Abstract
A significant cohort of patients is plagued by postoperative rotational instability after the anatomic anterior cruciate ligament (ACL) reconstruction surgery. Anatomic anterolateral ligament (ALL) reconstruction was performed in this study with the aim to assess the clinical role of ALL in knee’s stability and joint functions. Sixty patients were recruited and divided into three groups to perform the operations of anatomic single-bundle ACL reconstruction, anatomic double-bundle ACL reconstruction, and anatomic single-bundle ACL reconstruction + anterolateral ligament reconstruction, respectively. And then postoperative knee’s stability and joint functions were evaluated to compare the clinical outcomes among the three different kind of operations. The postoperative knee’s stability and joint functions of the anatomic double-bundle ACL reconstruction group and the anatomic single-bundle ACL reconstruction + ALL reconstruction group were better than the anatomic single-bundle ACL reconstruction group. No significant difference was observed between the anatomic double-bundle ACL reconstruction group and the anatomic single-bundle ACL reconstruction + ALL reconstruction group. The anatomic anterolateral ligament reconstruction could improve the clinical outcomes after patients performed the anatomic single-bundle anterior cruciate ligament reconstruction. This indicates that the anterolateral ligament plays a crucial role in knee’s stability and joint function, especially the rotational stability.
Key points.
Anatomic anterolateral ligament reconstruction combined with anatomic anterior cruciate ligament reconstruction was performed to treat the patients with ACL rupture.
Compared to the anatomic single-bundle ACL reconstruction group, the anatomic single-bundle ACL reconstruction + ALL reconstruction group achieve a better clinical outcomes.
The results suggest that the anterolateral ligament plays a crucial role in knee’s stability and joint function, especially the rotational stability.
Key words: Anterolateral ligament, anterior cruciate ligament, anatomic reconstruction, clinical outcomes
Introduction
Currently, there are mainly two technologies of beam reconstruction for the anterior cruciate ligament (ACL), single-bundle reconstruction and double-bundle reconstruction (Budny et al., 2016; Lorenz et al., 2007; Petersen et al., 2013). Because studies have shown that the isometric reconstruction technique couldn’t offer sufficient rotational stability for knee joint and may even result in early knee osteoarthritis, single-bundle reconstruction technique evolved from the isometric reconstruction to the anatomic reconstruction (van Eck et al., 2011). However, the clinical outcomes of anatomic single-bundle reconstruction are still far from excellent. Thus, the proposition of anatomic double-bundle reconstruction technique stems from a better understanding to the anatomy of anterior cruciate ligament. Based on their tibial attachment sites, the anterior cruciate ligament is divided into two functional bundles-the anteromedial (AM) and posterolateral (PL) (Franceschi et al., 2002). Between them, the anteromedial bundle mainly provides the anteroposterior stability. And the posterolateral bundle mainly provides the rotational stability (Amis 2012).
Over the years, biomechanical, clinical research and evidence-based medicine showed that the anatomic double-bundle reconstruction achieved a better restoration for the kinematic character of normal knee compared with the anatomic single-bundle reconstruction, especially the rotational stability (Mascarenhas et al., 2015; Plaweski et al., 2011; Sun et al., 2015; Zhu et al., 2013). But both the clinical outcomes and the risk of graft failure were equivalent (Kondo et al., 2010). Some scholars concluded that two kinds of reconstruction techniques obtained no significant difference in knee’s stability aspect through the biomechanical study of cadaveric knees (Goldsmith et al., 2013). There were even clinical studies showed that both the anatomic single-bundle and double-bundle ACL reconstruction could restore the joint functions and knee’s stability very well. However, the high incidences of medial patellar-femoral cartilage damage and poor PL status may occur in anatomic double-bundle reconstruction (Xu et al., 2014).
With the further deepen understanding of anterolateral ligament (ALL), some scholars believed that reconstructing this structure could improve the knee’s rotational stability effectively (Bonasia et al., 2015; Pomajzl et al., 2015; Sonnery-Cottet et al., 2015; Smith et al., 2015). Through the biomechanical study of ten cadaveric knees, Nitri et al demonstrated that reconstructing the ACL and ALL simultaneously could restore a better rotational stability compared to the isolated ACL reconstruction (Nitri et al., 2016). However, there are no clinical reports about the comprehensive comparision among the anatomic single-bundle ACL reconstruction, anatomic double-bundle ACL reconstruction, and anatomic single-bundle ACL reconstruction + anterolateral ligament reconstruction.
In this paper, sixty cases of patients with simple anterior cruciate ligament rupture were recruited to perform the operations of anatomic single-bundle ACL reconstruction, anatomic double-bundle ACL reconstruction, and anatomic single-bundle ACL reconstruction + anterolateral ligament reconstruction. All the patients received the same post-operative rehabilitation programs. In addition, post-operative knee’s stability and joint functions were evaluated to compare the clinical outcomes among the three different kinds of operations, with the aim to offer clinical reference for the choice of surgical approaches.
Methods
Experimental participants
This study was approved by the ethics committee of Chongqing Medical University and has therefore been performed in accordance with the ethical standards laid down in the 1964 Declaration of Helsinki. Written informed consent was obtained from all individuals participants included in the study. From July 2012 to July 2015, 60 cases of patients with simple anterior cruciate ligament rupture (mean age, 26.2 years; range 18 to 41 years) were collected to perform a prospective clinical study, in which 39 males and 21 females. The time from injury to surgery was one month to five years, an average of 1.3 years. There were no demographic differences among three groups as presented in Table 1. The inclusive criteria of experimental subjects were that all patients were non-professional athletes and non-heavy manual workers with sports injury or injury caused by light violence in daily life. The exclusive criteria of experimental subjects were that patients with multiple ligament injury, meniscus injury cartilaginous injury, severe osteoarthritis or fractures. All surgical operations were completed by one surgeon using the standardized surgical protocol.
Table 1.
Comparisons of demographic data among three groups.
| SB (n = 20) |
DB (n = 20) |
SBL (n = 20) |
Statistics | P value |
|
|---|---|---|---|---|---|
| Age (years) | 22.3 ± 5.3 | 28.3 ± 6.1 | 26.3 ± 6.8 | F=1.87 | .1649 |
| Gender (M/F) | 13/7 | 14/6 | 12/8 | χ²=0.44 | .8027 |
| BMI | 23.2 ± 3.1 | 24.8 ± 5.1 | 25.2 ± 4.1 | F=0.25 | .7809 |
| Time from injury to surgery (months) | 12.3 ± 4.3 | 14.2 ± 4.6 | 16.3 ± 3.6 | F=0.86 | .4302 |
SB: anatomic single-bundle ACL reconstruction group, DB: anatomic double-bundle ACL reconstruction group, SBL: anatomic single-bundle ACL reconstruction + ALL reconstruction group, M/F: Male/Female, BMI: Body Mass Index
All patients received conventional X-ray (antero-posterior and lateral views, patellar axial view) to exclude obvious fractures and assess the patellofemoral joint. In addition, X-ray of full length of lower extremities was performed to determine the limb alignment, to insure that the malalignment of all the knees was less than 10 degree. Three-dimensional CT was taken for all patients before the operation to determine the height and width of fossa intercondyloidea, the height of lateral intercondylar barren, the sizes of ACL femoral and tibial footprint, and the degree of ACL femoral footprint. The sizes of ACL femoral and tibial footprint included the longest diameter of ACL footprints, the width of anteromedial and posterolateral bundle.
Arthroscopic surgery was performed to confirm the parameters determined by 3D CT. Patients meeting the following conditions were included into anatomic double-bundle ACL reconstruction group (DB group, n = 20). The longest diameter of ACL femoral and tibial footprint was equal or greater than 14 mm. The width of fossa intercondyloidea was greater than 15 mm. The height of fossa intercondyloidea was greater than 19 mm. Grafts were enough. Other patients were performed the anatomic single-bundle ACL reconstruction and were divided into two groups: anatomic single-bundle ACL reconstruction group (SB group, n = 20) and anatomic single-bundle ACL reconstruction + ALL reconstruction group (SBL group, n = 20). Preoperative examinations, including Anterior drawer test, Lachman test, Pivot-shift test were carried out for all patients. Most patients were identified as grade II of Lachman test and grade I of Pivot-shift test. In addition, 3.0 T MRI was performed to assist in the diagnosis of ACL and ALL injury, to determine the anteroposterior diameter of ACL tibial footprint and the degree of ACL tibial footprint. Three measurement methods were displayed in Figure 1.
Figure 1.
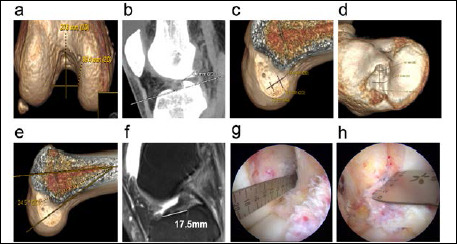
The parameters determined by 3D CT, MRI, and Arthroscopic. a refer to the height and width of fossa intercondyloidea, b refer to the height of lateral intercondylar barren, c refer to the size of ACL femoral footprint, d refer to the size of ACL tibial footprint, e refer to the degree of ACL femoral footprint, f refer to the anteroposterior diameter of ACL tibial footprint, g refer to the length of ACL femoral footprint, h refer to the width of fossa intercondyloidea
Technical note
High anterolateral portal (LP) was established for arthroscopic examination to confirm the ACL rupture, to clean the ruptured ACL and to properly preserve the tibial remanent of ACL (generally 3-5mm). And then central anteromedial protal (CP) and accessory anteromedial protal (AMP) were established (Araujo et al., 2011). Measurement ruler was put into articular cavity to determine the height and width of fossa intercondyloidea, the height of lateral intercondylar barren, the sizes of ACL femoral and tibial footprint, including the longest diameter of ACL footprints, the width of anteromedial and posterolateral bundle. The single-bundle or double-bundle ACL reconstructions were determined based on these measurement results. The semitendinosus and gracilis tendons were exposed, separated and harvested. The semitendinosus tendon was used for the graft of anteriormedial bundle. The gracilis tendon was used for the graft of posteriorlateral bundle. Grafts were prepared before the operation.
Anatomic single-bundle ACL reconstruction
Plasma knife marked the center of ACL femoral footprint. Femoral offset guider was placed with the knee at 120 degree of flexion. Guide needle with a tail hole was drilled into the footprint center and pierced through the anterolateral knee. 4.5 mm diameter hollow drill was used to drill the tunnel and measure the length of tunnel. The appropriate length of suspensory titanium plate was chosen. Graft was pulled through the loop of suspensory titanium plate. Guidewire was installed for spare. Femoral tunnel was drilled by the hollow drill with the same diameter of graft. Tibial tunnel guider was used to locate the center of ACL tibial footprint with the knee at 90 degree of flexion. Tibial tunnel was also drilled by the hollow drill with the same diameter of graft. Guidewire was installed to pull into the graft. And then the suspensory titanium plate was inverted. The graft tendon was tensioned and tested the impingement. Twenty repeated flexion and extension of knee were performed. Bio-absorbable interference screw in conjugation was utilized in tibial side with the knee at 30 degree of flexion. Toothed washer was used to fix the residual tendon in the vicinity of the distal tibial tunnel.
Anatomic double-bundle ACL reconstruction
Plasma knife marked the two bundles center of ACL femoral and tibial footprints. Femoral offset guider was placed with the knee at 120 degree of flexion. Tibial offset guider was placed with the knee at 90 degree of flexion. Anteromedial femoral and tibial tunnels were established. And then femoral and tibial double-bundle guiders were installed to establish the posterolateral tunnel. Posterolateral graft was first put through the PL tunnel and anteromedial passage was followed through the AM tunnel. The graft tendon was tensioned and tested the impingement. Twenty repeated flexion and extension of knee were performed. Anteromedial bundle was fixed by the interference screw with the knee at 30 degree of flexion. Posterolateral bundle was fixed by the interference screw with the knee in full extension. Toothed washer was used to fix the residual tendon in the vicinity of the distal tibial tunnel.
Anatomic single-bundle ACL reconstruction + ALL reconstruction
The procedure of single-bundle ACL reconstruction was the same as described above. The iliotibial band tendon was harvested for the graft of anterolateral ligament. Graft preparation was made before the operation. In our previous anatomic study of twenty Asian cadaveric knees, we confirm that the anterolateral ligament is started at the prominence of the lateral femoral epicondyle, slightly anterior to the origin of the lateral collateral ligament. And it ends at the anterolateral aspect of the proximal tibia articular surface, located at the position beyond the joint line 0.8-1.0 cm with equal distance to the Gerdy’s tubercle and the outermost point of the fibular head. Subcutaneous tunnel from the femoral side to tibial side of the anterolateral ligament was established for graft through. Guide needle with a tail hole was drilled into the femoral side and tibial side of anterolateral ligament. Non-absorbable suture was fixed on the two guide needles, with the aim to test the isometric resistance. Graft was pulled into the femoral and tibial tunnels through subcutaneous tunnel. Interference screw was used to fix the femoral side of anterolateral ligament. And then the crus was maintained at posterior drawer test position. The ACL tibial side of graft was fixed by interference screw firstly. With the knee at 30 degree of flexion, the ALL tibial side of graft was fixed by interference screw with the crus at externally rotated position. The process of anatomic ALL reconstruction was displayed in Figure 2.
Figure 2.
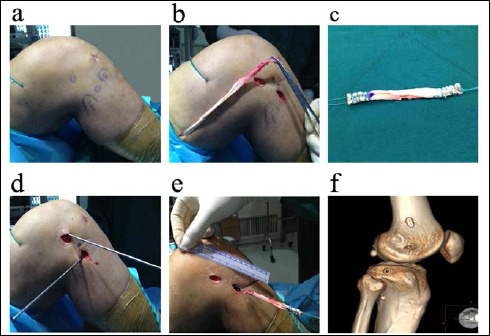
The procedure of anterolateral ligament reconstruction. a: label the bony landmarks, b: harvest the iliotibial band tendon, c: graft preparation, d: establish the femoral and tibial tunnels, e: implant the graft, f: reexamine the femoral and tibial tunnels by 3D CT.
Postoperative rehabilitation
The standard postoperative rehabilitation programs were performed in three groups, including the strength training and the joint functional training. The knee’s all activities were kept in knee brace for one month. The range of motion was controlled in 0-90 degree within one month. Partial weight-bearing walk was allowed within one month with crutch. One month later, full weight-bearing walk was allowed with a kneepad. Swimming training was recommended in four weeks after the operation. Jogging was allowed in six months after the operation. Competitive sports were not allowed until one year later.
Assessment method
The anteroposterior stability of involved and normal knee in three groups were examined in 3, 6, and 12 months post-operatively, including the Anterior drawer test, Lachman test, and the stress radiography. Joint laxity test was evaluated by KT-2000. In addition, the rotational stability of involved and normal knee in three groups were examined in 3, 6, and 12 months post-operatively, including the pivot-shift test, Rotameter stress three-dimensional CT test. In the stress three-dimensional CT test, the imitative Rotameter equipment was used to make the knee at 30 degree of flexion, with the aim to maximum internal rotate the knee (Figure 3). Meanwhile knee function and overall sports level scores were also assessed in 3, 6, and 12 months post-operatively, including the Lysholm score, Tegner score, and IKDC subjective score.
Figure 3.

The rotational stability of involved and normal knee examined by the imitative Rotameter equipment in three-dimensional CT.
Statistical analysis
SAS 9.0 statistical software was employed for the statistical analysis. All data were performed the normal distribution test. If the data was normal distribution, it was presented as mean ± standard deviation (x ± S). If the data was not normal distribution, it was presented as median. The comparison of rate was performed the chi-square test. The comparison among three groups was performed the analysis of variance (ANOVA). Duncan test was applied in pairwise comparison between groups. The significance level was α =0.05.
Results
The operations of all patients were completed successfully. All patients were successfully followed up in 1, 2, 3, 6, and 12 months post-operatively. All patients were examined in 3, 6 and 12 months post-operatively.
The stability results of three groups were displayed in Table 2. From the stability perspective, both anteroposterior and rotational stabilities of anatomic double-bundle ACL reconstruction group and anatomic single-bundle ACL reconstruction + ALL reconstruction group were better than the anatomic single-bundle ACL reconstruction group. The difference was statistically significant (p < 0.05). However, no significant difference was observed between the anatomic double-bundle ACL reconstruction group and anatomic single-bundle ACL reconstruction + ALL reconstruction group (p > 0.05). The comparison of stability between DB and SBL group was manifested in Table 3.
Table 2.
The anteroposterior and rotational stability of involved knees from DB and SBL Stabilityreconstruction groups.
| Group | 3 months | Statistical test | 6 months | Statistical test | 12 months | Statistical test | |
|---|---|---|---|---|---|---|---|
|
Anterior drawer test Positive-Rate |
DB | 20% | χ²= 0.254 P= 0.613 |
20% | χ²= 0.254 P= 0.613 |
20% | χ²= 0.254 P= 0.613 |
| SBL | 25% | 25% | 25% | ||||
|
Lachman test Positive-Rate |
DB | 20% | χ²= 0.284 P= 0.593 |
20% | χ²= 0.284 P= 0.593 |
20% | χ²= 0.284 P= 0.593 |
| SBL | 25% | 25% | 25% | ||||
|
Stress radiography D-Value (I/N) |
DB | 4.4 ± 0.3 mm | Duncan n.s. |
4.8 ± 0.4 mm | Duncan n.s. |
5.1 ± 0.3 mm | Duncan n.s. |
| SBL | 4.6 ± 0. 3 mm | 5.0 ± 0.3 mm | 5.3 ± 0.4 mm | ||||
|
KT-2000 D-Value (I/N) |
DB | 3.8 ± 0.2 mm | Duncan n.s. |
3.9 ± 0.2 mm | Duncan n.s. |
3.2 ± 0.2 mm | Duncan n.s. |
| SBL | 4.0 ± 0.2 mm | 3.9 ± 0.2 mm | 3.4 ± 0.2 mm | ||||
|
Pivot-shift test Positive-Rate |
DB | 20% | χ²= 0 P= 1 |
20% | χ²= 0 P= 1 |
20% | χ²= 0 P= 1 |
| SBL | 20% | 20% | 20% | ||||
|
Rotameter D-Value (I/N) |
DB | 1.1 ± 0.2 mm | Duncan n.s. |
1.1 ± 0.2 mm | Duncan n.s. |
1.2 ± 0.2 mm | Duncan n.s. |
| SBL | 1.0 ± 0.2 mm | 1.0 ± 0.2 mm | 1.1 ± 0.2 mm |
DB: anatomic double-bundle ACL reconstruction group, SBL: anatomic single-bundle ACL reconstruction + ALL reconstruction group, D-Value: Difference-Value, I/N: Involved vs Normal, n.s.: no significance
Table 3.
The clinical outcomes of anteroposterior and rotational stability of involved knee from three groups.
| Stability | Group | 3 months | Statistical test | 6 months | Statistical test | 12 months | Statistical test |
|---|---|---|---|---|---|---|---|
|
Anterior drawer test Positive-Rate |
SB | 40% | χ²=6.050 P=0.049 |
40% | χ²=6.050 P=0.049 |
45% | χ²=9.251 P=0.010 |
| DB | 20% | 20% | 20% | ||||
| SBL | 25% | 25% | 25% | ||||
|
Lachman test Positive-Rate |
SB | 45% | χ²=7.741 P=0.021 |
45% | χ²=7.741 P=0.021 |
50% | χ²=10.622 P=0.005 |
| DB | 20% | 20% | 20% | ||||
| SBL | 25% | 25% | 25% | ||||
|
Stress radiography Difference-Value (Involved vs Normal) |
SB | 7.0 ± 0.4 mm | F=337.29 P<0.001 |
7.6 ± 0.4 mm | F=392.04 P<0.001 |
8.5 ± 0.4 mm | F=581.10 P<0.001 |
| DB | 4.4 ± 0.3 mm | 4.8 ± 0.4 mm | 5.1 ± 0.3 mm | ||||
| SBL | 4.6 ± 0.3 mm | 5.0 ± 0.3 mm | 5.3 ± 0.4 mm | ||||
|
KT-2000 Difference-Value (Involved vs Normal) |
SB | 6.0 ± 0.3 mm | F=454.02 P<0.001 |
6.5 ± 0.3 mm | F=593.4 P<0.001 |
7.1 ± 0.3 mm | F=1500.96 P<0.001 |
| DB | 3.8 ± 0.2 mm | 3.9 ± 0.2 mm | 3.2 ± 0.2 mm | ||||
| SBL | 4.0 ± 0.2 mm | 3.9 ± 0.2 mm | 3.4 ± 0.2 mm | ||||
|
Pivot-shift test Positive-Rate |
SB | 50% | χ²=12.224 P=0.002 |
50% | χ²=12.224 P=0.002 |
55% | χ²=16.396 P=0.001 |
| DB | 20% | 20% | 20% | ||||
| SBL | 20% | 20% | 20% | ||||
|
Rotameter Difference-Value (Involved vs Normal) |
SB | 5.2 ± 0.3 mm | F=1985.1 P<0.001 |
4.9 ± 0.3 mm | F=1941.2 P<0.001 |
6.1 ± 0.3 mm | F=3233.3 P<0.001 |
| DB | 1.1 ± 0.2 mm | 1.1 ± 0.2 mm | 1.2 ± 0.2 mm | ||||
| SBL | 1.0 ± 0.2 mm | 1.0 ± 0.2 mm | 1.1 ± 0.2 mm |
DB: anatomic double-bundle ACL reconstruction group, SB: anatomic single-bundle ACL reconstruction, SBL: anatomic single-bundle ACL reconstruction + ALL reconstruction group.
The knee function and overall sports level score of three groups were displayed in Table 4. From the knee functional score perspective, no significant difference was observed among three groups in 3 months (P>0.05). But the anatomic double-bundle ACL reconstruction group and anatomic single-bundle ACL reconstruction + ALL reconstruction group were better than the anatomic single-bundle reconstruction group in 6 and 12 months. The difference was statistically significant (p < 0.05). However, there was no significant difference between the anatomic double-bundle ACL reconstruction group and anatomic single-bundle ACL reconstruction + ALL reconstruction groups (p > 0.05) (Table 5).
Table 4.
The involved knee function and sports level score from DB and SBL reconstruction groups.
| Group | 3 months | Statistical test | 6 months | Statistical test | 12 months | Statistical test | |
|---|---|---|---|---|---|---|---|
|
IKDC score |
DB | 73.9 ± 2.0 | F= 1.55 P= 0.22 |
89.6 ± 1.8 | Duncan n.s. |
95.1 ± 0.9 | Duncan n.s. |
| SBL | 74.9 ± 3.2 | 88.2 ± 3.2 | 96.2 ± 1.6 | ||||
|
Lysholm score |
DB | 80.1 ± 1.9 | F= 2.96 P= 0.06 |
86.2 ± 3.1 | Duncan n.s. |
95.2 ± 0.9 | Duncan n.s. |
| SBL | 81.4 ± 3.3 | 90.9 ± 1.8 | 96.3 ± 1.6 | ||||
|
Tegner score |
DB | 3.6 ± 0.3 | F= 2.99 P= 0.06 |
4.5 ± 0.3 | Duncan n.s. |
6.0 ± 0.4 | Duncan n.s. |
| SBL | 3.4 ± 0.3 | 4.8 ± 0.3 | 6.3 ± 0.3 |
DB: anatomic double-bundle ACL reconstruction group, SBL: anatomic single-bundle ACL reconstruction + ALL reconstruction group. n.s.: no significance
Table 5.
The involved knee function and sports level score of three groups.
| Group | 3 months | Statistical test | 6 months | Statistical test | 12 months | Statistical test | |
|---|---|---|---|---|---|---|---|
| IKDC score |
SB | 73.2 ± 3.0 | F=1.55 P=0.22 |
84.3 ± 3.1 | F=16.55 P<0.001 |
89.1 ± 2.6 | F=74.04 P<0.001 |
| DB | 73.9 ± 2.0 | 89.6 ± 1.8 | 95.1 ± 0.9 | ||||
| SBL | 74.9 ± 3.2 | 88.2 ± 3.2 | 96.2 ± 1.6 | ||||
| Lysholm score |
SB | 79.5 ± 2.1 | F=2.96 P=0.06 |
81.8 ± 2.8 | F=51.05 P<0.001 |
89.3 ± 2.3 | F=79.94 P<0.001 |
| DB | 80.1 ± 1.9 | 86.2 ± 3.1 | 95.2 ± 0.9 | ||||
| SBL | 81.4 ± 3.3 | 90.9 ± 1.8 | 96.3 ± 1.6 | ||||
| Tegner score |
SB | 3.4 ± 0.3 | F=2.99 P=0.06 |
4.0 ± 0.3 | F=24.4 P<0.001 |
4.8 ± 0.3 | F=86.90 P<0.001 |
| DB | 3.6 ± 0.3 | 4.5 ± 0.3 | 6.0 ± 0.4 | ||||
| SBL | 3.4 ± 0.3 | 4.8 ± 0.3 | 6.3 ± 0.3 |
DB: anatomic double-bundle ACL reconstruction group, SB: anatomic single-bundle ACL reconstruction, SBL: anatomic single-bundle ACL reconstruction + ALL reconstruction group.
In this study, one patient of the anatomic single-bundle ACL reconstruction group was infected post-operatively after five days. Debridement was performed in arthroscopy. The graft was retained. Closed washing and drainage were not performed until the flushing fluid was consecutively cultured negative for three times. Intravenous and oral antibiotics were applied for six weeks. Ultimately, the infection was controlled. The knee function restored very well after rehabilitation. In addition, in anatomic single-bundle ACL reconstruction + ALL reconstruction group, one patient’s interference screw of the tibial side did not completely enter the tunnel at the time of ALL reconstruction. But the patient did not complain any discomfort. No special treatment was made temporarily.
Discussion
Nowadays, as more and more people craved in sports and fitness, patients suffering from the athletic injury are also increasing. Epidemiological study of athletic injury showed that anterior cruciate ligament injury was one of the most common athletic injuries. Its incidence in general population was rising year by year (Voigt et al., 2006). In order to furthest rebuild its anatomical structure, and then restore the knee’s stability, meanwhile improve the joint functions, many scholars conducted a detailed study on the anatomy of anterior cruciate ligament and anterolateral ligament. Anatomical study confirmed that anterior cruciate ligament can be divided into the anteromedial bundle (AM) and posterolateral bundle (PL) according to their tibial attachment sites (Girgis et al., 1975; Schreiber et al., 2010). The anteromedial bundle mainly provides the anteroposterior stability. And the posterolateral bundle mainly provides the rotational stability. The origin of anterolateral ligament is started at the prominence of the lateral femoral epicondyle, slightly anterior to the origin of the lateral collateral ligament. And it ends at the anterolateral aspect of the proximal tibia articular surface, located midway between Gerdy’s tubercle and the tip of the fibular head. Given its anatomical characteristics, anterolateral ligament was considered to control the internal tibial rotation stability and reduce the positive rate of Pivot-shift test (Butler et al., 2013; Claes et al., 2013). However, in our preliminary anatomic study of twenty Asian cadaveric knees, we found that the tibial insertion of ALL was located at the position beyond the joint line 0.8-1.0 cm with equal distance to the Gerdy’s tubercle and the outermost point of the fibular head, rather than the midway between the Gerdy’s tubercle and the tip of the fibular head. This significant finding made us more accurately reconstruct Asian anterolateral ligament anatomically.
Numerous studies confirmed that anatomic single-bundle ACL reconstruction could often achieve comparatively ideal anteroposterior stability after ACL rupture. However, a considerable number of cases were unable to restore the desired rotational stability, while more difficult to restore to the pre-injury activity level (Georgoulis et al., 2005; 2007; Ristanis et al., 2003; Tashman et al., 2004). Thus, the IKDC score of anatomic single-bundle ACL reconstruction can reach only 61% -67% of normal level (Gianotti et al., 2009). Compared with anatomic single-bundle ACL reconstruction, anatomic double-bundle ACL reconstruction strengthened the stability of posterolateral bundle to the knee, especially the rotational stability (Yagi et al., 2007). But in clinical work, not all patients could perform the anatomic double-bundle ACL reconstruction. Many factors, such as the height and width of fossa intercondyloidea, the length and width of ACL footprint, must be synthetically considered. For the patients who can’t be implemented the anatomic double-bundle ACL reconstruction, the anatomic single-bundle ACL reconstruction is the best choice.
In recent years, the anatomic ACL reconstruction is becoming more and more popular. Whether the anatomic single-bundle reconstruction or the anatomic double-bundle reconstruction, there were a large number of clinical reports (Aglietti et al., 2007; Järvelä et al., 2008; Pombo et al., 2008; Shen et al., 2008; Siebold et al., 2008; Schreiber et al., 2010). In addition, with the further understanding of anatomical structure and function of anterolateral ligament, anatomic anterolateral ligament reconstruction is brought to the attention of the surgeon. However, the clinical outcomes of anatomic anterolateral ligament reconstruction are rarely reported. In this study, with the aim to improve the clinical outcomes of anatomic single-bundle ACL reconstruction, the method of reconstructing single-bundle ACL and anterolateral ligament simultaneously was conducted. The knee’s stability and joint functions were examined in 3, 6 and 12 months post-operatively. Results confirmed that this method could obtain better clinical outcomes.
This study confirmed that both anteroposterior and rotational stability of anatomic double-bundle reconstruction group and anatomic single-bundle reconstruction + ALL reconstruction group were better than anatomic single-bundle reconstruction group. However, no significant difference was observed between the DB group and SBL group. From an objective evaluation, the anterolateral ligament can improve the stability of knee. But the overall sports level scores of involved knee showed no significant difference post-operatively after 3 months. This might be attributed to the relatively conservative rehabilitation program. Many daily activities were not allowed within 3 months after surgery, which made the results couldn’t present the differences. In 6 and 12 months after surgery, the IKDC score, Lysholm score and Tegner score of anatomic double-bundle reconstruction group and anatomic single-bundle reconstruction + ALL reconstruction group were better than anatomic single-bundle reconstruction group. But there was still no significant difference between the anatomic double-bundle reconstruction group and anatomic single-bundle reconstruction + ALL reconstruction groups. This indicated that the anterolateral ligament might provide the rotational stability for the knee. In the present study, it was the first time that the anatomic single-bundle ACL reconstruction, the anatomic double-bundle ACL reconstruction, and the anatomic single-bundle ACL reconstruction + ALL reconstruction were performed to compare the clinical outcomes. Our results highlighted that reconstructing the single-bundle ACL and anterolateral ligament simultaneously could achieve the same clinical outcomes compared with the double-bundle ACL reconstruction. It had a strong guiding significance for clinic.
In fact, as early as before the first anterolateral ligament reconstruction applied in clinic, there were many kind of other anterolateral ligament reconstruction approaches adopted by clinicians to reduce the postoperative positive rate of Pivot-shift test (Hughston et al., 1976; Ireland et al., 1980). However, due to the poor understanding of the anatomy of anterolateral ligament, these approaches required a longer surgical incision and were non-anatomic surgery. These approaches often led to the excessive restriction of knee joint or ligament laxity, and failure eventually (Neyret et al., 1994). Therefore, many surgical approaches were eventually abandoned. Since the clear understanding of the anatomy of anterolateral ligament, some scholars had attempted to use the improved one-stage anterolateral ligament extra-articular reconstruction to treat the anterior cruciate ligament injury (Vadala et al., 2013; Zaffagnini et al., 2006). In order to restore the anteroposterior and rotational stability of knee joint after operation, this method achieved good clinical outcomes. With the in-depth understanding of the anatomy of anterolateral ligament, one-stage anatomic reconstruction of the anterior cruciate ligament and anterolateral ligament had been applied in clinic. Two years’ clinical follow-up results showed that it could achieve satisfying clinical outcomes (Sonnery-Cottet et al., 2015).
In this study, one case of the anatomic single-bundle ACL reconstruction + ALL reconstruction group occurred that the interference screw was fixed between the fibular head and the lateral tibial plateau. But it was not found during the operation. This was an early case. In our later operations, more attention was payed to avoid this mistake, which prevented this situation from happening again. Therefore, we concluded that the position which was beyond the joint line 0.8-1.0 cm, with equal distance to the center of Gerdy’s tubercle and the outermost point of fibular head was the best choice for the ALL tibial tunnel entrance. In addition, one case of the anatomic single-bundle ACL reconstruction + ALL reconstruction group occurred the movement-related pain at the femoral interference screw. The pain disappeared after removing the interference screw when considering the pain was caused by the friction between end cap of interference screw and iliotibial band.
For the anatomic anterior cruciate ligament reconstruction surgery, the purpose of operation was trying to achieve the anatomic reconstruction, to restore the biomechanics of knee joint, and to maximize the recovery of pre-injury activity level on the clinical effects. The application of preoperative imaging and arthroscopy to accurately measure the significant parameters and selectively performing the anatomic double-bundle ACL reconstruction or the anatomic single-bundle ACL reconstruction + ALL reconstruction, could restore the anteroposterior and rotational stability of the knee joint effectively, more conducive to the recovery of patients’ function postoperatively.
This study has some limitations. Sixty samples could not reflect the clinical outcomes of ALL reconstruction adequately. The follow-up is limited to one year, which is too short to evaluate the potential favorable and unfavorable changes. The Lysholm score, Tegner score, and IKDC score used to evaluate the knee function are subjective tests.
Conclusion
In conclusion, anatomic anterolateral ligament reconstruction combined with anatomic anterior cruciate ligament reconstruction could improve the postoperative clinical outcomes effectively. The obtained results indicated that the anterolateral ligament played a crucial role in knee’s stability and joint function, especially the rotational stability. Therefore, further studies are required to confirm the clinical role of anterolateral ligament. In addition, our results indicated that combined ACL and ALL reconstruction could be one more surgery choice for the patients who sufferings from the anterior cruciate ligament rupture.
Acknowledgments
The authors sincerely thank the patients who participated in this study. The authors are also acknowledged for the colleagues who participated in the clinical follow-up of postoperative patients. The authors declare that they have no conflict of interest.
Biographies

Hua ZHANG
Employment
Sports physician, Department of Orthopedics, The First Affiliated Hospital of Chongqing Medical University, China
Degree
PhD
Research interests
Knee injuries, Shoulder injuries, Sports traumatology, Arthroscopy, Sports medicine
E-mail: 939744839@qq.com

Man QIU
Employment
Anesthesiologist, Department of Anesthesiolog, The First Affiliated Hospital of Chongqing Medical University, China
Degree
MSc
Research interests
Knee injuries, Anesthesiology
E-mail: 786847365@qq.com

Aiguo ZHOU
Employment
Professor, Department of Orthopedics, The First Affiliated Hospital of Chongqing Medical University, China
Degree
PhD
Research interests
Joint injuries, Sports medicine, Sports traumatology, Muscle injuries, Arthroscopy, Joint replacement
E-mail: 369804524@qq.com

Jian ZHANG
Employment
Professor, Department of Orthopedics, The First Affiliated Hospital of Chongqing Medical University, China
Degree
PhD
Research interests
Joint injuries, Joint replacement, Sports medicine, Sports traumatology
E-mail: zhangjiancqmu@sohu.com

Dianming JIANG
Employment
Professor, Department of Orthopedics, The First Affiliated Hospital of Chongqing Medical University, China
Degree
PhD
Research interests
Muscle injuries, Knee injuries, Sports medicine, Sports traumatology, Joint replacement
E-mail: jdmcqmu@163.com
References
- Aglietti P., Giron F., Cuomo P., Losco M., Mondanelli N. (2007) Single-and double-incision double-bundle ACL reconstruction. Clinical Orthopaedics and Related Research 454, 108-113. [DOI] [PubMed] [Google Scholar]
- Amis A.A. (2012) The functions of the fibre bundles of the anterior cruciate ligament in anterior drawer, rotational laxity and the pivot shift. Knee Surgery Sports Traumatology Arthroscopy 20(4), 613-620. [DOI] [PubMed] [Google Scholar]
- Araujo P.H., van Eck C.F., Macalena J.A., Fu FH. (2011) Advances in the three-portal technique for anatomical single- or double-bundle ACL reconstruction. Knee Surgery Sports Traumatology Arthroscopy 19(8), 1239-1242. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bonasia D.E., D’Amelio A., Pellegrino P., Rosso F., Rossi R. (2015) Anterolateral ligament of the knee: back to the future in anterior cruciate ligament reconstruction. Orthopaedics Reviews (Pavia) 7(2), 5773. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Budny J., Fox J., Rauh M., Fineberq M. (2016) Emerging Trends in Anterior Cruciate Ligament Reconstruction. Journal of Knee Surgery DOI:10.1055/s-0036-1579788. [DOI] [PubMed] [Google Scholar]
- Butler P.D., Mellecker C.J., Rudert M.J., Albriqht J.P. (2013) Single-bundle versus double-bundle ACL reconstructions in isolation and in conjunction with extra-articular iliotibial band tenodesis. Iowa Orthopaedic Journal 33, 97-106. [PMC free article] [PubMed] [Google Scholar]
- Claes S., Vereecke E., Maes M., Victor J., Verdonk P., Bellemans J. (2013) Anatomy of the anterolateral ligament of the knee. Journal of Anatomy 223(4), 321-328. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Franceschi J.P., Sbihi A., Champsaur P. (2002) Arthroscopic reconstruction of the anterior cruciate ligament using double anteromedial and posterolateral bundles. Reveu Chirurgie Orthopedique Reparatrice Appareil Moteur 88(7), 691-697. [PubMed] [Google Scholar]
- Georgoulis A.D., Ristanis S., Chouliaras V., Moraiti C., Stergiou N. (2005) Anterior cruciate ligament reconstruction with a quadrupled hamstring auto graft does not restore tibial rotation. Techniques in Orthopaedics 20(3), 328-333. [Google Scholar]
- Georgoulis A.D., Ristanis S., Chouliaras V., Moraiti C., Stergiou N. (2007) Tibial rotation is not restored after ACL reconstruction with a hamstring graft. Clinical Orthopaedics and Related Research 454, 89-94. [DOI] [PubMed] [Google Scholar]
- Gianotti S.M., Marshall S.W., Hume P.A., Bunt L. (2009) Incidence of anterior cruciate ligament injury and other knee ligament injuries: a national population based study. Journal of Science Medicine in Sport 12(6), 62-627. [DOI] [PubMed] [Google Scholar]
- Girgis F.G., Marshall J.L., Monajem A. (1975) The cruciate ligaments of the knee joint. Anatomical, functional and experimental analysis. Clinical Orthopaedics and Related Research 106, 216-231. [DOI] [PubMed] [Google Scholar]
- Goldsmith M.T., Jansson K.S., Smith S.D., Enqebretsen L., LaPrade R.F., Wijdicks C.A. (2013) Biomechanical comparison of anatomic single- and double-bundle anterior cruciate ligament reconstructions: an in vitro study. American Journal Sports of Medicine 41(7), 1595-1604. [DOI] [PubMed] [Google Scholar]
- Hughston J.C., Andrews J.R., Cross M.J., Moschi A. (1976) Classification of knee ligament instabilities. Part II. The lateral compartment. Journal of Bone and Joint Surgery-American Volume 58, 173-179. [PubMed] [Google Scholar]
- Ireland J., Trickey E.L. (1980) Macintosh tenodesis for anterolateral instability of the knee. Journal of Bone and Joint Surgery-British Volume 62, 340-345. [DOI] [PubMed] [Google Scholar]
- Järvelä T., Moisala A.S., Sihvonen R., Järvelä S., Kannus P., Järvinen M. (2008) Double-Bundle Anterior Cruciate Ligament Reconstruction Using Hamstring Auto grafts and Bioabsorbable Interference Screw Fixation: Prospective, Randomized Clinical Study with 2-Year Results. American Journal Sports of Medicine 36(2), 290-297. [DOI] [PubMed] [Google Scholar]
- Kondo E., Merican A.M., Yasuda K., Amis A.A. (2010) Biomechanical comparisons of knee stability after anterior cruciate ligament reconstruction between 2 clinically available transtibial procedures: anatomic double bundle versus single bundle. American Journal Sports of Medicine 38(7), 1349-1358. [DOI] [PubMed] [Google Scholar]
- Lorenz S., Anetzberger H., Spang J.T., Imhoff A.B. (2007) Double-bundle technique - anatomic reconstruction of the anterior cruciate ligament. Operative Orthopadie Traumatologie 19(5-6), 473-488. [DOI] [PubMed] [Google Scholar]
- Mascarenhas R., Cvetanovich G.L., Sayegh E.T., Verma N.N., Cole B.J., Bush-Joseph C., Bach B.R., Jr. (2015) Does Double-Bundle Anterior Cruciate Ligament Reconstruction Improve Postoperative Knee Stability Compared With Single-Bundle Techniques? A Systematic Review of Overlapping Meta-analyses. Arthroscopy 31(6), 1185-1196. [DOI] [PubMed] [Google Scholar]
- Neyret P., Palomo J.R., Donell S.T., Dejour H. (1994) Extra-articular tenodesis for anterior cruciate ligament rupture in amateur skiers. British Journal Sports Medicine 28(1), 31-34. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Nitri M., Rasmussen M.T., Williams B.T., Moulton S.G., Cruz R.S., Dornan G.J., Goldsmith M.T., LaPrade R.F. (2016) An In Vitro Robotic Assessment of the Anterolateral Ligament, Part 2: Anterolateral Ligament Reconstruction Combined With Anterior Cruciate Ligament Reconstruction. American Journal Sports of Medicine 44(3), 593-601. [DOI] [PubMed] [Google Scholar]
- Petersen W., Forkel P., Achtnich A., Metzlaff S., Zantop T. (2013) Anatomic reconstruction of the anterior cruciate ligament in single bundle technique. Operative Orthopadie Traumatologie 25(2), 185-204. [DOI] [PubMed] [Google Scholar]
- Plaweski S., Grimaldi M., Courvoisier A., Wimsey S. (2011) Intraoperative comparisons of knee kinematics of double-bundle versus single-bundle anterior cruciate ligament reconstruction. Knee Surgery Sports Traumatology Arthroscopy 19(8), 1277-1286. [DOI] [PubMed] [Google Scholar]
- Pomajzl R., Maerz T., Shams C., Guettler J., Bicos J. (2015) A review of the anterolateral ligament of the knee: current knowledge regarding its incidence, anatomy, biomechanics, and surgical dissection. Arthroscopy 31(3), 583-591. [DOI] [PubMed] [Google Scholar]
- Pombo M.W., Shen W., Fu F.H. (2008) Anatomic double-bundle anterior cruciate ligament reconstruction: where are we today? Arthroscopy 24(10), 1168-1177. [DOI] [PubMed] [Google Scholar]
- Ristanis S., Giakas G., Papageorgiou C.D., Moraiti T., Stergiou N., Georgoulis A.D. (2003) The effects of anterior cruciate ligament reconstruction on tibial rotation during pivoting after descending stairs. Knee Surgery Sports Traumatology Arthroscopy 11(6), 360-365. [DOI] [PubMed] [Google Scholar]
- Schreiber V.M., van Eck C.F., Fu F.H. (2010) Anatomic Double-bundle ACL Reconstruction. Sports Med Arthrosc 18(1), 27-32. [DOI] [PubMed] [Google Scholar]
- Shen W., Forsythe B., Ingham S.M., Honkamp N.J., Fu F.H. (2008) The anatomic double bundle reconstruction concept to revision and augmentation anterior cruciate ligament surgeries. Journal Bone and Joint Surgery American 4, 20-34. [DOI] [PubMed] [Google Scholar]
- Siebold R., Dehler C., Ellert T. (2008) Prospective randomized comparison of double-bundle versus single-bundle anterior cruciate ligament reconstruction. Arthroscopy 24, 137-145. [DOI] [PubMed] [Google Scholar]
- Smith J.O., Yasen S.K., Lord B., Wilson A.J. (2015) Combined anterolateral ligament and anatomic anterior cruciate ligament reconstruction of the knee. Knee Surgery Sports Traumatology Arthroscopy 23(11), 3151-3156. [DOI] [PubMed] [Google Scholar]
- Sonnery-Cottet B., Thaunat M., Freychet B., Pupim B.H., Murphy C.G., Claes S. (2015) Outcome of a Combined Anterior Cruciate Ligament and Anterolateral Ligament Reconstruction Technique With a Minimum 2-Year Follow-up. American Journal Sports of Medicine 43(7), 1598-1605. [DOI] [PubMed] [Google Scholar]
- Sun R., Chen B.C., Wang F., Wang X.F., Chen J.Q. (2015) Prospective randomized comparison of knee stability and joint degeneration for double- and single-bundle ACL reconstruction. Knee Surgery Sports Traumatology Arthroscopy 23(4), 1171-1178. [DOI] [PubMed] [Google Scholar]
- Tashman S., Collon D., Anderson K., Kolowich P., Anderst W. (2004) Abnormal rotational knee motion during running after anterior cruciate ligament reconstruction. American Journal Sports of Medicine 32(4), 975-983. [DOI] [PubMed] [Google Scholar]
- Vadala A.P., Iorio R., De C.A., Bonifazi A., Iorio C., Gatti A., Rossi C., Ferretti A. (2013) An extra-articular procedure improves the clinical outcome in anterior cruciate ligament reconstruction with hamstrings in female athletes. International Orthopaedics 37(2), 187-192. [DOI] [PMC free article] [PubMed] [Google Scholar]
- van Eck C., Working Z., Fu F. (2011) Current concepts in anatomic single- and double-bundle anterior cruciate ligament reconstruction. Physician and Sports medicine 39(2), 140-148. [DOI] [PubMed] [Google Scholar]
- Voigt C., Schönaich M., Lill H. (2006) Anterior cruciate ligament reconstruction: state of the art. European Journal of Trauma 32, 332-329. [Google Scholar]
- Xu Y., Ao Y.F., Wang J.Q., Cui G.Q. (2014) Prospective randomized comparison of anatomic single- and double-bundle anterior cruciate ligament reconstruction. Knee Surgery Sports Traumatology Arthroscopy 22(2), 308-316. [DOI] [PubMed] [Google Scholar]
- Yagi M., Kuroda R., Nagamune K., Yoshiya S., Kurosaka M. (2007) Double-bundle ACL reconstruction can improve rotational stability. Clinical Orthopaedics and Related Research 454, 100-107. [DOI] [PubMed] [Google Scholar]
- Zaffagnini S., Marcacci M., Lo P.M., Giordano G., Iacono F., Neri M.P. (2006) Prospective and randomized evaluation of ACL reconstruction with three techniques: a clinical and radiographic evaluation at 5 years follow-up. Knee Surgery Sports Traumatology Arthroscopy 14(11), 1060-1069. [DOI] [PubMed] [Google Scholar]
- Zhu Y., Tang R.K., Zhao P., Zhu S.S., Li Y.G., Li J.B. (2013) Double-bundle reconstruction results in superior clinical outcome than single-bundle reconstruction. Knee Surgery Sports Traumatology Arthroscopy 21(5), 1085-1096. [DOI] [PubMed] [Google Scholar]


