Occupational radiation doses have been reduced substantially, and we found no evidence of excess mortality in U.S. radiologists who graduated from medical school after 1940.
Abstract
Purpose
To compare mortality rates from all causes, specific causes, total cancers, and specific cancers to assess whether differences between radiologists and psychiatrists are consistent with known risks of radiation exposure and the changes in radiation exposure to radiologists over time.
Materials and Methods
The authors used the American Medical Association Physician Masterfile to construct a cohort of 43 763 radiologists (20% women) and 64 990 psychiatrists (27% women) (comparison group) who graduated from medical school in 1916–2006. Vital status was obtained from record linkages with the Social Security Administration and commercial databases, and cause of death was obtained from the National Death Index. Poisson regression was used to estimate relative risks (RRs) and 95% confidence intervals (CIs) for all causes and specific causes of death.
Results
During the follow-up period (1979–2008), 4260 male radiologists and 7815 male psychiatrists died. The male radiologists had lower death rates (all causes) compared with the psychiatrists (RR = 0.94; 95% CI: 0.90, 0.97), similar cancer death rates overall (RR = 1.00; 95% CI: 0.93, 1.07), but increased acute myeloid leukemia and/or myelodysplastic syndrome death rates (RR = 1.62; 95% CI: 1.05, 2.50); these rates were driven by those who graduated before 1940 (RR = 4.68; 95% CI: 0.91, 24.18). In these earliest workers (before 1940) there were also increased death rates from melanoma (RR = 8.75; 95% CI: 1.89, 40.53), non-Hodgkin lymphoma (NHL) (RR = 2.69; 95% CI: 1.33, 5.45), and cerebrovascular disease (RR = 1.49; 95% CI: 1.11, 2.01). The 208 deaths in female radiologists precluded detailed investigation, and the number of female radiologists who graduated before 1940 was very small (n = 47).
Conclusion
The excess risk of acute myeloid leukemia and/or myelodysplastic syndrome mortality in radiologists who graduated before 1940 is likely due to occupational radiation exposure. The melanoma, NHL, and cerebrovascular disease mortality risks are possibly due to radiation. The authors found no evidence of excess mortality in radiologists who graduated more recently, possibly because of increased radiation protection and/or lifestyle changes.
© RSNA, 2016
Introduction
Internationally, it has been estimated that there are 2.3 million medical radiation workers, and they comprise about half of the workforce exposed to manmade sources of radiation (1). It is important to continue to study occupational groups who are exposed to radiation to determine if radiation protection measures are adequate (2). Patterns of mortality in radiologists can also contribute more generally to our understanding of the long-term effects of protracted low-level radiation exposure. Special features of radiologists compared with other radiation-exposed populations include generally good health compared with patient populations, the potential for long-term protracted radiation exposures, and higher doses in the past than most other radiation worker cohorts such as nuclear workers (2).
There have been eight epidemiologic studies of medical radiation worker cohorts (3,4), but only two include radiologists with long-term follow-up and both were relatively small (5–9). The British cohort of radiologists who were registered with a radiologic society between 1897 and 1979 (n = 2733) was followed up for mortality through 1997 (5–7). The U.S. cohort included 6500 male radiologists who were members of a professional society of radiologists and were followed up initially between 1920 and 1969 and subsequently, with the last mortality follow-up ending in 1974 (8,9).
We conducted a record linkage study using a nationwide listing of all U.S. physicians to identify a cohort of 43 763 radiologists and a comparison group of 64 990 psychiatrists, the latter with a low probability of occupational exposure to ionizing radiation. We performed this study to compare mortality rates attributed to all causes, specific causes, total cancers, and specific cancers to assess whether differences between radiologists and psychiatrists are consistent with known risks of radiation exposure and the changes in radiation exposure to radiologists over time.
Materials and Methods
Study Design
The study received institutional review board exemption as there was no direct contact with the study population.
The cohort was constructed by using membership listings from the American Medical Association (AMA). We obtained individual-level physician membership data from the AMA Physician Masterfile, which includes all physicians who practiced in the United States since 1902 regardless of whether they have ever been members of the AMA (http://www.ama-assn.org/ama/pub/about-ama/physician-data-resources/physician-masterfile.page). The AMA enrolls all U.S. physicians at the time they enter accredited medical schools or, in the case of international medical graduates, upon entry to an accredited postgraduate residency training program or when they obtain a state license in the United States. Additional professional certification information is added to the Masterfile record as they progress in their careers. The AMA updates their Masterfile database weekly with the information described earlier, self-reported physician survey data, and data from residency training programs, medical specialty boards, state licensing organizations, and other databases. The Masterfile includes basic demographic information, up to two medical specialties per physician (either self-declared or from residency programs), vital status, and date but not cause of death. The medical specialty information is updated and confirmed with use of several mechanisms. Every year, one-third of the physicians receive a self-administered annual survey that includes questions about current address, type of practice, and specialty. Thus, the entire group of physicians is contacted every 3 years. The response rate to the survey varies but is approximately 40%. If a physician does not ever complete or update a survey, the specialty for his or her most recent residency training is maintained in the file. Residency training information is obtained from the American Association of Medical Colleges by means of a data sharing agreement.
Physicians were eligible for the current cohort if they had a first or second specialty of radiology, including abdominal radiology, cardiothoracic radiology, diagnostic radiology, musculoskeletal radiology, nuclear radiology, and pediatric radiology. Interventional radiologists, defined as those who had this as their specialty or subspecialty in the AMA Masterfile, were excluded from the current analysis as we are studying them separately in a cohort of physicians who perform fluoroscopically guided procedures. We selected a sample of physicians with a primary or secondary specialty of psychiatry as the comparison group because of a very low probability of occupational exposure to radiation. The stratified random sample was selected to ensure at least a 1:1 ratio (psychiatrists:radiologists) in each of the strata defined according to birth year (5-year categories) and sex.
Outcome Ascertainment
We conducted a series of record linkages to ascertain identifying information that was not available in the AMA database and then matched the cohort with the Social Security Administration database to determine vital status. The physicians who were confirmed or presumed to be deceased were matched with the National Death Index (http://www.cdc.gov/nchs/ndi.htm). To obtain identifying information, we used commercial databases such as the Pension Benefits Incorporated, TransUnion, Accurint, and Fastdata databases and also used interactive tracing to obtain additional identifying information for individuals who could not be traced successfully by using the other sources. Uncertain matches were reviewed manually. Vital status was then confirmed with the Social Security Administration. We submitted records for physicians who were confirmed or presumed to be deceased for whom we had a date of death and for those deceased physicians for whom we did not have a date of death to the National Death Index. Because the National Death Index includes deaths for 98% of the U.S. population (10), subjects for whom no record of death was found were assumed to be alive.
Statistical Analysis
Physicians were followed up from January 1, 1979 (date of the start of the National Death Index), or from 1 year after medical school graduation (if after 1979) until date of death, loss to follow-up, or December 31, 2008. Follow-up was limited to deaths that occurred before age 85 years because cause of death is reported less reliably after that age (7). Poisson regression analysis was used to estimate relative risks (RRs) and 95% confidence intervals (CIs) for all causes of death and specific causes for radiologists versus psychiatrists. All analyses were adjusted (by means of stratification) for sex, year of birth, and attained age—the latter two characteristics in 5-year groups. We also compared the observed number of deaths from various causes to the expected number by means of standardized mortality ratios on the basis of rates in the general U.S. population, adjusted for age, sex, and calendar year of death.
We used the year of medical school graduation plus 1 year as a proxy for the year first exposed to radiation. Because occupational radiation exposures to noninterventional radiologists have been reduced over time owing to improved protection (11–14), the year of medical school graduation is a proxy for exposure level. We conducted a sensitivity analysis that was restricted to those physicians who were dead or confirmed to be alive through the Social Security Administration to assess whether there was bias related to completeness of follow-up. All analyses were conducted with software (Epicure; Risk Sciences International, Ottawa, Ontario, Canada).
Results
We identified a cohort of 43 763 radiologists (8851 women [20%]) and 64 990 psychiatrists (17 493 women [27%]) from the AMA Masterfile. The cohort consists of physicians who started practicing as early as 1916 and who were still alive in 1979, which is when the National Death Index was introduced.
Overall, radiologists were slightly younger and slightly more likely to have graduated from medical school in 1960 or later compared with psychiatrists. Radiologists were also more likely than psychiatrists to be born in the United States (Table 1).
Table 1.
Description of the Study Cohort

Note.—Except where indicated, data are numbers of patients, with percentages in parentheses.
*Cause of death was missing in 133 cases.
†Cause of death was missing in 337 cases.
‡Cause of death was missing in 14 cases.
§Cause of death was missing in 55 cases.
In the male cohort, 4260 of 43 763 radiologists (12%) and 7815 of 47 443 psychiatrists (16%) were confirmed to have died between 1979 and 2008 (Table 2). Cause of death was not ascertained for 133 (3%) of the 4260 male radiologists and 337 (4%) of the 7815 male psychiatrists. In the female cohort, 208 (2%) of the 8851 radiologists and 524 (3%) of the 17 493 psychiatrists died during the follow-up period. Overall, the radiologists and the psychiatrists had substantially lower death rates than the general population (standardized mortality ratio = 0.47 for radiologists and 0.52 for psychiatrists) (Table E1 [online]). Given the small number of female radiologists, our analyses focused on men; Table E1 (online) provides additional details about the female subjects.
Table 2.
RRs and 95% CIs of Death from All Causes, All Cancers, and Site-specific Cancers in Male Radiologists (n = 34 912) and Male Psychiatrists (n = 47 497) according to Year of Medical School Graduation
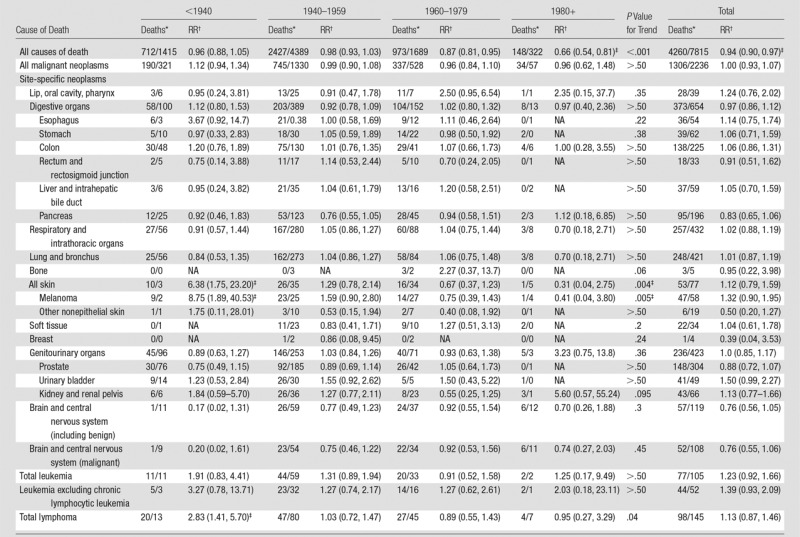
*Data are numbers of radiologists/numbers of psychiatrists.
†Stratified on year of attained age, year of birth, and year of medical school graduation. Numbers in parentheses are 95% CIs. NA = not applicable.
‡P <.05 for difference in risk between radiologists and psychiatrists is based on the Wald test.
The male radiologists had a lower risk of death overall than did the male psychiatrists (RR = 0.94; 95% CI: 0.90, 0.97) but a similar risk of death from any cancer (RR = 1.00; 95% CI: 0.93, 1.07). There was an increased risk of skin cancer mortality in the radiologists who graduated before 1940 (RR = 6.38; 95% CI: 1.75, 23.20) that was driven by an excess of melanoma (RR = 8.75; 95% CI: 1.89, 40.53) (Table 2).
Overall, there was an increased risk of death for all myeloid leukemias (RR = 1.43; 95% CI: 1.00, 2.05), which was largely due to acute myeloid leukemia and/or myelodysplastic syndrome in those who graduated before 1940 (RR = 4.68; 95% CI: 0.91, 24.18) (Table 3). There was also an increased risk of death from all lymphoid malignancies (lymphomas) in these earliest radiologists (RR = 2.24; 95% CI: 1.31, 3.86) because of an increased risk of death from NHL (RR = 2.69; 95% CI: 1.33, 5.45). There were no significantly increased risks of cancer mortality in those who graduated after 1940 for all solid cancers, hematologic malignancies, or site-specific solid cancers.
Table 3.
RRs and 95% CIs of Death from Hematopoietic and Lymphoproliferative Disorders in Male Radiologists (n = 34 912) and Male Psychiatrists (n = 46 846) according to Year of Medical School Graduation
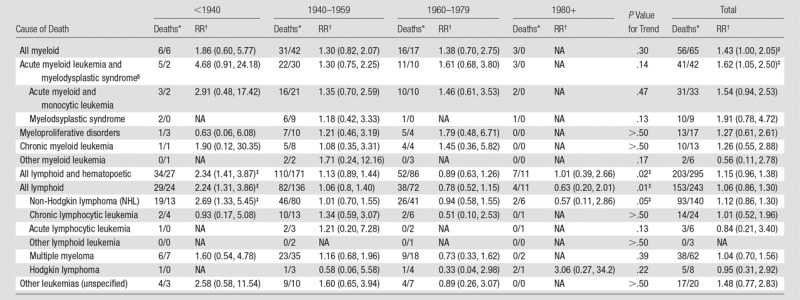
*Data are numbers of radiologists/numbers of psychiatrists.
†Stratified on year of attained age, year of birth, and year of medical school graduation. Numbers in parentheses are 95% CIs. NA = not applicable.
‡P < .05 for difference in risk between radiologists and psychiatrists is based on the Wald test.
§Includes all malignant, benign, and uncertain behavior.
In the deaths from noncancer causes, we noted an excess risk of cerebrovascular deaths in the radiologists who graduated before 1940 (RR = 1.49; 95% CI: 1.11, 2.01) (Table 4). However, there were decreased risks of infectious diseases (RR = 0.43; 95% CI: 0.34, 0.55)—primarily human immunodeficiency virus (RR = 0.32; 95% CI: 0.22, 0.45) (Table 4), respiratory diseases (RR = 0.85; 95% CI: 0.73, 0.99), accidents (RR = 0.77; 95% CI: 0.67, 0.89), and suicides (RR = 0.66; 95% CI: 0.55, 0.80). Many of these decreases were greatest in the physicians who graduated most recently (1980 and later).
Table 4.
RRs and 95% CIs of Death from Noncancer Causes in Male Radiologists (n = 34 912) and Male Psychiatrists (n = 46 846) according to Year of Medical School Graduation
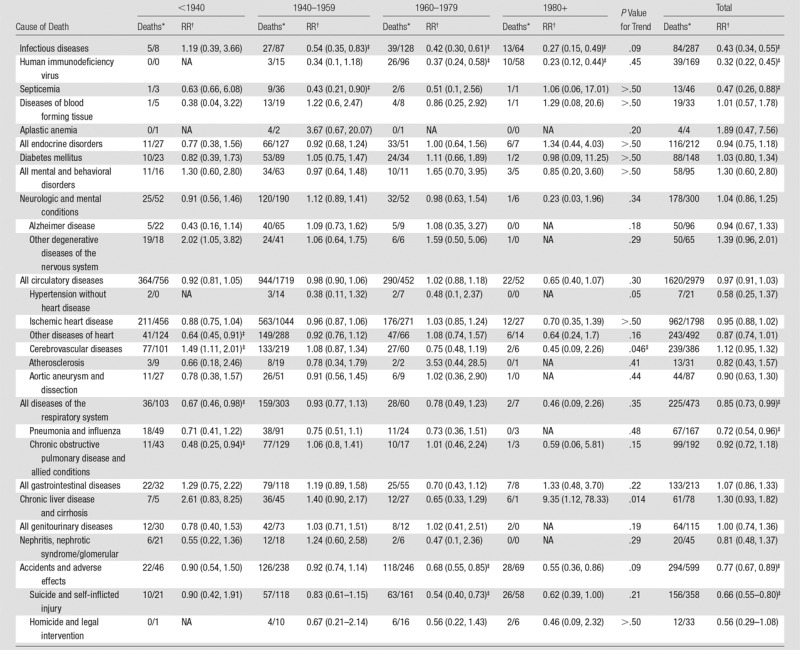
*Data are numbers of radiologists/numbers of psychiatrists.
†Stratified on year of attained age, year of birth, and year of medical school graduation. Numbers in parentheses are 95% CIs. NA = not applicable.
‡P < .05 for difference in risk between radiologists and psychiatrists is based on the Wald test.
In a sensitivity analysis, we restricted the subjects to those who were confirmed as dead or alive by the Social Security Administration, and the results were essentially equivalent to those with the full analyses (Table E2 [online]).
There were no clear increases in mortality in the female radiologists compared with female psychiatrists (Table 5). Overall, total mortality was lower in female radiologists compared with female psychiatrists, but total cancer risks were similar. Risk of all circulatory diseases and particularly cerebrovascular disease was notably reduced in radiologists compared with psychiatrists, albeit these are based on small numbers. The relatively small number of deaths in this group (n = 208), however, prevented detailed investigation.
Table 5.
RRs and 95% CIs for Deaths from All Causes, All Cancers, Leukemia, and Selected Circulatory Diseases in Female Radiologists (n = 8851) and Female Psychiatrists (n = 17 493) according to Year of Medical School Graduation
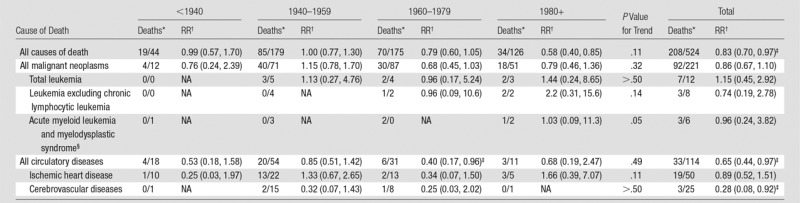
*Data are numbers of radiologists/numbers of psychiatrists.
†Stratified on year of attained age, year of birth, and year of medical school graduation. Numbers in parentheses are 95% CIs. NA = not applicable.
‡P < .05 for difference in risk between radiologists and psychiatrists is based on the Wald test.
§Includes all malignant, benign, and uncertain behavior.
Discussion
We established the largest cohort to date of radiologists who had practiced in the United States throughout the last century and a comparison group of psychiatrists unlikely to have had occupational radiation exposure. Overall, compared with the psychiatrists, the radiologists had a significantly lower risk of death from all causes and a similar risk of death from all cancers combined and most other specific causes of death, but we did observe an increased risk of acute myeloid leukemia and/or myelodysplastic syndrome, melanoma, and NHL in the radiologists who graduated before 1940—when radiation exposures would have been the highest. There was also an excess risk of cerebrovascular death in these earliest radiologists. There were no increased risks of cancer mortality or other causes of death in the radiologists who graduated after 1940.
The previous U.S. cohort of mortality to 1974 in radiologists who joined the Radiological Society of North America (RSNA) between 1920 and 1969 (9) also showed excess mortality rates for radiation-related cancers, which were only observed in the earliest radiologists (who joined the RSNA before 1940); however, follow-up was limited for those who joined after 1940. In a much larger population with longer-term follow-up, we have confirmed that excess mortality rates in U.S. radiologists are mostly restricted to those who worked before 1940. In a U.K. cohort, results of long-term follow-up suggested that excess mortality rates were restricted to those who worked before 1954 (7).
Early case studies of radiologists provided the first evidence that leukemia was a radiation-related cancer (15). Further systematic studies of U.K. and U.S. radiologists confirmed this finding (6,16), and our results for acute myeloid leukemia are consistent with the results of those studies. The elevated risk of acute myeloid leukemia has also been shown to persist in atomic bomb survivors for more than 55 years after exposure (17).
Skin cancer mortality, particularly melanoma, was also increased in the radiologists who graduated before 1940, which is interesting because ionizing radiation is not thought to be a cause of melanoma (18). There were significant excess risks of deaths from nonmelanoma skin cancer in the United Kingdom (7) and in the previous cohort of U.S. radiologists (16), but not melanoma. Melanoma is a relatively rare cancer and, therefore, has been difficult to study in most previous radiation epidemiology cohorts. In the last cancer incidence analysis of Japanese atomic bomb survivors, there were only 17 cases, which precluded informative analysis (19). There was a nonstatistically significant dose response in U.K. nuclear workers (n = 261) (20) and a significant excess in the U.S. Radiologic Technologists study among those who first worked before 1950 (21). Confounding by solar ultraviolet radiation, which is a strong risk factor for melanoma (22), cannot be ruled out, but the radiologists who graduated before 1940 would have needed higher exposure to ultraviolet radiation for this to explain the patterns of results.
NHL is also not classified as a radiation-inducible cancer because of the inconsistency in findings across studies (18). There is a weak suggestion of a radiation dose response for NHL among male atomic bomb survivors, but not for female survivors (17), and an excess was observed in the U.K. radiologists—although the numbers were small (n = 9) (7). Again, as with melanoma, the elevated risk in the earliest radiologists is compatible with higher radiation doses but could be due to unknown confounding factors if they were more common in radiologists who graduated before 1940. Because death rates from the human immunodeficiency virus were significantly lower in the radiologists than the psychiatrists and NHL is an acquired immune deficiency syndrome–related cancer (23), this may have biased the risk estimates in those radiologists who graduated after 1940 toward the null.
An increased risk of cerebrovascular disease mortality was not reported in any of the previous radiologist cohorts (7,16) but has been observed at higher dose levels (>0.5 Gy) in atomic bomb survivors (24), after radiation therapy for breast cancer (25), and in the Mayak worker cohort (26). It is less certain whether doses less than 0.5 Gy are associated with heart disease and cerebrovascular disease, although a recent meta-analysis provided some evidence that it may be (27).
The major strengths of our study are the large size of the population, our ability to capture the majority of radiologists who practiced in the United States and were still alive in 1979, and the internal comparison group of physicians who were unlikely to have been exposed to radiation through their occupation. Our long-term follow-up of radiologists who graduated before 1940 provides an assessment of risks several decades after first exposure. We also had systematic follow-up through a large number of tracing sources, with a sensitivity analysis that excluded large follow-up biases.
The large-scale nature of the study also brought limitations, including a lack of data on whether a physician is currently practicing medicine, a lack of data about lifestyle factors, and a lack of individual occupational radiation doses. The AMA physicians’ database has been used for previous surveys of the radiology workforce because it is more complete than the American College of Radiology membership (28), which is estimated to include about 75% of practicing radiologists. The American College of Radiology currently reports that about 21 000 members are diagnostic radiologists (29). In 2002, Bhargavan et al (30) estimated, by using American College of Radiology data, that there were about 25 000 radiologists practicing in the United States in 2001. Our cohort included about 30 000 radiologists who are currently younger than 70 years, which suggests that the cohort is quite complete. Radiologists are also unlikely to have been misclassified as psychiatrists or vice versa. Lack of data on confounding factors, such as smoking, could have biased our results in either direction. Mortality rates from chronic obstructive pulmonary disease were significantly lower in the radiologists than in the psychiatrists who graduated before 1940 (RR = 0.48; 95% CI: 0.25, 0.94), which suggests that smoking rates are lower in this group, which probably biased smoking-related mortality risks toward the null, particularly lung cancer. Lower smoking rates in radiologists than psychiatrists were also reported in the survey of the British Doctors Study in 1951 and 1966 (31). There are few medical specialties now that have no occupational radiation exposure, which is why psychiatrists were selected as the comparison. As with an earlier study of psychiatrists in the United States, we found higher death rates from suicide, accidents, and human immunodeficiency virus among psychiatrists compared with radiologists (32). As noted earlier, this may have biased results for NHL toward the null. Finally, even in this study that included the majority of U.S. radiologists who practiced in the last century there were too few women to study their mortality rates in detail. In addition, very few female radiologists worked during the early period, when exposures were likely highest.
There have been dramatic improvements in radiation protection since the earliest radiologists started practicing, including general lead shielding of equipment, personal use of lead aprons and glasses, and use of room shields (3). Early fluoroscopy procedures were likely a common and important source of radiation exposure to the radiologists who were practicing before 1940 (3). Decreases in the maximum permissible occupational dose have also occurred (33), and changes in radiation protection have changed the organs that received the highest radiation exposure. Early radiologists had high skin doses to hands and arms, used no personal protection garments, and received whole-body exposure from unshielded x-ray tubes (3). Current radiologists routinely wear lead or lead-equivalent aprons when performing fluoroscopy and may wear thyroid shields and leaded eyewear as well. The development of sensitive film badge monitors and government-required monitoring of medical radiation workers, along with a series of standards for radiation protection, also contributed to notable decreases in occupational radiation exposures, as borne out by survey data (11–14). Finally, there have been substantial changes in practice, with a shift toward radiologic technologists performing radiologic examinations rather than radiologists (3). Radiologists now receive radiation doses almost exclusively from fluoroscopy and some nuclear medicine procedures. The mean annual doses for radiologists in the United Kingdom decreased from 5 mGy in 1964 to 0.5 mGy in 1984, and the mean annual doses for radiologists in the United States from 1972 to 1978 ranged from 3.6 to 0.7 mGy (34). Exposures to physicians have increased in certain medical specialties in which fluoroscopically guided interventions are performed routinely, however, and these physicians, including interventional radiologists, are the subject of a separate investigation (3).
In conclusion, the excess risk of acute myeloid leukemia and/or myelodysplastic syndrome in radiologists compared with psychiatrists who graduated before 1940 is likely due to higher occupational radiation exposures. Excess risks of skin cancer, NHL, and cerebrovascular disease mortality in these earliest radiologists were observed. Low-dose radiation exposure is not an established cause of these cancers, but these findings warrant further investigation to test this possibility. Occupational radiation doses have been reduced substantially, and we found no evidence of excess mortality in U.S. radiologists who graduated from medical school after 1940, possibly because of increased radiation protection and/or lifestyle changes.
Advances in Knowledge
■ The study included 43 763 radiologists and 64 990 psychiatrists (comparison group) who graduated from medical school in 1916–2006; in the radiologists who graduated after 1940, there was no evidence of increased mortality from radiation-related causes such as cancer or cardiovascular disease.
■ In the radiologists who graduated before 1940, there was an increased risk of mortality from leukemia and/or myelodysplastic syndrome (relative risk [RR] = 4.68; 95% confidence interval [CI]: 0.91, 24.18) that was likely related to their occupational radiation exposure.
■ There was also increased mortality from melanoma (RR = 8.75; 95% CI: 1.89, 40.53), non-Hodgkin lymphoma (RR = 2.69; 95% CI: 1.33, 5.45), and cerebrovascular disease (RR = 1.49; 95% CI: 1.11, 2.01) in those that graduated before 1940, and this is possibly due to occupational radiation exposure.
SUPPLEMENTAL TABLES
Received November 9, 2015; revision requested December 14; revision received March 29, 2016; accepted April 19; final version accepted April 24.
Supported by National Institutes of Health Intramural Research Program (grant Z01 CP010133-21).
Disclosures of Conflicts of Interest: A.B.d.G. disclosed no relevant relationships. E.N. disclosed no relevant relationships. C.M.K. disclosed no relevant relationships. E.G. disclosed no relevant relationships. D.L.M. disclosed no relevant relationships. R.A.K. disclosed no relevant relationships. M.S.L. disclosed no relevant relationships.
Abbreviations:
- AMA
- American Medical Association
- CI
- confidence interval
- NHL
- non-Hodgkin lymphoma
- RR
- relative risk
References
- 1.United Nations Scientific Committee on the Effects of Atomic Radiation . Sources and effects of ionizing radiation. New York, NY: United Nations, 2000; 453–487. [Google Scholar]
- 2.Richardson DB, Cardis E, Daniels RD, et al. Risk of cancer from occupational exposure to ionising radiation: retrospective cohort study of workers in France, the United Kingdom, and the United States (INWORKS). BMJ 2015;351:h5359. [Published correction appears in BMJ 2015;351:h6634.] [DOI] [PMC free article] [PubMed]
- 3.Linet MS, Kim KP, Miller DL, Kleinerman RA, Simon SL, Berrington de Gonzalez A. Historical review of occupational exposures and cancer risks in medical radiation workers. Radiat Res 2010;174(6):793–808. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Yoshinaga S, Mabuchi K, Sigurdson AJ, Doody MM, Ron E. Cancer risks among radiologists and radiologic technologists: review of epidemiologic studies. Radiology 2004;233(2):313–321. [DOI] [PubMed] [Google Scholar]
- 5.Court Brown WM, Doll R. Expectation of life and mortality from cancer among British radiologists. BMJ 1958;2(5090):181–187. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Smith PG, Doll R. Mortality from cancer and all causes among British radiologists. Br J Radiol 1981;54(639):187–194. [DOI] [PubMed] [Google Scholar]
- 7.Berrington A, Darby SC, Weiss HA, Doll R. 100 years of observation on British radiologists: mortality from cancer and other causes 1897–1997. Br J Radiol 2001;74(882):507–519. [DOI] [PubMed] [Google Scholar]
- 8.Matanoski GM, Sternberg A, Elliott EA. Does radiation exposure produce a protective effect among radiologists? Health Phys 1987;52(5):637–643. [DOI] [PubMed] [Google Scholar]
- 9.Matanoski GM, Seltser R, Sartwell PE, Diamond EL, Elliott EA. The current mortality rates of radiologists and other physician specialists: deaths from all causes and from cancer. Am J Epidemiol 1975;101(3):188–198. [DOI] [PubMed] [Google Scholar]
- 10.Schall LC, Buchanich JM, Marsh GM, Bittner GM. Utilizing multiple vital status tracing services optimizes mortality follow-up in large cohort studies. Ann Epidemiol 2001;11(5):292–296. [DOI] [PubMed] [Google Scholar]
- 11.1990 Recommendations of the International Commission on Radiological Protection. Ann ICRP 1991;21(1-3):1–201. [PubMed] [Google Scholar]
- 12.International Commission on Radiological Protection. ICR Publication 26 Annals of the ICRP: 1977 Recommendations of the International Commission on Radiological Protection: Elsevier Health Sciences; 1977.
- 13.National Council on Radiation Protection and Measurements . Recommendations on limits for exposure to ionizing radiation. Bethesda, Md: NCRP, 1987. [Google Scholar]
- 14.National Council on Radiation Protection and Measurements . Limitation of exposure to ionizing radiation. Bethesda, Md: NCRP, 1993. [Google Scholar]
- 15.March HC. Leukemia in radiologists. Radiology 1944;43(3):275–278. [Google Scholar]
- 16.Matanoski GM, Seltser R, Sartwell PE, Diamond EL, Elliott EA. The current mortality rates of radiologists and other physician specialists: specific causes of death. Am J Epidemiol 1975;101(3):199–210. [DOI] [PubMed] [Google Scholar]
- 17.Hsu WL, Preston DL, Soda M, et al. The incidence of leukemia, lymphoma and multiple myeloma among atomic bomb survivors: 1950–2001. Radiat Res 2013;179(3):361–382. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.United Nations Scientific Committee on the Effects of Atomic Radiation . Effects of ionizing radiation: report to the General Assembly, with scientific annexes. New York, NY: United Nations Publications, 2008. [Google Scholar]
- 19.Preston DL, Ron E, Tokuoka S, et al. Solid cancer incidence in atomic bomb survivors: 1958–1998. Radiat Res 2007;168(1):1–64. [DOI] [PubMed] [Google Scholar]
- 20.Muirhead CR, O’Hagan JA, Haylock RG, et al. Mortality and cancer incidence following occupational radiation exposure: third analysis of the National Registry for Radiation Workers. Br J Cancer 2009;100(1):206–212. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Freedman DM, Sigurdson A, Rao RS, et al. Risk of melanoma among radiologic technologists in the United States. Int J Cancer 2003;103(4):556–562. [DOI] [PubMed] [Google Scholar]
- 22.International Agency for Research on Cancer . Radiation. In: IARC monographs on the evaluation of carcinogenic risks to humans, volume 100D. Lyon, France: IARC, 2012;103–210. [Google Scholar]
- 23.Silverberg MJ, Chao C, Leyden WA, et al. HIV infection and the risk of cancers with and without a known infectious cause. AIDS 2009;23(17):2337–2345. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Shimizu Y, Kodama K, Nishi N, et al. Radiation exposure and circulatory disease risk: Hiroshima and Nagasaki atomic bomb survivor data, 1950–2003. BMJ 2010;340:b5349. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Stokes EL, Tyldesley S, Woods R, Wai E, Olivotto IA. Effect of nodal irradiation and fraction size on cardiac and cerebrovascular mortality in women with breast cancer treated with local and locoregional radiotherapy. Int J Radiat Oncol Biol Phys 2011;80(2):403–409. [DOI] [PubMed] [Google Scholar]
- 26.Azizova TV, Haylock RG, Moseeva MB, Bannikova MV, Grigoryeva ES. Cerebrovascular diseases incidence and mortality in an extended Mayak worker cohort 1948–1982. Radiat Res 2014;182(5):529–544. [DOI] [PubMed] [Google Scholar]
- 27.Little MP, Azizova TV, Bazyka D, et al. Systematic review and meta-analysis of circulatory disease from exposure to low-level ionizing radiation and estimates of potential population mortality risks. Environ Health Perspect 2012;120(11):1503–1511. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Owen JB, Chan WC, Sunshine JH, Shaffer KA. The sex ratio of American radiologists: comparison and implications by age, subspecialty, and type of practice. AJR Am J Roentgenol 1995;165(6):1337–1341. [DOI] [PubMed] [Google Scholar]
- 29.American College of Radiology . Basic facts about the ACR. http://www.acr.org/About-Us/Media-Center/Basic-Facts-About-the-ACR. Accessed March 11, 2016.
- 30.Bhargavan M, Sunshine JH, Schepps B. Too few radiologists? AJR Am J Roentgenol 2002;178(5):1075–1082. [DOI] [PubMed] [Google Scholar]
- 31.Doll R, Peto R. Mortality among doctors in different occupations. BMJ 1977;1(6074):1433–1436. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Rich CL, Pitts FN, Jr. Suicide by psychiatrists: a study of medical specialists among 18,730 consecutive physician deaths during a five-year period, 1967–72. J Clin Psychiatry 1980;41(8):261–263. [PubMed] [Google Scholar]
- 33.Inkret WC, Meinhold CB, Taschner JC. Protection standards. Los Alamos Sci 1995;(23):116–123. [Google Scholar]
- 34.Brenner DJ, Hall EJ. Mortality patterns in British and US radiologists: what can we really conclude? Br J Radiol 2003;76(901):1–2. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.


