Aortic stenosis (AS) has become a leading cause of morbidity and mortality among a growing population of older adults.[1] The number of elderly patients with severe symptomatic AS requiring aortic valve replacement has been significantly increasing in recent years. Latest echocardiographic research in USA showed the rate of severe AS in patients older than 75 years as 2.8%.[2] The mortality rate of patients with severe AS who are not surgical candidates has been shown to be 68% in two years.[3] Although the gold standard approach to severe AS is surgical treatment, approximately 30% of patients were not referred to surgery due to the advanced age, left ventricular dysfunction, and/or significant multiple comorbidities.[4] Therefore, transcatheter aortic valve implantation (TAVI) has emerged as a treatment option for elderly inoperable or high surgical risk patients with severe AS.[5],[6] However, can TAVI be trusted as a safe and effective alternate to surgical management in very elderly (age > 100 years) patients?
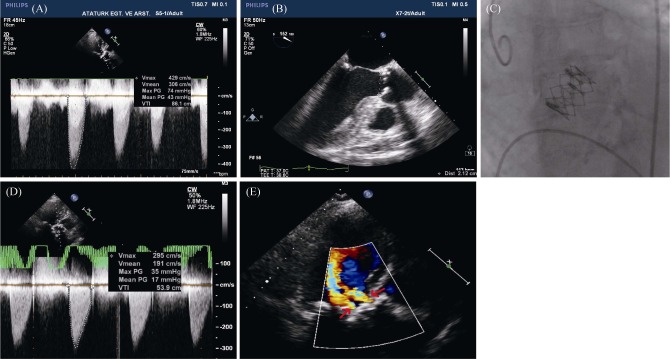
A 102-year-old female patient with progressive dyspnea and chronic obstructive pulmonary disease (COPD) was consulted to our department due to development of acute palpitation. Electrocardiogram revealed atrial fibrillation with a rate of 145 beats/min. Transthoracic echocardiography (TTE) revealed left ventricular (LV) global hypokinesia with an ejection fraction of 40%, concentric LV hypertrophy, severe AS (mean gradient 43 mmHg, aortic valve area: 0.5 cm2) (Figure 1A), moderate to severe tricuspid regurgitation (TR) and severe pulmonary hypertension (PHT) [systolic pulmonary artery pressure (sPAP): 60 mmHg]. The patient was admitted to our coronary intensive care unit. The other co-morbidities at this time included severe COPD [FEV1/FVC (forced expiratory volume in one second/forced vital capacity): 40%] and chronic renal failure stage 3 (estimated glomerular filtration rate: 46 mL/min per 1.73 m2). Coronary angiography demonstrated diffuse calcification of coronary arteries without significant stenosis. The patient's calculated logistic EuroSCORE was 79% and Society of Thoracic Surgeons (STS) score was 14%. Her Duke Activity Status Index (DASI) was 1.75 due to the severe respiratory insufficiency. We have learned from the relatives of the patient that the patient had a good cognitive function and living without any care assistant until one month ago.
Figure 1. Pre-procedural evaluation of aortic valve anatomy and transvalvular gradient.
(A): Apical 5-chamber transthoracic continuous wave Doppler analysis showing a mean gradient of 43 mmHg; (B): transesophageal echocardiography end-systolic mid-esophageal atrioventricular long-axis view showing bulky calcification and annulus diameter as 21 mm; (C): peri-procedural fluoroscopic image of a successfully deployed Edwards Sapien XT valve; (D) follow-up transthoracic Doppler echocardiography at four years follow-up with 5-chamber continuous wave Doppler analysis showing a mean gradient of 17 mmHg; and (E) mild bilateral paravalvular aortic regurgitation (arrows) at parasternal long axis view.
The heart team evaluated the patient and decided to proceed with TAVI based on high surgical risk scores and patient's co-morbid illnesses. For an accurate measurement of annular dimension and evaluation of aortic valve anatomy, transesophageal echocardiography was performed and determined the annulus diameter as 21 mm (Figure 1B). Then, the patient was taken to the catheterization laboratory and successful deployment of a 23 mm Edwards Sapien XT valve (Edwards Lifesciences, Irvine, CA, USA) was performed under general anesthesia using a transfemoral approach (Figure 1C). This led to a marked improvement of the transvalvular gradient with only mild paravalvular AR. Thereafter, the patient was taken to the coronary intensive care unit and extubated 12 h after the procedure. Before the hospital discharge, echocardiography showed functional aortic bioprosthetic valve (mean gradient 18 mmHg and aortic valve area 1.7 cm2), mild paravalvular AR, moderate tricuspid regurgitation, moderate PHT (sPAP: 50 mmHg) and near normal ejection fraction (50%).
Electrocardiogram revealed normal sinus rhythm with a ventricular rate of 80 beats/min. Atrial fibrillation was also detected to be resolved after TAVI. She has stayed in the coronary intensive care unit service for three days, and then taken to the cardiology service. After follow up for a total of 13 days, she was discharged without any complications. She has been followed for four years clinically and with TTE (Table 1), and now her DASI is 15.45. She lives with her daughter and need no assistance in her daily life. Her functional capacity is very good [New York Heart Association (NYHA) class 1-2] despite the presence of severe gonarthrosis and osteolysis. The last TTE performed at March 2016 revealed normal LV ejection fraction (65%), functional aortic valve bio-prosthesis [mean gradient: 17 mmHg, aortic valve area (AVA): 1.7 cm2] (Figure 1D), mild paravalvular AR (Figure 1E), mild mitral stenosis (mean gradient: 4 mmHg), mild tricuspid regurgitation and mild PHT (sPAB: 40 mmHg). Even though post-procedural complications of TAVI occur more frequently in patients with advanced age and high surgical risk score, there were no complications in our patient. And currently, the patient is able to perform her daily activities with no care assistant.
Table 1. The pre-procedural, post-procedural and follow up echocardiographic parameters.
| Parameters | Time of echocardiography |
||||||
| Pre-TAVI | Post-TAVI | 2012 | 2013 | 2014 | 2015 | 2016 | |
| AVA, cm2 | 0.5 | 1.7 | 1.8 | 1.7 | 1.8 | 1.7 | 1.7 |
| LV/Ao peak gradient, mmHg | 74 | 35 | 36 | 35 | 36 | 37 | 35 |
| LV/Ao mean gradient, mmHg | 43 | 18 | 18 | 17 | 17 | 18 | 17 |
| AR, grade | 1 | 1 | 1 | 1 | 1 | 1 | 1 |
| MR, grade | 2 | 1 | 1 | 1 | Trivial | Trivial | Trivial |
| TR, grade | 3-4 | 2 | 2 | 2 | 1 | 1 | 1 |
| sPAP, mmHg | 60 | 50 | 50 | 45 | 40 | 40 | 40 |
| LVEF, % | 40 | 50 | 55 | 60 | 65 | 65 | 65 |
| LVEDD, cm | 4.5 | 4.4 | 4.4 | 4.2 | 4.2 | 4.2 | 4.1 |
| LVESD, cm | 2.8 | 2.7 | 2.7 | 2.4 | 2.4 | 2.4 | 2.5 |
| IVSDD, cm | 1.4 | 1.4 | 1.4 | 1.4 | 1.3 | 1.3 | 1.3 |
| PWDD, cm | 1.3 | 1.3 | 1.2 | 1.2 | 1.2 | 1.2 | 1.2 |
Ao: aorta; AR: aortic regurgitation; AVA: aortic valve area (calculated from continuity equation); IVSDD: interventricular septum diastolic diameter; LV: left ventricular; LVEDD: left ventricular end-diastolic diameter; LVEF: left ventricular ejection fraction (as measured by Biplane Simpson's method); LVESD: left ventricular end-systolic diameter; MR: mitral regurgitation; PWDD: posterior wall diastolic diameter; sPAP: systolic pulmonary artery pressure; TAVI: transcatheter aortic valve implantation; TR: tricuspid regurgitation.
TAVI is a miracle treatment for inoperable patients with severe AS due to advanced age and comorbidities. However, as the geriatric population is increasingly growing in the Western countries, there is an increasing challenge to assess the appropriate management of cardiovascular morbidities in the very elderly, especially when considering invasive therapies over medical therapies. In a Swedish study, 734 patients were randomized (136 patients were older than 90 years), and comparison of outcomes of TAVI in patients ≥ 90 years versus < 90 years indicated that performing balloon-expandable TAVI in nonagenarians (> 90 years) is feasible and safe.[7] Nonagenarians were found to have several significantly different co-morbidities compared to younger patients. They stated high device success rate in both age groups and similar 30-day and 1-year survival, short-term major complication rates, and NYHA functional capacity improvement. Nonagenarians had significantly higher rates of minor vascular complications.
In another study, Yamamoto, et al.,[8] compared the clinical outcomes of TAVI in patients ≤ 90 years old to patients ≥ 90 years old and found similar procedural success in both groups. Although 30-day and 6-month mortality trended to be higher in patients older than 90 years old, the differences in mortality rates were statistically insignificant (6% vs. 15%, P = 0.22; and 14% vs. 27%, P = 0.14, respectively). Moreover, the cumulative survival after 13.4 ± 8.0 months of follow-up was comparable between both groups (P = 0.22). Jabs, et al.,[9] have reported their experience with a 99 year old AS patient who underwent TAVI using CoreValve aortic bioprosthesis after presenting with syncope and progressive dyspnea. Following TAVI, AVA improved from 0.6 cm2 to 1.5 cm2 and the patient was discharged to a geriatric rehabilitation unit two days after the procedure. For the next four years, the patient remained independent, with mild exertional dyspnea, and without recurrent syncopes. However, our case is older than this patient and to the best of our knowledge, we have presented the oldest patient to have treated with transfemoral TAVI using Edwards Sapien XT bioprosthesis who is currently living in a good functional status at the age of 106 years. Although at initial evaluation, we were not disposed to perform TAVI due to the advanced age and presence of severe co-morbid diseases (e.g., severe PHT, severe COPD and atrial fibrillation) that increases mortality rate too much, the heart team suggested TAVI. Ultimately, the patient underwent TAVI and she is still very good without any complaint of dyspnea or tachycardia. Moreover, we realized and surprised about that both the transvalvular gradient and the grade of paravalvular AR had not changed even in a mild fashion within four years. This may also give a clue about the durability of the valve. Therefore, TAVI may be beneficial and tolerable in very old patients who suffer from severe AS.
References
- 1.Osnabrugge RL, Mylotte D, Head SJ, et al. Aortic stenosis in the elderly: disease prevalence and number of candidates for transcatheter aortic valve replacement: a meta-analysis and modeling study. J Am Coll Cardiol. 2013;62:1002–1012. doi: 10.1016/j.jacc.2013.05.015. [DOI] [PubMed] [Google Scholar]
- 2.Nkomo VT, Gardin JM, Skelton TN, et al. Burden of valvular heart diseases: a population-based study. Lancet. 2006;368:1005–1011. doi: 10.1016/S0140-6736(06)69208-8. [DOI] [PubMed] [Google Scholar]
- 3.Makkar RR, Fontana GP, Jilaihawi H, et al. Transcatheter aortic-valve replacement for inoperable severe aortic stenosis. N Engl J Med. 2012;366:1696–1704. doi: 10.1056/NEJMoa1202277. [DOI] [PubMed] [Google Scholar]
- 4.Iung B, Cachier A, Baron G, et al. Decisionmaking in elderly patients with severe aortic stenosis: why are so many denied surgery? Eur Heart J. 2005;26:2714–2720. doi: 10.1093/eurheartj/ehi471. [DOI] [PubMed] [Google Scholar]
- 5.Leon MB, Smith CR, Mack M, et al. Transcatheter aortic-valve implantation for aortic stenosis in patients who cannot undergo surgery. N Engl J Med. 2010;363:1597–1607. doi: 10.1056/NEJMoa1008232. [DOI] [PubMed] [Google Scholar]
- 6.Smith CR, Leon MB, Mack MJ, et al. PARTNER Trial Investigators. Transcatheter versus surgical aorticvalve replacement in high-risk patients. N Engl J Med. 2011;364:2187–2198. doi: 10.1056/NEJMoa1103510. [DOI] [PubMed] [Google Scholar]
- 7.Abramowitz Y, Chakravarty T, Jilaihawi H, et al. Comparison of outcomes of transcatheter aortic valve implantation in patients ≥ 90 years versus < 90 years. Am J Cardiol. 2015;116:1110–1115. doi: 10.1016/j.amjcard.2015.06.033. [DOI] [PubMed] [Google Scholar]
- 8.Yamamoto M, Meguro K, Mouillet G, et al. Comparison of effectiveness and safety of transcatheter aortic valve implantation in patients aged ≥ 90 years versus < 90 years. Am J Cardiol. 2012;110:1156–1163. doi: 10.1016/j.amjcard.2012.05.058. [DOI] [PubMed] [Google Scholar]
- 9.Jabs A, Kilic T, Schnelle N, et al. Transcatheter aortic valve implantation and four-year follow up in a 99-year-old patient. J Heart Valve Dis. 2013;22:261–264. [PubMed] [Google Scholar]