Abstract
Purpose
Physical and psychological symptoms experienced by patients with advanced cancer influence their wellbeing; how patient and family caregivers' symptom distress influence each other's wellbeing is less understood. This study examined the influence of patient and caregiver symptom distress on their threat appraisals and self-efficacy to cope with cancer.
Methods
We conducted secondary analysis of baseline data from an RCT that enrolled patients with advanced cancer and their family caregivers (N=484 dyads). Structural equation modeling and the actor-partner interdependence mediation model (APIMeM) were used to examine two models: threat appraisals as a mediator of the relationship between symptom distress and individual and family-related self-efficacy; and, self-efficacy (individual and family dimensions) as mediators of the relationship between symptom distress and threat appraisals.
Results
Data suggest the self-efficacy mediation model was the preferred model. More patient and caregiver symptom distress was directly associated with their own lower self-efficacy and more threatening appraisals. Patient and caregiver individual self-efficacy also mediated the relationship between their own symptom distress and threat appraisals. There were also significant interdependent effects. More patient symptom distress was associated with less caregiver family-related self-efficacy; and, more caregiver symptom distress was directly associated with more threatening patient appraisals.
Conclusions
Patient and caregiver symptom distress influenced their own, and in some cases each other's, cognitive appraisals. Limitations of this study include the use of cross-sectional data and assessments of individually-focused (vs. family-focused) threat appraisals. These findings highlight the need to consider the management of patient and caregiver symptoms during advanced cancer.
Keywords: symptoms, caregiving, advanced cancer, dyad, cognitive appraisal, self-efficacy
A diagnosis of advanced cancer is a challenging life event for patients and their family caregivers. At advanced stages of disease, the goals of treatment are no longer curative [1] and patients and caregivers must navigate the complexities of a life-threatening disease. Stress and coping theory [2] suggests that patient and caregiver cognitive appraisals about the cancer experience are key contributors to their wellbeing. In this theoretical framework, primary appraisals are evaluations of the significance of the advanced cancer [3], such as the ways in which the cancer diagnosis threatens their lives and livelihood. Secondary appraisals are assessments of their ability to manage the consequences of the illness; that is, their self-efficacy to cope with the cancer or caregiving situation [4]. Patient and caregiver cancer-related appraisals have been associated with their use of coping strategies [5], life satisfaction [6], and, quality of life [7]. Nonetheless, a number of critical knowledge gaps remain. A potentially important but understudied area is how the experience of physical and psychological symptoms, by patients and caregivers alike, influence their cancer-related appraisals.
Patients with advanced cancer are often dealing simultaneously with side effects from cancer treatment and symptoms from the disease itself [8]. Commonly experienced symptoms include nausea, pain, and fatigue, all of which can have detrimental influences on wellbeing [9,10]. As a result, symptom control is a frequent desire of patients [11] and their caregivers who often help with symptom management [12,13]. Unmanaged symptoms may impair patients' functional and psychologial wellbeing and complicate the day-to-day support needed from family caregivers.
Caregivers' own symptom experience warrants attention because their physical and mental health has implications for their own wellbeing [14] and their ability to provide care [15,16]. As the prevalence of chronic diseases such as diabetes, heart disease, and arthritis increases with age [17], cancer caregivers, who tend to be older [18], are likely to also be managing symptoms related to their own health conditions. Unfortunately, the demands of caring for a loved one with advanced cancer may impede caregivers' ability to attend to their own symptom management [19,20].
Taken together, patients' and caregivers' experience of symptoms may make advanced cancer more daunting and threatening (i.e. primary appraisal). In addition, these symptoms may negatively influence their self-efficacy to deal with the challenges of advanced cancer and caregiving (secondary appraisals). As part of a family, patients and caregivers often have concerns about how other members of the family are handling the illness [21,22]. Thus, it is useful to consider two related but distinct dimensions of self-efficacy to capture the range of secondary appraisals made by patients and caregivers: patients' and caregivers' own self-efficacy to cope with cancer/caregiving (individual self-efficacy) and self-efficacy to help other family members manage cancer-related issues (family-related self-efficacy).
Purpose & Aims
This study examines the influence of patient and caregiver symptom distress, as a significant stressor in their cancer experience, on their threat appraisals and their self-efficacy to cope with cancer (among patients) and the demands of cancer caregiving (among caregivers). Despite the ordinal naming of the concepts, stress and coping theory does not propose that a stressor (i.e., symptom distress) influences appraisal processes in a temporal fashion [2]. Previous research found that as patient and caregiver self-efficacy (i.e. secondary appraisal) for coping with cancer/caregiving increased, their negative illness-related appraisals (i.e. primary appraisal) decreased [7]. It is possible that the reverse relationship also exists. That is, patient and caregiver threat appraisals could influence their self-efficacy to cope with disease. Research suggests that in situations where the stressor is likely to be threatening and a source of significant strain, such as with advanced cancer, threat appraisals may have a significant influence on an individual's self-efficacy about their ability to cope with the illness and its consequences [23]. Moreover, how symptom distress might influence this relationship between self-efficacy and threat appraisals among patient-caregiver dyads in advanced cancer has not been explored.
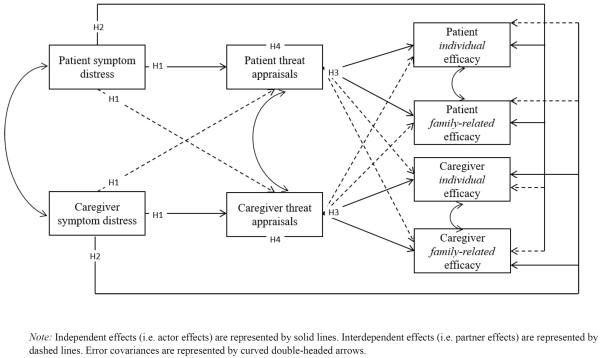
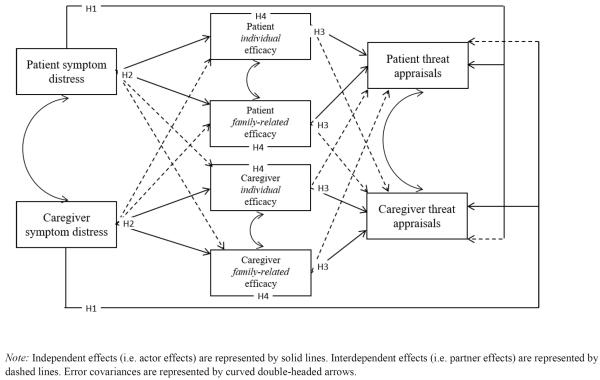
Thus, in this study, two competing models will be tested: a threat mediated model, which examines threat appraisal as a mediator of the relationship between symptom distress and self-efficacy (Figure 1); and, an efficacy mediated model, which examines self-efficacy as a mediator of the relationship between symptom distress and threat appraisal (Figure 2). The interdependent nature of the patient-caregiver relationship during the advanced cancer stage suggests that patient and caregiver symptom distress and cognitive appraisals may be interrelated [24,25]. As a result, this study explores independent effects (i.e., how an individual's symptom distress influences their own appraisals) and interdependent effects (i.e., how an individual's symptom distress influences the other person's appraisals). Our hypotheses are as follows:
-
H1:
Symptom distress reported by patients and caregivers will be positively associated with their own threat appraisals and the threat appraisals of the other member of the dyad.
-
H2:
Symptom distress reported by patients and caregivers will be negatively associated with their own self-efficacy (individual and family-related) and the self-efficacy of the other member of the dyad.
-
H3:
a) In the threat mediated model, threat appraisals reported by patients and caregivers will be negatively associated with their own self-efficacy (individual and family-related) and the other member of the dyad.
b) In the efficacy mediated model, self-efficacy reported by patients and caregivers will be negatively associated with their own threat appraisals and the threat appraisals of the other member of the dyad.
-
H4:
a) In the threat mediated model, symptom distress will have a negative indirect effect on self-efficacy (mediated by threat appraisals).
b) In the efficacy mediated model, symptom distress will have a positive indirect effect on threat appraisals (mediated by self-efficacy).
Figure 1.
Threat Mediated Model Testing the Influence of Patient and Caregiver Symptom Distress on Threat Appraisals (Mediator) and Efficacy
Figure 2.
Efficacy Mediated Model Testing the Influence of Patient and Caregiver Symptom Distress on Self-Efficacy (Mediator) and Threat Appraisals
Method
Study Design
Data came from a randomized clinical trial (RCT) for patients with advanced cancer and their family caregivers that tested the efficacy of the evidence-based FOCUS program. Data were collected in the home by research staff who were blinded to the RCT group assignments of dyads. Patients and caregivers completed their questionnaires separately, without consulting each other, while a research staff member was present in the home. Our current analysis used baseline data. Detailed information related to the RCT procedures and study outcomes have been published elsewhere [26]. Institutional Review Board approval was obtained from the patient's cancer center and the University of Michigan (coordinating site).
Participants
The study sample included patients with advanced cancer and their family caregivers (N=484 dyads). All patients: were age 21 or older; had a confirmed diagnosis of advanced breast, colon, lung or prostate cancer and were within 6 months of the diagnosis, progression of their cancer, or a change of treatment for it; and, had a life expectancy of at least 6 months (as assessed by a physician). Patients diagnosed with multiple primary cancer sites were excluded from the study. The percentages of advanced cancers reported by patients were as follows: 32.4% breast cancer; 29.1% lung cancer; 25.4% colorectal cancer; and, 13.0% prostate cancer. A majority of patients were undergoing chemotherapy treatment (68.8%). Patients also reported receiving hormone therapy (16.5%), radiation therapy (8.3%), watchful waiting (7.6%), surgical treatment (2.9%) or another treatment not specified (5.4%) at baseline. Multiple responses for treatment were possible.
A family caregiver was defined as “the family member or significant other identified by the patient as his or her primary source of physical or emotional support during the advanced phase of cancer and confirmed by the designated individual” [26]. Family caregivers were age 18 or older and were excluded from the study if they had been diagnosed with cancer during the previous year and/or were in active treatment for cancer.
Patient and caregiver demographic information is presented in Table 1. The average age of patients was 60.5 years (SD: 11.5; range: 26–95) and of caregivers were 56.5 years (SD: 13.4; range: 18–88). Most patients (62%) and caregivers (56.8%) were female. Patients and caregivers were predominantly White (approximately 80%). A majority of patients (75.6%) and caregivers (82.9%) were married or living as married and 70% were in a marital relationship with each other.
Table 1.
Patient and Caregiver Demographic Information
| Patients (N=484) | Caregivers (N=484) | Difference Test | |
|---|---|---|---|
| Age in years | |||
| Mean (SD) | 60.5(11.5) | 56.5(13.4) | p=.004a |
| Range | 26–95 | 18–88 | |
| Sex (%) | |||
| Female | 62.0 | 56.8 | p=.237b |
| Male | 38.0 | 43.1 | |
| Race (%) | |||
| American Indian/Alaskan Native | 0.2 | 0 | p=.589c |
| Asian | 1.0 | 1.2 | |
| Black | 15.3 | 15.9 | |
| Pacific Islander | 0.2 | 0 | |
| White | 79.3 | 79.6 | |
| Multiracial | 3.9 | 2.5 | |
| Highest level of education in years | |||
| Mean (SD)a | 14.5 (2.7) | 14.6(2.8) | p=.748a |
| Marital Status (%) | |||
| Married/Living as married | 75.6 | 82.9 | p=.002c |
| Divorced/Separated | 13.2 | 8.1 | |
| Widowed | 6.0 | 2.3 | |
| Never married | 5.2 | 6.8 | |
| Relationship to patient (%; caregiver only) | -- | ||
| Spouse | -- | 70.0 | |
| Daughter | -- | 12.0 | |
| Son | -- | 3.3 | |
| Sister/Brother | -- | 0.2 | |
| Other relative | -- | 5.6 | |
| Friend | -- | 4.3 | |
| Unknown/Coding error | -- | 4.5 | |
| Currently living with patient (caregiver only) | -- | ||
| % Yes | -- | 82.6 |
Paired sample t-tests;
McNemar's Test;
Chi-Square Test.
Instruments
Symptom distress
The 16-item Symptom Scale of the Risk for Distress Scale (patients: α = .74; caregivers: α = .89) was used to assess patient and caregiver physical and psychological symptom distress [27,28]. Patients reported on the trouble experienced because of their cancer related and non-cancer symptoms during the past week; caregivers reported on the trouble experienced because of their own symptoms during the past week. Descriptive response options were appropriate for the symptoms and generally represented: 0) no trouble, 1) some, and, 2) a lot. The z-scored total scale score was used in the analysis to standardize the items, with higher scores indicating higher symptom distress.
Threat appraisal
Threat appraisals were assessed with the 11-item subscale of the Appraisal of Illness Scale (patients: α = .90) and a corresponding 11-item subscale of the Appraisal of Caregiving Scale (caregivers: α =.89) [29–31]. Respondents answered questions based upon how they felt “over the last week including today.” An example item is “This situation threatens to overwhelm me.” Both instruments have a 5-point response scale ranging from “strongly disagree” to “strongly agree.” The total subscale score was used in the analysis with higher scores indicating higher threat appraisals.
Self-efficacy
Self-efficacy to manage the impact of the illness was measured using two-subscales from the shorter version of the CASE Scale [32]. The 11-item individual self-efficacy subscale measured patient/caregiver confidence in their ability to manage the general impact of cancer on themselves (patients: α = .96; caregivers: α = .95). An example item from this subscale is “I am confident that I can put the cancer into proper perspective in my life.” The 4-item family-related self-efficacy subscale measured patient/caregiver confidence in their ability to manage the impact of cancer on their family (patients: α = .94; caregivers: α = .91). An example item from this subscale is “I am confident that I have what it takes to help my family through the illness.” Responses were on a 10-point scale ranging from 0 (not at all confident) to 10 (very confident). The total subscale scores were used in the analysis with higher scores indicating higher self-efficacy.
Covariates
There are a number of demographic and medical factors which may influence relationships between patient and caregiver symptom distress and appraisal processes in advanced cancer. For example, younger age, lower income and female has been associated with more negative appraisals [33,34] and differences in appraisals have been seen by caregiver relationship type [33] as well as cancer type and time since diagnosis [35]. Age, sex, income, patient cancer type, patient treatment (chemotherapy vs. other; hormone therapy vs. other), length of time since patient diagnosis, living arrangements (living together vs. other), and the relationship between patient and caregiver (spouse vs. other) were obtained from patient medical records and the self-administered Risk for Distress Scale, which was adapted from the original Omega Clinic Screening Interview [26–28].
Data Analysis Strategy
The hypotheses were examined using the actor-partner interdependence mediation model or APIMeM [36]. This model consists of three pairs of variables corresponding to each dyad member: predictor variables (symptom distress); mediator variables (threat appraisals); and, outcome variables (self-efficacy). Path analysis with structural equation modeling (SEM) was used to estimate the model parameters using MPlus version 7. There was a small percentage (<1%) of missing data for the main study variables (symptom distress and appraisals); among covariates, there was missing data among caregiver gender (<1%) and income (12%) variables. To account for missing data, full information maximum likelihood estimation (FIML) was utilized. All models included covariances between predictor variables, and covariances between error terms of patient and caregiver threat appraisals and efficacy variables.
Mediation effects were tested using the bootstrapping procedure in MPlus. Three fit indices were used to determine the adequacy of model fit: the comparative fit index (CFI), the root mean squared error of approximation (RMSEA), and the standardized root-mean-square residual (SRMR). The indicators of adequate model fit for these indices (i.e. the indication that the model fits the sample data well) are a CFI value of .90 or more; a RMSEA value of .06 or less; a non-significant chi-square (χ2) value; and, a SRMR value of .08 or less [37]. The Bayesian Information Criterion (BIC) was used for model selection, with a difference in BIC values of greater than 10 very strong evidence that the model with the smaller BIC value is preferred [38].
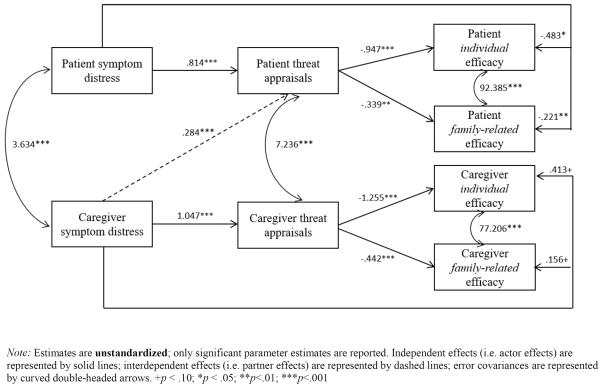
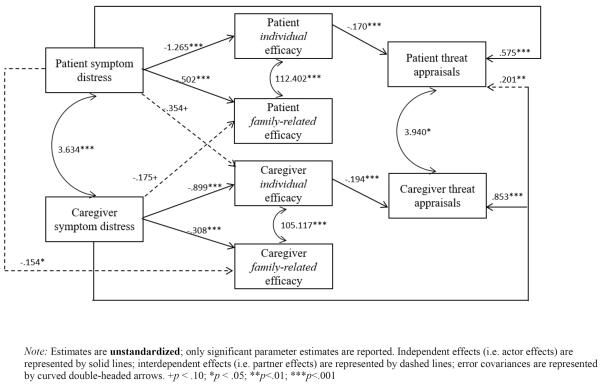
Results
Table 2 provides means, standard deviations for symptom distress, threat appraisals, and self-efficacy variables and the correlations among these variables. Significant differences were found between patient and caregiver threat appraisals (p<.001) and symptom distress (p<.001). Two models were tested (unstandardized results presented in Figures 3 & 4, respectively). The model fit was good in the threat mediated model (CFI=1.00; RMSEA=.000 (CI: 0.000, 0.043); χ2(16) = 16.26, p=0.3685; SRMR=.009) and the efficacy mediated model (CFI=1.00; RMSEA =.013 (CI: 0.000, 0.049); χ2(16) = 16.26, p=0.4351; SRMR=.007). The efficacy mediated model had a lower BIC value (43821.492 vs. 43800.015), and a difference in values greater than 10 (BIC difference = 21.477), indicating that the efficacy mediated model is preferred. Thus, we focus the discussion of results on the efficacy mediated model (Figure 4).
Table 2.
Means, Standard Deviations and Correlations for Symptom Distress, Threat Appraisals and Self-Efficacy among Patients and Caregivers (N=484)
| Symptom Distress | Threat Appraisals | Individual Self-Efficacy | Family-Related Self-Efficacy | |||||
|---|---|---|---|---|---|---|---|---|
| PT | CG | PT | CG | PT | CG | PT | CG | |
| Means | 10.25 | 5.98 | 35.76 | 30.84 | 85.69 | 85.18 | 31.04 | 31.69 |
| SD | 4.65 | 4.32 | 9.11 | 8.62 | 19.22 | 18.22 | 7.94 | 6.94 |
| Difference Testa | p<.001 | p<.001 | p=.754 | p=.130 | ||||
| Correlations | ||||||||
| PT Symptom Distress | 1 | |||||||
| CG Symptom Distress | .18*** | 1 | ||||||
| PT Symptom Distress | .44*** | .18*** | 1 | |||||
| CG Symptom Distress | .14** | .54*** | .21*** | 1 | ||||
| PT Symptom Distress | −.31*** | −.14** | −.50*** | −.15** | 1 | |||
| CG Symptom Distress | −.13** | −.23*** | −.13** | −.55*** | .09+ | 1 | ||
| PT Symptom Distress | −.32*** | −.14** | −.47*** | −.14** | .87*** | .09+ | 1 | |
| CG Symptom Distress | −.13** | −.22*** | −.13** | −.51*** | .11* | .92*** | .11* | 1 |
PT=Patient; CG=Caregiver
Paired sample t-test.
p < .10;
p < .05;
p<.01;
p<.001
Symptom distress scores: patient range = 0 – 23; caregiver range: 0–23. Minimum possible score = 0; maximum possible score = 32.
Threat appraisal scores: patient range = 11 – 55; caregiver range: 11–53. Minimum possible score = 5; maximum possible score = 55.
Individual self-efficacy scores: patient range = 4 – 110; caregiver range: 21 – 110. Minimum possible score = 0; maximum possible score = 110.
Family-related self-efficacy scores: patient range = 2 – 40; caregiver range: 5 – 40. Minimum possible score = 0; maximum possible score = 40.
Figure 3.
Path Analysis Results: the Influence of Patient and Caregiver Symptom Distress on Threat Appraisals and Efficacy
Figure 4.
Path Analysis Results: the Influence of Patient and Caregiver Symptom Distress on Efficacy and Threat Appraisals
H1. Symptoms→ threat. Supporting our hypothesis, holding all other variables constant, patients and caregivers higher in symptom distress were higher in threat appraisals (actor effects). Specifically, for every one unit increase in patient symptom distress, patient threat appraisals were expected to increase by .575 units (p<.001). Similarly, for every one unit increase in caregiver symptom distress, caregiver appraisals were expected to increase by .853 units (p<.001). The second part of the hypothesis was partially supported. Holding all other variables constant, where caregivers were higher in symptom distress, patients were higher in threat appraisals (partner effect): a one unit increase in caregiver symptom distress was expected to result in a .201 unit increase in patient threat appraisals (p=.008).
H2. Symptom → efficacy. In line with the hypothesis, holding all other variables constant, patients and caregivers with higher symptom distress were lower in individual- and family-related self-efficacy (actor effects). Specifically, for every one unit increase in patient symptom distress, patient individual self-efficacy was expected to decrease by 1.265 units (p<.001) and patient family-related self-efficacy was expected to decrease by .502 units (p<.001). Similarly, for every one unit increase in caregiver symptom distress, caregiver individual self-efficacy was expected to decrease by .899 units (p<.001), and caregiver family-related self-efficacy was expected to decrease by .308 units (p<.001). There was also a significant partner effect: holding all other variables constant, where patients were higher in symptom distress, caregiver family-related self-efficacy was lower. Specifically, for every one unit increase in patient symptom distress, caregiver family-related self-efficacy was expected to decrease by .154 units (p=.034).
H3. Efficacy → threat. As hypothesized, holding all other variables constant, patients and caregivers with higher individual-related self-efficacy were lower in threat appraisals (actor effects). For every one unit increase in patient individual self-efficacy, patient threat appraisals were expected to decrease by .170 units (p<.001); similarly, for every one unit increase in caregiver individual self-efficacy, caregiver threat appraisals were expected to decrease by .194 units (p<.001). However, neither patient nor caregiver family-related self-efficacy were significantly associated with decreases in their own threat appraisals. In addition, there were no partner effects of self-efficacy on threat appraisals.
H4. Indirect effects of symptoms on threat. Patient symptom distress had a positive indirect effect on patient threat appraisals through patient individual self-efficacy (β=.215; 95% CI: 0.117, .348). Caregiver symptom distress had a positive indirect effect on caregiver threat appraisals through caregiver individual self-efficacy (β=.175; 95% CI: 0.075, 0.318).
Discussion
The purpose of this study was to examine the influence of patient and caregiver symptom distress on their threat appraisals and their self-efficacy for coping with the illness (individual and family-related) in two competing models: one in which threat appraisals mediated the relationship between symptom distress and self-efficacy (threat mediated model), and another which in which self-efficacy mediated the relationship between symptom distress and threat appraisals (efficacy mediated model). Symptom distress was assessed for cancer (patients) and non-cancer related health problems (patients and caregivers). Symptom distress had direct effects on both dimensions of self-efficacy, and direct and indirect effects on threat appraisals. Results support self-efficacy as a mediator of the relationship between symptom distress and threat appraisals.
Supporting our hypothesis, patients and caregivers with more symptom distress appraised the cancer situation as more threatening and reported less individual and family-related self-efficacy. This suggests that cancer-related symptoms and non-cancer related symptoms influence their appraisals about the cancer experience. In addition, more caregiver symptom distress was directly associated with higher patient threat appraisals, suggesting that caregivers' own health issues influence how threatening patients appraise their cancer situation. Tishelman and colleagues [39] describe the influence of symptom distress from both physical and psychological perspectives. Physically, the effects of the symptoms themselves could influence the extent to which patients appraise the cancer/caregiving situation as threatening and their assessment of their ability to manage the consequences of advanced cancer. Psychologically, the meanings the symptoms have for an individual also have importance. For example, patients' experience of symptoms could be perceived as turning points in their health status or reminders of their current and future dependency on others [40]. Caregivers' experience of symptoms could be perceived as a consequence of providing care and a reminder of their own care needs.
Symptom distress also had indirect effects on threat appraisals. As a mediating factor, patient and caregiver individual self-efficacy helped to explain the relationship between their own symptom distress and threat appraisals (i.e., indirect effects). This suggests that the management of patient and caregiver symptoms may benefit their cancer-related cognitive appraisals. While a number of studies have reported how various domains of self-efficacy (e.g. general, symptom management, caregiving self-efficacy) predict symptom-related outcomes [41,42] this study contributes to the literature by demonstrating that cancer and non-cancer related symptoms are important predictors of cancer/caregiving-related self-efficacy and that attention to patient and caregiver symptom distress could positively influence self-efficacy and threat related outcomes.
Furthermore, while symptom distress had indirect effects on threat appraisals, this indirect effect operated only through patients' and caregivers' own individual self-efficacy. This could be due to the fact that the items assessing threat appraisals were individual in nature (e.g., I feel that things are going to get worse for me). Future studies that examine this relationship should also include threat appraisals specifically related to the family. Evidence shows that cancer has a significant impact on the entire family system and despite their own needs, patients and caregivers provide support to others [22,43]. An important finding of this study is that their self-efficacy to do so was strongly influenced by their symptom distress. While much of the cancer literature has focused on how social support from family members influence patient and caregiver outcomes, more research is needed on how factors such symptom distress influence their capacity (self-efficacy) to help others.
Theory and research on self-efficacy often focuses on individual efforts [44]. Similarly, research on adults with advanced cancer and caregivers often conceptualize the “family” as represented by these two individuals. In reality, as noted by Bandura and colleagues [44], the dyad “is but one of the multiple interdependent subsystems operating within a family system.” Factors associated with family systems – including interdependence, support, alliances, and resources – likely influence an individual's own self-efficacy in various domains [44,45]. As such, aspects of the dyad and the broader family system likely affect the degree of individual and family-related self-efficacy reported by patients and caregivers in this study. This should be considered explicitly in future research. In addition, future studies may benefit from understanding the relationship between patient, caregiver and broader family members' individual self-efficacy and their collective family efficacy for coping with the disease, caregiving, and its consequences. Very little research has been done in this area [45]. Understanding these different types of efficacy will likely be useful to interventions focused on self and family-management of cancer and chronic conditions.
There are study limitations to consider. First, patients were asked to report about their cancer and non-cancer related symptoms. It would be useful to determine if patients' beliefs about the cause of the symptoms (i.e. cancer related or non-cancer related) influence their appraisal and self-efficacy. One of the challenges in collecting this information is that it can often be difficult for individuals to determine a cause for symptoms where multimorbidity exists; however, it could be argued that what matters more is patient/caregiver perceptions of symptom origin. In addition, this study utilized cross-sectional data. Longitudinal investigations of the relationship between symptom distress and cognitive appraisals could highlight key points of transition and need throughout the trajectory of the advanced cancer experience. As mentioned above, our measure of threat appraisals included threat perceptions related to patients and caregivers as individuals (e.g., I feel that things are going to get worse for me) and not as a part of a family system (e.g., I feel that things are going to get worse for my family). Future studies should consider the inclusion of family-related threat appraisals. Lastly, there are a number of familial factors (e.g., family structure, communalism) that could influence relationships between the study variables and should be considered in future research. Despite these limitations, strengths of this study include the ability to recruit a relatively large sample of advanced cancer patient/caregiver dyads and the consideration of the health issues of both individuals.
Conclusions
This study suggests that the management of patients' and caregivers' symptoms are worthwhile intervention goals. While a number of successful pharmacological and behavioral interventions exist for improving symptom management for patients, many barriers to timely use of palliative care remain. Moreover, though caregiver assessment tools often take caregiver health into account, the use of caregiver assessment tools in practice is not consistent. Increased usage of patient palliative care, caregiver assessments, and supportive health care for family caregivers may be helpful for identifying the need for additional intervention and resources. Given the noted importance of cognitive appraisals in the stress and coping process, future research and interventions should take into account how the health concerns of both members of the dyad influence these factors.
Acknowledgements
The preparation of this manuscript by the first author was supported by Rackham Graduate School at the University of Michigan, and the Cancer Health Disparities Training Program (2T32CA128582-06) and Center for Health Equity Research at the University of North Carolina. Data come from a study funded by a grant from the National Cancer Institute (RO1CA107383, L. Northouse).
Footnotes
Disclosures: None
References
- 1.Schofield P, Carey M, Love A, Nehill C, Wein S. Would you like to talk about your future treatment options?' Discussing the transition from curative cancer treatment to palliative care. Palliative Medicine. 2006;20(4):397–406. doi: 10.1191/0269216306pm1156oa. doi:10.1191/0269216306pm1156oa. [DOI] [PubMed] [Google Scholar]
- 2.Lazarus RS, Folkman S. Stress, appraisal, and coping. Springer Pub. Co.; New York: 1984. [Google Scholar]
- 3.Wenzel L, Glanz K, Lerman C. Stress, coping and health behavior. In: Glanz K, Rimer BK, Lewis FM, editors. Health behavior and health education. 3rd edn Jossey-Bass; San Francisco: 2002. pp. 210–239. [Google Scholar]
- 4.Strecher VJ, McEvoy DeVellis B, Becker MH, Rosenstock IM. The role of self-efficacy in achieving health behavior change. Health Education & Behavior. 1986;13(1):73–92. doi: 10.1177/109019818601300108. doi:10.1177/109019818601300108. [DOI] [PubMed] [Google Scholar]
- 5.Franks HM, Roesch SC. Appraisals and coping in people living with cancer: a meta-analysis. Psycho-Oncology. 2006;15(12):1027. doi: 10.1002/pon.1043. [DOI] [PubMed] [Google Scholar]
- 6.Fitzell A, Pakenham KI. Application of a stress and coping model to positive and negative adjustment outcomes in colorectal cancer caregiving. Psycho-Oncology. 2010;19(11):1171–1178. doi: 10.1002/pon.1666. [DOI] [PubMed] [Google Scholar]
- 7.Northouse LL, Walker J, Schafenacker A, Mood D, Mellon S, Galvin E, Harden J, Freeman-Gibb L. A family-based program of care for women with recurrent breast cancer and their family members. Oncology Nursing Forum. 2002;29(10):1411–1419. doi: 10.1188/02.ONF.1411-1419. doi:10.1188/02.onf.1411-1419. [DOI] [PubMed] [Google Scholar]
- 8.Given BA, Sherwood PR, Given CW. What knowledge and skills do caregivers need? American Journal of Nursing. 2008;108(9 SUPPL.):28–34. doi: 10.1097/01.NAJ.0000336408.52872.d2. [DOI] [PubMed] [Google Scholar]
- 9.Walsh D, Rybicki L. Symptom clustering in advanced cancer. Supportive care in cancer. 2006;14(8):831–836. doi: 10.1007/s00520-005-0899-z. doi:10.1007/s00520-005-0899-z. [DOI] [PubMed] [Google Scholar]
- 10.Chang H-H. Functional food consumption and depression among the elderly — What can we learn from a longitudinal survey? Economic Modelling. 2013;33(0):187–193. doi: http://dx.doi.org/10.1016/j.econmod.2013.04.023. [Google Scholar]
- 11.Peppercorn JM, Smith TJ, Helft PR, DeBono DJ, Berry SR, Wollins DS, Hayes DM, Von Roenn JH, Schnipper LE. American Society of Clinical Oncology statement: Toward individualized care for patients with advanced cancer. Journal of Clinical Oncology. 2011;29(6):755–760. doi: 10.1200/JCO.2010.33.1744. doi:10.1200/jco.2010.33.1744. [DOI] [PubMed] [Google Scholar]
- 12.Barnes EA, Bruera E. Fatigue in patients with advanced cancer: A review. International Journal of Gynecological Cancer. 2002;12(5):424–428. doi: 10.1046/j.1525-1438.2002.t01-1-01147.x. doi:10.1046/j.1525-1438.2002.t01-1-01147.x. [DOI] [PubMed] [Google Scholar]
- 13.Riley-Doucet C. Beliefs about the controllability of pain: Congruence between older adults with cancer and their family caregivers. Journal of Family Nursing. 2005;11(3):225–241. doi: 10.1177/1074840705279157. doi:10.1177/1074840705279157. [DOI] [PubMed] [Google Scholar]
- 14.Litzelman K, Green P, Yabroff KR. Cancer and quality of life in spousal dyads: spillover in couples with and without cancer-related health problems. Supportive Care in Cancer. 2015;24(2):763–771. doi: 10.1007/s00520-015-2840-4. doi:10.1007/s00520-015-2840-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Northouse LL, Katapodi MC, Schafenacker AM, Weiss D. The impact of caregiving on the psychological well-being of family caregivers and cancer patients. Seminars in Oncology Nursing. 2012;28(4):236–245. doi: 10.1016/j.soncn.2012.09.006. doi :http://dx.doi.org/10.1016/j.soncn.2012.09.006. [DOI] [PubMed] [Google Scholar]
- 16.Northouse LL. Helping patients and their family caregivers cope with cancer. Oncology Nursing Forum. 2012;39(5):500–506. doi: 10.1188/12.ONF.500-506. doi:10.1188/12.onf.500-506. [DOI] [PubMed] [Google Scholar]
- 17.Centers for Disease Control & Prevention Trends in aging--United States and worldwide. MMWR Morbidity and Mortality Weekly Report. 2003;52(6):101. [PubMed] [Google Scholar]
- 18.Romito F, Goldzweig G, Cormio C, Hagedoorn M, Andersen BL. Informal caregiving for cancer patients. Cancer. 2013;119(0 11) doi: 10.1002/cncr.28057. 10.1002/cncr.28057. doi:10.1002/cncr.28057. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Acton GJ. Health-promoting self-care in family caregivers. Western Journal of Nursing Research. 2002;24(1):73–86. doi: 10.1177/01939450222045716. [DOI] [PubMed] [Google Scholar]
- 20.Vitaliano PP, Zhang J, Scanlan JM. Is caregiving hazardous to one's physical health? A meta-analysis. Psychological Bulletin. 2003;129(6):946–972. doi: 10.1037/0033-2909.129.6.946. [DOI] [PubMed] [Google Scholar]
- 21.Mellon S, Northouse L. Family survivorship and quality of life following a cancer diagnosis. Research in Nursing Health. 2001;24(6):446. doi: 10.1002/nur.10004. [DOI] [PubMed] [Google Scholar]
- 22.Ashing-Giwa KT, Padilla G, Tejero J, Kraemer J, Wright K, Coscarelli A, Clayton S, Williams I, Hills D. Understanding the breast cancer experience of women: a qualitative study of African American, Asian American, Latina and Caucasian cancer survivors. Psycho-Oncology. 2004;13(6):408. doi: 10.1002/pon.750. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Guillet L, Hermand D, Mullet E. Cognitive processes involved in the appraisal of stress. Stress and Health. 2002;18(2):91–102. doi: 10.1002/smi.927. [Google Scholar]
- 24.Lewis MA, McBride CM, Pollak KI, Puleo E, Butterfield RM, Emmons KM. Understanding health behavior change among couples: An interdependence and communal coping approach. Social Science & Medicine. 2006;62(6):1369–1380. doi: 10.1016/j.socscimed.2005.08.006. doi:10.1016/j.socscimed.2005.08.006. [DOI] [PubMed] [Google Scholar]
- 25.Rusbult CE, Van Lange PA. Interdependence, interaction, and relationships. Annual Review of Psychology. 2003;54(1):351–375. doi: 10.1146/annurev.psych.54.101601.145059. [DOI] [PubMed] [Google Scholar]
- 26.Northouse LL, Mood DW, Schafenacker A, Kalemkerian G, Zalupski M, LoRusso P, Hayes DF, Hussain M, Ruckdeschel J, Fendrick AM, Trask PC, Ronis DL, Kershaw T. Randomized clinical trial of a brief and extensive dyadic intervention for advanced cancer patients and their family caregivers. Psycho-Oncology. 2013;22(3):555–563. doi: 10.1002/pon.3036. doi:10.1002/pon.3036. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Mood D, Bickes J. Strategies to enhance self-care in radiation therapy. Oncology Nursing Forum. 1989;16(Suppl):143. [Google Scholar]
- 28.Northouse LL, Mood DW, Montie JE, Sandler HM, Forman JD, Hussain M, Pienta KJ, Smith DC, Sanda MG, Kershaw T. Living with prostate cancer: patients' and spouses' psychosocial status and quality of life. Journal of Clinical Oncology. 2007;25(27):4171–4177. doi: 10.1200/JCO.2006.09.6503. doi:10.1200/jco.2006.09.6503. [DOI] [PubMed] [Google Scholar]
- 29.Lambert SD, Yoon H, Ellis KR, Northouse L. Measuring appraisal during advanced cancer: Psychometric testing of the appraisal of caregiving scale. Patient Education and Counseling. 2015;98(5):633–639. doi: 10.1016/j.pec.2015.01.009. doi: http://dx.doi.org/10.1016/j.pec.2015.01.009. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Oberst M. Appraisal of Illness Scale (AIS-Revised): Manual for Use. Wayne State University; Detroit, MI: 1991. [Google Scholar]
- 31.Oberst M. Appraisal of Caregiving Scale (ACS-Revised): Manual for Use. Wayne State University; Detroit, MI: 1991. [Google Scholar]
- 32.Lewis FM. Family home visitation study final report. National Cancer Institute; National Institutes of Health: 1996. [Google Scholar]
- 33.Kim Y, Baker F, Spillers RL, Wellisch DK. Psychological adjustment of cancer caregivers with multiple roles. Psycho-Oncology. 2006;15(9):795–804. doi: 10.1002/pon.1013. doi: 10.1002/pon.1013. [DOI] [PubMed] [Google Scholar]
- 34.Oberst MT, Thomas SE, Gass KA, Ward SE. Caregiving demands and appraisal of stress among family caregivers. Cancer Nursing. 1989;12(4):209–215. [PubMed] [Google Scholar]
- 35.van't Spijker A. Psychological sequelae of cancer diagnosis: a meta-analytical review of 58 studies after 1980. Psychosomatic Medicine. 1997;59(3):280–293. doi: 10.1097/00006842-199705000-00011. [DOI] [PubMed] [Google Scholar]
- 36.Ledermann T, Macho S, Kenny DA. Assessing mediation in dyadic data using the actor-partner interdependence model. Structural Equation Modeling: A Multidisciplinary Journal. 2011;18(4):595–612. [Google Scholar]
- 37.Hu Lt, Bentler PM. Cutoff criteria for fit indexes in covariance structure analysis: Conventional criteria versus new alternatives. Structural Equation Modeling: A Multidisciplinary Journal. 1999;6(1):1–55. doi:10.1080/10705519909540118. [Google Scholar]
- 38.Raftery AE. Bayesian model selection in social research. Sociological Methodology. 1995;25:111–164. [Google Scholar]
- 39.Tishelman C, Taube A, Sachs L. Self-reported symptom distress in cancer patients: Reflections of disease, illness or sickness? Social Science & Medicine. 1991;33(11):1229–1240. doi: 10.1016/0277-9536(91)90071-j. doi: http://dx.doi.org/10.1016/0277-9536(91)90071-J. [DOI] [PubMed] [Google Scholar]
- 40.Oechsle K, Wais MC, Vehling S, Bokemeyer C, Mehnert A. Relationship between symptom burden, distress, and sense of dignity in terminally ill cancer patients. Journal of Pain and Symptom Management. 2014;48(3):313–321. doi: 10.1016/j.jpainsymman.2013.10.022. doi :http://dx.doi.org/10.1016/j.jpainsymman.2013.10.022. [DOI] [PubMed] [Google Scholar]
- 41.Keefe FJ, Ahles TA, Porter LS, Sutton LM, McBride CM, Pope MS, Baucom DH. The self-efficacy of family caregivers for helping cancer patients manage pain at end-of-life. Pain. 2003;103(1–2):157–162. doi: 10.1016/s0304-3959(02)00448-7. [DOI] [PubMed] [Google Scholar]
- 42.Lev EL, Paul D, Owen SV. Age, self-efficacy, and change in patients' adjustment to cancer. Cancer Practice. 1999;7(4):170–176. doi: 10.1046/j.1523-5394.1999.74004.x. doi: 10.1046/j.1523-5394.1999.74004.x. [DOI] [PubMed] [Google Scholar]
- 43.Segrin C, Badger T, Dorros SM, Meek P, Lopez AM. Interdependent anxiety and psychological distress in women with breast cancer and their partners. Psycho-Oncology. 2007;16(7):634–643. doi: 10.1002/pon.1111. doi:10.1002/pon.1111. [DOI] [PubMed] [Google Scholar]
- 44.Bandura A, Caprara GV, Barbaranelli C, Regalia C, Scabini E. Impact of family efficacy beliefs on quality of family functioning and satisfaction with family life. Applied Psychology. 2011;60(3):421–448. [Google Scholar]
- 45.Bandura A. Exercise of human agency through collective efficacy. Current directions in Psychological Science. 2000;9(3):75–78. [Google Scholar]