Abstract
Purpose
Over 20% of young adults in New Mexico currently smoke. We evaluated cigarette smoking prevalence of young adult bar patrons during an anti-tobacco Social Branding intervention.
Methods
The Social Branding intervention used a smoke-free brand, “HAVOC,” to compete with tobacco marketing within the “Partier” young adult peer crowd. A series of cross-sectional surveys were collected from adults aged 18–26 in bars and nightclubs in Albuquerque, New Mexico, from 2009 to 2013 using randomized time-location sampling. Multivariable multinomial regression using full information maximum likelihood estimation to account for missing data evaluated differences in daily and nondaily smoking during the intervention, controlling for demographics, other risk behaviors, and tobacco-related attitudes.
Results
Data were collected from 1,069 individuals at Time 1, and 720, 1,142, and 1,149 participants at Times 2, 3, and 4, respectively. Current smoking rates decreased from 47.5% at Time 1 to 37.5% at Time 4 (p < .001). Among Partiers, the odds of daily smoking decreased significantly, but nondaily smoking was unchanged. Partiers that recalled, liked, and understood the smoke-free message of HAVOC had lower odds of nondaily (odds ratio: .48, 95% CI: .31–.75) and daily (odds ratio: .31,95% CI: .14–.68) smoking than those who did not recall HAVOC. HAVOC recall was associated with attitudes that were also associated with smoking behavior.
Conclusions
The significant decrease in daily smoking among young adult Partiers in New Mexico was associated with HAVOC recall and understanding. Social Branding interventions efficiently target and may decrease tobacco use among young adult bar patrons.
Keywords: Cigarette smoking, Young adult, Tobacco use disorder/prevention and control, Social marketing
Long-term nicotine dependence often begins during adolescence and young adulthood, when almost all adult daily smokers initiate cigarette smoking or transition from experimentation to regular smoking [1]. Cigarette smoking is associated with increased mortality, primarily from cardiopulmonary diseases, and malignancy [2]. To decrease these risks, it is important to discourage smoking initiation and encourage smoking cessation in younger individuals, as the risk of death from diseases caused by smoking is greatly reduced by stopping smoking before age 40 [2,3].
Approximately, 19.7% [4] of young adults aged 18–24 years old in New Mexico are current cigarette smokers, exceeding the 19.1% [4] and 17.8% [5] prevalence for all adults in New Mexico and the United States, respectively. New Mexico's comprehensive law prohibiting smoking in indoor workplaces and most public places, such as restaurants and bars, has been in place since June 2007. Even in the presence of smoke-free policies, young adults remain susceptible to tobacco industry marketing [6,7], particularly in social environments such as bars and nightclubs [8,9]. In addition, young adults continue to report high levels of secondhand smoke exposure in bars, even in cities with comprehensive smoke-free policies [10].
Most previous studies of smoking cessation interventions tailored for U.S. young adults have focused on college students, and evidence for their efficacy in this population has been limited [11]. In studies of the general adult population, young adults receiving interventions such as pharmacotherapy or behavioral therapy have higher odds of smoking cessation than young adults in control groups [12]; however, fewer young adults use such treatments. Anti-smoking campaigns designed for youth have been associated with decreased smoking initiation [13], and awareness of such interventions among young adults is associated with anti-smoking attitudes [14], which can be important for both discouraging initiation among nonsmokers and encouraging cessation among smokers. Furthermore, research suggests that for young adults, peer smoking behavior and perceived social norms of smoking are associated with smoking [15]. Thus, interventions incorporating anti-smoking messaging and peers can be an effective means of influencing young adult smoking.
One such intervention focused on peer influence is Social Branding. Developed by Rescue, a public health marketing agency, Social Branding is a variant of social marketing, an approach that aims to influence people's behaviors using commercial marketing strategies [16]. Specifically, Social Branding uses “social brands” targeted to specific peer crowds at high risk for unhealthy behaviors to associate healthy behaviors with peer crowd values. Although most branded social marketing efforts create brands to promote health behaviors to general audiences, such as “tweens” (VERB) [17] or “teens open to smoking” (truth) [17,18], a critical component of Social Branding is that a social brand is precisely targeted to a high-risk peer crowd by specifically aligning with the peer crowd's interests to establish cultural authenticity and brand equity. Then, the social brand uses its status within the peer crowd to associate certain values unique to that peer crowd with a positive health behavior through the use of interactive experiences at events, culturally relevant influencers, and interactive digital media. The multi-component intervention strategy has been further described previously and is summarized in Figure A (Online Supplement) [19,20]. Social Branding interventions targeting smoking behavior have been implemented previously in bars in San Diego, California [19], Oklahoma City, Oklahoma [11], and Las Vegas, Nevada [19–21], with decreases in smoking prevalence noted in different populations of young adults. We aimed to evaluate young adult smoking prevalence over the course of 3 years during a Social Branding intervention implemented in bars and nightclubs in a different city, Albuquerque, New Mexico, and also to explore potential mediators in the association between the intervention and smoking status.
Methods
The study was designed as a series of cross-sectional surveys of the target population (young adult bar patrons of Partier bars) during the implementation of the intervention, without a comparison community. A series of cross-sectional surveys were collected from adults aged 18–26 years in bars and nightclubs popular among young adults in Albuquerque, New Mexico, at Time 1 (June 2009–August 2009) and three subsequent periods (Time 2: October 2009–May 2010, Time 3: March 2011–December 2011, and Time 4: December 2012–December 2013). A Social Branding intervention called HAVOC [20] was implemented in New Mexico during this time. To determine the target population for this intervention, surveys, ethnographic observation, and focus groups were conducted in three cities in New Mexico, including Albuquerque, in September 2008–October 2008. A total of 316 young adults completed surveys, and 79 participated in a total of 12 focus groups. The groups included young adults from various peer crowds, and through those groups, distinct peer crowds were identified and described. This formative research revealed that the Partier peer crowd had the largest reach of influence with a relatively high young adult smoking prevalence, and therefore, this group was the target for the HAVOC intervention.
Peer crowds are social groups with similar interests, lifestyle norms, and habits that are consistently found across different geographic areas [22]. Partiers are characterized by attendance at large nightclubs, high concern for fashion, valuing physical attractiveness, preferring DJ venues over live music, and achieving high social status by exuding an image of confidence and financial success [20]. Young adults who affiliate with many different peer crowds go to bars and socialize, but Partiers are perceived by other young adults both to attend certain venues, and to go out to bars more frequently, for longer hours, and with greater consumption of alcohol and/or other substances, which led to the name “Partiers.” Although in this study “Partiers” refers to this group, the term is not used in the public face of the campaign, and it does not apply to all young adults who go to parties.
The HAVOC brand was established initially without any anti-tobacco messaging in April 2009, to promote the brand's appeal, influence, and social acceptability within the Partier social scene. After the brand gained acceptance of more Partiers (ex. through more event attendance), anti-tobacco messaging was introduced in July 2009. The intervention consisted of several interrelated components (Figure A, Online Supplement). Examples of targeted messaging included, “75% of young adults prefer to date, kiss, and be with nonsmokers,” “smokers are four times more likely to feel like they do not sleep well and more likely to have bags under their eyes than nonsmokers.” The HAVOC campaign included sponsored social events at bars and nightclubs (approximately 8–10 events per year), trained brand ambassadors (social leaders and trendsetters recruited to disseminate the smoke-free message at HAVOC events and in their daily lives), a website, a social media presence (i.e., Facebook, YouTube, Instagram, Twitter) including paid advertising, and direct mail promotions that advertised events and conveyed anti-tobacco messages. Similar to studies of adolescents in schools [23], where informal nonclassroom interactions with influential peers have been associated with decreased smoking compared with usual school smoking education, and opinion leaders in human immunodeficiency virus education, where behavior change messages are integrated by these leaders in their regular conversations, the influence of brand ambassadors was primarily intended to be within day to day life, rather than in a formal instructional setting [24]. Social rewards, such as clothing, prizes, and VIP status, were also used to reinforce and promote health behaviors.
Time location sampling, which has been effective in sampling hard-to-reach populations [25–27], was used to recruit young adults attending Partier bars and clubs at randomly selected venues, dates, and times. The census of popular Partier bars was identified using focus groups and interviews with individuals such as bartenders, party promoters, and disc jockeys familiar with the local Partiers. Data collection did not occur at the same time that HAVOC events were hosted, but the same bars could have been used for data collection and an event. At each study site, trained personnel approached individuals who appeared to be under 30 years old and screened them for age between 18 and 26 years old, residence, and prior survey completion. Those who qualified were invited to fill out a handwritten survey including demographic information and questions about tobacco and alcohol use patterns, exposure to the HAVOC intervention, and tobacco-related attitudes. Individuals who were out of age range had previously completed the survey, did not live in Albuquerque, or appeared visibly intoxicated or were unwilling to provide oral informed consent were excluded from the study. Participants received $5 for completing the questionnaire. After data collection, individuals whose age as calculated by date of birth was <18 or >26 were excluded from analysis. Individuals who did not currently reside in Albuquerque, New Mexico, or were in college outside of Albuquerque were also excluded given that the target population was that which lived in the area of the intervention. The study protocol was approved by the Committee for Human Research (the Institutional Review Board) at the University of California San Francisco.
Measures
Peer crowd affiliation
As described elsewhere [19,20,22], participants selected pictures of young adults from a grid based on whom they were most and least likely to be friends with, and selected venues from a list of bars and nightclubs that they were most and least likely to attend. The pictures and bars included in the surveys were selected through observation, focus groups, and surveys with young adults before the intervention. During focus groups, participants sorted pictures of young adults into groups that they felt were likely to be friends and described the characteristics and bars where members of each group were likely to socialize. Participants also selected the three pictures they felt were the best representation of each group. This process was repeated until saturation/consensus on peer crowds, the best representative pictures and venues was reached. The best 28 photos and a list of the most popular bars that were identified with each peer crowd were included on the surveys. Survey participants were shown the 28 photos and asked to rank the three people who would best fit into their main group of friends and the three people who would least fit into their group of friends. For bars, they were given a list of 17 bars and clubs in Albuquerque and asked to select the three bars they were most likely and three they were least likely to attend. The top choices for pictures and bars/clubs were given a score of 3, 2, or 1, and the bottom choices were scored −3, −2, and −1; the total picture score and the total bar score each ranged from −6 to 6, so the overall peer crowd affiliation score ranged from −12 to 12. Individuals who scored the highest for a particular peer crowd compared with their other scores were coded as being of that peer crowd. Those who had highest affiliation with the Partier peer crowd were classified as Partiers. While the intervention targeted Partiers, members of all peer crowds were included in analyses, as non-Partiers may serve as a comparison group.
Tobacco product and alcohol use patterns
Participants were asked on how many of the previous 30 days they had used cigarettes. Current nonsmokers reported smoking cigarettes on 0 of the past 30 days. Current smokers reported any cigarette use in the past 30 days and were divided into nondaily (smoked on 1–29 of the past 30 days) and daily (smoked on 30 of the past 30 days) smokers. The use of other tobacco products (such as cigars, little cigars, hookah, snus, dip, and electronic cigarettes) was also assessed among participants; description of these findings have been reported elsewhere [28]. Unless otherwise noted, smoking refers just to the use of cigarettes throughout this study.
Participants who reported binge drinking (drinking at least five alcoholic shots or drinks within a few hours or same night) on at least one of the past 30 days were classified as current binge drinkers.
Tobacco-related measures
Using a standard measure [29], participants were asked, “Would you ever use a tobacco promotional item?” (yes/no). Those who said “yes” were coded as having tobacco advertising receptivity.
As in other studies [30,31], support for action against the tobacco industry was assessed with agreement with three statements (“I would like to see cigarette companies go out of business,” “I want to be involved with efforts to get rid of cigarette smoking,” and “Taking a stand against smoking is important to me”), measured on a five-point Likert scale from “not at all” to “a great deal.” The mean of the three items was used as a continuous variable in analyses.
Perceived peer prevalence of smoking tobacco was assessed by asking participants, “Based on what you have seen, how many people your age smoke tobacco?” and asking them to circle a percentage from 0%–100% on an 11-point scale. Participants were asked about changes in perceived tobacco use and attitudes in the past year by rating the statements, “In the places I party, people are smoking tobacco” and “I can relate to reasons not to smoke cigarettes” (reverse coded) on a five-point Likert scale from “a lot less” to “a lot more” [19,20].
Social prioritization index
Participants were asked a series of questions about their personality traits and social behaviors to assess the degree of identification with social behaviors and socialization at bars. The Social Prioritization Index was derived from the sum of the answers and was used as a continuous variable for analyses [19,32].
Recall of the smoke-free intervention, liking intervention, and understanding message
Participants were asked whether they had (1) heard of the HAVOC intervention; (2) ever been to a HAVOC event; or (3) visited HAVOC's website or social media site. Those who answered yes to any of the previously mentioned questions were characterized as having recall of the HAVOC intervention.
Participants were also asked “How much do you like HAVOC?” and “If HAVOC hosted an event on a night that you usually go somewhere else, how likely is it that you would go to the HAVOC event instead?” Those who said they “like” or “really like” HAVOC or “probably would go” or “definitely would go” to a HAVOC event were coded as liking the intervention. Participants rated a series of statements judging how well each of the statements represented HAVOC on a five-point scale ranging from 1 = “not at all,” 2 = “a little,” 3 = “a moderate amount,” 4 = “a lot” to 5 = “a great deal.” One of the statements reflected the intent of the brand (“Partying smoke-free”) and the others did not (e.g., “socializing and meeting new people,” “getting drunk”). Rating “partying smoke-free” from 3 to 5 was coded as understanding the smoke-free message.
Demographics
In addition to date of birth, participants were asked to report their sex, race/ethnicity (non-Hispanic Caucasian, Hispanic, and non-Hispanic Other Race [African-American, Asian, Pacific Islander/Hawaiian, American Indian/Native Alaskan]), sexual orientation (straight or lesbian, gay, bisexual, or other [LGB]), and level of education (“high school only or college dropout,” “in college,” and “college graduate”).
Data analysis
Planned missing data
To decrease participant response burden, which is particularly important in the bar/nightclub setting where this study was conducted, the Time 4 questionnaire used a three-form planned missing data design (surveys at Time 1 through 3 did not have planned missing data) [33]. Specifically, participants completed one of three randomly selected versions of the questionnaire; each version contained a core set of questions that appear on all forms, combined with other questions that appear on only two of the three forms, with the plan to subsequently impute the missing values. This made use of a longer questionnaire feasible in this setting. By design, approximately one third of participants were not asked about the use of a tobacco promotional item, the social prioritization index, or recall of the HAVOC intervention, with the plan to impute missing values [33].
Full information maximum likelihood (FIML) directly estimates model parameters and standard errors using all the raw data that are available across all the waves of data collected rather than imputing or filling in missing values. This type of estimation has been shown to be an optimal approach to deal with missing data in a wide variety of situations [34].
Analysis of smoking among Partiers and non-Partiers
Multivariable multinomial logistic regression assessed predictors of smoking status (daily or nondaily smoking). All models were estimated using Mplus 7.2 (Los Angeles, CA) with FIML estimation [35,36]. The FIML method has been shown to produce more accurate estimates in models by adjusting for the uncertainty caused by missing data [34,37]. Separate regression coefficients were estimated for Partiers (the target population of the intervention) and non-Partiers. Groups were also compared based on intervention recall (Partiers with HAVOC recall, Partiers without HAVOC recall, non-Partiers with HAVOC recall, and non-Partiers without HAVOC recall) to examine the moderating effects of Partier status and recall on smoking status.
An exploratory subgroup analysis was conducted to examine potential mediators of the association between HAVOC recall and smoking status among Partiers (n = 758). To better address the effect of the smoke-free brand, among those who recalled HAVOC we examined three groups: (1) those who recall HAVOC but do not like or understand it; (2) recall HAVOC and like OR understand it: and (3) recall HAVOC and like AND understand it. We ran three sets of analyses to examine how the relationship between these groups and smoking might be mediated by tobacco-related attitudes. First, logistic regression models examined the relationship between liking/understanding groups and smoking status both with and without controls for demographic variables. Second, we examined how group status was related to different measures of tobacco-related attitudes (advertising receptivity, support for action against the tobacco industry, perceived smoking prevalence among peers, and perceptions of trends in smoking and smoking cessation) using analysis of variance, PROC GLM in SAS, version 9.4 (SAS Institute, Inc., Cary, NC). Third, we examined how these tobacco-related measures were related to smoking status in univariable models (SAS) and multivariable models (Mplus), controlling for demographic factors.
Results
Demographics
Multiple tobacco product use among young adult bar patrons in New MexicoData were collected from 1,069 individuals at Time 1, and 720, 1,142, and 1,149 participants at Times 2, 3, and 4, respectively. The overall survey response rate among eligible young adults for 2010–2013 was 75.8%. The lower data collection rate at Time 2 corresponded to reduced funding at that time. Most respondents in all study years were over age 21; the largest population of 18–20 year olds was seen in Time 3 (25%). Most (54%–60%) of the total study participants were in college locally in Albuquerque. Approximately, one third of participants were Partiers at Time 1 (33%) and Time 2 (29%); in Times 3 and 4, approximately half of respondents were Partiers. Other demographic characteristics of the study population are shown in Table 1.
Table 1. Demographics by time of study.
| Time 1; n (%) | Time 2; n (%) | Time 3; n (%) | Time 4; n (%) | |
|---|---|---|---|---|
| Age, years (n = 4,080) | ||||
| 18–20 | 20 (2) | 15 (2) | 285 (25) | 154 (13) |
| 21–23 | 676 (63) | 439 (61) | 531 (46.5) | 609 (53) |
| 24–26 | 373 (35) | 266 (37) | 326 (28.5) | 386 (34) |
| Race/ethnicity (n = 4,046) | ||||
| White | 502 (48) | 283 (40) | 273 (24) | 277 (24) |
| Hispanic | 374 (36) | 301 (42) | 692 (61) | 686 (60) |
| Other | 170 (16) | 131 (18) | 176 (15) | 181 (16) |
| Education (n = 4,071) | ||||
| HS only/college dropout | 150 (14) | 155 (21.5) | 248 (22) | 285 (25) |
| In college | 614 (58) | 396 (55) | 687 (60) | 620 (54) |
| College Graduate | 302 (28) | 169 (23.5) | 204 (18) | 241 (21) |
| Male sex (n = 4,051) | 608 (58) | 403 (56) | 497 (44) | 574 (50) |
| LGB sexual orientation (n = 4,069)a | 101 (9.5) | 85 (12) | 216 (19) | 188 (16) |
| Smoking status (n = 3,909) | ||||
| Nonsmoker | 553 (53) | 348 (50) | 633 (57) | 658 (63) |
| Nondaily smoker | 328 (31) | 214 (31) | 344 (31) | 298 (28) |
| Daily smoker | 169 (16) | 132 (19) | 136 (12) | 96 (9) |
| Tobacco advertising receptivity (n = 3,675) | 261 (25) | 244 (35) | 291 (26) | 183 (23) |
| HAVOC intervention recall (n = 3,622) | 111 (11) | 106 (15) | 262 (23) | 268 (37) |
| Partier peer crowd association (n = 4,080) | 352 (33) | 212 (29) | 581 (51) | 586 (51) |
| Binge drinking in past 30 days (n = 3,887) | 830 (79.5) | 506 (73.5) | 641 (58) | 778 (74) |
| Anti-industry attitude (mean, SD) (n = 4,000) | 2.5 (1.3) | 2.6 (1.3) | 3.0 (1.3) | 2.6 (1.3) |
| Social Prioritization Index (mean, SD; n = 3,396) | 9.1 (3.2) | 8.2 (3.0) | 9.6 (3.1) | 9.2 (3.1) |
HS = high school; n = total row n.
Lesbian, gay, bisexual.
Smoking and binge drinking prevalence
The prevalence of current smoking was 47% at Time 1, 50% at Time 2, 43% at Time 3, and 37.5% at Time 4. Figure 1 shows the distribution of daily and nondaily smokers for the overall study population and for the subgroups of Partiers and Partiers with HAVOC recall.
Figure 1.
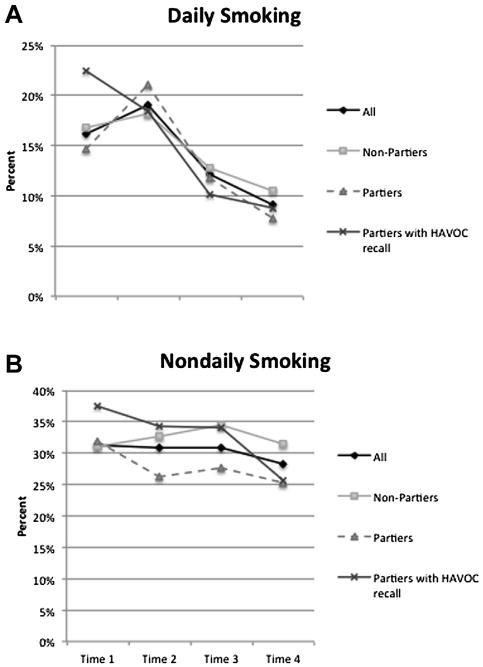
Daily and Non-daily smoking behavior at each time point among the total sample, Partiers, non-Partiers, and Partiers who recalled exposure to the HAVOC intervention.
Odds of binge drinking at Time 4 compared to Time 1 were .82 (95% CI: .71–.85), controlling for demographics and social prioritization index.
Exposure to smoke-free intervention, liking intervention, and understanding message
At Time 1, 11% of those surveyed reported HAVOC intervention recall. HAVOC recall was 15% at Time 2, 23% at Time 3, and 37% at Time 4. Of those exposed to the intervention, 34% at Time 2, 42% at Time 3, and 47% at Time 4 said that they either “like it” or “really like it” when asked how much they liked HAVOC. Of those exposed to the intervention, 42% of respondents at Time 2, 48% in Time 3, and 52% in Time 4 said that they either “probably would go” or “definitely would go” if HAVOC hosted an event on a night they usually go somewhere else. Overall, 63% of the participants exposed to HAVOC understood its smoke-free message.
Partier status, HAVOC recall, and other correlates of smoking status
Predictors of daily and nondaily smoking were analyzed using multivariable multinomial regression, stratified by Partier status (Tables 2 and 3). Specifically, for duration of intervention, Partiers with HAVOC recall (odds ratio [OR]: .41, 95% CI: .19–.84) and Partiers without HAVOC recall (OR: .56, 95% CI: .36–.89) had lower odds of being daily smokers compared to nonsmokers by Time 4 compared to Time 1, controlling for all other demographic and attitudinal factors associated with smoking (Table 2).
Table 2. Daily and nondaily smoking among Partiers over 3 years of smoke-free intervention.
| Partiers with HAVOC recall | Partiers without HAVOC recall | |
|---|---|---|
|
|
|
|
| aOR (95% CI) | aOR (95% CI) | |
| Predictors of being a daily smoker (vs. nonsmoker) | ||
| Age | .86 (.71–1.04) | .92 (.83–1.03) |
| Race | — | — |
| White | 4.01 (1.86–8.67)a | 1.75 (1.15–2.67)a |
| Other | .68 (.21–2.18) | .96 (.53–1.75) |
| Hispanic (ref) | — | — |
| Education | — | — |
| HS only/college dropout | 1.97 (.62–6.19) | 2.01 (1.30–3.10)a |
| In college | 1.46 (.51–4.15) | 1.08 (.58–1.99) |
| College graduate (ref) | — | — |
| Male sex | .78 (.37–1.61) | .84 (.56–1.27) |
| LGB sexual orientation | .92 (.36–2.33) | 1.63 (.92–2.81) |
| Anti-industry attitude | .62 (.45–.87)a | .61 (.51–.73)a |
| Social Prioritization Index | 1.03 (.92–1.15) | 1.04 (.97–1.12) |
| Tobacco advertising receptivity | 1.83 (.80–4.19) | 1.39 (.92–2.13) |
| Binge drinking in past 30 days | 1.32 (.54–3.21) | 4.84 (2.29–10.22)a |
| Duration since intervention start (over three years) | .41 (.19–.84)a | .56 (.36–.89)a |
| Predictors of being a nondaily smoker (vs. nonsmoker) | ||
| Age | 1.06 (.93–1.17) | .96 (.90–1.03) |
| Race | — | — |
| White | .81 (.44–1.49) | .72 (.52–1.00) |
| Other | .83 (.43–1.60) | .92 (.62–1.37) |
| Hispanic (ref) | — | — |
| Education | — | — |
| HS only/college dropout | 1.36 (.66–2.49) | 1.42 (.89–2.60) |
| In college | .94 (.49–1.62) | 1.16 (.68–1.03) |
| College graduate (ref) | — | — |
| Male sex | 1.31 (.80–1.98) | 1.27 (.95–1.72) |
| LGB sexual orientationb | 1.62 (.89–2.93) | 1.74 (1.15–2.64)a |
| Anti-industry attitude | .76 (.62–.90)a | .91 (.82–1.02) |
| Social Prioritization Index | 1.05 (.97–1.14) | 1.02 (.97–1.07) |
| Tobacco advertising receptivity | 1.47 (.81–2.64) | 1.50 (1.07–2.10)a |
| Binge drinking in past 30 days | 2.12 (1.17–3.50)a | 1.70 (1.20–2.43)a |
| Duration since intervention start (over three years) | .61 (.36–1.01) | .91 (.82–1.02) |
aOR = adjusted odds ratio.
Denotes statistical significance (p < .05).
Lesbian, gay, bisexual.
Table 3. Daily and nondaily smoking among non-Partiers over 3 years of smokefree intervention.
| Non-Partiers with HAVOC recall | Non-Partiers without HAVOC recall | |
|---|---|---|
|
|
|
|
| aOR (95% CI) | aOR (95% CI) | |
| Predictors of being a daily smoker (vs. nonsmoker) | ||
| Age | 1.10 (.92–1.31) | 1.01 (.94–1.09) |
| Race | — | — |
| White | .77 (.33–1.79) | 1.61 (1.16–2.22)a |
| Other | 1.10 (.43–2.82) | 1.47 (.96–2.25) |
| Hispanic (ref) | — | — |
| Education | — | — |
| HS only/college dropout | 1.07 (.40–2.86) | 2.04 (1.35–3.09)a |
| In college | .43 (.18–1.01) | .99 (.68–1.44) |
| College graduate (ref) | — | — |
| Male sex | 1.03 (.48–2.22) | .97 (.72–1.31) |
| LGB sexual orientation | .97 (.40–2.32) | 1.18 (.78–1.77) |
| Anti-industry attitude | .64 (.44–.94)a | .62 (.54–.72)a |
| Social Prioritization Index | .96 (.84–1.09) | 1.10 (1.04–1.15)a |
| Tobacco advertising receptivity | 2.53 (1.14–5.62)a | 1.89 (1.39–2.57)a |
| Binge drinking in past 30 days | 2.15 (.68–6.82) | 1.89 (1.29–2.76)a |
| Duration since intervention start (over three years) | .73 (.36–1.47) | .75 (.54–1.10) |
| Predictors of being a non-daily smoker (vs. nonsmoker) | ||
| Age | .87 (.77–.98)a | .99 (.93–1.05) |
| Race | — | — |
| White | 1.21 (.69–2.09) | .86 (.68–1.10) |
| Other | .78 (.41–1.48) | 1.38 (1.01–1.89)a |
| Hispanic (ref) | — | — |
| Education | — | — |
| HS only/college dropout | .96 (.44–2.09) | .90 (.64–1.27) |
| In college | 1.12 (.60–2.08) | 1.20 (.91–1.58) |
| College graduate (ref) | — | — |
| Male sex | 1.25 (.76–2.06) | 1.15 (.98–1.44) |
| LGB sexual orientationb | 2.18 (1.20–3.98)a | 1.96 (1.45–2.64)a |
| Anti-industry attitude | .77 (.62–.96)a | .82 (.74–.90)a |
| Social Prioritization Index | 1.04 (.96–1.14) | 1.05 (1.01–1.09)a |
| Tobacco advertising receptivity | 2.47 (1.43–4.25)a | 1.34 (1.04–1.72)a |
| Binge drinking in past 30 days | 2.27 (1.21–4.29)a | 2.07 (1.59–2.69)a |
| Duration since intervention start (over three years) | .76 (.47–1.23) | 1.02 (.81–1.32) |
aOR = adjusted odds ratio.
Denotes statistical significance (p < .05).
Lesbian, gay, bisexual.
Daily or nondaily smoking did not change significantly among non-Partiers during the intervention (Table 3).
Subgroup analysis: association of HAVOC liking and understanding with smoking
For individuals with HAVOC recall (n = 747), the degree of liking and understanding HAVOC was related to smoking status. Specifically, individuals in the group that recalled HAVOC, liked it and understood it (group 3) had lower odds of being both nondaily (adjusted OR: .48, 95% CI: .31–.75) or daily smokers (adjusted OR: .31, 95% CI: .14–.68) than those who recalled HAVOC but did not like or understand it, controlling for age, race/ethnicity, sex, LGB, and education (data not shown in tables).
Subgroup analysis: smoking-related attitudes and HAVOC recall
For individuals with HAVOC recall, five variables thought to be related to smoking were evaluated in univariable and multivariable models as potential mediators between recall and smoking behavior. In univariable models, group status based on recall, liking, and understanding was related to tobacco advertising receptivity, anti-industry attitudes, perceived peer prevalence of smoking, perceived smoking in places where the individual parties, and being able to relate to reasons not to smoke cigarettes (p < .05). Specifically, individuals in Groups 2 (recall, like, or understand) and 3 (recall, like, and understand) had higher anti-industry attitudes and higher ability to relate to reasons not to smoke than those who recalled HAVOC but did not like or understand it. Odds of advertising receptivity were lower in Group 3 compared to Group 1 (HAVOC recall, but did not like or understand).
Subgroup analysis: relationship of smoking attitudes with smoking status
We then examined whether the smoking attitudes associated with HAVOC recall were related to smoking status. In univariable models, individuals with higher tobacco advertising receptivity, lower anti-industry attitudes, higher perceived peer prevalence of smoking, higher perceived smoking in places that the individual parties, and lower ability to relate to reasons not to smoke had higher odds of being nondaily smokers compared to non-smokers (Table 4). For daily smoking, those with higher tobacco advertising receptivity, lower anti-industry attitudes, higher perceived peer prevalence of smoking, and lower ability to relate to reasons not to smoke had higher odds of being daily smokers compared to nonsmokers (Table 4).
Table 4. Potential mediators of smoking status among individuals with HAVOC recall.
| Potential mediator | Univariable OR (95% CI) | Multivariable aOR (95% CI) |
|---|---|---|
| Daily smoking | ||
| Perceived peer prevalence | 1.34 (1.21–1.49)a | 1.01 (.99–1.01) |
| Anti-industry attitude | .49 (.39–.63)a | .59 (.43–.80)a |
| Tobacco advertising receptivity | 5.54 (3.18–9.66)a | 2.93 (1.43–6.03)a |
| In places I party, people are smoking tobacco | 1.18 (.78–1.80) | .50 (.28–.77)a |
| I can relate to reasons not to smoke cigarettes (reverse coded) | 1.53 (1.07–2.18)a | .71 (.43–1.18) |
| Nondaily smoking | ||
| Perceived peer prevalence | 1.10 (1.04–1.19)a | 1.00 (.99–1.00) |
| Anti-industry attitude | .63 (.55–.73)a | .86 (.72–1.04) |
| Tobacco advertising receptivity | 4.36 (2.90–6.54)a | 1.88 (1.13–3.13)a |
| In places I party, people are smoking tobacco | 1.39 (1.07–1.81)a | 1.91 (1.39–2.62)a |
| I can relate to reasons not to smoke cigarettes (reverse coded) | 1.48 (1.18–1.86)a | 1.64 (1.20–2.24)a |
Denotes statistical significance (p < .05).
In a second step, all these variables were included in a multivariable model that also included demographics (age, sex, race/ethnicity, LGB, and education). Odds of nondaily smoking compared to nonsmoking were higher for those with tobacco advertising receptivity, higher perceived smoking in places that the individual parties, and lower ability to relate to reasons not to smoking cigarettes. Daily smoking was associated with higher advertising receptivity, lower anti-industry attitudes, and lower perceived smoking in places where the individual parties compared to nonsmoking (Table 4).
Discussion
Current cigarette smoking prevalence among young adult bar patrons during a bar and nightclub-based Social Branding intervention in Albuquerque, New Mexico, decreased from 47.5% at Time 1 to37.5% at Time 4. Specifically, daily smoking decreased among Partiers, the target population of the intervention, over time. While the study was limited by lack of a comparison community, the decrease in smoking was only observed among Partiers, while young adults surveyed in bars but who did not associate with the Partier crowd (who might be considered a comparison) had no change in smoking behavior. A previous Social Branding intervention targeting a different peer crowd (“Hipsters”) of this age group in San Diego, California was also associated with a significant reduction in current smoking over time [19]. In addition, while an intervention targeting the Partier peer crowd in Oklahoma was not associated with a significant change in smoking prevalence overall, Partiers who recalled HAVOC had decreased odds of daily smoking and unchanged nondaily smoking, while Partiers and non-Partiers who did not recall HAVOC had increased odds of smoking over time [20]. Further exploring potential factors associated with Social Branding interventions in bars and smoking prevalence, an intervention focused on Lesbian, Gay, Bisexual, or Transgender (LGBT) bar culture in young adults in Las Vegas, Nevada, found that higher intervention exposure was associated with decreased smoking among individuals who understood the smoke-free message of the intervention [21].
In this study, we aimed to expand upon the associations seen in previous Social Branding studies by exploring some of the different factors associated with the campaign and their association with campaign exposure. With longer intervention duration, participants' exposure to the intervention, liking of the intervention, and interest in attending intervention events increased. This highlights the improved reach of the campaign and the appeal to young adults. Partiers who recalled HAVOC had the highest smoking rates at Time 1 and lower rates at Time 2–4 (Figure 1). One explanation for this may be that the HAVOC intervention is designed to appeal to high risk young adults, so that early high smoking rates might indicate appeal to the correct target audience. In addition, for the first several months, HAVOC promotions do not contain any smoke-free messaging. The subsequent lower smoking rates among those who recall HAVOC suggests an association between the brand and smoking behavior, but its direction cannot be determined from cross sectional data.
Almost two thirds of participants who recalled HAVOC understood its smoke-free message. In subgroup analyses, participants who recalled HAVOC, liked it, and understood its smoke-free message had lower odds of daily and nondaily smoking than those who recalled HAVOC but did not like or understand it. This suggests that liking and understanding of the smoke-free message may be important factors in the association between HAVOC recall and lower smoking prevalence, and this finding is consistent with McGuire's input-output framework for persuasive communication, which identifies recall and liking as mediators between persuasive messaging and behavior change [38].
Anti-tobacco industry attitudes, tobacco advertising receptivity, and perceived smoking in places that participants party may be potential mediators to further explore in the association between intervention recall and smoking status. These factors were significantly associated with HAVOC recall and smoking behavior, and they may be particularly important to emphasize in the specific messaging of the campaign. For example, HAVOC media and materials could more specifically focus on educating individuals on deceptive tobacco industry advertising practices or by emphasizing the decreasing popularity of smoking within the Partier culture [11].
Few interventions address smoking among young adults who have graduated or dropped out of college or young adults without a college education [39]. Almost half of the young adults in this study were not attending college. This study is consistent with others [40] showing a strong association between binge drinking and smoking and showing higher rates of cigarette smoking (over 35%) than the national average for adults (17.8%) and adults aged 18–24 (18.7%) in 2013 [5]. Therefore, interventions in bars may efficiently reach young adults at higher risk for smoking. We monitored rates of binge drinking during the Social Branding intervention and found that odds of binge drinking did not increase (and actually decreased); this finding is consistent with Social Branding interventions in other locations [19,20].
This study is subject to a number of limitations. Data were collected through a series of cross-sectional surveys; therefore, longitudinal trends in cigarette smoking could not be assessed among the same individuals. Similarly, mediation could not be formally assessed although we identified promising candidate mediators for subsequent longitudinal studies. In addition, we did not have a control city to which to compare secular trends in smoking rates. Given that data were collected in bars and nightclubs in Albuquerque, the results may not be generalizable to young adults who do not attend bars or those in other cities. Results were consistent with those from San Diego, CA, Oklahoma City, OK, and Las Vegas, NV; however, suggesting Social Branding is a promising strategy in diverse contexts. Smoking and binge drinking rates were obtained by self-report; therefore, recall bias may be present. Reverse causality may also be present given the cross sectional nature of data collection in this study. While participants were screened for eligibility, it is possible that the same individuals took the survey more than once over the four years of data collection. Finally, since the venues, dates, and time of data collection were randomly selected, it is possible that bar patrons with different demographic characteristics were sampled at different time points, and while many of these factors were controlled for in analyses, it is possible that uncontrolled confounders could have influenced the results.
This study adds to the evidence that Social branding interventions aimed at young adult bar patrons may help reduce smoking rates in this population. Bar-based interventions tailored to specific peer crowd values and lifestyles are an efficient way to address risky behaviors among high-risk young adults.
Supplementary Material
Implications and Contribution.
During a Social Branding intervention targeting young adult bar patrons in New Mexico, decreased daily smoking rates were associated with intervention recall and understanding. As also suggested by Social Branding interventions in other cities, such interventions may help to decrease tobacco use in this population.
Acknowledgments
The authors thank the New Mexico Department of Health's Tobacco Use Prevention and Control Program for funding the HAVOC young adult tobacco intervention efforts. This work was presented as a poster at the 2014 National Meeting of the Society for General Internal Medicine. The study sponsors had no role in study design; collection, analysis, and interpretation of data; writing the report; or the decision to submit the report for publication.
Funding Sources: This work was supported by NIH NRSA T32HP19025 (Kalkhoran), National Cancer Institute (U01-154240), and New Mexico Department of Health's Tobacco Use Prevention and Control Program.
Footnotes
Conflicts of Interest: J.J. is an employee of Rescue, the company that implemented the HAVOC intervention in Albuquerque. S.K., N.E.L., T.B.N., and P.M.L. have no competing interests to declare.
Disclaimer: The content is solely the responsibility of the authors and does not necessarily represent the official views of the National Institutes of Health. Everyone who has made a significant contribution to the study has been mentioned in the acknowledgments.
Supplementary Data: Supplementary data related to this article can be found at http://dx.doi.org/10.1016/j.jadohealth.2016.04.003.
References
- 1.US Department of Health and Human Services. Preventing tobacco use among youth and young adults: A report of the surgeon general. Atlanta, GA: U.S. Department of Health and Human Services, Centers for Disease Control and Prevention, National Center on Chronic Disease Prevention and Health Promotion, Office on Smoking and Health; 2012. [Google Scholar]
- 2.Jha P, Ramasundarahettige C, Landsman V, et al. 21st-century hazards of smoking and benefits of cessation in the united states. N Engl J Med. 2013;368:341–50. doi: 10.1056/NEJMsa1211128. [DOI] [PubMed] [Google Scholar]
- 3.Doll R, Peto R, Boreham J, Sutherland I. Mortality in relation to smoking: 50 years' observations on male British doctors. BMJ. 2004;328:1519. doi: 10.1136/bmj.38142.554479.AE. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4. [Accessed May 6, 2014];New mexico department of health, indicator-based information system for public health. [cited May 6, 2014]; Available at: http://ibis.health.state.nm.us.
- 5.Jamal A, Agaku IT, O'Connor E, et al. Current cigarette smoking among adults - United states, 2005-2013. MMWR Morb Mortal Wkly Rep. 2014;63:1108–12. [PMC free article] [PubMed] [Google Scholar]
- 6.Ling PM, Glantz SA. Why and how the tobacco industry sells cigarettes to young adults: Evidence from industry documents. Am J Public Health. 2002;92:908–16. doi: 10.2105/ajph.92.6.908. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Ridner SL, Myers JA, Hahn EJ, Ciszewski TN. College students' exposure to tobacco marketing in nightclubs and bars. J Am Coll Health. 2010;59:159–64. doi: 10.1080/07448481.2010.483716. [DOI] [PubMed] [Google Scholar]
- 8.Sepe E, Ling PM, Glantz SA. Smooth moves: Bar and nightclub tobacco promotions that target young adults. Am J Public Health. 2002;92:414–9. doi: 10.2105/ajph.92.3.414. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Sepe E, Glantz SA. Bar and club tobacco promotions in the alternative press: Targeting young adults. Am J Public Health. 2002;92:75–8. doi: 10.2105/ajph.92.1.75. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Kalkhoran S, Neilands TB, Ling PM. Secondhand smoke exposure and smoking behavior among young adult bar patrons. Am J Public Health. 2013;103:2048–55. doi: 10.2105/AJPH.2013.301287. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Villanti AC, McKay HS, Abrams DB, et al. Smoking-cessation interventions for U.S. Young adults: A systematic review. Am J Prev Med. 2010;39:564–74. doi: 10.1016/j.amepre.2010.08.009. [DOI] [PubMed] [Google Scholar]
- 12.Suls JM, Luger TM, Curry SJ, et al. Efficacy of smoking-cessation interventions for young adults: A meta-analysis. Am J Prev Med. 2012;42:655–62. doi: 10.1016/j.amepre.2012.02.013. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Farrelly MC, Nonnemaker J, Davis KC, Hussin A. The influence of the national truth campaign on smoking initiation. Am J Prev Med. 2009;36(5):379–84. doi: 10.1016/j.amepre.2009.01.019. [DOI] [PubMed] [Google Scholar]
- 14.Richardson AK, Green M, Xiao H, et al. Evidence for truth®: The young adult response to a youth-focused anti-smoking media campaign. Am J Prev Med. 2010;39:500–6. doi: 10.1016/j.amepre.2010.08.007. [DOI] [PubMed] [Google Scholar]
- 15.Green KJ, Hunter CM, Bray RM, et al. Peer and role model influences for cigarette smoking in a young adult military population. Nicotine Tob Res. 2008;10:1533–41. doi: 10.1080/14622200802398763. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Evans WD, Hastings G. Public health branding: Applying marketing for social change. Oxford, UK: Oxford University Press; 2008. [Google Scholar]
- 17.Asbury LD, Wong FL, Price SM, Nolin MJ. The verb campaign: Applying a branding strategy in public health. Am J Prev Med. 2008;34(6 Suppl):S183–7. doi: 10.1016/j.amepre.2008.03.010. [DOI] [PubMed] [Google Scholar]
- 18.Evans WD, Price S, Blahut S. Evaluating the truth brand. J Health Commun. 2005;10:181–92. doi: 10.1080/10810730590915137. [DOI] [PubMed] [Google Scholar]
- 19.Ling PM, Lee YO, Hong J, et al. Social branding to decrease smoking among young adults in bars. Am J Public Health. 2014;104:751–60. doi: 10.2105/AJPH.2013.301666. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Fallin A, Neilands TB, Jordan JW, et al. Wreaking “havoc” on smoking: Social branding to reach young adult “partiers” in Oklahoma. Am J Prev Med. 2015;48(1 Suppl. 1):S78–85. doi: 10.1016/j.amepre.2014.09.008. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Fallin A, Neilands TB, Jordan JW, Ling PM. Social branding to decrease lesbian, gay, bisexual, and transgender young adult smoking. Nicotine Tob Res. 2015;17:983–9. doi: 10.1093/ntr/ntu265. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Lee YO, Jordan JW, Djakaria M, Ling PM. Using peer crowds to segment black youth for smoking intervention. Health Promot Pract. 2014;15:530–7. doi: 10.1177/1524839913484470. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Campbell R, Starkey F, Holliday J, et al. An informal school-based peer-led intervention for smoking prevention in adolescence (assist): A cluster randomised trial. Lancet (London, England) 2008;371:1595–602. doi: 10.1016/S0140-6736(08)60692-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Kelly JA. Popular opinion leaders and HIV prevention peer education: Resolving discrepant findings, and implications for the development of effective community programmes. AIDS Care. 2004;16:139–50. doi: 10.1080/09540120410001640986. [DOI] [PubMed] [Google Scholar]
- 25.Raymond H, Ick T, Grasso M, et al. Resource guide: Time location sampling (tls) San Francisco, CA: San Francisco Department of Public Health, HIV Epidemiology Section, Behavioral Surveillance Unit; 2010. [Google Scholar]
- 26.Muhib FB, Lin LS, Stueve A, et al. A venue-based method for sampling hard-to-reach populations. Public Health Rep. 2001;116(Suppl. 1):216–22. doi: 10.1093/phr/116.S1.216. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Magnani R, Sabin K, Saidel T, Heckathorn D. Review of sampling hard-to-reach and hidden populations for HIV surveillance. AIDS. 2005;19(Suppl 2):S67–72. doi: 10.1097/01.aids.0000172879.20628.e1. [DOI] [PubMed] [Google Scholar]
- 28.Kalkhoran S, Padilla JL, Neilands TB, Ling PM. Multiple tobacco product use among young adult bar patrons in New Mexico. Prev Med. 2016;83:16–21. doi: 10.1016/j.ypmed.2015.11.024. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Gilpin EA, White MM, Messer K, Pierce JP. Receptivity to tobacco advertising and promotions among young adolescents as a predictor of established smoking in young adulthood. Am J Public Health. 2007;97:1489–95. doi: 10.2105/AJPH.2005.070359. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Ling PM, Neilands TB, Glantz SA. The effect of support for action against the tobacco industry on smoking among young adults. Am J Public Health. 2007;97:1449–56. doi: 10.2105/AJPH.2006.098806. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Ling PM, Neilands TB, Glantz SA. Young adult smoking behavior: A national survey. Am J Prev Med. 2009;36:389–394e2. doi: 10.1016/j.amepre.2009.01.028. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Lisha NE, Neilands TB, Jordan JW, et al. The social prioritization index and tobacco use among young adult bar patrons. Health Educ Behav. 2015 doi: 10.1177/1090198115621867. Epub ahead of print. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Graham JW, Taylor BJ, Olchowski AE, Cumsille PE. Planned missing data designs in psychological research. Psychol Methods. 2006;11:323–43. doi: 10.1037/1082-989X.11.4.323. [DOI] [PubMed] [Google Scholar]
- 34.Collins LM, Schafer JL, Kam CM. A comparison of inclusive and restrictive strategies in modern missing data procedures. Psychol Methods. 2001;6:330. [PubMed] [Google Scholar]
- 35.Rubin DB. Inference and missing data. Biometrika. 1976;63:581–92. [Google Scholar]
- 36.Little RJA, Rubin DB. Statistical analysis with missing data. New York, NY: Wiley; 1987. [Google Scholar]
- 37.McArdle JJ, Hamagami F. Modeling incomplete longitudinal and cross-sectional data using latent growth structural models. Exp Aging Res. 1992;18:145–66. doi: 10.1080/03610739208253917. [DOI] [PubMed] [Google Scholar]
- 38.McGuire WJ. McGuire's classic input-output framework for constructing persuasive messages. In: Rice RE, Atkins CK, editors. Public Communication Campaigns. 4th. Los Angeles: Sage; 2013. [Google Scholar]
- 39.Green MP, McCausland KL, Xiao H, et al. A closer look at smoking among young adults: Where tobacco control should focus its attention. Am J Public Health. 2007;97:1427–33. doi: 10.2105/AJPH.2006.103945. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Jiang N, Lee YO, Ling PM. Association between tobacco and alcohol use among young adult bar patrons: A cross-sectional study in three cities. BMC Public Health. 2014;14:500. doi: 10.1186/1471-2458-14-500. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.


