Abstract
Background:
Operative repair of distal biceps tendon ruptures has shown successful outcomes. However, little is known about the amount of tendon or repair site lengthening after repair.
Purpose/Hypothesis:
The purpose of this study was to evaluate distal biceps tendon repair via intratendinous radiostereometric analysis to analyze tendon lengthening at different time intervals of healing. The hypothesis was that there is significant lengthening after repair.
Study Design:
Case series; Level of evidence, 4.
Methods:
Eleven patients with distal biceps ruptures requiring operative repair were recruited. During repair, two 2-mm tantalum beads with laser-etched holes were sutured to the distal biceps tendon. Beads were evaluated via computed tomography scans immediately postoperatively and at 16 weeks. Radiographs were obtained at time 0 and then at 4, 8, and 16 weeks postoperatively. Measurements were made using the button-to-bead and bead-to-bead distances to assess repair site elongation as well as tendon elongation over time. After final follow-up, patients filled out the Disabilities of the Arm, Shoulder, and Hand (DASH) questionnaire and underwent ultrasound to confirm the integrity of the tendon.
Results:
Ten patients had complete ruptures, with 1 having a partial rupture that underwent completion of the tear and subsequent repair. All patients showed statistically significant lengthening after surgery. The mean amount of tendon lengthening after surgery was 22.8 mm (range, 11.2-30.9 mm; P < .05), and the repair site lengthened a mean 17.0 mm (range, 9.6-30.6 mm; P < .05) from surgery to final follow-up. The greatest change in lengthening was noted between time 0 and week 4 (mean, 11.3 mm; P < .05), with the least amount of lengthening between weeks 8 and 16 (mean, 2.6 mm; P < .05). The mean DASH score was 11.2. Final ultrasound evaluations found all tendons to be in continuity.
Conclusion:
All patients undergoing distal biceps tendon repair have significant elongation after surgery, with the greatest amount of lengthening seen in the early postoperative period.
Keywords: distal biceps, radiostereometric, tendon repair, tendon lengthening
Distal biceps tendon ruptures, commonly caused by an eccentric contraction at the elbow, are common injuries mostly seen in middle-aged men.6,13 The injury is most common in the dominant extremity, with less load to failure noted as the elbow moves toward a flexion angle of 90°.16 The pathogenesis leading to distal biceps ruptures has been proposed as mechanical impingement of the tendon during forearm rotation as well as a hypovascular zone contributing to attritional ruptures.15 As the incidence of distal biceps ruptures has shown increases from previous studies, the treatment of this condition is of continued importance.6
Treatment of distal biceps ruptures is focused on primarily regaining function, most specifically supination and flexion strength. Previous evaluations of patients treated nonoperatively showed satisfactory patient-reported outcomes; however, strength deficits in supination and flexion were noted.5 A previous biomechanical study by Morrey et al10 found a mean loss of 40% supination strength and 30% flexion strength, with more recent studies showing only 10% to 20% loss of flexion strength.5,14 Although nonoperative treatment is an option, surgical repair of the distal biceps tendon has been shown to result in better supination and flexion strength compared with nonoperative treatment.1,2,14
Typical protocols for rehabilitation after distal biceps repair involve a period of immobilization followed by passive elbow range of motion and progressive active elbow range of motion. More recent techniques with tendon fixation have led to more aggressive postoperative therapy protocols.9,12 Some recent studies have even advocated for immediate active range of motion and activities of daily living.3,19 However, no standard rehabilitation protocol exists for when to begin therapy after repair and when the repair is strong enough to begin active motion and, eventually, strengthening.
Radiostereometric analysis (RSA) has been a useful tool in orthopaedics that can accurately assess changes in distance with precision of less than 1 mm.4 RSA has commonly been used to measure wear in the arthroplasty literature; however, it has also been very reliable and useful for evaluating tendon and ligament healing following rotator cuff repairs and anterior cruciate ligament (ACL) reconstructions.4,7,8,17 However, little is known about tendon healing and tendon elongation/creep after distal biceps repair.
The purpose of this study was to serve as a primary study to evaluate the amount of tendon elongation seen in the distal biceps after repair. This was a study using RSA to evaluate changes seen over different time points of the repair with regard to tendon elongation over time as well as at the repair site. This was performed to give additional insight to the stages of distal biceps tendon healing after repair and to aid in various aspects of surgical planning, such as fixation technique, immobilization, and the physical therapy time frame.
Methods
This study was reviewed and approved by our institutional review board. Patients were eligible for inclusion if they had a distal biceps rupture requiring operative repair between July 2014 and August 2015. Patients with chronic tears, tears greater than 6 weeks old, and patients with significant medical comorbidities precluding surgery were excluded from the study.
Surgery was standardized to all patients in the study and performed by the senior authors (S.M. and V.M.). A single incision approach was utilized for repair. Tendon repair and fixation was performed using a button (Smith & Nephew) construct and the Krackow technique to secure the tendon using a No. 2 Fiberwire suture (Arthrex). The tendon was secured with the elbow flexed to the amount needed to allow the tendon to be secured in the radial tunnel with the greatest amount of tension. The button was confirmed in the flipped position using fluoroscopic assistance.
A novel technique was used to secure the radiopaque tantalum beads to the biceps tendon. Prior to sterilization, 2-mm tantalum beads had a laser-etched hole drilled to allow for passage of a suture. Two beads were placed during the operation, each secured to the tendon with suture fixation (4-0 Prolene; Ethicon) through the drill hole (Figure 1). One bead was placed at the insertion of the biceps tendon at the radius interface and the other bead placed approximately 1 cm proximal to the first bead (Figure 2).
Figure 1.
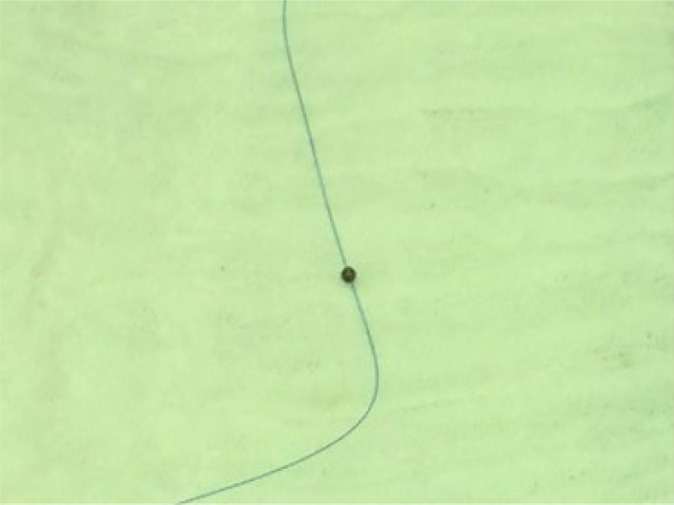
Two-mm tantalum bead with laser-etched hole drilled in the center to allow for suture passage.
Figure 2.

Tantalum beads secured to biceps tendon with 4-0 Prolene suture. The first bead was placed at the insertion of the tendon to the radius (left) and the second approximately 1 cm proximal (right).
Postoperatively, patients were placed into a posterior mold splint at 90° of flexion, which was removed at the first postoperative visit 7 to 10 days postoperatively. An immediate postoperative computed tomography (CT) scan of the elbow as well as radiographs were performed and represented time 0. CT scans were performed with the arm in the neutral position at 90° of flexion. A low-dose CT protocol with metal subtraction was used to limit radiation exposure. The CT cuts used were 1.25 mm. All images were then reformatted to align the beads and the button in 1 plane for appropriate measurement. This initial CT was used as the initial measurement, which allowed for specific bead placement distance intraoperatively to be less imperative. Follow-up radiographs were then obtained in the clinic at weeks 4, 8, and 16. Radiographs were taken using the lateral view for measurement, with the arm positioned at 90° of flexion and neutral rotation. A lateral view was deemed appropriate if there was appropriate overlap of the capitellum and trochlea of the humerus and the button was viewed in profile; if significant rotation was seen, then a repeat image was obtained. Magnification was determined using the known size of the beads as 2.0 mm, and measurements were calculated based on image magnification. A final CT scan was again performed at week 16. Ultrasound examinations were also performed and read by musculoskeletal fellowship–trained radiologists at final follow-up to confirm the integrity of the repair. The Disabilities of the Arm, Shoulder, and Hand (DASH) questionnaire was completed at the patient’s final follow-up visit. Formal strength testing was not routinely performed.
Postoperative protocols were standardized for all patients. Initial immobilization after surgery consisted of a posterior mold splint, with the elbow at 90° of flexion. After splint removal, patients were instructed to begin passive elbow range of motion and began physical therapy. Passive range of motion was limited to 30° to 120° of flexion. Passive supination and pronation were also allowed but not performed near full extension. Active supination as well as elbow flexion and extension were allowed at 3 weeks with no resistance and a goal of full extension at 6 weeks. Resistance exercises began at 6 weeks, with gradual increase in strengthening. Full return to vigorous labor/sports was allowed after 4 months, which was after the final follow-up visit for this study.
Measurements of tendon lengthening at the aforementioned time intervals were performed by measuring the button-to-bead distance as well as the bead-to-bead distance. The button-to–first bead distance was more representative of tendon healing or fixation laxity, whereas the bead-to-bead measurement indicated tendon elongation. The button-to–second bead distance represented overall tendon lengthening, with the first bead–to–second bead distance measuring the intratendinous lengthening. Measurements were taken at each time interval to evaluate whether more lengthening occurred early or late in the postoperative course. Changes in tendon lengthening were measured over time and compared with the initial time 0 measurements, with significant changes set at P < .05. Changes in lengthening of the tendon at final follow-up as well as changes seen between time intervals were correlated with final DASH scores using a correlation coefficient, with significance set at P < .05.
Results
Eleven patients were eligible and all consented to participate in the study. All patients were male (n = 11). The majority of patients were right-handed (n = 9), with 1 ambidextrous patient. The dominant arm was injured in 40% (4/10) of patients (Table 1). One patient had a partial rupture that was treated with completion of the tear and subsequent repair at the time of surgery; the remaining patients had complete rupture of the tendon, confirmed intraoperatively. All patients were found to have an intact biceps tendon repair at final follow-up, confirmed by clinical examination as well as ultrasound evaluation.
TABLE 1.
Patient Demographics (N = 11)
| Variable | Value |
|---|---|
| Age, y, mean (range) | 52.4 (40-62) |
| Male sex, n (%) | 11 (100) |
| Right-handed, n (%) | 9 (82) |
| Dominant arm injured, n (%)a | 4 of 10 (40) |
aOne patient was ambidextrous and injured the right elbow.
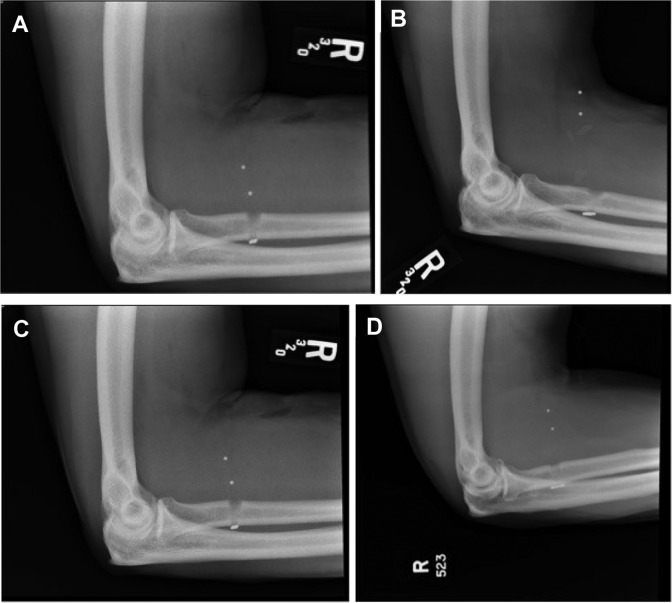
There was significant tendon lengthening throughout the follow-up period. Total tendon lengthening at the 16-week follow-up was a mean 22.8 mm (range, 11.2-30.9 mm; P < .05) (Table 2). Repair site lengthening (button to bead 1) averaged 17.0 mm (range, 9.6-30.6 mm; P < .05). Intratendinous lengthening (bead 1 to bead 2) averaged 6.2 mm (range, 0.3-17.7 mm; P < .05) (Table 3). The majority of repairs showed the greatest amount of lengthening through the repair site (button to bead 1); however, 2 of 11 (18%) patients had more lengthening through the tendon region (bead 1 to bead 2) (Table 3). Examples of radiographs showing the initial radiograph with beads in place compared with final follow-up evaluation are demonstrated in Figure 3.
TABLE 2.
Overall Tendon Elongation for Each Patient Showing Total Tendon Elongation as Well as Elongation at Different Postoperative Time Pointsa
| Patient | Tendon Elongation, mm | DASH Score | |||
|---|---|---|---|---|---|
| 0-4 wk | 4-8 wk | 8-16 wk | Total | ||
| 1 | 6.0 | 18.9 | 3.2 | 28.1 | 16.7 |
| 2 | 9.1 | 0.2 | 1.9 | 11.2 | 2.5 |
| 3 | 9.8 | 8.8 | 2.8 | 21.4 | 12.5 |
| 4 | 12.4 | 12.1 | 2.8 | 27.3 | N/Ac |
| 5 | 3.7 | 8.5 | 5.0 | 17.2 | 1.7 |
| 6 | 23.8 | 7.0 | 0.1 | 30.9 | 0.75 |
| 7b | 20.2 | 6.5 | 0.9 | 27.6 | 38 |
| 8 | 2.7 | 11.5 | 3.3 | 17.5 | 8.25 |
| 9 | 10.3 | 7.5 | 6.1 | 23.9 | 0 |
| 10 | 15.6 | 6.7 | 1.3 | 23.6 | N/Ac |
| 11 | 11.2 | 9.4 | 1.4 | 22.0 | 20 |
| Mean | 11.3 | 8.8 | 2.6 | 22.8 | 11.2 |
aDASH, Disabilities of the Arm, Shoulder, and Hand; N/A, not available.
bPatient with partial biceps rupture treated with completion and repair at surgery.
cPatient either unwilling or unavailable for DASH completion.
TABLE 3.
Distal Biceps Repair Elongation From Time 0 to Final 16-Week Follow-upa
| Elongation, mm | |||
|---|---|---|---|
| Patient | Repair Site (Button to Bead 1) | Intratendinous (Bead 1 to Bead 2) | Overall (Button to Bead 2) |
| 1 | 16.8 | 12.3 | 28.1 |
| 2 | 10.6 | 1.3 | 11.2 |
| 3 | 9.7 | 13.9 | 21.4 |
| 4 | 16.5 | 10.6 | 27.3 |
| 5 | 12.8 | 4.2 | 17.2 |
| 6 | 30.6 | 0.3 | 30.9 |
| 7b | 9.6 | 17.7 | 27.6 |
| 8 | 12.2 | 5.5 | 17.5 |
| 9 | 23.4 | 1.6 | 23.9 |
| 10 | 23.1 | 0.4 | 23.6 |
| 11 | 21.2 | 0.9 | 22.0 |
| Mean | 17.0 | 6.2 | 22.8 |
| P value | <.05 | <.05 | <.05 |
aElongation of the repair site (button to bead 1), elongation through the tendon (bead 1 to bead 2), and overall elongation (button to bead 2) are represented. The majority of the elongation was through the repair site, with a few cases showing greater elongation through the tendon.
bPatient with partial biceps rupture treated with completion and repair at surgery.
Figure 3.
(A) Time 0 radiograph compared with (B) 16-week radiograph showing significant elongation, most significantly from the button to first bead length. (C) Time 0 radiograph compared with (D) 16-week radiograph again showing significant lengthening, however, much less than that shown in (A) and (B).
The greatest amount of lengthening was seen between time 0 and 4 weeks, with the least amount of lengthening between weeks 8 and 16. However, 27.3% (3/11) of patients had the greatest amount of lengthening over 4 to 8 weeks. Over weeks 0 to 4, the tendon elongated a mean 11.3 mm overall (range, 2.7-23.8 mm), which represents 50% of total lengthening observed. Over weeks 4 to 8, the tendon elongated a mean 8.8 mm overall (range, 0.2-18.9 mm). Over weeks 8 to 16, the tendon elongated a mean 2.6 mm overall (range, 0.1-6.1 mm), representing 11% of total lengthening. The mean DASH score at final follow-up was 11.2, with 2 patients either refusing to complete the questionnaire or unable to be contacted. No significant correlation was noted for DASH scores compared with amount of lengthening of the tendon (R 2 = 0.13, P = .35). However, the least amount of lengthening (11.2 mm) was associated with a low DASH score (2.5) and the greatest DASH score (38) was associated with one of the greatest lengthenings (27.6 mm); additionally, the greatest amount of lengthening (30.9 mm) was associated with one of the lowest DASH scores (0.75).
Discussion
To maintain supination and flexion strength, operative repair is the standard of treatment for distal biceps tendon ruptures. Although some studies have evaluated outcomes after repair and the results of aggressive early rehabilitation, it is largely unknown what happens to the repaired tendon after fixation. Surgical decision making with regard to appropriate tendon repair fixation as well as postoperative protocols are typically based on anecdotal evidence and general tendon healing principles.3,19 Knowledge of when and how much a tendon may lengthen after repair may provide insight into tendon healing and theories of appropriate fixation strategies and rehabilitation protocols. This current study found significant tendon lengthening after distal biceps tendon repairs, with the most significant lengthening occurring within the first 4 weeks in the early postoperative period.
This is the first study, to our knowledge, to use RSA to evaluate tendon lengthening after distal biceps repair. RSA has previously been established in the literature to evaluate movement between 2 points in space and has shown an accuracy of within 1 mm.4 This is a reliable technique that has more recently been used to evaluate tendon and ligament changes as well.4,7,8,17 We also employed a novel technique by suturing the bead to the tendon to help eliminate concerns of bead migration throughout final evaluation of distal biceps repair.
Evaluations of fixation strength of distal biceps repair have previously shown button fixation to provide adequate strength of repair at time 0. Cil et al3 reported the button to have sufficient strength after repair to allow for early active range of motion and early rehabilitation.18 These studies have typically evaluated construct fixation strength and load to failure at 1 time point. Our current study, on the other hand, evaluated tendon elongation over time to show the change seen throughout the tendon healing process. Although good fixation strength has been found with multiple fixation methods in previous studies at 1 time point, we found significant lengthening after repair most notably in the early postoperative period. Although the majority of tendon repairs lengthened in the early postoperative period (0-4 weeks), a small amount showed greater elongation at 4 to 8 weeks, with minimal change at 8 to 16 weeks.
With this initial amount of lengthening, several surgical decisions must be taken into consideration. Morrey et al11 previously evaluated repair of distal biceps ruptures in extreme flexion and found good range of motion and satisfaction among patients at final follow-up. Due to the amount of lengthening found after repair in this current study, fixation at maximal tension, which may require a greater degree of flexion, may be prudent. A period of immobilization as well as delay of physical therapy may also be of benefit to deter the amount of tendon lengthening. The amount of immobilization as well as timing for the start of therapy, however, is uncertain. This study showed that every repair performed showed lengthening after initial fixation, with even the smallest change greater than 1 cm. The concern with changes in treatment regarding fixation in flexion as well as prolonged immobilization must be weighed against the risk for significant elbow stiffness.
The total amount of lengthening observed in this study after repair averaged just over 2 cm, with all tendon repairs showing significant lengthening after surgery. Reasons for lengthening can be multiple, including suture elongation, suture breakage, slippage of Krackow stitches, or tendon remodeling. Although it would seem intuitive that this amount of lengthening would be detrimental, conclusions about how this amount of lengthening effects overall function are limited in this study with limited patients. Several patients with quite significant lengthening had some of the lowest DASH scores, and some of the highest DASH scores were seen in patients with a great deal of elongation as well. Even with this amount of lengthening observed, all tendons were found to be intact at final follow-up, and mean DASH scores were acceptable. While tendon lengthening has been shown to decrease strength based on previous tendon studies, it is possible that the repair shortened the muscle-tendon unit and the lengthening noted is adaptive to the body trying to reset to the appropriate length.
There were multiple limitations to this study. One limitation was the number of patients evaluated. A larger number of patients could have offered a more decisive conclusion about expected tendon lengthening after surgery and would have allowed conclusions to be drawn about patient and surgical specifics and their effects on lengthening. There was also only 1 technique evaluated, and a 2-incision technique or interference fixation may have yielded different findings. However, as a primary study to evaluate distal biceps tendon lengthening, this small cohort of patients is similar to previous studies on tendon healing, and the amount of lengthening observed still allowed valuable conclusions about distal biceps repair to be made.4,7,8,17 Although the beads were securely fixed to the tendon via a suture through a hole in the bead, there is the possibility that the beads could have loosened after surgery. A future study with greater power would give more information about factors affecting lengthening and further functional outcomes. Another limitation to this current study was the lack of evaluation of strength postoperatively. Although tendon integrity was confirmed with final ultrasound evaluation, strength was not determined at final evaluation. Although strength measurements would add information to this cohort, the primary goal of the study was to evaluate tendon healing via tendon elongation after surgery. This is the first study to our knowledge to evaluate distal biceps repair healing and elongation after surgery.
Surgical technique and postoperative rehabilitation for distal biceps repair is largely based on previous tendon healing principles and anecdotal findings. This study found significant tendon lengthening using RSA after distal biceps repair. This amount of lengthening was observed in all distal biceps repairs and occurred mostly in the early postoperative period. These findings lend insight into decision-making with regard to intraoperative repair fixation and postoperative activity protocols while also adding knowledge to overall tendon repair principles.
Footnotes
One or more of the authors has declared the following potential conflict of interest or source of funding: This project was supported by a general medical education (GME) grant at Henry Ford Hospital to cover the cost of supplies and radiographic studies. Funding was provided by the Henry Ford Hospital Medical Education Department directly.
References
- 1. Baker BE, Bierwagen D. Rupture of the distal tendon of the biceps brachii. Operative versus non-operative treatment. J Bone Joint Surg Am. 1985;67:414–417. [PubMed] [Google Scholar]
- 2. Chillemi C, Marinelli M, De Cupis V. Rupture of the distal biceps brachii tendon: conservative treatment versus anatomic reinsertion—clinical and radiological evaluation after 2 years. Arch Orthop Trauma Surg. 2007;127:705–708. [DOI] [PubMed] [Google Scholar]
- 3. Cil A, Merten S, Steinmann SP. Immediate active range of motion after modified 2-incision repair in acute distal biceps tendon rupture. Am J Sports Med. 2009;37:130–135. [DOI] [PubMed] [Google Scholar]
- 4. Derwin KA, Milks RA, Davidson I, Iannotti JP, McCarron JA, Bey MJ. Low-dose CT imaging of radio-opaque markers for assessing human rotator cuff repair: accuracy, repeatability and the effect of arm position. J Biomech. 2012;45:614–618. [DOI] [PubMed] [Google Scholar]
- 5. Freeman CR, McCormick KR, Mahoney D, Baratz M, Lubahn JD. Nonoperative treatment of distal biceps tendon ruptures compared with a historical control group. J Bone Joint Surg Am. 2009;91:2329–2334. [DOI] [PubMed] [Google Scholar]
- 6. Kelly MP, Perkinson SG, Ablove RH, Tueting JL. Distal biceps tendon ruptures: an epidemiological analysis using a large population database. Am J Sports Med. 2015;43:2012–2017. [DOI] [PubMed] [Google Scholar]
- 7. Khan R, Konyyes A, Rama KR, Thomas R, Amis AA. RSA can measure ACL graft stretching and migration: development of a new method. Clin Orthop Relat Res. 2006;448:139–145. [DOI] [PubMed] [Google Scholar]
- 8. Lorbach O, Kieb M, Raber F, Busch LC, Kohn DM, Pape D. Three-dimensional evaluation of cyclic displacement in single-row and double-row rotator cuff reconstructions under static external rotation. Am J Sports Med. 2013;41:153–162. [DOI] [PubMed] [Google Scholar]
- 9. Miyamoto RG, Elser F, Millett PJ. Distal biceps tendon injuries. J Bone Joint Surg Am. 2010;92:2128–2138. [DOI] [PubMed] [Google Scholar]
- 10. Morrey BF, Askew LJ, An KN, Dobyns JH. Rupture of the distal tendon of the biceps brachii. A biomechanical study. J Bone Joint Surg Am. 1985;67:418–421. [PubMed] [Google Scholar]
- 11. Morrey ME, Abdel MP, Sanchez-Sotelo J, Morrey BF. Primary repair of retracted distal biceps tendon ruptures in extreme flexion. J Shoulder Elbow Surg. 2014;23:679–685. [DOI] [PubMed] [Google Scholar]
- 12. Rose DM, Archibald JD, Sutter EG, Belkoff SM, Wilckens JH. Biomechanical analysis suggests early rehabilitation is possible after single-incision Endobutton distal biceps repair with FiberWire. Knee Surg Sports Traumatol Arthrosc. 2011;19:1019–1022. [DOI] [PubMed] [Google Scholar]
- 13. Safran MR, Graham SM. Distal biceps tendon ruptures: incidence, demographics, and the effect of smoking. Clin Orthop Relat Res. 2002;404:275–283. [PubMed] [Google Scholar]
- 14. Sarda P, Qaddori A, Nauschutz F, Boulton L, Nanda R, Bayliss N. Distal biceps tendon rupture: current concepts. Injury. 2013;44:417–420. [DOI] [PubMed] [Google Scholar]
- 15. Seiler JG, Parker LM, Chamberland PD, Sherbourne GM, Carpenter WA. The distal biceps tendon. two potential mechanisms involved in its rupture: arterial supply and mechanical impingement. J Shoulder Elbow Surg. 1995;4:149–156. [DOI] [PubMed] [Google Scholar]
- 16. Shukla DR, Morrey BF, Thoreson AR, An KN, O’Driscoll SW. Distal biceps tendon rupture: an in vitro study. Clin Biomech (Bristol, Avon). 2012;27:263–267. [DOI] [PubMed] [Google Scholar]
- 17. Solomon LB, Callary SA. Emerging ideas: soft tissue applications of radiostereometric analysis. Clin Orthop Relat Res. 2011;469:1512–1516. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18. Spang JT, Weinhold PS, Karas SG. A biomechanical comparison of Endobutton versus suture anchor repair of distal biceps tendon injuries. J Shoulder Elbow Surg. 2006;15:509–514. [DOI] [PubMed] [Google Scholar]
- 19. Sutton KM, Dodds SD, Ahmad CS, Sethi PM. Surgical treatment of distal biceps rupture. J Am Acad Orthop Surg. 2010;18:139–148. [DOI] [PubMed] [Google Scholar]