Abstract
Background
Care for patients with chronic conditions often requires coordination between multiple physicians and delivery sites. Electronic Health Record (EHR) use could improve care quality and efficiency in part by facilitating care coordination.
Objectives
We examined the association between EHR use and clinician perceptions of care coordination for patients transferred across clinicians and delivery sites.
Research Design
Repeated surveys of primary care clinicians during the staggered implementation of an outpatient EHR (2005-2008), followed by an integrated inpatient EHR (2006-2010). We measured the association between EHR use stages (no use, outpatient EHR only, and integrated inpatient-outpatient EHR) and care coordination using logistic regression, adjusting for clinician characteristics, study year, and medical center.
Subjects
Adult primary care clinicians in a large integrated delivery system.
Measures
Three measures of clinician-reported care coordination for patient care transferred across clinicians (e.g., from specialist to primary care team) and across delivery sites (e.g., from the hospital to outpatient care).
Results
Outpatient EHR use was associated with higher reports of access to complete and timely clinical information and higher agreement on clinician roles and responsibilities for patients transferred across clinicians, but not for patients transferred across delivery sites. Use of the integrated outpatient-inpatient EHR was associated with higher reports of access to timely and complete clinical information, clinician agreement on the patient's treatment plan for patients transferred across delivery sites, and with all coordination measures for patients transferred across clinicians.
Conclusions
Use of an integrated EHR with health information exchange across delivery settings improved patient care coordination.
Keywords: Clinical information systems, continuity of care, coordinated care, health care technology, informatics, survey research
Introduction
Care for patients with chronic conditions often requires coordination across multiple physicians and delivery sites.1-4 Electronic Health Records (EHRs) and health information exchanges have been promoted as policy priorities for improving the quality and efficiency of the American healthcare system, largely through improved coordination.5-10 Meaningful use incentive payments continue to propel EHR adoption, however, participation in health information exchanges remains limited.11 There is little information on the impact of EHRs with and without electronic exchange of health information on care coordination.
We conducted repeated surveys of primary care clinicians working in a large Integrated Delivery System (IDS) during the staggered implementation of a commercially available outpatient EHR (2005-2008) followed by an integrated inpatient EHR (2006-2010). We examined whether use of the outpatient EHR alone and then the integrated outpatient-inpatient EHR were associated with three clinician reported measures of care coordination for patients transferred both across clinicians and across delivery sites.
Methods
Study Setting
This study was conducted in Kaiser Permanente Northern California (KPNC), a large, prepaid IDS providing comprehensive medical care for over three million members. The IDS included over 7,000 primary care and specialty clinicians and 18 medical centers. Each medical center contained a hospital, at least one emergency department (ED), and multiple outpatient clinics for primary and specialty care. Physicians received salaries and quality driven incentives for providing care exclusively to health plan members.12 Several characteristics of this healthcare system, including the partnership between the insurance plan and the medical group and the structural integration of the delivery system, are ideal for assessing the incremental contribution of EHR use and electronic clinical data exchange on care coordination.
Electronic Health Record
In February 2005, the IDS began a five-year staggered implementation of a commercially available, Epic-based certified-EHR system. The system was rolled out in two phases: 1) staggered across outpatient clinics (2005-2008), followed two years later by 2) staggered deployment across inpatient hospitals and EDs (2006-2010). Once implemented, use of the EHR system was mandatory and completely replaced paper medical charts.
The outpatient EHR integrated all outpatient visit records into one system, including primary and specialty care, outpatient labs, and pharmacy records, but did not include clinical information from hospitalizations or ED visits. The second phase integrated all inpatient and ED patient records with the outpatient EHR records. We exploit the discrepancy in the implementation schedules to assess first the impact of the outpatient EHR alone, then the impact of extending information exchange to include hospital and ED records.
Prior to the EHR, there was a patchwork of non-integrated Health IT applications available. Use of these early applications was voluntary and limited, and paper-based medical charts and alternatives for the same functions were common.
We categorized primary care clinicians as having access to the outpatient EHR when over 80 percent of visits made by their team were entered using the EHR system, typically within a month of initial installation.13 We used the implementation schedule to define the date when the integrated inpatient EHR system went live at each hospital/ED. We categorized three successive stages of EHR implementation: 1) no EHR, 2) EHR available at the outpatient clinic, and 3) integrated outpatient-inpatient EHR available. Each clinician's integrated EHR status was based on their team and hospital's EHR status on the date they completed the survey.
Survey Collection
In 2005, 2006, and 2008 we mailed a self-administered questionnaire to all adult primary care clinicians working in the IDS, including physicians, nurse practitioners, and physician assistants. We excluded clinicians who did not have an active panel of patients at the time of the survey. Each clinician received a letter introducing the study, the survey, and a pre-paid return envelope. Respondents who completed the survey received a small gift card. Non-respondents were re-sent reminder letters and surveys; up to four follow-up mailings were sent during each year of survey collection. The Kaiser Foundation Research Institute Institutional Review Board approved the study protocol and materials.
Care Coordination Measures
On the survey, we asked clinicians questions about two care transition situations: when patient care is transferred across clinicians (e.g., from a specialist to the primary care team and the reverse) and when care is transferred across delivery sites (e.g., from the hospital to the outpatient team and the reverse).
For each care transition situation, respondents rated “How often does each of the following occur?”
“All relevant medical information is available.”
“The information transfer is timely, i.e. available when it is needed.”
“All clinicians agree on the treatment goals and plans.”
“All clinicians agree on roles and responsibilities of each party.”
The response categories were: never, rarely, sometimes, usually, and always. These measures of care coordination were developed by an expert panel of scientific advisors specifically for this study, and have since been incorporated in the AHRQ Care Coordination Measures Atlas.14
We combined the responses to the survey questions asking if “all relevant medical information is available” and if “information transfer is timely.” We reasoned that in order for information to be useful, it must be both complete and timely (responses to these questions were highly correlated,>0.8). We categorized clinicians as having access to “complete and timely information” when ratings of both items were “always” or “usually.” We categorized clinicians as reporting “agreement on treatment goals and plans” and “agreement on roles and responsibilities” when ratings of each item were “always” or “usually.”
Clinician Characteristics
Our survey also collected several respondent characteristics, including race/ethnicity, gender, job title, and hours worked per week. In addition, we collected information from the IDS' administrative database on clinician age, gender, job title, and race/ethnicity.
Data Analysis
We first calculated the percent of respondents who reported each coordination outcome by EHR implementation stage. To analyze the adjusted association between EHR implementation stage and care coordination, we used logistic regression with generalized estimating equation and robust standard errors to control for repeated within-subject measurements. Models were adjusted for clinician characteristics (age, gender, race/ethnicity, professional title, and weekly hours worked), study year to control for temporal trends, and medical center indicators. We used Stata version 11.2 (StataCorp).
Results
In 2005, 565 primary care clinicians responded (48% response rate), 678 in 2006 (62% response rate), and 626 in 2008 (61% response rate). In 2005, 95%respondents were not yet using the EHR system; by 2006, 41% were using outpatient EHR, and 6% using the integrated outpatient-inpatient EHR; and in 2008, all primary care clinicians were using the outpatient EHR and 48% using the integrated outpatient-inpatient EHR (Table 1). There were a few notable differences between respondents and non-respondents: in 2005 and 2006, women were more likely to respond than men, and nurse practitioners more than physicians; and in 2005, clinicians using the outpatient EHR were more likely to respond than those not yet using the EHR (Appendix).
Table 1. Respondent characteristics by survey year.
| 2005 | 2006 | 2008 | |
|---|---|---|---|
| % | (N=565) | (N=678) | (N=626) |
| Response Rate | 48.1 | 61.5 | 60.8 |
|
| |||
| Gender: | |||
| Female | 54.7 | 54.0 | 51.5 |
| Male | 45.3 | 46.0 | 48.5 |
|
| |||
| Race/Ethnicity: | |||
| White | 49.0 | 43.1 | 39.6 |
| Non-white | 51.0 | 56.9 | 60.4 |
|
| |||
| Job Title: | |||
| M.D./D.O. | 84.3 | 88.4 | 94.4 |
| N.P/P.A. | 15.8 | 11.7 | 5.6 |
|
| |||
| Age: | |||
| 25-39 | 36.0 | 38.1 | 38.5 |
| 40-49 | 32.5 | 32.0 | 33.5 |
| 50+ | 31.5 | 29.9 | 28.0 |
|
| |||
| EHR Status: | |||
| No EHR | 95.0 | 41.3 | 0.0 |
| Outpatient EHR only | 5.0 | 52.4 | 52.3 |
| Integrated EHR | 0.0 | 6.3 | 47.7 |
Clinicians who worked in facilities where both the inpatient and outpatient EHR components were implemented were defined as having an integrated EHR. Overall, 1033 unique clinicians completed the survey in at least one year, 314 clinicians completed the survey in 2 out of the 3 years, and 274 clinicians completed the survey in all 3 years of data collection.
Care Transitions Across Clinicians
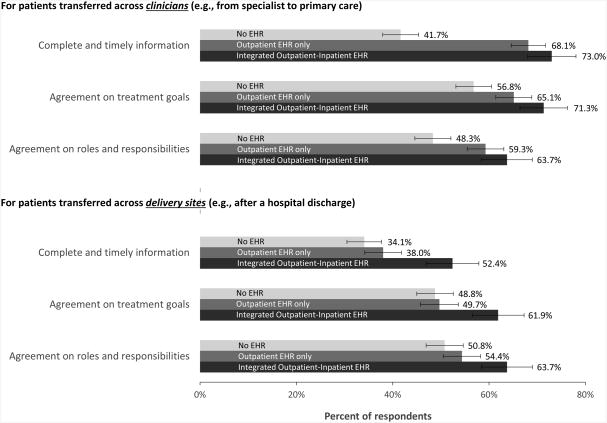
Figure 1 shows the unadjusted clinician-reported coordination measures by EHR implementation stage. Use of the outpatient EHR was associated with large increases in coordination for patients transferred across clinicians (e.g., from a specialist to the primary care team), while use of the added integrated inpatient EHR was associated with modest, not statistically significant, increases in these measures.
Figure 1.
Unadjusted percentage of primary care clinicians who reported each type of care coordination measure for care transferred across clinicians and across delivery sites by EHR Implementation Stage, with 95 percent confidence intervals.
In adjusted analyses, compared with no EHR, use of the outpatient EHR was associated with significantly higher reports of complete and timely information (OR=1.64, 95% CI: 1.12-2.40) and agreement on each other's roles and responsibilities (OR=1.51, 95% CI: 1.31-4.34) for patients transferred across clinicians (Table 2). Use of the integrated outpatient-inpatient EHR was associated with significantly higher reports of the three care coordination measures for patients transferred across clinicians compared with no EHR.
Table 2. Adjusted association between reported care coordination and EHR implementation stage.
| Access to complete and timely information | Agreement on treatment goals | Agreement on roles and responsibilities | ||||
|---|---|---|---|---|---|---|
| For patients transferred across clinicians (e.g., from specialist to primary care) | ||||||
| EHR implementation stage | OR | 95% CI | OR | 95% CI | OR | 95% CI |
| No EHR (reference) | 1.00 | 1.00 | 1.00 | |||
| Outpatient EHR | 1.64* | [1.12,2.40] | 1.40+ | [0.96,2.06] | 1.51* | [1.04,2.19] |
| Integrated outpatient-inpatient EHR | 2.05* | [1.08,3.92] | 2.30** | [1.24,4.28] | 2.38** | [1.31,4.34] |
| For patients transferred across delivery sites (e.g., after a hospital discharge) | ||||||
| EHR implementation stage | OR | 95% CI | OR | 95% CI | OR | 95% CI |
| No EHR (reference) | 1.00 | 1.00 | 1.00 | |||
| Outpatient EHR | 1.35 | [0.92,1.98] | 1.14 | [0.79,1.64] | 1.17 | [0.80,1.70] |
| Integrated outpatient-inpatient EHR | 2.25** | [1.24,4.09] | 1.80* | [1.01,3.19] | 1.55 | [0.85,2.83] |
Model: Generalized estimating equation, logistic regression model with robust standard errors, also adjusted for clinician characteristics (age, gender, race/ethnicity, job title, and weekly hours worked), study year, and medical center fixed effects. Clinicians who worked in facilities where both the inpatient and outpatient EHR components were implemented were defined as having an integrated EHR. The number of missing outcomes values was small (<5%) and not correlated with EHR status, therefore missing responses were dropped from the analyses.
p<0.1,
p<0.05,
p<0.01
Care Transitions Across Delivery Sites
Use of the outpatient EHR alone was associated with modest, not statistically significant, increases in coordination for patients transferred across delivery sites, while use of the integrated EHR was associated with larger, statistically significant, increases in coordination across delivery sites (Figure 1). In adjusted analyses, use of the outpatient EHR alone was not associated with changes in the three measures of care coordination for patients transferred across delivery sites. Whereas the use of the integrated outpatient-inpatient EHR was associated with significantly higher reports of complete and timely information (OR=2.25, 95% CI: 1.24-4.09, p<0.01) and clinician agreement on the patient's treatment goals and plans (OR=1.80, 95% CI: 1.01-3.19, p<0.05) compared with no EHR use (Table 2) or use of the outpatient EHR alone (Appendix) for patients transferred across delivery sites.
Discussion
One of the principal functions of EHRs is to provide clinicians with their patients' comprehensive health information when making decisions. For patients with multiple clinicians, however, coordination could be limited unless these clinicians share a single integrated EHR system or participate in a functionally equivalent health information exchange. Accordingly, we found that use of an outpatient EHR alone did not significantly impact coordination for patients transferred across care settings.
Our findings highlight the importance of using EHRs with information sharing across all of settings where patients receive care in order to improve care coordination. Stage 2 Meaningful Use incentive payments will require that eligible physicians electronically transmit a summary of care record for certain patients who they transfer or refer to other care settings; whether the incentive or the details of the satisfying criteria are sufficient remain unknown.15,16 Past federal support has increased the number of operational exchange efforts, but most are struggling to find a sustainable financial model or adequate participation.17 Few existing exchanges are equipped to support meaningful use requirements, and none allow for the robust exchange of information that could be necessary for clinicians and patients to make real-time decisions.15,17
Outside of health information exchanges, many practices still rely on fax machines to share partial patient records.18 As a result of inadequate information sharing, patient safety can be jeopardized during transitions in care.6,19-21 Although use of EHRs may be a necessary step toward improving care coordination, without a proven mechanism for and incentives to share information, it may not be sufficient. Given these challenges, policy makers should promote sustainable mechanisms that facilitate the electronic sharing of clinical records as well as new payment models, like accountable care organizations or bundled payments, which provide incentives for sharing patient records across settings. These efforts need to be supplemented by clear standards and regulations concerning information exchange.
This study has several limitations. It was conducted within a single IDS, using a specific EHR system; thus our findings cannot be generalized to other practice settings or delivery systems. The coordination measures were based on self-reported data, not on an audit of actual information available. Nonetheless, there are no comparable care coordination measures available using automated data. Our previous work found similar associations between the EHR use and unfavorable clinical event rates, which may be partly explained by improvements in care coordinating.13,14 Lastly, although we used a rigorous analytic approach, this is an observational study and therefore we cannot rule out unmeasured confounding.
Conclusion
Initial implementation of an outpatient EHR was associated with improved care coordination for patients receiving care from multiple clinicians, but not for those receiving care in multiple delivery settings. Use of an integrated outpatient-inpatient EHR was associated with improvements in care coordination for patients receiving care from multiple clinicians and delivery settings. To improve care coordination and fully realize the promise of EHRs, sustainable models are needed to allow easy exchange electronic health information across settings. Future studies should examine the relationship between EHR use, information exchanges, and care coordination in less integrated settings, and test whether improvements in care coordination measures are associated with changes in care quality.
Supplementary Material
Acknowledgments
Supported by grants from the Agency for Healthcare Research and Quality (1R36HS021082 and R01HS015280).
Footnotes
The findings were presented at the 2014 Academy Health Annual Research Meeting in June 2014 in San Diego, CA.
The authors declare no conflict of interest.
References
- 1.Schoen C, Osborn R, How SK, Doty MM, Peugh J. In chronic condition: experiences of patients with complex health care needs, in eight countries, 2008. Health Affairs. 2009 Jan-Feb;28(1):w1–16. doi: 10.1377/hlthaff.28.1.w1. [DOI] [PubMed] [Google Scholar]
- 2.Thorpe KE, Ogden LL, Galactionova K. Chronic conditions account for rise in Medicare spending from 1987 to 2006. Health Affairs. 2010 Apr;29(4):718–724. doi: 10.1377/hlthaff.2009.0474. [DOI] [PubMed] [Google Scholar]
- 3.Bodenheimer T, Chen E, Bennett HD. Confronting the growing burden of chronic disease: can the U.S. health care workforce do the job? Health Affairs. 2009 Jan-Feb;28(1):64–74. doi: 10.1377/hlthaff.28.1.64. [DOI] [PubMed] [Google Scholar]
- 4.Partnership for S, Johns Hopkins U. Chronic Conditions: Making The Case for Ongoing Care. 0-9727261-0-1. [Google Scholar]
- 5.Bodenheimer T. Primary care in the United States. Innovations in primary care in the United States. Bmj. 2003;326(7393):796–799. doi: 10.1136/bmj.326.7393.796. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Bodenheimer T. Coordinating care--a perilous journey through the health care system. N Engl J Med. 2008;358(10):1064–1071. doi: 10.1056/NEJMhpr0706165. [DOI] [PubMed] [Google Scholar]
- 7.Bodenheimer T, Wagner EH, Grumbach K. Improving primary care for patients with chronic illness: the chronic care model, Part 2. Jama. 2002;288(15):1909–1914. doi: 10.1001/jama.288.15.1909. [DOI] [PubMed] [Google Scholar]
- 8.Bodenheimer T, Wagner EH, Grumbach K. Improving primary care for patients with chronic illness. Jama. 2002;288(14):1775–1779. doi: 10.1001/jama.288.14.1775. [DOI] [PubMed] [Google Scholar]
- 9.Graetz I, Reed M, Rundall T, Bellows J, Brand R, Hsu J. Care Coordination and Electronic Health Records: Connecting Clinicians. AMIA Annu Symp Proc. 2009;2009:208–212. [PMC free article] [PubMed] [Google Scholar]
- 10.Williams C, Mostashari F, Mertz K, Hogin E, Atwal P. From the Office of the National Coordinator: the strategy for advancing the exchange of health information. Health affairs (Project Hope) 2012 Mar;31(3):527–536. doi: 10.1377/hlthaff.2011.1314. [DOI] [PubMed] [Google Scholar]
- 11.Adler-Milstein J, Bates DW, Jha AK. Operational health information exchanges show substantial growth, but long-term funding remains a concern. Health affairs. 2013 Aug;32(8):1486–1492. doi: 10.1377/hlthaff.2013.0124. [DOI] [PubMed] [Google Scholar]
- 12.McCarthy D, Mueller K, Wrenn J, Fund C. Kaiser Permanente: Bridging the quality divide with integrated practice, group accountability, and health information technology. Commonwealth Fund; New York: 2009. [Google Scholar]
- 13.Bardach NS, Huang J, Brand R, Hsu J. Evolving health information technology and the timely availability of visit diagnoses from ambulatory visits: A natural experiment in an integrated delivery system. BMC medical informatics and decision making. 2009;9(1):35. doi: 10.1186/1472-6947-9-35. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.McDonald KM. Care coordination measures atlas. 2010 [Google Scholar]
- 15.Adler-Milstein J, Bates DW, Jha AK. A survey of health information exchange organizations in the United States: implications for meaningful use. Ann Intern Med. 2011 May 17;154(10):666–671. doi: 10.7326/0003-4819-154-10-201105170-00006. [DOI] [PubMed] [Google Scholar]
- 16.The Government Accountability Office. Electronic Health Records: HHS Strategy to Address Information Exchange Challenges Lacks Specific Prioritized Actions and Milestones. 2014 Mar 24;2014 [Google Scholar]
- 17.Adler-Milstein J, Bates DW, Jha AK. Operational health information exchanges show substantial growth, but long-term funding remains a concern. Health Affairs. 2013;32(8):1486–1492. doi: 10.1377/hlthaff.2013.0124. [DOI] [PubMed] [Google Scholar]
- 18.Stille CJ, Jerant A, Bell D, Meltzer D, Elmore JG. Coordinating Care across Diseases, Settings, and Clinicians: A Key Role for the Generalist in Practice. Annals of Internal Medicine. 2005;142(8):700–708. doi: 10.7326/0003-4819-142-8-200504190-00038. [DOI] [PubMed] [Google Scholar]
- 19.Coleman EA. Falling Through the Cracks: Challenges and Opportunities for Improving Transitional Care for Persons with Continuous Complex Care Needs. Journal of the American Geriatrics Society. 2003;51(4):549–555. doi: 10.1046/j.1532-5415.2003.51185.x. [DOI] [PubMed] [Google Scholar]
- 20.Coleman EA, Berenson RA. Lost in Transition: Challenges and Opportunities for Improving the Quality of Transitional Care. Annals of Internal Medicine. 2004;141(7):533. doi: 10.7326/0003-4819-141-7-200410050-00009. [DOI] [PubMed] [Google Scholar]
- 21.Coleman EA, Boult C. Improving the quality of transitional care for persons with complex care needs. Journal of the American Geriatrics Society. 2003;51(4):556–557. doi: 10.1046/j.1532-5415.2003.51186.x. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.