Medical professionals and laypeople alike understand the fact that people with diabetes are at increased risk for serious medical complications such as cardiovascular disease, kidney disease, peripheral neuropathy, and lower extremity amputations.1 However, I have observed that many people, including people with diabetes and the rehabilitation health providers treating them, are not aware of a large body of evidence linking diabetes with increased risk for numerous musculoskeletal impairments and complications.2 These impairments are apparent in type 1 diabetes (due to beta cell destruction, usually leading to absolute insulin deficiency) and type 2 diabetes (due to progressive loss of insulin secretion on the background of insulin resistance). The purpose of this point of view is to highlight the musculoskeletal impairments that are exacerbated, or potentially even caused, by metabolic disorders associated with diabetes. This article will focus on those musculoskeletal impairments most often encountered by physical therapists and other rehabilitation practitioners, describe the systemic condition of limited joint mobility, and briefly outline a likely mechanism for musculoskeletal impairments. Finally, the article will briefly provide clinical and research implications for those in rehabilitation working with this population.
Common Musculoskeletal Problems in People With Diabetes
Metabolic dysfunctions clearly leave people with diabetes at high risk for developing musculoskeletal pain and impairments. In a large Danish study that compared patients with type 2 diabetes (n=951) directly with age-, sex-, and region-matched control participants (n=22,923), the patients with diabetes were 1.7 to 2.1 times more likely to report musculoskeletal pain compared with those without diabetes.3 Consistent with this high risk for musculoskeletal disorders, the group with diabetes reported high incidences of shoulder or neck pain (52%); low back pain (60%); and arm, hand, knee, or hip pain (71%).3 Furthermore, people pursuing physical therapy for musculoskeletal pain and impairments often have a secondary diagnosis of diabetes or have risk factors for diabetes. Although people with diabetes make up about 9% of the total population in the United States (21 million diagnosed and 8.1 million undiagnosed Americans), Kirkness et al4 reported that approximately 80% of the 52,667 patients referred for physical therapy as part of the national primary care electronic medical record database had diabetes, prediabetes, or risk factors associated with diabetes. This same report indicated that the majority of physical therapy visits from this population were for musculoskeletal-related conditions.
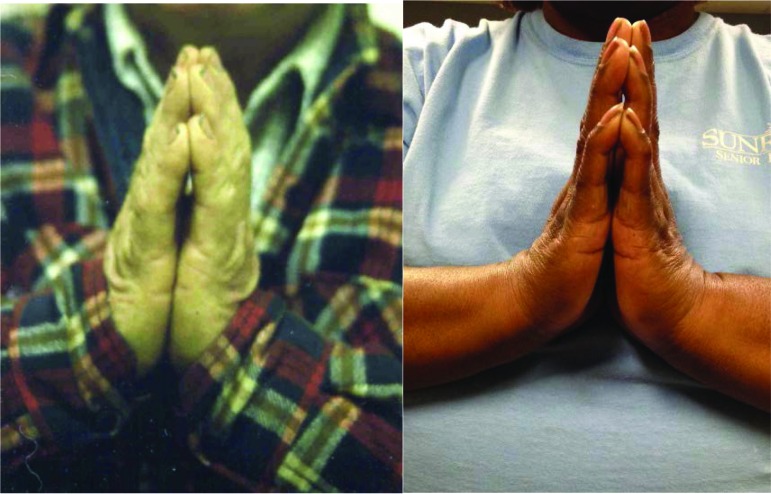
Musculoskeletal complications of diabetes in the upper extremity have been well documented. Larkin et al5 reported that 66% of participants of a large diabetes trial (N=1,217) had cheiroarthropathy, defined as the development of periarticular thickening of skin on the hands and limited joint mobility. Participants with type 1 diabetes were classified as having cheiroarthropathy if they showed adhesive capsulitis, carpal tunnel syndrome, flexor tenosynovitis, or a “positive prayer sign” using a targeted medical history and standardized physical examination.5 The positive prayer sign can be used as an indicator of systemic limited joint mobility problems and is defined as an inability to approximate interphalangeal joints of the hand when pressed together (Figure).6 Likewise, in a group of participants with type 2 diabetes attending a diabetes center, Shah et al7 reported that 63% (149/236) had shoulder pain or disability as measured with the Shoulder Pain and Disability Index (SPADI) (median SPADI score=10, interquartile range=0.0–39.6). In another recent, larger study, Mustafa et al8 reported that 69.5% of patients (n=1,000) with type 2 diabetes had hand disorders, with limited joint mobility (Figure) being the most prevalent condition (63%). Dupuytren contracture, trigger finger, and carpal tunnel syndrome are other musculoskeletal disorders of the hand that have high incidences in people with diabetes.2,5,8
Figure.
Positive prayer sign used as a screen for limited joint mobility. Individuals unable to approximate hands when asked to press them together, indicating limited joint mobility in the interphalangeal joints (ie, limited joint motion throughout their body) that often is an indicator of systemic limited joint motion.
As noted above, limited joint mobility was first observed in the hands and described as the positive prayer sign (Figure).6 The incidence of a positive prayer sign varies widely (30%–76%) depending on the diabetes duration and control of the study participants, but recent articles report rates of 63% compared with an expected rate of 4% to 20% in people without diabetes.2,7 In addition to the upper extremity, limited joint mobility also is well documented in the talocrural, subtalar, and metatarsophalangeal joints of the feet of people with diabetes and especially those with peripheral neuropathy.9,10 Skin and joints of the feet become less flexible and less sensitive to pain and pressure, develop faulty movement patterns, and are less able to distribute stresses.11–13 This combination of limited joint mobility and neuropathy in the feet of people with diabetes is especially problematic because of their established risk factors for lower extremity amputation.13
Limited joint mobility has been best documented and described in the relatively small joints of the hands and feet, likely because limitations are more noticeable and more easily measured compared with the larger, more proximal joints. However, there is growing evidence for an insidious reduction of mobility in larger, more proximal joints, including the hip and shoulder joints, of people with diabetes.7,14,15 This gradual and insidious loss of glenohumeral motion may be a precursor to more severe shoulder problems. The high incidence of severe shoulder problems such as adhesive capsulitis in people with diabetes is well documented. As one example, Milgrom et al16 reported that men and women with diabetes had a risk ratio of 5.0 to 5.9 (95% confidence interval=3.3, 7.5; P<.001) for developing idiopathic frozen shoulder compared with those without diabetes. Because of the systemic influence of diabetic complications on collagen tissues (described below), limited joint mobility likely affects every joint in the body, not just the hands, feet, and shoulder joints, where its effects have been best documented.
Possible Mechanisms for Musculoskeletal Disorders in People With Diabetes
Although there are several possible mechanisms, a primary mechanism for musculoskeletal complications observed in people with diabetes appears to be the formation of nonenzymatic advanced glycation end products (AGEs) and AGE receptors (RAGEs) in collagen-rich structures.15,17–19 These AGEs form in all people and generally accumulate in various tissues with aging.15,19 However, AGEs and RAGEs form at a much faster rate and accumulate more in people with diabetes compared with those without diabetes.15,18 In people with diabetes, the excessive glucose condenses with metabolic intermediates to form AGEs, which are broken down only when the metabolic intermediates degrade. These AGEs generally accumulate with duration and severity of the disease state (ie, lack of glycemic control).5,17 These metabolic disorders associated with diabetes are systemic, with the potential to affect every cell in the body. Advanced glycation end products, such as pentosidine, and RAGEs tend to accumulate, however, in tissues with low-protein turnover such as tendons, ligaments, and skin.17,20,21 The tissues tend to become thicker, stiffer, weaker, and more susceptible to injury.20,22
Although there is conflicting evidence in some studies, some reports have shown increased thickness or injury of collagen-rich tissues such as the Achilles tendon, the plantar fascia, the long head of the biceps tendon and supraspinatus tendon, fibrous contractures, and dense collagen matrix in the joint capsules.15,20,23 These changes, which leave tissues thick, stiff, and weak, contribute to systemic limited joint mobility and increased risk for the types of musculoskeletal disorders described above. The AGE-RAGE mechanism leads to increased production of reactive oxygen species, which can result in increased inflammation.19 This elevated inflammatory status from excessive AGEs and RAGEs in individuals with diabetes may manifest in complaints of pain.3,5,23,24 Recent articles5,23 have shown a direct relationship between levels of AGEs estimated in the skin (using skin intrinsic fluorescence) and shoulder impairments, pain, and disability.
Diabetes and its metabolic complications have a direct effect on skin, nerve, muscle, bone, and fat, which, in turn, affects musculoskeletal disorders in this population.9–24 Peripheral neuropathy occurs in up to 50% of patients with diabetes and causes muscle weakness and atrophy in the foot and ankle muscles.25–27 Indeed, some evidence indicates that elevated AGEs may be a common mechanism of both limited joint mobility and neuropathy.28,29 Peripheral neuropathy can result in a profound infiltration of adipose tissue between the muscle fibers known as intermuscular adipose tissue. This pathological adipose tissue may have detrimental effects beyond the obvious loss of lean muscle tissue and has been associated with substantial weakness, foot deformity, and loss of physical function.25–27 Even apart from peripheral neuropathy, obesity and diabetes can negatively affect muscle and muscle function, with increased fat infiltration and reduced ability to generate force (ie, decreased strength).30,31 These sarcopenic changes, which also have been associated with high AGE and RAGE levels, can result in reduced ability to generate force and likely impair basic mobility functions such as stair climbing and even walking.30–32
Implications
A primary implication from this point of view is that all physical therapists and rehabilitation specialists should be aware that their patients with diabetes, especially those with a duration of 10 years or more or in poor glycemic control, likely have one or more musculoskeletal complications. Clinicians should be aware that metabolic disorders such as diabetes are associated with elevated levels of AGEs or RAGEs that can make tissues less tolerant of physical stress. In other words, these metabolic by-products, which are known to make tissues thicker, stiffer, and weaker,20 can be a physiological factor that likely lowers the threshold of tissue injury.33 Therefore, at the same level of stress, these tissues with a higher saturation of glycated by-products likely will be injured more easily than tissues with low AGE levels, hence the higher incidence of musculoskeletal disorders in people with diabetes.
Patients with diabetes should be educated that not only is good control of their blood glucose levels important to minimize complications such as cardiovascular disease and peripheral neuropathy,34 but it also is likely critical to help minimize musculoskeletal complications. I believe that physical therapists should routinely ask their patients with diabetes to identify their most recent hemoglobin A1c value. Hemoglobin A1c reflects average glycemia over several months and has strong predictive value for diabetes complications. The current hemoglobin A1c target fostered by the American Diabetes Association for adults with diabetes who are not pregnant is <7.0% (53 mmol/mol).35 Patients with hemoglobin A1c values considerably higher (ie, >8.0) can be encouraged to follow up with their physician for management. Given that tailored and appropriate exercise is critical for proper management of diabetes34 and that physical therapists are experts at exercise in pathological conditions, especially in people with musculoskeletal impairments, physical therapists are in an optimal position to help this growing population manage their chronic disease, its complications, and subsequent movement impairments.
Additional research is needed to better understand the links among diabetes, elevated glucose levels, AGE and RAGE levels, neuropathy, musculoskeletal impairments, and movement impairments and what can be done to minimize these musculoskeletal complications. Investigations in this area have been challenging, perhaps because other complications of diabetes have been viewed as more life-threatening and perhaps more important. Indeed, complications such as cardiovascular disease deserve full attention due to the heightened risk of stroke or myocardial infarction. However, complications affecting the joints and muscles and leading to musculoskeletal disorders and reduced physical mobility represent a substantial burden to morbidity and quality of life in this population. Research efforts are needed to better understand how (1) general aerobic, resistive, and flexibility exercises and (2) specific therapeutic, impairment-based interventions can help to reduce musculoskeletal complications in this high-risk population. Because a substantial portion of the underlying cause of these musculoskeletal complications appears to be systematic, the best treatment approaches to ensure long-term and sustainable benefits likely will need to include interdisciplinary, systemic interventions. From a rehabilitation and prevention standpoint, a complete intervention likely would include instruction on appropriate physical activity level and nutritional status. Additional research also is needed to better understand how pharmaceutical interventions may help to reduce AGE and RAGE levels and subsequent musculoskeletal complications.
In summary, people with diabetes are at elevated risk of developing musculoskeletal impairments. Health care practitioners should be aware that this metabolic disorder can make their patients more susceptible to musculoskeletal injury and, in some situations, less responsive to treatment. The incidence of shoulder and hand problems is particularly elevated in people with diabetes, but essentially all musculoskeletal disorders appear to be more frequently seen in this population compared with those without diabetes. Additional research is needed to understand the links between these musculoskeletal impairments and what can be done to manage and even prevent them from occurring.
Footnotes
The author thanks Dr David Sinacore and Dr Mary Hastings for their review and suggestions for the final version of the manuscript.
The author acknowledges funding related to this work from the National Institutes of Health, National Institute of Diabetes and Digestive and Kidney Diseases, grant 5 R21 DK100793.
References
- 1. American Diabetes Association. Statistics about diabetes. 2016. Available at: http://www.diabetes.org/diabetes-basics/statistics/ Accessed June 17, 2016.
- 2. Lebiedz-Odrobina D, Kay J. Rheumatic manifestations of diabetes mellitus. Rheum Dis Clin North Am. 2010;36:681–699. [DOI] [PubMed] [Google Scholar]
- 3. Molsted S, Tribler J, Snorgaard O. Musculoskeletal pain in patients with type 2 diabetes. Diabetes Res Clin Pract. 2012;96:135–140. [DOI] [PubMed] [Google Scholar]
- 4. Kirkness CS, Marcus RL, Lastayo PC, et al. Diabetes and associated risk factors in patients referred for physical therapy in a national primary care electronic medical record database. Phys Ther. 2008;88:1408–1416. [DOI] [PubMed] [Google Scholar]
- 5. Larkin ME, Barnie A, Braffett BH, et al. Musculoskeletal complications in type 1 diabetes. Diabetes Care. 2014;37:1863–1869. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6. Rosenbloom AI, Silverstein J, Lezotte DC, et al. Limited joint mobility in childhood diabetes mellitus indicates increased risk for microvascular disease. N Engl J Med. 1981;305:191–194. [DOI] [PubMed] [Google Scholar]
- 7. Shah KM, Clark BR, McGill JB, Mueller MJ. Upper extremity impairments, pain and disability in patients with diabetes mellitus. Physiotherapy. 2015;101:147–154. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8. Mustafa KN, Khader YS, Bsoul AK, Ajlouni K. Musculoskeletal disorders of the hand in type 2 diabetes mellitus: prevalence and its associated factors. Int J Rheum Dis. 2016;19:730–735. [DOI] [PubMed] [Google Scholar]
- 9. Mueller MJ, Diamond JE, Delitto A, Sinacore DR. Insensitivity, limited joint mobility, and plantar ulcers in patients with diabetes mellitus. Phys Ther. 1989;69:453–459. [DOI] [PubMed] [Google Scholar]
- 10. Delbridge L, Perry P, Marr S, et al. Limited joint mobility in the diabetic foot: relationship to neuropathic ulceration. Diabet Med. 1988;5:333–337. [DOI] [PubMed] [Google Scholar]
- 11. Cheuy VA, Hastings MK, Mueller MJ. Metatarsophalangeal hyperextension movement pattern related to diabetic forefoot deformity. Phys Ther. 2016;96:1143–1151. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12. Klaesner JW, Hastings MK, Zou DQ, et al. Plantar tissue stiffness in patients with diabetes mellitus and peripheral neuropathy. Arch Phys Med Rehabil. 2002;83:1796–1801. [DOI] [PubMed] [Google Scholar]
- 13. Boulton AJ, Armstrong DG, Albert SF, et al. Comprehensive foot examination and risk assessment: a report of the Task Force of the Foot Care Interest Group of the American Diabetes Association, with endorsement by the American Association of Clinical Endocrinologists [reprint]. Phys Ther. 2008;88:1436–1443. [DOI] [PubMed] [Google Scholar]
- 14. Shah KM, Ruth CB, McGill JB, et al. Shoulder limited joint mobility in people with diabetes mellitus. Clin Biomech (Bristol, Avon). 2015;30:308–313. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15. Abate M, Schiavone C, Pelotti P, Salini V. Limited joint mobility (LJM) in elderly subjects with type II diabetes mellitus. Arch Gerontol Geriatr. 2011;53:135–140. [DOI] [PubMed] [Google Scholar]
- 16. Milgrom C, Novack V, Weil Y, et al. Risk factors for idiopathic frozen shoulder. Isr Med Assoc J. 2008;10:361–364. [PubMed] [Google Scholar]
- 17. Brownlee M. Glycation products and the pathogenesis of diabetic complications. Diabetes Care. 1992;15:1835–1843. [DOI] [PubMed] [Google Scholar]
- 18. Schnider SL, Kohn RR. Glucosylation of human collagen in aging and diabetes mellitus. J Clin Invest. 1980;66:1179–1181. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19. Ramasamy R, Vannucci SJ, Yan SS, et al. Advanced glycation end products and RAGE: a common thread in aging, diabetes, neurodegeneration, and inflammation. Glycobiology. 2005;15:16R–28R. [DOI] [PubMed] [Google Scholar]
- 20. Reddy GK. Cross-linking in collagen by nonenzymatic glycation increases the matrix stiffness in rabbit achilles tendon. Exp Diabesity Res. 2004;5:143–153. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21. Haus JM, Carrithers JA, Trappe SW, Trappe TA. Collagen, cross-linking, and advanced glycation end products in aging human skeletal muscle. J Appl Physiol (1985). 2007;103:2068–2076. [DOI] [PubMed] [Google Scholar]
- 22. Tang SY, Vashishth D. Non-enzymatic glycation alters microdamage formation in human cancellous bone. Bone. 2010;46:148–154. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23. Shah KM, Clark BR, McGill JB, et al. Relationship between skin intrinsic fluorescence—an indicator of advanced glycation end products—and upper extremity impairments in individuals with diabetes mellitus. Phys Ther. 2015;95:1111–1119. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24. Yan SF, Ramasamy R, Schmidt AM. Mechanisms of disease: advanced glycation end-products and their receptor in inflammation and diabetes complications. Nat Clin Pract Endocrinol Metab. 2008;4:285–293. [DOI] [PubMed] [Google Scholar]
- 25. Hilton TN, Tuttle LJ, Bohnert KL, et al. Excessive adipose tissue infiltration in skeletal muscle in individuals with obesity, diabetes mellitus, and peripheral neuropathy: association with performance and function. Phys Ther. 2008;88:1336–1344. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26. Tuttle LJ, Sinacore DR, Cade WT, Mueller MJ. Lower physical activity is associated with higher intermuscular adipose tissue in people with type 2 diabetes and peripheral neuropathy. Phys Ther. 2011;91:923–930. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27. Cheuy VA, Hastings MK, Commean PK, et al. Intrinsic foot muscle deterioration is associated with metatarsophalangeal joint angle in people with diabetes and neuropathy. Clin Biomech (Bristol, Avon). 2013;28:1055–1060. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28. Conway BN, Aroda VR, Maynard JD, et al. Skin intrinsic fluorescence correlates with autonomic and distal symmetrical polyneuropathy in individuals with type 1 diabetes. Diabetes Care. 2011;34:1000–1005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29. Monnier VM, Sell DR, Genuth S. Glycation products as markers and predictors of the progression of diabetic complications. Ann NY Acad Sci. 2005;1043:567–581. [DOI] [PubMed] [Google Scholar]
- 30. Bittel DC, Bittel AJ, Tuttle LJ, et al. Adipose tissue content, muscle performance and physical function in obese adults with type 2 diabetes mellitus and peripheral neuropathy. J Diabetes Complications. 2015;29:250–257. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31. Almurdhi MM, Reeves ND, Bowling FL, et al. Reduced lower-limb muscle strength and volume in patients with type 2 diabetes in relation to neuropathy, intramuscular fat, and vitamin D levels. Diabetes Care. 2016;39:441–447. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32. Semba RD, Bandinelli S, Sun K, et al. Relationship of an advanced glycation end product, plasma carboxymethyl-lysine, with slow walking speed in older adults: the InCHIANTI study. Eur J Appl Physiol. 2010;108:191–195. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33. Mueller MJ, Maluf KS. Tissue adaptation to physical stress: a proposed “Physical Stress Theory” to guide physical therapist practice, education, and research. Phys Ther. 2002;82:383–403. [PubMed] [Google Scholar]
- 34. Colberg SR, Sigal RJ, Fernhall B, et al. Exercise and type 2 diabetes: the American College of Sports Medicine and the American Diabetes Association: joint position statement. Diabetes Care. 2010;33:e147–e167. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35. American Diabetes Association. 5: glycemic targets. Diabetes Care. 2016;39(suppl 1):S39–S46. [DOI] [PubMed] [Google Scholar]