeloid leukemia and high-risk myelodysplastic syndromes. Cancer. 2008;113(7):1605–13. 10.1002/cncr.23785 [DOI] [PubMed] [Google Scholar]
- 26.Gianelli U, Fracchiolla NS, Cortelezzi A, Pellegrini C, Savi F, Moro A, et al. Survivin expression in "low-risk" and "high-risk" myelodysplastic syndromes. Annals of hematology. 2007;86(3):185–9. 10.1007/s00277-006-0215-0 [DOI] [PubMed] [Google Scholar]
- 27.Yamamoto K, Abe S, Nakagawa Y, Suzuki K, Hasegawa M, Inoue M, et al. Expression of IAP family proteins in myelodysplastic syndromes transforming to overt leukemia. Leukemia research. 2004;28(11):1203–11. 10.1016/j.leukres.2004.03.020 [DOI] [PubMed] [Google Scholar]
- 28.Yoshida A, Zokumasu K, Wano Y, Yamauchi T, Imamura S, Takagi K, et al. Marked upregulation of Survivin and Aurora-B kinase is associated with disease progression in the myelodysplastic syndromes. Haematologica. 2012;97(9):1372–9. 10.3324/haematol.2011.055681 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Boudard D, Sordet O, Vasselon C, Revol V, Bertheas MF, Freyssenet D, et al. Expression and activity of caspases 1 and 3 in myelodysplastic syndromes. Leukemia. 2000;14(12):2045–51. [DOI] [PubMed] [Google Scholar]
- 30.Hellstrom-Lindberg E, Schmidt-Mende J, Forsblom AM, Christensson B, Fadeel B, Zhivotovsky B. Apoptosis in refractory anaemia with ringed sideroblasts is initiated at the stem cell level and associated with increased activation of caspases. British journal of haematology. 2001;112(3):714–26. [DOI] [PubMed] [Google Scholar]
- 31.Bouscary D, Chen YL, Guesnu M, Picard F, Viguier F, Lacombe C, et al. Activity of the caspase-3/CPP32 enzyme is increased in "early stage" myelodysplastic syndromes with excessive apoptosis, but caspase inhibition does not enhance colony formation in vitro. Experimental hematology. 2000;28(7):784–91. [DOI] [PubMed] [Google Scholar]
- 32.Claessens YE, Park S, Dubart-Kupperschmitt A, Mariot V, Garrido C, Chretien S, et al. Rescue of early-stage myelodysplastic syndrome-deriving erythroid precursors by the ectopic expression of a dominant-negative form of FADD. Blood. 2005;105(10):4035–42. 10.1182/blood-2004-08-3166 [DOI] [PubMed] [Google Scholar]
- 33.Golub TR, Slonim DK, Tamayo P, Huard C, Gaasenbeek M, Mesirov JP, et al. Molecular classification of cancer: class discovery and class prediction by gene expression monitoring. Science. 1999;286(5439):531–7. [DOI] [PubMed] [Google Scholar]
- 34.Kohlmann A, Bullinger L, Thiede C, Schaich M, Schnittger S, Dohner K, et al. Gene expression profiling in AML with normal karyotype can predict mutations for molecular markers and allows novel insights into perturbed biological pathways. Leukemia. 2010;24(6):1216–20. 10.1038/leu.2010.73 [DOI] [PubMed] [Google Scholar]
- 35.Valk PJ, Verhaak RG, Beijen MA, Erpelinck CA, Barjesteh van Waalwijk van Doorn-Khosrovani S, Boer JM, et al. Prognostically useful gene-expression profiles in acute myeloid leukemia. The New England journal of medicine. 2004;350(16):1617–28. 10.1056/NEJMoa040465 [DOI] [PubMed] [Google Scholar]
- 36.Bullinger L, Dohner K, Bair E, Frohling S, Schlenk RF, Tibshirani R, et al. Use of gene-expression profiling to identify prognostic subclasses in adult acute myeloid leukemia. The New England journal of medicine. 2004;350(16):1605–16. 10.1056/NEJMoa031046 [DOI] [PubMed] [Google Scholar]
- 37.Raponi M, Lancet JE, Fan H, Dossey L, Lee G, Gojo I, et al. A 2-gene classifier for predicting response to the farnesyltransferase inhibitor tipifarnib in acute myeloid leukemia. Blood. 2008;111(5):2589–96. 10.1182/blood-2007-09-112730 [DOI] [PubMed] [Google Scholar]
- 38.Ebert BL, Galili N, Tamayo P, Bosco J, Mak R, Pretz J, et al. An erythroid differentiation signature predicts response to lenalidomide in myelodysplastic syndrome. PLoS medicine. 2008;5(2):e35 10.1371/journal.pmed.0050035 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Theilgaard-Monch K, Boultwood J, Ferrari S, Giannopoulos K, Hernandez-Rivas JM, Kohlmann A, et al. Gene expression profiling in MDS and AML: potential and future avenues. Leukemia. 2011;25(6):909–20. 10.1038/leu.2011.48 [DOI] [PubMed] [Google Scholar]
- 40.Sorlie T, Perou CM, Tibshirani R, Aas T, Geisler S, Johnsen H, et al. Gene expression patterns of breast carcinomas distinguish tumor subclasses with clinical implications. Proceedings of the National Academy of Sciences of the United States of America. 2001;98(19):10869–74. 10.1073/pnas.191367098 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Boyd JM, Gallo GJ, Elangovan B, Houghton AB, Malstrom S, Avery BJ, et al. Bik, a novel death-inducing protein shares a distinct sequence motif with Bcl-2 family proteins and interacts with viral and cellular survival-promoting proteins. Oncogene. 1995;11(9):1921–8. [PubMed] [Google Scholar]
- 42.Elangovan B, Chinnadurai G. Functional dissection of the pro-apoptotic protein Bik. Heterodimerization with anti-apoptosis proteins is insufficient for induction of cell death. The Journal of biological chemistry. 1997;272(39):24494–8. [DOI] [PubMed] [Google Scholar]
- 43.Hur J, Bell DW, Dean KL, Coser KR, Hilario PC, Okimoto RA, et al. Regulation of expression of BIK proapoptotic protein in human breast cancer cells: p53-dependent induction of BIK mRNA by fulvestrant and proteasomal degradation of BIK protein. Cancer research. 2006;66(20):10153–61. 10.1158/0008-5472.CAN-05-3696 [DOI] [PubMed] [Google Scholar]
- 44.Real PJ, Sanz C, Gutierrez O, Pipaon C, Zubiaga AM, Fernandez-Luna JL. Transcriptional activation of the proapoptotic bik gene by E2F proteins in cancer cells. FEBS letters. 2006;580(25):5905–9. 10.1016/j.febslet.2006.08.088 [DOI] [PubMed] [Google Scholar]
- 45.Spender LC, O'Brien DI, Simpson D, Dutt D, Gregory CD, Allday MJ, et al. TGF-beta induces apoptosis in human B cells by transcriptional regulation of BIK and BCL-XL. Cell death and differentiation. 2009;16(4):593–602. 10.1038/cdd.2008.183 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Choi YC, Yoon S, Byun Y, Lee G, Kee H, Jeong Y, et al. MicroRNA library screening identifies growth-suppressive microRNAs that regulate genes involved in cell cycle progression and apoptosis. Experimental cell research. 2015;339(2):320–32. 10.1016/j.yexcr.2015.10.012 [DOI] [PubMed] [Google Scholar]
- 47.Garcia N, Salamanca F, Astudillo-de la Vega H, Curiel-Quesada E, Alvarado I, Penaloza R, et al. A molecular analysis by gene expression profiling reveals Bik/NBK overexpression in sporadic breast tumor samples of Mexican females. BMC cancer. 2005;5:93 10.1186/1471-2407-5-93 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48.Lan KL, Yen SH, Liu RS, Shih HL, Tseng FW, Lan KH. Mutant Bik gene transferred by cationic liposome inhibits peritoneal disseminated murine colon cancer. Clinical & experimental metastasis. 2007;24(6):461–70. [DOI] [PubMed] [Google Scholar]
- 49.Valdez BC, Murray D, Ramdas L, de Lima M, Jones R, Kornblau S, et al. Altered gene expression in busulfan-resistant human myeloid leukemia. Leukemia research. 2008;32(11):1684–97. 10.1016/j.leukres.2008.01.016 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50.Ferreira AF, de Oliveira GL, Tognon R, Collassanti MD, Zanichelli MA, Hamerschlak N, et al. Apoptosis-related gene expression profile in chronic myeloid leukemia patients after imatinib mesylate and dasatinib therapy. Acta haematologica. 2015;133(4):354–64. 10.1159/000369446 [DOI] [PubMed] [Google Scholar]
- 51.Zou Y, Peng H, Zhou B, Wen Y, Wang SC, Tsai EM, et al. Systemic tumor suppression by the proapoptotic gene bik. Cancer research. 2002;62(1):8–12. [PubMed] [Google Scholar]
- 52.Viedma-Rodriguez R, Baiza-Gutman LA, Garcia-Carranca A, Moreno-Fierros L, Salamanca-Gomez F, Arenas-Aranda D. Suppression of the death gene BIK is a critical factor for resistance to tamoxifen in MCF-7 breast cancer cells. International journal of oncology. 2013;43(6):1777–86. 10.3892/ijo.2013.2127 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 53.Viedma-Rodriguez R, Ruiz Esparza-Garrido R, Baiza-Gutman LA, Velazquez-Flores MA, Garcia-Carranca A, Salamanca-Gomez F, et al. Involvement of multiple cellular pathways in regulating resistance to tamoxifen in BIK-suppressed MCF-7 cells. Tumour biology: the journal of the International Society for Oncodevelopmental Biology and Medicine. 2015;36(9):6991–7005. [DOI] [PubMed] [Google Scholar]
- 54.Xi Y, Gao H, Callaghan MU, Fribley AM, Garshott DM, Xu ZX, et al. Induction of BCL2-Interacting Killer, BIK, is Mediated for Anti-Cancer Activity of Curcumin in Human Head and Neck Squamous Cell Carcinoma Cells. Journal of Cancer. 2015;6(4):327–32. 10.7150/jca.11185 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 55.Lu Y, Lemon W, Liu PY, Yi Y, Morrison C, Yang P, et al. A gene expression signature predicts survival of patients with stage I non-small cell lung cancer. PLoS medicine. 2006;3(12):e467 10.1371/journal.pmed.0030467 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 56.Arena V, Martini M, Luongo M, Capelli A, Larocca LM. Mutations of the BIK gene in human peripheral B-cell lymphomas. Genes, chromosomes & cancer. 2003;38(1):91–6. [DOI] [PubMed] [Google Scholar]
- 57.Stirewalt DL, Meshinchi S, Kopecky KJ, Fan W, Pogosova-Agadjanyan EL, Engel JH, et al. Identification of genes with abnormal expression changes in acute myeloid leukemia. Genes, chromosomes & cancer. 2008;47(1):8–20. [DOI] [PubMed] [Google Scholar]
- 58.Rashmi R, Pillai SG, Vijayalingam S, Ryerse J, Chinnadurai G. BH3-only protein BIK induces caspase-independent cell death with autophagic features in Bcl-2 null cells. Oncogene. 2008;27(10):1366–75. 10.1038/sj.onc.1210783 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 59.Ruiz Esparza-Garrido R, Torres-Marquez ME, Viedma-Rodriguez R, Velazquez-Wong AC, Salamanca-Gomez F, Rosas-Vargas H, et al. Breast cancer cell line MDA-MB-231 miRNA profile expression after BIK interference: BIK involvement in autophagy. Tumour biology: the journal of the International Society for Oncodevelopmental Biology and Medicine. 2016;37(5):6749–59. [DOI] [PubMed] [Google Scholar]
- 60.Evangelisti C, Evangelisti C, Chiarini F, Lonetti A, Buontempo F, Neri LM, et al. Autophagy in acute leukemias: a double-edged sword with important therapeutic implications. Biochimica et biophysica acta. 2015;1853(1):14–26. 10.1016/j.bbamcr.2014.09.023 [DOI] [PubMed] [Google Scholar]
- 61.Poklepovic A, Gewirtz DA. Outcome of early clinical trials of the combination of hydroxychloroquine with chemotherapy in cancer. Autophagy. 2014;10(8):1478–80. 10.4161/auto.29428 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 62.Vogl DT, Stadtmauer EA, Tan KS, Heitjan DF, Davis LE, Pontiggia L, et al. Combined autophagy and proteasome inhibition: a phase 1 trial of hydroxychloroquine and bortezomib in patients with relapsed/refractory myeloma. Autophagy. 2014;10(8):1380–90. 10.4161/auto.29264 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 63.Song J, So T, Croft M. Activation of NF-kappaB1 by OX40 contributes to antigen-driven T cell expansion and survival. Journal of immunology. 2008;180(11):7240–8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 64.Gramaglia I, Weinberg AD, Lemon M, Croft M. Ox-40 ligand: a potent costimulatory molecule for sustaining primary CD4 T cell responses. Journal of immunology. 1998;161(12):6510–7. [PubMed] [Google Scholar]
- 65.Lane PJ, McConnell FM, Anderson G, Nawaf MG, Gaspal FM, Withers DR. Evolving strategies for cancer and autoimmunity: back to the future. Frontiers in immunology. 2014;5:154 10.3389/fimmu.2014.00154 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 66.Jensen SM, Maston LD, Gough MJ, Ruby CE, Redmond WL, Crittenden M, et al. Signaling through OX40 enhances antitumor immunity. Seminars in oncology. 2010;37(5):524–32. 10.1053/j.seminoncol.2010.09.013 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 67.Moran AE, Kovacsovics-Bankowski M, Weinberg AD. The TNFRs OX40, 4-1BB, and CD40 as targets for cancer immunotherapy. Current opinion in immunology. 2013;25(2):230–7. 10.1016/j.coi.2013.01.004 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 68.Webb GJ, Hirschfield GM, Lane PJ. OX40, OX40L and Autoimmunity: a Comprehensive Review. Clinical reviews in allergy & immunology. 2016;50(3):312–32. [DOI] [PubMed] [Google Scholar]
- 69.Will B, Zhou L, Vogler TO, Ben-Neriah S, Schinke C, Tamari R, et al. Stem and progenitor cells in myelodysplastic syndromes show aberrant stage-specific expansion and harbor genetic and epigenetic alterations. Blood. 2012;120(10):2076–86. 10.1182/blood-2011-12-399683 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 70.Guerenne L, Beurlet S, Said M, Gorombei P, Le Pogam C, Guidez F, et al. GEP analysis validates high risk MDS and acute myeloid leukemia post MDS mice models and highlights novel dysregulated pathways. Journal of hematology & oncology. 2016;9:5. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Patient characteristics: n/a = not available; * Normal Hemoglobin (Hb) range in adults = 2.0–2.7 mmol/L in males, 1.8–2.5 mmol/L in females; ** Normal granulocyte absolute count range in adults = 1.3–8.0 x10^9. Depending on material availability and quantity, it was possible to sort CD34+, CD71+, and CD13/33+ cell fractions from each patient.
(DOCX)
Complete list of 384 apoptosis-related genes with Gene symbols, RefSeq record, assay number, and assay replicate
(DOCX)
Genes with notable expression differences of patients versus low-risk MDS versus high-risk MDS in A) in the CD34+, B) in the CD71+, and C) in the CD13/33+ cell fraction. * indicates significant difference (p<0.05) in expression after posthoc analysis. ** indicates significant difference (p<0.05) using p-value for multiple testing.
(DOCX)
Data Availability Statement
Complete data are retrievable on Gene Expression Omnibus with the accession number GSE89579.