Supplemental digital content is available in the text.
Key Words: OLDER ADULTS, PHYSICAL ACTIVITY, ACCELEROMETER, FALLS, MOBILITY LIMITATIONS, COHORT STUDY
ABSTRACT
Background
Physical activity (PA) has many health benefits but may increase falls risk among older adults. We study how objectively measured habitual daily PA is related to falls by exploring the modifying effect of mobility limitations and the mediating roles of fitness and lower-limb strength.
Methods
One thousand six hundred fifty-five (53%) of 3137 surviving participants (men age 71–91 yr) in an ongoing UK-population-based cohort study wore an ActiGraph GT3x accelerometer over the hip for 1 wk in 2010–2012 to measure PA (exposure) and reported demographic and health status, including mobility limitations. One year later, 825 men reported falls history (outcome).
Results
Seven hundred of 825 men had ≥600 min·d−1 of accelerometer wear for ≥3 d. Nineteen percent (n = 128) reported falls 1 yr later. Associations between PA and falls differed by presence of mobility limitations. Among 66% (n = 471) of men without mobility limitations, number of falls increased incrementally (for every 30 min of moderate to vigorous PA [MVPA]: incidence rate ratio [IRR], 1.50; 95% confidence interval [CI], 1.10–2.03, adjusted for falls risk factors). Step count was not related to number of falls below 9000 steps per day but was related to number of falls ≥9000 steps per day (for every additional 1000 steps per day: IRR, 1.59; 95% CI, 1.16–2.18). Among 33% (n = 229) of men with mobility limitations, falls risk declined with increasing activity (for every 1000 steps per day: IRR, 0.80; 95% CI, 0.70–0.91; for every 30 min of MVPA: IRR, 0.61; 95% CI, 0.42–0.89; for every additional 30 min of sedentary behavior ≥600 min·d−1: IRR, 1.22; 95% CI, 1.07–1.40).
Conclusions
Interventions to promote MVPA in older men should incorporate falls prevention strategies. Among adults with mobility limitations, trials should investigate whether increasing MVPA levels can reduce falls risk.
Physical activity (PA) reduces the risk of many important causes of morbidity and mortality in older adults and helps to maintain good mobility and functioning (8). Older adults have the lowest PA levels of any age group (1,2,10,12,38), but PA promotion must also consider potential adverse consequences, including falls and associated injuries. One quarter to one third of community-dwelling individuals older than 65 yr fall each year (4,37). With increasing longevity worldwide, falls prevention is a global public health challenge (42).
Epidemiologic studies have identified many risk factors for falling in older people—the most consistent being abnormal gait and poor balance (16). Trials have demonstrated that these physiological deficits can be improved with exercise programs including a sufficient dose (>50 h) of moderate- to high-balance challenging activities (33). Yet, in practice, very few older people habitually engage in these planned and structured exercise programs. Instead, older adults derive their daily PA mostly from unstructured lifestyle PA, which includes functional activities such as walking for transport or recreation, household chores and gardening, and caring or volunteering work (14). Understanding how habitual activity relates to falls has important public health implications for PA recommendations.
Prospective studies of older adults have investigated how self-reported PA (from questionnaires) is related to falls, but findings have been inconsistent. Some studies reported that only high levels of moderate-intensity to vigorous-intensity PA reduce the risk of falls (22,30,36). Conversely, others reported that high PA levels increase the risk of falls (7), whereas others reported that both high and low PA levels raise the risk of falls (29), resulting in the hypothesis that there may be a U-shaped association where falls risk is elevated both among older adults who are very active (perhaps due to increased exposure to environmental risks) and also older adults who are very inactive (perhaps due to poorer muscle strength, coordination, and balance). The relationship between PA and falls may differ according to functional abilities and age: among oldest-old individuals (>80 yr), those with lower PA levels were at increased risk for falls, whereas among younger-old individuals (<80 yr) (6) and those with better functional ability (stronger leg strength) (7), higher PA levels were associated with increased falls risk.
Inconsistencies in findings about the shape of the dose–response relationship between PA and falls may partly be due to limitations of prior studies, including how PA was measured (e.g., examining just one PA domain, such as leisure), use of self-reported PA (resulting in misclassification biases), and inadequate control of confounders (18). Some of these limitations can be overcome using objective measures of PA. We therefore use data from hip-worn accelerometers to investigate how objectively measured PA is prospectively related to onset of falls. To our knowledge, this is the first study to do so. Given the importance of understanding dose–response relationships for formulating PA guidelines, we investigate i) the shape of associations between total amount and intensity of PA and occurrence of falls; ii) whether associations between PA levels and risk of falls differ by age and mobility status; and iii) the role of selected mediators. We study these questions using a sample of community-dwelling older adults who were part of an ongoing cohort study including oldest-old individuals in order to better understand these associations in a representative sample of community-dwelling adults.
METHODS
Study Population
The British Regional Heart Study is an ongoing prospective cohort. A total of 7735 free-living men (age 40–59 yr) were recruited from a single primary care center in each of 24 British towns in 1978–1980 and were followed up repeatedly. In 1998–2000, participants (age 60–79 yr) completed a questionnaire, providing information on habitual PA (77% response rate) (40). For the purposes of this article, the baseline time point is 2010–2012, when 3137 surviving community-dwelling men were invited to attend a physical examination, to complete questionnaires, and to participate in a study of objectively measured PA. One year later, the men were sent a questionnaire where they reported falls history. The National Research Ethics Service Committee for London provided ethical approval. Participants provided a written informed consent for the investigation, which was performed in accordance with the Declaration of Helsinki.
Measures
Baseline accelerometer data
In 2010–2012, participants were asked to wear the GT3x accelerometer (ActiGraph, Pensacola, FL) over the right hip on an elasticated belt for 7 d during waking hours, removing it when swimming or bathing. The data collected were processed using standard methods; raw data collected from movements registering on the vertical axis were integrated into 60-s periods (epochs). Nonwear time was identified and excluded using a commonly used and freely available computer package “Physical Activity” (9). Valid wear days were defined as ≥600 min of wear time; participants with three or more valid days were included in the analysis, a conventional requirement to estimate usual PA levels (13,19,20). The number of minutes per day spent in PA of different intensity levels was categorized using standard count-based intensity threshold values (counts per minute) developed for older adults (11): <100 for sedentary behavior (SB) (<1.5 METs), 100–1040 for light activity (1.5–3 METs), and ≥1040 for moderate to vigorous PA (MVPA) (>3 METs). The following variables were used as exposure: steps per day (to indicate total volume of activity); minutes per day of sedentary time, light PA, and MVPA in 1-min bouts; and minutes per day of MVPA accumulated in 10-min bouts (to indicate intensity of activity). For each PA variable, the mean value for all valid days over the week was averaged to obtain an average per valid day. Coefficients were scaled to 1000 steps and 30 min of sedentary time, light PA, and MVPA for ease of interpretation in regression models.
Baseline covariate data
In 2010–2012, men completed questionnaires including the following questions: i) “At the present time, are you afraid that you may fall over?” [very fearful, somewhat fearful, not fearful]; responses to a similar single question on fear of falling correlate with validated scales, including the Falls Efficacy Scale and the Survey of Activities and Fear of Falling in the Elderly scale (25); and ii) “Do you have any difficulties getting about outdoors?” [no difficulty vs slight difficulty, moderate difficulty, severe difficulty, unable to do]. Men were identified as having vision problems if they reported suffering from macular degeneration, glaucoma, or cataract. The number of chronic conditions (in the following list) that men suffered from was recorded: “heart attack, heart failure, angina, other heart trouble, diabetes, stroke, osteoporosis, claudication, Parkinson’s disease, and arthritis affecting knees, hips, or feet.” Men completed the four-item Geriatric Depression Score; those scoring ≥2 were classified as depressed. Men reported whether they lived alone or with others. They completed the Duke Activity Status Index (DASI) fitness scale (a series of questions on the ability to do increasingly strenuous activities) from which a fitness score estimating peak V˙O2 was calculated (23). Nurses administered a sit-to-stand test, recording the number of times within a timed 30-s period that men could sit down on a chair and stand up again without using their hands.
Habitual PA level was self-reported on a questionnaire completed 10 yr earlier (1998–2000); a six-point PA score based on self-reported usual walking, cycling, and sporting and recreational activities was validated against forced expiratory volume in 1 s and heart rate (41). Social position was based on the longest-held occupation reported in previous surveys (classified as manual or nonmanual).
Outcome data
Men were followed up (2011–2013) 1 yr after the accelerometer survey and completed a questionnaire. Men were asked: “Have you had a fall in the past 12 months?” [yes/no] and “If yes, how many falls have you had in the past 12 months?” This question has high specificity and acceptable sensitivity for detecting falls in the previous 12 months (17).
Statistical Methods
Summary measures of baseline demographic and social variables were calculated according to history of falls in the past 12 months. Linear regression models tested differences in continuous variables across three groups (nonfallers, single fallers, and recurrent fallers); differences in categorical variables were tested using chi-square test. The same approach was taken to compare men with mobility limitations and men without mobility limitations.
Number of falls was highly positively skewed (mean, 0.4; variance, 3.3), indicating overdispersed data. Therefore, negative binomial models were used; these are comparable to Poisson regression in terms of mean structure but have an extra parameter to model overdispersion (3). The incidence rate ratio (IRR) for total number of falls over the year (range, 0–40) was estimated for each PA measure. Interactions between each PA variable and i) mobility limitations (no difficulty vs some difficulty, moderate difficulty, severe difficulty getting about outdoors) and ii) age (under vs over 80 yr) were tested by fitting an interaction term and testing model fit with a likelihood ratio test. When significant interactions were detected, analyses were stratified.
Using a negative binomial generalized additive model (GAM), we investigated the hypothesis that the association between PA and number of falls may be nonlinear. GAM is a nonparametric model that permits nonlinear relationships to be modeled flexibly without specifying the nonlinear functional form. This modeling approach is an extension of the generalized linear model, where parametric regression terms are replaced by nonparametric functions such as scatterplot smoothers (21). We used GAM to approximate the synergistic contribution of a number of covariates, such as PA levels and participant characteristics, to the response variable (number of falls after 1 yr) without making any a priori assumptions about the underlying processes or trends, which may be highly complex. Analyses were performed using the “mgcv” package in R (version 2.15.3; ©2013, The R Foundation for Statistical Computing) (21,31,43). The best-fit GAM was chosen based on the Akaike information criterion and by using the lowest number of degrees of freedom if the Akaike information criterion score was approximately the same. Predictions from GAM were plotted and restricted to the central 95% of the data because data were very sparse at the extremes of the distribution (although all data were retained in regression models).
Next, we assessed the role of mediators between each PA variable and onset of falls. For linear associations, negative binomial models with PA variables fitted as linear variables were used. For nonlinear associations, we used the Stata function “mkspline” to model associations between PA and risk of falls, specifying one knot at a point selected based on the shape of the association seen in GAM. The spline model provides an estimate of the association before and after the turning point of the function (knot). To evaluate the role of potential mediators, we adjusted model 1 for confounders: age, region of residence, season of accelerometer wear, and accelerometer wear time (minutes per day). Model 2 additionally included history of falls at baseline. Model 3 additionally included risk factors for falls: number of chronic diseases, number of medications, depression, vision problems (presence of glaucoma, macular degeneration, or cataract), and living alone. Model 4 included the DASI as a measure of fitness, and model 5 included the sit-to-stand test as an indicator of lower-limb strength. Analyses were conducted in Stata version 13 (35). Sensitivity analyses i) used a higher cutpoint of 1952 counts per minute, which was calibrated to identify MVPA in middle-age (rather than older) adults and is widely used (15); and ii) compared single fallers to nonfallers and recurrent fallers to nonfallers to evaluate the importance of recurrent falls.
RESULTS
A total of 3137 surviving men were invited to attend a clinic-based rescreen in 2010–2012, of which 1655 (52%) agreed to attend the clinic-based rescreen and to wear an accelerometer. Of these, 1566 (95%) returned the accelerometer. The sample was restricted to 1455 (88%) of 1655 community-dwelling men (living at home, i.e., excluding residents of care homes) who did not report being confined to a chair and had ≥600 min of accelerometer wear time for 3–7 d (mean age, 78.3 yr; range, 71–93 yr). Among these men, 940 (65%) of 1455 provided follow-up data 10–14 months later, of whom 700 (74%) of 940 had complete covariate data (Table, Supplemental Digital Content 1, Flow chart for participants in study at baseline and follow-up, http://links.lww.com/MSS/A522). Comparing the 700 participants retained in the analysis to men who completed the 2010–2012 questionnaires but were not included in the analysis, those retained were more active (62% vs 52% self-reported light or greater PA 10 yr earlier; P < 0.001) and less likely to have fallen once or more at baseline in 2010–2012 (16% vs 19%; P = 0.03).
Participant characteristics
Among the 700 ambulatory men at 1-yr follow-up, 9% (n = 61) reported one fall in the previous 12 months and 10% (n = 67) had recurrent falls (range, 2–40; only two men fell >10 times). Among fallers, the median number of falls was 2 (interquartile range [IQR], 1–3) per man. Characteristics of the analysis sample (overall and stratified by falls at 1-yr follow-up) are reported in Table 1. Single fallers had more characteristics similar to those of nonfallers. However, compared to nonfallers and single fallers, recurrent fallers were older, were more often from the manual social class, had more chronic diseases, had higher prevalence of fear of falling, vision problems and depression, and were more likely to live alone. Recurrent fallers had lower scores on the sit-to-stand test (weaker lower-limb strength) and lower DASI fitness scores. They had lower activity levels (total counts, steps, MVPA, and less SB) than single fallers and nonfallers.
TABLE 1.
Baseline characteristics of 700 men who reported falls history at 1-yr follow-up and baseline mobility limitations.
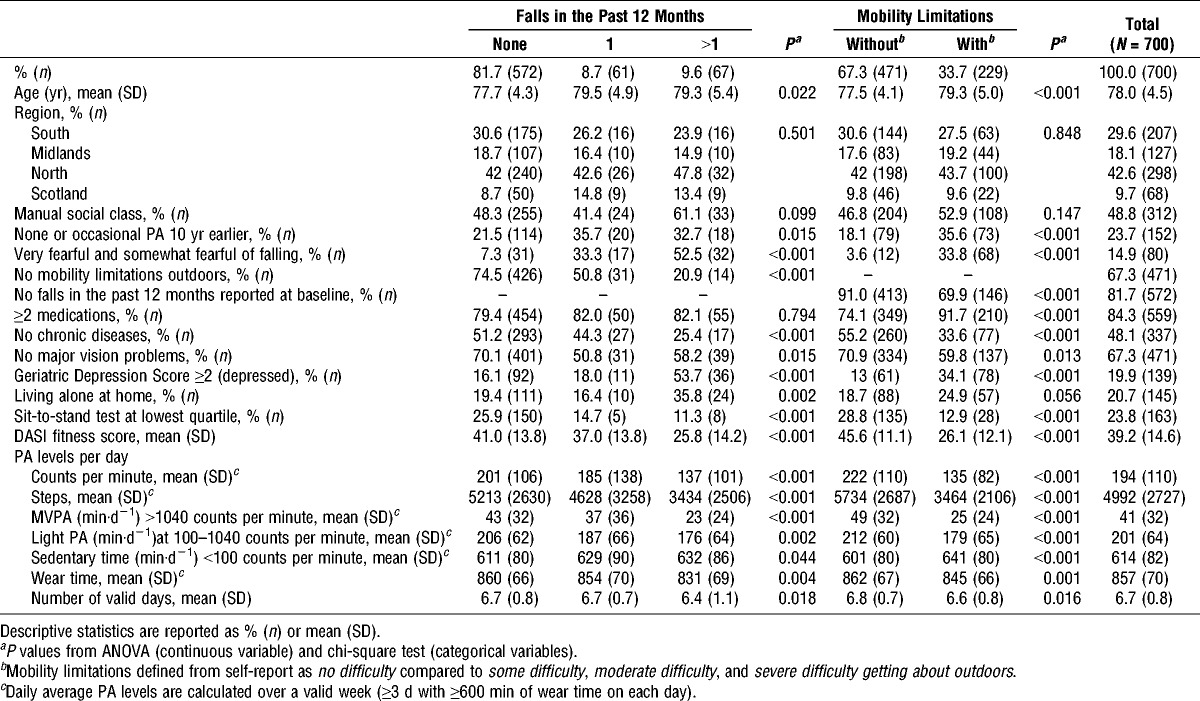
Table 1 presents the characteristics of 66% (n = 471) of men who reported that they had no problems getting about outdoors and 33% (n = 229) of men who reported slight to severe mobility problems outdoors. Men with no mobility difficulties had higher scores on the sit-to-stand test (better lower-limb strength) and higher DASI fitness scores. They took more steps per day (5734 vs 3464 steps per day; P < 0.01) and spent more time in light PA and MVPA and less time in SB than did men with mobility difficulties. Men reporting mobility limitations also reported more difficulties with activities of daily living (Table, Supplemental Digital 2, Characteristics of men with and without mobility limitations, http://links.lww.com/MSS/A523).
Associations between PA and number of falls in men with and without mobility limitations
Associations between baseline PA levels (step counts, sedentary time, light PA, and MVPA) and number of falls differed by presence of mobility limitations (likelihood ratio test for interaction, P < 0.05 for all PA types). However, there was no evidence of interaction with age group (<80 vs ≥80 yr) (likelihood ratio test for interaction, P > 0.05 in each case). Models were therefore stratified by mobility limitations.
The shape of the associations between each PA measure and number of falls was investigated using GAM. Figures 1 and 2 present predicted estimates and 95% confidence intervals (CI) from GAM stratified by mobility limitations and adjusted for falls risk factors (baseline number of falls, age, body mass index [BMI], number of chronic diseases, number of medications, depression, vision problems, and living alone) and measurement-related confounders (wear time, region, and season). In men with no mobility limitations, higher activity levels (step counts and 1-min or 10-min bouts of MVPA; Fig. 1A, C, E) were associated with increased risk of more falls, whereas the trend of higher number of falls at lower levels of SB was not statistically significant (Fig. 2C). The opposite pattern was seen for men with mobility limitations; lower activity levels (step counts and 1-min or 10-min bouts of MVPA; Fig. 1B, D, F) and more time in SB were related to higher risk of more falls (Fig. 2D). There was a trend for light PA being associated with falls risk in the same direction as MVPA, although more weakly; however, this did not reach statistical significance in either mobility limitations group (Fig. 2A, B). A visual examination of the plots indicated that there was little suggestion of nonlinear associations, with the exception of the association between step count and number of falls in men without mobility limitations; men with the highest step counts had increased risks of more falls. At around 9000 steps per day, the lower 95% CI crossed the risk of one fall (indicating that the risk increases significantly) and the risk increased rapidly thereafter; at around 11,000 steps per day, the risk had doubled to two falls. However, only 12% of participants took over 9000 steps per day. The other potential nonlinear association was between sedentary time and number of falls among men with mobility limitations: risk of falls began to rise after ≥600 min·d−1 of sedentary time (this level of SB was reached by 72% of participants). In these two cases, we then investigated whether categorical variables—high step count (≥9000 steps per day compared to less) and sedentary time (≥600 min·d−1 compared to less)—were associated with falls.
FIGURE 1.
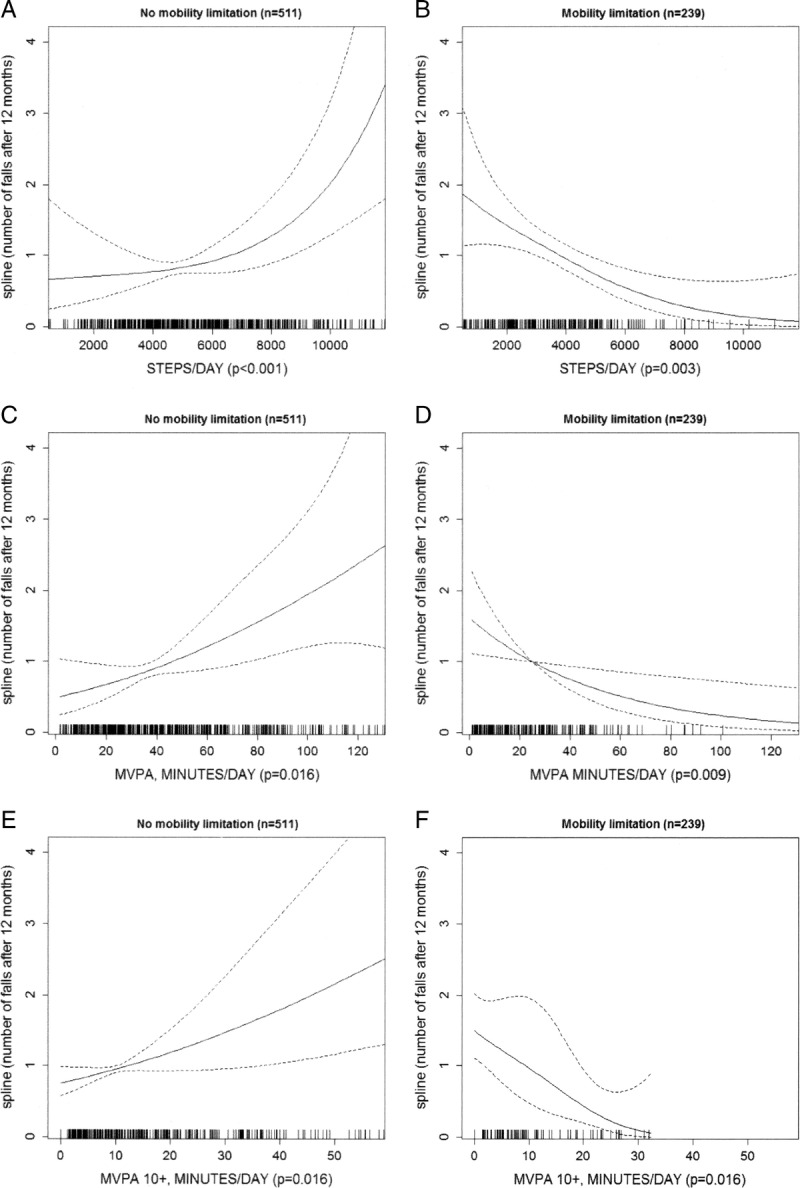
Relationships between steps per day (panels A and B) and daily minutes of MVPA (accumulated in single minutes in panels C and D, and accumulated in bouts lasting 10 minutes or more in panels E and F) and number of falls, stratified by mobility limitations (no mobility limitations vs slight/moderate/severe mobility limitations). For each PA level, smoothed function from GAM, 95% CI (dotted lines), and P values are reported. Each model is adjusted for wear time, age, region, season, number of falls at baseline, living alone, BMI, number of chronic diseases, depression, vision problems, and use of medications.
FIGURE 2.
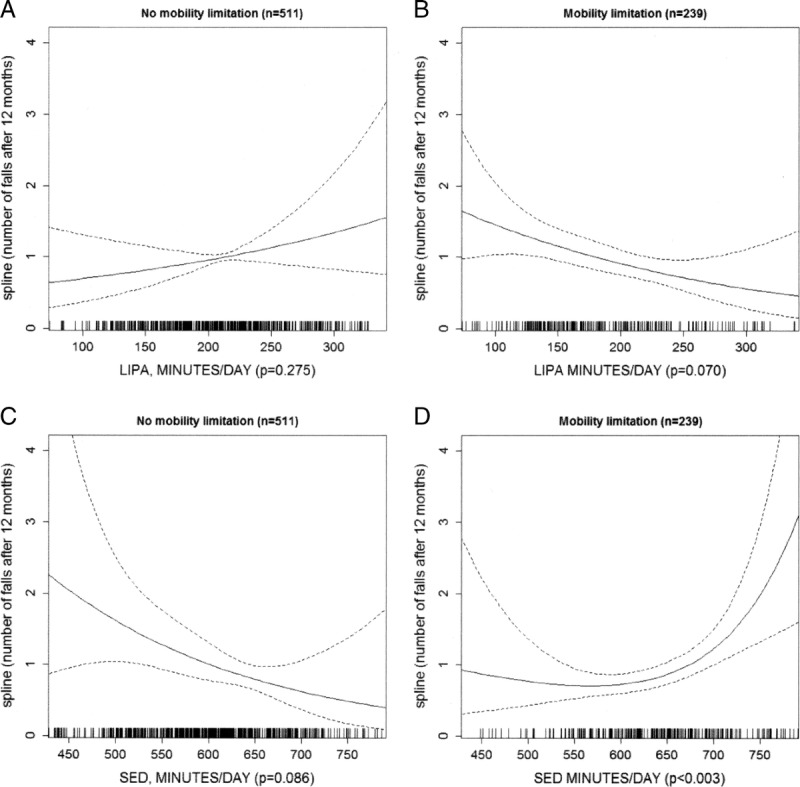
Relationships between daily minutes of light-intensity physical activity (LIPA) (panels A and B) and sedentary time (SED) (panels C and D) and number of falls, stratified by mobility limitations (no mobility limitations vs slight/moderate/severe mobility limitations). For each PA level, smoothed function from GAM, 95% CI (dotted lines), and P values are reported. Each model is adjusted for wear time, age, region, season, number of falls at baseline, living alone, BMI, number of chronic diseases, depression, vision problems, and use of medications.
Table 2 presents continuous associations indicating the strength of association between each PA measure and number of falls. Models were sequentially adjusted for measurement-related confounders (model 1) and falls history (model 2). Further adjustments for falls risk factors (model 3) and potential mediators (models 4 and 5) changed the strength of associations very little. Therefore, model 3 (adjusted for falls risk factors) is discussed here. Among men with no mobility problems, there was no evidence that light activity or SB was related to falls (Table 2). However, each 30 min of MVPA (accumulated in 1-min bouts) was associated with an IRR for falls of 1.50 (95% CI, 1.10–2.03) (Table 2, model 3). MVPA accumulated in ≥10-min bouts was even more strongly related to number of falls (IRR, 1.97; 95% CI, 1.20–3.22). In sensitivity analyses using a higher cutpoint of 1952 counts per minute to define MVPA, the IRR was 1.98 (95% CI, 1.28–3.08). Further adjustments for mediators—DASI fitness scale (model 4) and sit-to-stand test (model 5)—changed the estimates very little. Higher step count was associated with increased risk of more falls; however, given that GAM suggested a nonlinear association, negative binomial regression models using a spline with a knot at 9000 steps per day are presented in Table 3. There was no significant association between steps per day and falls risk for men taking <9000 steps per day (IRR, 1.03; 95% CI, 0.85–1.24), whereas the IRR for falls was 1.59 (95% CI, 1.16–2.18) for every 1000 steps, starting at 9000 steps per day (Table 3, model 3). Step count was related to MVPA level (MVPA >1040 counts per minute): geometric mean of 106 min·d−1 (IQR, 88–128) in men taking ≥9000 steps per day versus geometric mean of 38 min·d−1 (IQR, 22–56) in men taking <9000 steps per day.
TABLE 2.
Associations between baseline PA and onset of falls (N = 700 men).
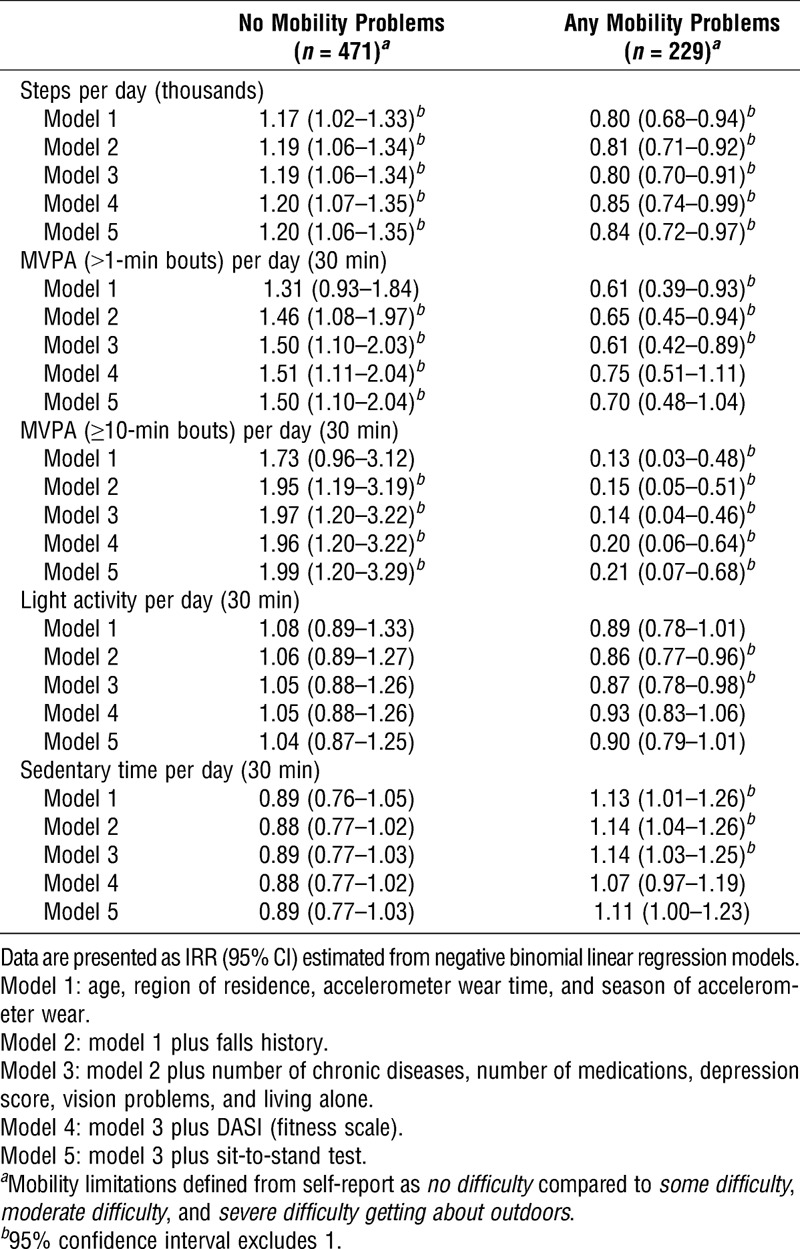
TABLE 3.
Associations between baseline PA level and onset of falls: steps per day and falls in 471 men with no mobility limitations, and sedentary time (minutes per day) and falls in 229 men with mobility limitations.
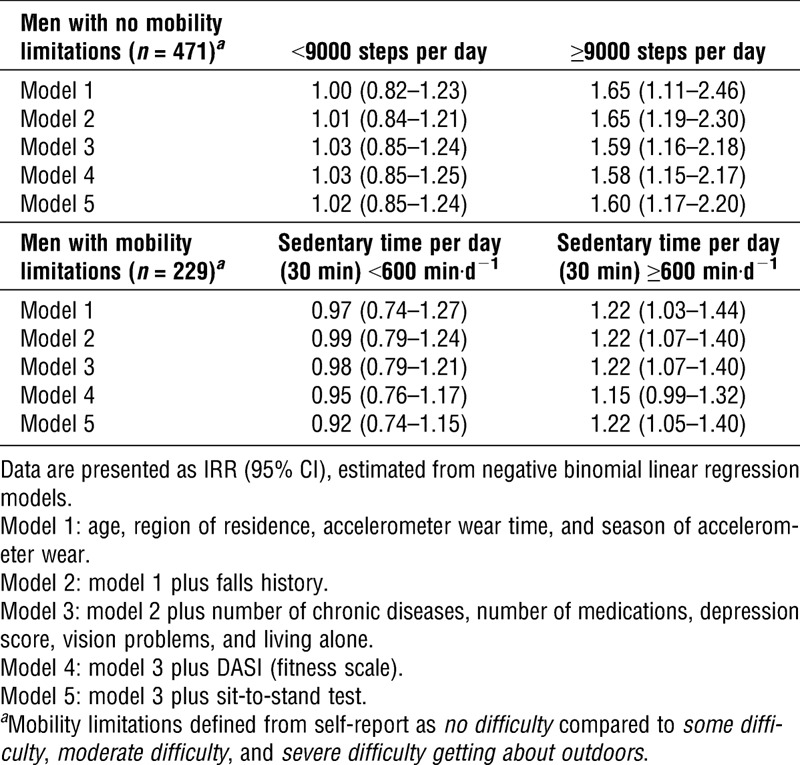
The associations between PA and number of falls were in the opposite direction among men with self-reported mobility problems. Higher step counts and MVPA levels were associated with reduced risks of falls, and higher sedentary time was associated with increased risks of falls. For number of falls, the values are as follows: IRR, 0.80 (95% CI, 0.70–0.91) for every 1000 steps per day (Table 2, model 3); IRR, 0.87 (95% CI, 0.78–098) for every 30 min of light activity; IRR, 0.61 (95% CI, 0.42–0.89) for every 30 min of MVPA accumulated in 1-min bouts; IRR, 0.14 (95% CI, 0.04–0.46) for MVPA accumulated in ≥10-min bouts. In sensitivity analyses using the higher cutpoint of ≥1952 counts per minute for MVPA, the IRR was 0.29 (95% CI, 0.12–0.69). Further adjustments for DASI fitness scale (model 4) and sit-to-stand test (model 5) slightly attenuated the associations between steps and long bouts of MVPA with number of falls. The associations of both light PA and short bouts of MVPA with number of falls were fully attenuated upon adjustment for DASI and sit-to-stand test. Overall, higher levels of SB were related to higher IRR for falls (for every 30 min·d−1 of SB: IRR, 1.14; 95% CI, 1.03–1.25) (Table 2). However, given that GAM identified a nonlinear relationship, Table 3 presents a spline regression model using a knot at 600 min·d−1 SB. No significant association between SB and falls risk (IRR, 0.98; 95% CI, 0.79–1.21) was observed for men with <600 min·d−1 of SB; however, for more sedentary men, the IRR for falls was 1.22 (95% CI, 1.07–1.40) for every 30 min of SB starting at 600 min·d−1 (Table 3, model 3). The increased risk was totally mediated upon adjustment for DASI score (Table 3, model 4), but not for sit-to-stand test (Table 3, model 5).
Sensitivity analyses comparing single fallers to nonfallers and recurrent fallers to nonfallers suggest that the associations were not strongly influenced by individuals with many falls.
DISCUSSION
In this study of free-living older men, the associations between PA levels and subsequent risk of falls depended on mobility status. Among men without mobility problems (who were a more active group), there was an incremental increase in number of falls (IRR, 1.5) for every 30-min increase in MVPA. There was a steeper increase in number of falls at the highest step counts (≥9000 steps per day, a level achieved by only the most active 10% of the study sample), but lower step counts were not related to falls risk. Conversely, among men with mobility limitations, number of falls increased incrementally with lower step counts and lower levels of MVPA, and a nonlinear association between falls risk and SB was observed; SB >10 h·d−1 was associated with steeper increases in number of falls.
How our findings fit with other studies
Based on existing literature (7), we hypothesized that the association between PA and falls may differ by mobility limitations, and we found this to be the case. PA could either increase or decrease falls risk, depending on functional status, which may explain prior findings of a U-shaped relation between PA and falls risk (18,29). One unifying explanation for these opposite relationships may be that highly active individuals perform beyond their abilities (7). Men with mobility limitations may be more aware of their physical capacities or exercise under practitioners’ supervision or guidance due to their limitations; hence, activity workload is proportional to their abilities and provides the expected benefits preventing falls. In contrast, men without mobility limitations may expose themselves to greater risk either by being too fatigued to initiate corrective responses to prevent falls or by engaging in activities that do not suit their age and abilities. It is also possible that people with mobility limitations may perform types of activities different from those performed by people without limitations (accelerometer data are informative about duration intensity and frequency—but not type—of activity); if the activity has an inherently different risk of injury (e.g., if walking had a lower risk than gardening), this could account for the different associations between activity level and risk of falls in the groups defined by mobility limitations.
Men with mobility limitations
Men with mobility limitations were less active than men without mobility limitations. Among men with mobility limitations, higher step counts, light PA, and MVPA were associated with lower number of falls. Number of falls declined by around 15% for every 30 min of light activity and by 40% for MVPA in bouts lasting 1 min, and the reduction was even greater for MVPA in ≥10-min bouts. However, for adults with difficulties getting about outdoors, doing 30 min·d−1 of MVPA in ≥10-min bouts would be especially hard, as this level of activity is unlikely to occur indoors. The associations between light PA and MVPA and number of falls were not much mediated by falls history (except for MVPA levels) but were mediated, in part, by lower fitness levels and weaker lower-limb strength. Men with mobility limitations had lower baseline levels of fitness and weaker lower-limb strength than men without limitations and thus may have more potential to gain from PA. Indeed, lower-limb weakness is reported to be an important predictor of falls (27), and increasing muscle strength may prevent falls, in part, due to better central and peripheral neural functions, which may in turn improve balance (32). However, aerobic fitness is not considered an important fitness dimension for fall prevention (33). We observed that higher levels of SB were associated with increased number of falls, particularly for SB >10 h·d−1. The effect is in the same direction as prior observational studies of self-reported SB (36), although most studies just reported SB as low PA level rather than asking about sedentary activities. To our knowledge, the only other study that investigated objectively measured SB in relation to falls used an arm-worn monitor rather than a hip-worn monitor. Although results were not statistically significant, that study found that the associations were in the same direction as in our study; among men older than 80 yr, higher levels of SB were associated with higher risks of falls (6). Caution may be needed in interpreting findings in men with mobility limitations in that the degree of inactivity may in fact be a sensitive indicator of the severity of the disabling disease and that people with such a condition (who will also have limited strength) will be more likely to fall. We addressed this issue in the analyses by adjusting for the presence of a wide range of chronic conditions.
Men without mobility limitations
Among men without mobility limitations, very high levels of activity were associated with higher risks of falls, potentially due to men stretching themselves beyond their abilities and exposing themselves to greater fatigue and, hence, risk of falls. The finding about higher step counts increasing the risk of falls fits with the findings of a meta-analysis, which showed that walking attenuated the beneficial effect of exercise programs on falls prevention and that high amounts of walking (>3 h·wk−1), but not total MVPA level, increased the incidence of fractures (28,33). Similarly, in the Osteoporotic Fractures in Men cohort, the strongest men in the highest quintiles of household activities were at the highest risk for falling (7). We did not see clear evidence that physical capabilities were important mediators between PA and falls risk in men without mobility limitations, perhaps because they already had higher baseline levels of lower-limb strength and aerobic fitness.
We learned from other prospective studies that PA is important for preventing the development of mobility limitations (39), which may in turn contribute to risk of falls. Although we did not aim to investigate whether higher activity levels were associated with reductions in the prevalence of mobility limitations in this study, we did find that 65% of men who reported mobility limitations at baseline also reported mobility limitations 1 yr later.
Strengths and limitations
The study sample is a prospective study drawn from a community-dwelling cohort of older men spanning a 20-yr age range, rather than a special “at-risk” clinical population, which permitted us to investigate interactions between PA and both age and presence of mobility problems on falls risk. Our sample size is larger than those of previously published studies of objectively measured PA in older adults, and our study also benefits from extensive data on covariates that are risk factors for falls or mediators. Uniquely, the study benefits from using objectively measured PA at baseline. To our knowledge, this is the first study to investigate how objectively measured SB, using a hip-worn sensor, is prospectively related to risk of falls. To date, only one prospective study has investigated, using the arm-mounted Sensewear accelerometer, how objectively measured PA is related to risk of falls (6), but the comparability of Sensewear data with the most commonly used and validated hip-mounted accelerometer is unknown. Although accelerometers have the benefit of measuring intensity of PA, the type of activity that generated the MVPA was not recorded; hence, we are unable to determine whether the association with MVPA is type- or volume-dependent. This is important because of the different effects of MVPA on falls risk in those with or without mobility limitations; if people with mobility limitations were aware of their risk and therefore derived MVPA from safer activities in a safe setting, then the protective effect could be due to type of activity rather than volume. Our response rate was 52%, which was higher than those in other accelerometer studies of older adults: 21% (13) and 43% (19); in the Health Survey for England, 37% of women and 48% of men over 75 yr had four or more days with valid data (12). However, after restrictions, our analytic sample was smaller, which could introduce some selection bias. Although it is likely that physically inactive and immobile men are underrepresented, this will not necessarily affect the observed associations between PA and falls risk. Our study is limited to men, who, based on existing literature, would be expected to have lower rates of falls and higher levels of PA, particularly MVPA, compared to women (24). Therefore, our results may not be generalizable to older women. Prevalence of falls was a little lower in our study than in other studies (26), which may be partly explained by the male sample or by selection bias, as healthier individuals were more likely to participate and be followed up (we found that men with accelerometer data who were followed up had higher self-reported PA levels and lower prevalence of falls compared to men who only completed the baseline questionnaire in 2010–2012). Our assessment of falls at follow-up is a retrospective question about the past year and, thus, is not a truly prospective assessment, which may result in underreporting of falls compared to studies that use prospective monthly fall diaries; any nondifferential underreporting should bias the results toward the null hypothesis, which may mean that our estimates of associations are conservative. A review of studies investigating the effects of duration of recall period for falls reporting found that recall of falls over the previous year was specific (specificity, 91%–95%) although less sensitive (sensitivity, 80%–89%) than the gold standard of prospective data collection (fall calendars or postcards) (17).
Policy implications
PA has a wide range of benefits for many health outcomes and is encouraged by public health guidelines. One of the few potential side effects is accident/injury; older adults are at the highest risk for falls, which can have serious health and social consequences on subsequent long-term rehabilitation and care both for fallers and for the society. Programs that encourage older adults with no mobility limitations to be physically active may need to incorporate falls prevention strategies to avoid excess falls, particularly among the most active individuals. Older adults mostly have low activity levels, and our data suggest that moderate increases in PA (especially light PA and overall step count) would have a very small impact on falls risk. However, if policies will focus on increasing MVPA (which is needed to achieve national PA guidelines), the need to include falls prevention measures alongside PA intervention will become more critical. To date, the most effective falls prevention programs (Otago, Falls Management Exercise, etc) (5,34) incorporate balance challenge activities; this may be an important aspect of PA that is not fully addressed by encouraging walking. Additionally, awareness of and educational strategies for falls prevention in older adults may play a role in encouraging individuals to perform within reasonable activity levels. Future interventions could investigate whether programs that encourage more PA and less SB may help reduce the risk of falls in adults who report mobility limitations outdoors.
We stratified our sample using a simple one-item self-report of mobility problems outdoors—a question that could easily be used in primary care practice to screen for mobility problems. The results of the question were highly related to reports of problems with activities of daily living and thus have content validity. This question could therefore be used as a screening question to identify older adults who may have increased risk of falls if they are highly active and have no mobility problems or, conversely, older adults who may have reduced risk of falls if they are highly active but have mobility limitations.
CONCLUSIONS
PA has multiple health benefits for older adults who are at high risk for diseases that can be ameliorated by PA. Activities that reduce the risk of falls, such as balance challenge activities (current UK PA guidelines recommend that balance challenge activities be performed twice a week), should be encouraged in highly active older adults who have no mobility impairments in order to reduce the risks of falls. Our findings can help shape public health recommendations for older adults without mobility limitations. However, among older adults with mobility limitations who have low levels of activity, our results suggest that future trials could investigate whether interventions increasing time spent in ambulation and reducing sedentary time may prevent falls, and whether increasing moderate to vigorous activities that raise heart rate and induce breathlessness might be particularly effective at reducing the risk of falls. Although we have described the associations between different intensities of activities and number of falls, we do not know exactly what type of activities were carried out. Thus, further research is needed to understand relationships between types of activities (e.g., walking, gardening, bowling) and falls.
Supplementary Material
Acknowledgments
We acknowledge the British Regional Heart Study team for data collection.
B. J. Jefferis and C. Sartini were funded by a National Institute for Health Research Postdoctoral Fellowship (PDF-2010-03-23 to B. J. Jefferis). The British Regional Heart Study was supported by a British Heart Foundation program grant (RG/08/013/25942). The analyses presented here were supported by National Institute for Health Research National School of Primary Care project number 80. D. Merom was supported by a National Health and Medical Research Council (Australia) Postdoctoral Fellowship (571150).
The National Institute for Health Research and the British Heart Foundation had no role in the design and conduct of the study; collection, management, analysis, and interpretation of the data; preparation, review, or approval of the manuscript; and decision to submit the manuscript for publication. The views expressed in this publication are those of the authors and not necessarily those of the National Institute for Health Research and the British Heart Foundation.
The authors report no conflicts of interest.
The results of the present study do not constitute endorsement by the American College of Sports Medicine.
Footnotes
Supplemental digital content is available for this article. Direct URL citations appear in the printed text and are provided in the HTML and PDF versions of this article on the journal’s Web site (www.acsm-msse.org).
REFERENCES
- 1. Ashe MC, Miller WC, Eng JJ, Noreau L. Older adults, chronic disease and leisure-time physical activity. Gerontology. 2009; 55: 64– 72. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2. Baptista F, Santos DA, Silva AM, et al. Prevalence of the Portuguese population attaining sufficient physical activity. Med Sci Sports Exerc. 2012; 44(3): 466– 73. [DOI] [PubMed] [Google Scholar]
- 3. Cameron AC, Trivedi PK. Basic count regression. In: Regression Analysis of Count Data. Cambridge: Cambridge University Press; 2013. pp. 69– 109. [Google Scholar]
- 4. Campbell AJ, Borrie MJ, Spears GF, Jackson SL, Brown JS, Fitzgerald JL. Circumstances and consequences of falls experienced by a community population 70 years and over during a prospective study. Age Ageing. 1990; 19(2): 136– 41. [DOI] [PubMed] [Google Scholar]
- 5. Campbell AJ, Robertson MC, Gardner MM, Norton RN, Tilyard MW, Buchner DM. Randomised controlled trial of a general practice programme of home based exercise to prevent falls in elderly women. BMJ. 1997; 315(7115): 1065– 9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6. Cauley JA, Harrison SL, Cawthon PM, et al. Objective measures of physical activity, fractures and falls: the Osteoporotic Fractures in Men Study. J Am Geriatr Soc. 2013; 61(7): 1080– 8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7. Chan BK, Marshall LM, Winters KM, Faulkner KA, Schwartz AV, Orwoll ES. Incident fall risk and physical activity and physical performance among older men: the Osteoporotic Fractures in Men Study. Am J Epidemiol. 2007; 165(6): 696– 703. [DOI] [PubMed] [Google Scholar]
- 8. Chodzko-Zajko WJ, Proctor DN, Fiatarone Singh MA, et al. American College of Sports Medicine Position Stand: exercise and physical activity for older adults. Med Sci Sports Exerc. 2009; 41(7): 1510– 30. [DOI] [PubMed] [Google Scholar]
- 9. Choi L, Liu Z, Matthews C, Buchowski MS. Physical Activity: Process Physical Activity Accelerometer Data (computer program). 2011. [Google Scholar]
- 10. Colley RC, Garriguet D, Janssen I, Craig CL, Clarke J, Tremblay MS. Physical activity of Canadian adults: accelerometer results from the 2007 to 2009 Canadian Health Measures Survey. Health Rep. 2011; 22(1): 7– 14. [PubMed] [Google Scholar]
- 11. Copeland JL, Esliger DW. Accelerometer assessment of physical activity in active, healthy older adults. J Aging Phys Act. 2009; 17(1): 17– 30. [DOI] [PubMed] [Google Scholar]
- 12. Craig R, Mindell J, Hirani V. Health Survey for England 2008. Physical Activity and Fitness. Summary of Key Findings. London: The Health and Social Care Information Centre; 2009. pp. 5– 9 [Google Scholar]
- 13. Davis MG, Fox KR, Hillsdon M, Sharp DJ, Coulson JC, Thompson JL. Objectively measured physical activity in a diverse sample of older urban UK adults. Med Sci Sports Exerc. 2011; 43(4): 647– 54. [DOI] [PubMed] [Google Scholar]
- 14. DiPietro L. Physical activity in aging: changes in patterns and their relationship to health and function. J Gerontol A Biol Sci Med Sci. 2001; 56(2 Suppl): 13– 22. [DOI] [PubMed] [Google Scholar]
- 15. Freedson PS, Melanson E, Sirard J. Calibration of the Computer Science and Applications, Inc. accelerometer. Med Sci Sports Exerc. 1998; 30(5): 777– 81. [DOI] [PubMed] [Google Scholar]
- 16. Ganz DA, Bao Y, Shekelle PG, Rubenstein LZ. Will my patient fall? JAMA. 2007; 297(1): 77– 86. [DOI] [PubMed] [Google Scholar]
- 17. Ganz DA, Higashi T, Rubenstein LZ. Monitoring falls in cohort studies of community-dwelling older people: effect of the recall interval. J Am Geriatr Soc. 2005; 53(12): 2190– 4. [DOI] [PubMed] [Google Scholar]
- 18. Gregg EW, Pereira MA, Caspersen CJ. Physical activity, falls, and fractures among older adults: a review of the epidemiologic evidence. J Am Geriatr Soc. 2000; 48(8): 883– 93. [DOI] [PubMed] [Google Scholar]
- 19. Harris TJ, Owen CG, Victor CR, Adams R, Cook DG. What factors are associated with physical activity in older people, assessed objectively by accelerometry? Br J Sports Med. 2009; 43(6): 442– 50. [DOI] [PubMed] [Google Scholar]
- 20. Hart TL, Swartz AM, Cashin SE, Strath SJ. How many days of monitoring predict physical activity and sedentary behaviour in older adults? Int J Behav Nutr Phys Act. 2011; 8: 62. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21. Hastie TJ, Tibshirani RJ. Generalized Additive Models. Boca Raton (FL): Chapman and Hall; 1990. [Google Scholar]
- 22. Heesch KC, Byles JE, Brown WJ. Prospective association between physical activity and falls in community-dwelling older women. J Epidemiol Community Health. 2008; 62(5): 421– 6. [DOI] [PubMed] [Google Scholar]
- 23. Hlatky MA, Boineau RE, Higginbotham MB, et al. A brief self-administered questionnaire to determine functional capacity (the Duke Activity Status Index). Am J Cardiol. 1989; 64(10): 651– 4. [DOI] [PubMed] [Google Scholar]
- 24. Jefferis BJ, Sartini C, Lee IM, et al. Adherence to physical activity guidelines in older adults, using objectively measured physical activity in a population-based study. BMC Public Health. 2014; 14(1): 382. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25. Lachman ME, Howland J, Tennstedt S, Jette A, Assmann S, Peterson EW. Fear of falling and activity restriction: the Survey of Activities and Fear of Falling in the Elderly (SAFE). J Gerontol B Psychol Sci Soc Sci. 1998; 53(1): 43– 50. [DOI] [PubMed] [Google Scholar]
- 26. Masud T, Morris RO. Epidemiology of falls. Age Ageing. 2001; 30: 3– 7. [DOI] [PubMed] [Google Scholar]
- 27. Moreland JD, Richardson JA, Goldsmith CH, Clase CM. Muscle weakness and falls in older adults: a systematic review and meta-analysis. J Am Geriatr Soc. 2004; 52(7): 1121– 9. [DOI] [PubMed] [Google Scholar]
- 28. Nikander R, Gagnon C, Dunstan DW, et al. Frequent walking, but not total physical activity, is associated with increased fracture incidence: a 5-year follow-up of an Australian population-based prospective study (AusDiab). J Bone Miner Res. 2011; 26(7): 1638– 47. [DOI] [PubMed] [Google Scholar]
- 29. O’Loughlin JL, Robitaille Y, Boivin JF, Suissa S. Incidence of and risk factors for falls and injurious falls among the community-dwelling elderly. Am J Epidemiol. 1993; 137(3): 342– 54. [DOI] [PubMed] [Google Scholar]
- 30. Peeters GM, van Schoor NM, Pluijm SM, Deeg DJ, Lips P. Is there a U-shaped association between physical activity and falling in older persons? Osteoporos Int. 2010; 21(7): 1189– 95. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.R Core Team. R: A Language and Environment for Statistical Computing (computer program). 2013. [Google Scholar]
- 32. Sherrington C, Henschke N. Why does exercise reduce falls in older people? Unrecognised contributions to motor control and cognition? Br J Sports Med. 2013; 47(12): 730– 1. [DOI] [PubMed] [Google Scholar]
- 33. Sherrington C, Whitney JC, Lord SR, Herbert RD, Cumming RG, Close JC. Effective exercise for the prevention of falls: a systematic review and meta-analysis. J Am Geriatr Soc. 2008; 56(12): 2234– 43. [DOI] [PubMed] [Google Scholar]
- 34. Skelton D, Dinan S, Campbell M, Rutherford O. Tailored group exercise (Falls Management Exercise—FaME) reduces falls in community-dwelling older frequent fallers (an RCT). Age Ageing. 2005; 34(6): 636– 9. [DOI] [PubMed] [Google Scholar]
- 35.StataCorp. Stata Statistical Software: Release 13 (computer program). 2013. [Google Scholar]
- 36. Thibaud M, Bloch F, Tournoux-Facon C, et al. Impact of physical activity and sedentary behaviour on fall risks in older people: a systematic review and meta-analysis of observational studies. Eur Rev Aging Phys Act. 2012; 9(1): 5– 15. [Google Scholar]
- 37. Tinetti ME, Speechley M, Ginter SF. Risk factors for falls among elderly persons living in the community. N Engl J Med. 1988; 319(26): 1701– 7. [DOI] [PubMed] [Google Scholar]
- 38. Troiano RP, Berrigan D, Dodd KW, Masse LC, Tilert T, McDowell M. Physical activity in the United States measured by accelerometer. Med Sci Sports Exerc. 2008; 40(1): 181– 8. [DOI] [PubMed] [Google Scholar]
- 39. Visser M, Simonsick EM, Colbert LH, et al. Type and intensity of activity and risk of mobility limitation: the mediating role of muscle parameters. J Am Geriatr Soc. 2005; 53(5): 762– 70. [DOI] [PubMed] [Google Scholar]
- 40. Walker M, Whincup PH, Shaper AG. The British Regional Heart Study 1975–2004. Int J Epidemiol. 2004; 33(6): 1185– 92. [DOI] [PubMed] [Google Scholar]
- 41. Wannamethee SG, Lowe GD, Whincup PH, Rumley A, Walker M, Lennon L. Physical activity and hemostatic and inflammatory variables in elderly men. Circulation. 2002; 105(15): 1785– 90. [DOI] [PubMed] [Google Scholar]
- 42.WHO. WHO Global Report on Falls Prevention in Older Age. Geneva: WHO; 2007. p. 47. [Google Scholar]
- 43. Wood SN. GAMs with GCV/AIC/REML Smoothness Estimation and GAMMs by PQL (computer program). 2011. Available from: http://cran.r-project.org/web/packages/mgcv/ [cited 2014 January].
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.


