Abstract
Background
Problem substance use often begins in adolescence. This vulnerability likely stems, at least partially, from relatively rapid increases in sensation seeking occurring in early to mid adolescence and more gradual improvements in impulse control occurring through later adolescence. Better understanding how these processes develop in high-risk youth may lead to enhanced substance use disorder treatment and prevention strategies
Methods
We characterized trajectories of self-reported impulsivity and sensation seeking in 305 FH+ youths who at minimum had a father with a history of alcohol or other drug use disorders and 81 youths with no family histories of substance use disorders (FH−). Assessments started at ages 10–12 and continued at 6-month intervals for up to 42 months. In addition, a subset of 58 FH+ youths who began alcohol or other drug use before age 15 (FH+ Users) were compared to 58 FH+ propensity- matched adolescents who did not initiate substance use before age 15 (FH+ Non-Users).
Results
Compared to FH− youths at pre-adolescence, FH+ youths reported higher general impulsivity and higher impulsivity related to poor planning and attention. Over time, there were no differential effects of FH status on changes in impulsivity or sensation seeking across adolescence. FH+ Users had smaller decreases in general impulsivity and impulsivity related to restlessness and fidgeting across adolescence than FH+ Non-Users. FH+ Users also had greater increases in sensation seeking across adolescence than FH+ Non-Users.
Conclusions
Increased impulsivity in FH+ youths may make them less able to regulate sensation seeking drives that peak in adolescence, which may contribute to their high-risk for developing substance use disorders. Additionally, FH+ adolescents who initiate early use may be at increased risk in part due to increased impulsivity coupled with greater increases in sensation seeking.
Keywords: family history, adolescence, impulsivity, sensation seeking, early-onset substance use
Problem alcohol and other drug use often begins in adolescence (Grant and Dawson, 1997, Webb et al., 1991), and this appears at least partially due to normal developmental changes in impulsivity and sensation seeking (Somerville and Casey, 2010). Impulsivity and sensation seeking appear to be distinct processes that develop independently across adolescence (Shulman et al., 2014). Impulsivity includes a predisposition toward rapid, unplanned reactions to internal or external stimuli regardless of negative consequences of these reactions (Moeller et al., 2001). Sensation seeking is the tendency to seek out novel, stimulating, and often risky experiences (Zuckerman and Link, 1968). Typically, impulsivity slowly decreases across adolescence into early adulthood; in contrast sensation seeking rapidly increases through mid-adolescence and decreases by early adulthood (Harden and Tucker-Drob, 2011). Elevated impulsivity and sensation seeking in adolescence are both associated with increased alcohol and other drug use (Pedersen et al., 2012, Quinn and Harden, 2013), and decreased impulsivity and sensation seeking in early adulthood are associated with decreased problem alcohol use (Littlefield et al., 2009, Littlefield et al., 2010, Quinn and Harden, 2013).
According to the Dual Systems Model, adolescents are predisposed to engage in deviant behaviors such as problem alcohol and other drug use because their sensation seeking drives are poorly inhibited, which is a consequence of sensation seeking peaking prior to the development of adult levels of impulse control (Ernst et al., 2006, Steinberg et al., 2008, Shulman et al., 2014). However, it is not clear how these processes develop in adolescent populations at high-risk for substance use disorders. Plausibly, high-risk populations may have poorer impulse control and/or elevated sensation seeking, resulting in even poorer ability to regulate sensation seeking drives (Bjork and Pardini, 2015). High risk youths may have relative deficits in impulse control already present in pre-adolescence, and/or may have poorer improvements in impulse control across adolescence. Similarly, high risk youths may have elevated sensation seeking already present in pre-adolescence, and/or have greater increases in sensation-seeking across adolescence. A better understanding of how these processes develop in high-risk youth may improve our understanding of substance use disorder vulnerability.
One commonly studied high-risk population is adolescents with family histories of alcohol and other substance use disorders (FH+), and there is evidence that increased impulsivity and sensation seeking may contribute to their elevated risk. FH+ individuals are 4 to 7 times more likely to develop substance use disorders themselves than those without such family histories (FH−, Cotton, 1979, Merikangas, 1990), and FH+ youths who initiate substance use in early adolescence are particularly vulnerable to developing substance use disorders (Warner et al., 2007, Kramer et al., 2009, Dawson, 2000). Relative to FH− controls, FH+ pre-adolescents, adolescents, and adults have elevated self-reported impulsivity (Dick et al., 2010, Gierski et al., 2013, Dougherty et al., 2014, Handley et al., 2011), and FH+ adolescents and young adults with high family densities of alcohol use disorders have elevated sensation seeking (Finn et al., 1992, Handley et al., 2011). Further longitudinal studies indicate impulsivity and sensation seeking are important contributors to risk in FH+ individuals, For instance, impulsivity and sensation seeking has been shown to mediate links between parental alcoholism and the development of problem and alcohol and other drug use across adolescence and early adulthood (Chassin et al., 2004, King and Chassin, 2004). Similarly, increased impulsive behavior symptoms together with emotion dysregulation and cognitive impairments in pre-adolescence have both been linked to parental substance use disorders and shown to be predictive of developing substance use disorders in early adulthood (Chapman et al., 2007, Vanyukov et al., 2009). Furthermore, increased impulsivity in FH+ children as young as 3 years old predicts later development of substance use disorders (Martel et al., 2009). However, these studies did not directly compare impulse control and sensation seeking trajectories, thus it is unclear how these processes develop in FH+ youths (and consequently how these trajectories vary from typical adolescent development), although the above findings suggest that FH+ youths have overall greater impulsivity as well as increased sensation seeking that emerges by adolescence.
The current study characterized trajectories of self-reported impulsivity and sensation seeking in 305 FH+ and 81 FH− youths. Preadolescents (ages 10–12 years) were assessed at 6-month intervals and provided self-reports of impulsivity and sensation seeking for up to 42 months. In addition, to examine impulsivity and sensation seeking trajectories in higher and lower risk FH+ youths, a subset of 58 FH+ youths who began alcohol or other drug use before age 15 (FH+ Users) were compared to 58 FH+ youths who did not initiate substance use before age 15 (FH+ Non-Users). We tested the hypothesis that FH+ youths (compared to FH− youths) would have elevated impulsivity and sensation seeking in pre-adolescence, blunted decreases in impulsivity across early adolescence, and greater increases in sensation seeking across early adolescence. Similarly, we tested the hypothesis that FH+ Users (compared to FH+ Non-Users) would have elevated impulsivity and sensation seeking in pre-adolescence, blunted decreases in impulsivity across early adolescence, and greater increases in sensation seeking across early adolescence.
Methods
Participants
A total of 305 children with (FH+; n = 152 boys) and 81 children without (FH−; n = 35 boys) family histories of alcohol and other substance use disorders participated in this ongoing longitudinal study of substance use and impulsivity. Youths and their parents were recruited from the San Antonio, Texas community through radio, internet, and television advertisements targeting families with 10 to 12 year old children who had fathers who have had drug or alcohol problems and for families with no drug or alcohol problems who had 10 to 12 year old children. At study entry, all children were 10–12 years old. FH+ children were oversampled to increase the likelihood of obtaining a range of substance use outcomes. One parent or guardian participated with each child. Information about demographic characteristics, family history of substance use disorders, psychiatric disorders, and stressors was collected at entry. For a detailed description of this sample, see Ryan et al. (2016). The Institutional Review Board of The University of Texas Health Science Center at San Antonio approved the study procedures. Participant data were further protected by a Certificate of Confidentiality from the Department of Health and Human Services.
Screening and Study Procedures
At study entry, parents provided information about demographic characteristics, family history of substance use disorders, and family socioeconomic status (Four Factor Index of Social Status; Hollingshead, 1975). Pre-adolescents underwent a physical exam by a physician or physician’s assistant. Exclusion criteria included regular substance use by the child prior to study entry (defined as use at least once per month for six consecutive months; Clark et al., 2005); positive urine drug test at time of screening; low IQ (<70, Wechsler Abbreviated Scale of Intelligence; Wechsler, 1999); or physical/developmental disabilities that would interfere with the ability to complete study procedures. Substance use at later visits was not exclusionary. Psychiatric disorders, impulsivity, sensation seeking, and substance use were assessed at study entry and repeated at each visit. The median length of follow up was 30 months (spanning 6 assessment periods).
Families were classified as FH+ and FH− based on parental responses regarding psychiatric and substance abuse issues in first- and second-degree relatives on the Family History Assessment Module (Janca et al., 1992, Rice et al., 1995). All FH+ preadolescents had a biological father with a past or present substance use disorder; additional diagnoses in parents or other relatives were not exclusionary. FH− youths had no parents or grandparents with past or present substance use disorders. Symptoms of psychiatric disorders were evaluated (Schedule for Affective Disorders and Schizophrenia for School-Age Children-Present and Lifetime Version; Kaufman et al., 1997). FH− preadolescents with psychiatric diagnoses were excluded at study entry but retained if diagnosis occurred at later visits. Because Oppositional Defiant Disorder, Conduct Disorder, ADHD, Dysthymia, and Anxiety Disorders are commonly comorbid with substance use involvement and more common in FH+ individuals (Iacono et al., 2008), these diagnoses were not exclusionary at study entry for the FH+ group.
Upon arrival for each visit, parents and children were placed in separate sound-attenuated rooms to complete a battery of self-report, interview, and behavioral measures. Children provided expired-air samples to screen for recent alcohol use (AlcoTest® 7110 MKIII C, Dräger Safety Inc., Durango, CO) and urine samples to screen for the metabolites of recent drug use (THC, cocaine, benzodiazepines, opiates, and amphetamines; RediTest Panel-Dip Drug Screen, Redwood Toxicology Laboratory, Santa Rosa, CA) at each visit. Longitudinal follow-up appointments were scheduled at 6-month intervals. Participating children and parents were each paid $75 for completing the on-site screening visit and $120 each for the initial baseline study visit. For every subsequent follow up visit, children and parents were paid $120 and $75, respectively.
Measures
Impulsiveness
Youths were assessed on self-reported impulsiveness using the Barratt Impulsiveness Scale (BIS-11; Patton et al., 1995), a 30-item questionnaire in which respondents rate the frequency of several impulsive (e.g., “I do things without thinking”) or non-impulsive (“I am self-controlled”) behavioral traits on a scale from 1 = Rarely/never to 4 = Almost always/always. Scores across items are summed and Total impulsiveness scores can range from 30 to 120, with higher scores indicating more impulsiveness. Factor analyses of the BIS suggests at least 3 subscales can be derived with 11 items for Non-Planning impulsiveness (i.e., spontaneity, lack of careful planning), 8 items for Attentional impulsiveness (i.e., distractibility, inability to sustain attention), and 11 items Motor impulsiveness (i.e., fidgeting, restlessness; Patton et al., 1995). We examined reliability of the BIS-11 in this sample at baseline and observed all measures had adequate to good internal consistency (Cronbach’s α for BIS-11 Total = 0.75, Attentional = 0.57, Motor = 0.53, and Non-Planning = 0.66). The BIS-11 has previously been used to assess impulsiveness in pre- and early adolescents as well as substance-using populations (Burdick et al., 2013, Gilbert et al., 2011, Nandagopal et al., 2011, Sanches et al., 2014, Soloff et al., 2000).
Sensation seeking
The Sensation Seeking Scale for Children (SSS-C; Russo et al., 1993) is a self-report measure comprised of 40 forced-choice items used to assess an individual’s tendency towards varied, novel, complex, and intense situations. Participants are shown items such as “I’d like to try mountain climbing” and “I think people who do dangerous things like mountain climbing are foolish” and are asked to choose which option best described themselves. Items where the more sensation-averse option was endorsed are scored as 0, and items were the more sensation seeking option was endorsed were scored as 1. Total possible scores ranged from 0 to 40, with higher scores indicating greater sensation seeking. We examined reliability of the SSS-C in this sample at baseline and observed good internal consistency (Cronbach’s α = 0.85). The SSS-C has been related to risky behavior among pre and early adolescents (Aklin et al., 2005, Li et al., 2001, Russo et al., 1993) and predictive of adolescent substance use onset (Donohew et al., 1999).
Substance Use
In addition to breath and urine screenings to test for recent substance use, adolescents were also interviewed using a drug-history questionnaire that assessed patterns of use for a number of licit and illicit drugs (Dougherty et al., 2013). The drug history questionnaire assesses quantity and frequency of current (last month) and lifetime drug use, age at first use and liking of drug. Assessments are made separately for 14 drug classes (e.g. nicotine, alcohol, marijuana, cocaine, etc). These data were self-reported and answers were not shared with the parent/guardian.
Propensity Matching
FH+ Users (n=58) were identified as FH+ adolescents who initiated substance use prior to age 15, during the 42 months of testing after baseline. A 1-1 nearest neighbor propensity score matching without replacement method was used to select 58 FH+ who did not initiate substance use before age 15. Not all FH+ Non-User participants were age 15 during the 42 months of testing after baseline, however their lack of substance use prior to age 15 was verified as part of subsequent prospective monitoring of this cohort. Propensity scores were computed from a logistic regression model that included as covariates: number of visits, sex, ethnicity (Hispanic, Non-Hispanic), race (Caucasian, African-American), age at study entry in months (120–155), and IQ (70–133). Propensity scores were computed from a logistic regression model including all covariates in the previous propensity score model plus number of parents and grandparents with substance use disorders (0–6), internalizing disorder diagnosis, and externalizing disorder diagnosis. The goal was to reduce the imbalances baseline demographic characteristics between the FH+ User and FH+ Non-User groups on the aggregate level, which was achieved after propensity score matching.
Data Analyses
Demographic measures were analyzed with independent samples t tests or chi-square tests as appropriate. Changes in the primary dependent measures (BIS-11 subscales and Total score; SSS-C Total score) from ages 10 to 15 were analyzed using hierarchical linear modeling (HLM; Bryk and Raudenbush, 1987, Bryk and Raudenbush, 1992). HLM extends multiple linear regression modeling to repeated-measures data, provides a framework for analyzing individual change over time, and can accommodate time-invariant and time-varying predictors to determine whether individual characteristics are related to initial status or change over time. Changes in BIS-11 and SSS-C scores were modeled as functions of age in half-year increments from 10 to 15 years; group membership (FH+ or FH−) was then added as a predictor of initial status at pre-adolescence and change over time across adolescence. To examine trajectories of impulsiveness and sensation seeking in relation to substance use during adolescence, these analyses were repeated with propensity-matched groups (FH+ Users and FH+ Non-Users), with matched group membership as a predictor of initial status at pre-adolescence and change over time across adolescence. IQ and SES were not associated with the sensation seeking and impulsivity measures either at baseline or over time and including these items as covariates did not affect the outcomes of our analyses. As a result IQ and SES were not included as covariates in our final analyses.
Propensity score matching was performed using Stata (Version 13, StataCorp, College Station, Texas). Other analyses were conducted using SPSS (Version 21; IBM Corp., Armonk, NY) and SAS software (SAS Institute, Inc., Cary, North Carolina). HLMs were fit using a compound symmetry covariance structure for the repeated-measures and fixed effects for the intercepts and slopes; SAS PROC MIXED was used to fit all models using restricted maximum likelihood estimation, which accounts for missing data on the repeated-measures outcomes under the missing at random assumption. In order to examine nonlinear effects of age, cubic and quadratic terms for age were tested, however these results were generally non significant or significant but negligible effects and are not reported.
Results
Participant Characteristics
Demographics
Group demographic characteristics for both the full sample and propensity matched groups at study entry are presented in Table 1. The groups did not differ in age at study entry, sex ratios, race, or ethnicity, though FH+ adolescents (including both User and Non-Users) had lower socioeconomic status and lower IQs than did FH− youth. The FH+ groups did not significantly differ in psychiatric health histories.
Table 1.
Demographic Characteristics at Study Entry
| FH+ Full Sample n = 305 | FH− Full Sample n = 81 | FH+ Users n = 58 | FH+ Non- Users n = 58 | |||||
|---|---|---|---|---|---|---|---|---|
| M | (SD) | M | (SD) | M | (SD) | M | (SD) | |
|
| ||||||||
| Age at Study Entry | 10.96 | (0.85) | 11.05 | (0.82) | 11.62 | (0.92) | 11.61 | (0.85) |
| Age at Last Testing | 14.7 | (1.4) | 14.7 | (1.6) | 14.58 | (0.70) | 14.83 | (0.60) |
| Total IQ Score | 94.88 | (11.18) | 102.32 | (12.18)* | 95.43 | (11.62) | 93.22 | (11.34) |
| Socioeconomic Status | 43.5 | (10.8) | 32.2 | (11.4)* | 31.10 | (10.47) | 31.39 | (11.16) |
| Family Density1 | 2.80 | (1.23) | - | - | 2.91 | (1.26) | 2.87 | (1.18) |
|
| ||||||||
| n | (%) | n | (%) | n | (%) | n | (%) | |
|
| ||||||||
| Sex | ||||||||
| Male | 152 | (50) | 35 | (43) | 27 | (47) | 27 | (47) |
| Female | 153 | (50) | 46 | (57) | 31 | (53) | 31 | (53) |
| Race | ||||||||
| African-American | 37 | (12) | 5 | (6) | 6 | (10) | 5 | (9) |
| Caucasian | 261 | (86) | 74 | (91) | 51 | (88) | 51 | (88) |
| Other | 7 | (2) | 2 | (2) | 1 | (2) | 2 | (3) |
| Ethnicity | ||||||||
| Hispanic/Latino | 246 | (81) | 57 | (70) | 46 | (79) | 53 | (91) |
| Psychiatric Disorders | ||||||||
| ADHD | 90 | (30) | 0 | (0) | 18 | (31) | 13 | (22) |
| Disruptive Behavior Disorder NOS | 18 | (6) | 0 | (0) | 2 | (3) | 1 | (2) |
| Oppositional Defiant Disorder | 29 | (10) | 0 | (0) | 7 | (12) | 6 | (10) |
| Conduct Disorder | 2 | (1) | 0 | (0) | 0 | (0) | 0 | (0) |
| Dysthymia | 1 | (0) | 0 | (0) | 0 | (0) | 0 | (0) |
| Anxiety Disorders | 57 | (19) | 0 | (0) | 6 | (10) | 12 | (20) |
| Drug Use2 | ||||||||
| Marijuana | 58 | (19) | 5 | (6) | 40 | (69) | 0 | (0) |
| Alcohol | 64 | (21) | 10 | (12) | 40 | (69) | 0 | (0) |
| Tobacco | 31 | (10) | 3 | (4) | 21 | (36) | 0 | (0) |
| Stimulants | 4 | (1) | 0 | (0) | 3 | (5) | 0 | (0) |
| Hallucinogens | 2 | (1) | 1 | (1) | 2 | (3) | 0 | (0) |
| Inhalants | 2 | (1) | 0 | (0) | 1 | (2) | 0 | (0) |
| Sedatives | 3 | (1) | 0 | (0) | 1 | (2) | 0 | (0) |
Note.
Family density = the number of biological parents or grandparents with a substance use disorder;
mean age of use = 13.5 (SD = 1.06); median number of substances each adolescent used = 2 (range = 1–3).
indicates significant difference (p < .05) from FH+ youths.
A total of 386 participants provided data at up to 8 assessment visits, one every 6 months from baseline to 42 months post-baseline. A total of 39 participants (9% of the sample) were lost to attrition across the entire observation period. Approximately 85–90% of participants completed their 6 month to 30 month assessment visits. Absences were due to a combination of attrition and participants still enrolled in the study occasionally missing a study visit. Completion of the 36 and 42 months assessments dropped to 74% and 51% respectively. This drop was due in part to only 94% of subjects being enrolled in the study long enough to be due for their 36 month assessment visits and only 79% being enrolled long enough to be due for their 42 month visits. As a result 173 participants provided data at 8 assessments, 93 participants at 7 assessments, 54 participants at 6 assessments, 20 participants at 5 assessments, 6 participants at 4 assessments, 15 participants at 3 assessments, 13 participants at 2 assessments, and 12 participants at 1 assessment.
For analysis, participants were organized according to age, rounded to half-year increments: 60 participants provided data at age 10, 118 at age 10.5, 177 at age 11, 233 at age 11.5, 284 at age 12, 335 at age 12.5, 330 at age 13, 310 at age 13.5, 261 at age 14, 210 at age 14.5, and 149 at age 15. At the baseline assessment, 60 participants were aged 10, 68 aged 10.5, 64 aged 11, 58 aged 11.5, 58 aged 12, and 79 aged 12.5.
Substance Use
Participants’ substance use from the drug history interview is also reported in Table 1. Mean age of substance use initiation was 13.5 years, and FH+ Users reported using 2 substances on average. The most commonly used substance was marijuana, followed by alcohol, and then tobacco. Only four participants reported using any additional substances.
Substance Use Disorder Family Histories
Substance use disorder histories in FH+ parents and grandparents are reported in Table 2. Most FH+ youths had a father with an alcohol use disorder history and over half had fathers with cannabis and cocaine use disorder histories. Some had FH+ youths had mothers with substance use disorder histories, most commonly for alcohol, cannabis, or cocaine. Substance use disorder histories were also present in over half of FH+ youths paternal and maternal grandfathers and about a quarter of paternal and maternal grandmothers. Like for FH+ parents, the most common substance use disorders among FH+ grandparents were for alcohol, cannabis, and cocaine use disorders.
Table 2.
Substance use disorder histories in FH+ parents and grandparents
| FH+ Full Sample n= 305 | FH+ Users n = 58 | FH+ Non-Users n = 58 | ||||
|---|---|---|---|---|---|---|
| n | (%) | n | (%) | n | (%) | |
| Paternal substance use disorder history | ||||||
| -Alcohol use disorder | 232 | (76) | 42 | (72) | 49 | (84) |
| -Cannabis use disorder | 178 | (58) | 38 | (66) | 36 | (62) |
| -Cocaine use disorder | 181 | (59) | 37 | (64) | 33 | (57) |
| -Other drug use disorder | 96 | (32) | 27 | (47) | 18 | (31) |
| Maternal substance use disorders History | ||||||
| -Alcohol use disorder | 51 | (17) | 8 | (14) | 11 | (19) |
| -Cannabis use disorder | 37 | (12) | 7 | (12) | 9 | (16) |
| -Cocaine use disorder | 38 | (13) | 7 | (12) | 8 | (14) |
| -Other drug use disorder | 23 | (8) | 9 | (16) | 4 | (7) |
| Grandparent any substance use disorder history | ||||||
| -Paternal grandfather | 158 | (52) | 32 | (55) | 35 | (60) |
| -Paternal grandmother | 77 | (25) | 17 | (29) | 14 | (24) |
| -Maternal grandfather | 158 | (52) | 33 | (57) | 31 | (53) |
| -Maternal grandmother | 65 | (21) | 13 | (22) | 15 | (26) |
Impulsivity and Sensation Seeking
For all analyses, see top half of Table 3 for parameter estimates at pre-adolescence (intercept differences); see bottom half for the trajectories across adolescence (slope differences). Parameter estimates are beta weights with standard errors.
Table 3.
Comparison of FH+ vs. FH− youths and FH+ Users vs. Non- Users at study entry and across early adolescence
| FH+ vs. FH− | FH+ Users vs. FH+ Non-Users | |
|---|---|---|
| At Study Entry1 | ||
| BIS-11 | ||
| Total | 3.91 (1.29)* | 0.19 (1.84) |
| Non-Planning | 1.87 (0.68)* | 0.36 (1.02) |
| Attentional | 1.20 (0.50)* | 0.42 (0.72) |
| Motor | 0.89 (0.50) | −0.35 (0.77) |
| SSS-C | ||
| Total | 0.22 (0.66) | −1.27 (1.07) |
| Across Adolescence2 | ||
| BIS-11 | ||
| Total | −0.03 (0.14) | 0.54 (0.21)* |
| Non-Planning | 0.06 (0.08) | 0.17 (0.12) |
| Attentional | 0.01 (0.06) | 0.08 (0.09) |
| Motor | −0.10 (0.07) | 0.25 (0.10)* |
| SSS-C | ||
| Total | 0.06 (0.07) | 0.69 (0.10)* |
Note. Beta weights with standard errors in parentheses.
Intercept;
Slopes.
indicates significant difference (p < .05)
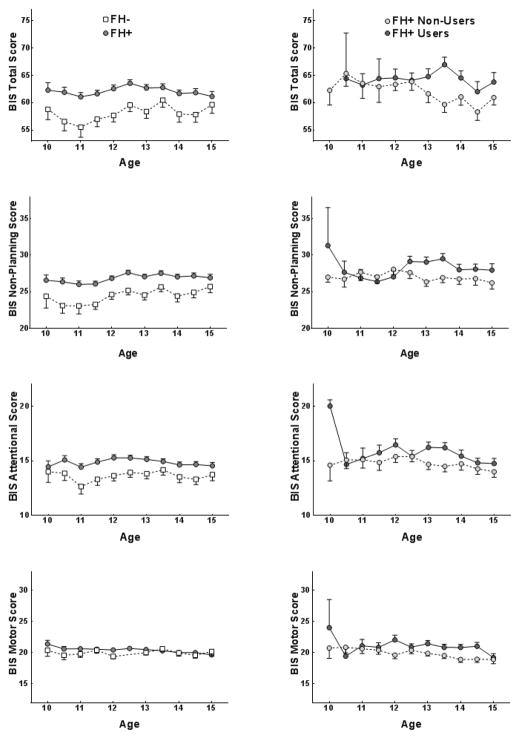
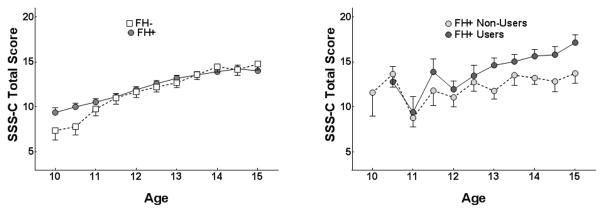
FH+ and FH−
At pre-adolescence, FH+ youths had significantly higher Total impulsiveness, Non-Planning, and Attentional impulsiveness than FH− youths (Figure 1, left panel). Across adolescence, there were no effects of FH+ status on change over time for any of the impulsiveness measures. FH+ and FH− youths were also not different on sensation seeking at preadolescence, and there were also not effects of FH status on change over time (Figure 2, left panel). These results were not affected by excluding FH+ youths with psychiatric diagnoses from the analyses.
Figure 1.
Barratt Impulsiveness Scale (BIS-11) scores on Total, Non-Planning, Attentional, and Motor impulsiveness (means and standard error) across ages 10–15 are shown for FH+ and FH− youths (left panel) and FH+ Users and FH+ Non-Users (right panel).
Figure 2.
Sensation Seeking Scale (SSS-C) scores (means and standard error) across ages 10–15 are shown for FH+ and FH− youths (left panel) and FH+ Users and FH+ Non-Users (right panel).
FH+ Users and FH+ Non-Users
FH+ Users and Non-Users were not different on any of impulsiveness measures or sensation seeking at pre-adolescence (Figure 1, right panel). Across adolescence, FH+ Non-Users had greater decreases in Total and Motor impulsiveness. FH+ Users had greater increases in sensation seeking (Figure 2, right panel). These analyses included living with the biological father or not as a control variable, however including this variable did not change the substantive results for any outcome measures.
Discussion
FH+ youths reported higher overall impulsivity (Total impulsiveness) and higher impulsivity related to lack of planning and poor attention (Non-Planning and Attentional impulsiveness) than FH− individuals at pre-adolescence. There were no differential effects of FH status on changes in these measures or sensation seeking across adolescence. When comparing FH+ youths who initiated drug use before 15 (FH+ Users) to FH+ youths who had been prospectively determined not to initiate drug use before 15 (FH+ Non-Users), FH+ Non-Users had greater decreases in Total and Motor impulsiveness, while FH+ Users had greater increases in sensation seeking.
The present study extends previous findings on both impulsivity and sensation seeking in FH+ individuals. Our findings of increased impulsivity in FH+ youths are consistent with previous findings in FH+ pre-adolescents, adolescents, and adults tested with both self-report and laboratory behavioral measures (Dick et al., 2010, Gierski et al., 2013, Dougherty et al., 2014, Handley et al., 2011, Acheson et al., 2011a, Acheson et al., 2011b, Lieb et al., 2002, Saunders et al., 2008, Nigg et al., 2004). The consistency among these findings suggests that elevated impulsivity in individuals with substance use disorders (de Wit, 2009, MacKillop, 2013, Verdejo-Garcia and Perez-Garcia, 2007, Li et al., 2009) likely at least partially pre-dates problem substance use. Similarly, the elevated sensation seeking in FH+ Users is consistent with findings in FH+ adolescents and young adults with high family densities of alcohol use disorders (Finn et al., 1992, Handley et al., 2011), suggesting that this elevated sensation seeking may emerge by mid-adolescence, at least in higher risk FH+ youths.
Impulsivity and sensation seeking appear to be distinct constructs that develop independently, with sensation seeking rapidly increasing through mid-adolescence but decreasing by early adulthood and impulsivity more steadily decreasing through later adolescence to early adulthood (Harden and Tucker-Drob, 2011, Shulman et al., 2014). The disparity between rapid increases in sensation seeking and slower decreases in impulsivity is thought to contribute to liability to engage in alcohol and other drug use and other problem behaviors in adolescence (Ernst et al., 2006, Steinberg et al., 2008, Shulman et al., 2014). Our results help extend previous work in this area by identifying how pre to mid-adolescent trajectories of impulsivity and sensation seeking are altered in FH+ youths. Our findings suggest FH+ adolescents have larger relative gaps between impulse control and sensation seeking because of both elevated impulsivity and greater increases in sensation in high risk FH+ youths. The resulting impaired ability to regulate sensation seeking drives may plausibly contribute to FH+ youths’ increased vulnerability to developing alcohol and other substance use disorders. Thus, the enhanced risk for substance use disorders in FH+ youths may be at least partially driven by developmental processes present for all youth, but at a more risky end of their continuums of variation.
This study had limitations. Our cohort was recruited through advertising, thus potential participants were self-selected and may not be fully representative of the FH+ and FH− youth in our area. Further, while our sample demographics of mostly Caucasian and Hispanic participants are consistent with the greater San Antonio metropolitan area, these findings may not necessarily generalize to other ethnic and racial FH+ and FH− populations. This study relied on self-report data and did not include parent or other third party report measures, although the measures we used have been successfully used in populations this age this age range before (e.g., Li et al., 2001, Gilbert et al., 2011, Nandagopal et al., 2011, Sanches et al., 2014). Furthermore, we included FH+ but not FH− youths with disorders common in families with substance use disorders because these diagnoses are associated with increased vulnerability for developing problem substance use (Iacono et al., 2008, Tarter, 2002). However, our follow-up analyses indicated these disorders did not drive the FH group differences, and we were still able differentiate FH+ Users and Non-Users on impulsivity and sensation seeking despite these groups being matched on disorder diagnoses. Finally FH+ youths had lower SES and IQ than FH− youths, although neither of these items was associated with the impulsivity and sensation seeking measures either at baseline or across adolescence.
In summary, increased impulsivity in FH+ youths may make them less able to regulate sensation seeking drives that peak in adolescence, which may contribute to their increased risk for developing substance use disorders. It will be important for future studies to examine how processes develop across late adolescence in FH+ youth and examine reciprocal interactions with the development and progression of substance use disorders. It will also be of interest to examine how environmental factors such as substance use in the extended family, peer relationships, and stressful life events interact with impulsivity and sensation seeking on substance use disorder outcomes. A better understanding of how these processes influence risk may lead to improved prevention and treatment strategies in vulnerable youths.
Acknowledgments
Research reported in this publication was supported by NIDA and NIMH of the National Institutes of Health under award numbers R01-DA026868, R01-DA033997, R01-MH081181, and R01-AA012207. DMD is the recipient of the William and Marguerite Wurzbach Distinguished Professorship. The content is solely the view of the authors and does not necessarily represent the official view of the National Institutes of Health.
References
- Acheson A, Richard DM, Mathias CW, Dougherty DM. Adults with a family history of alcohol related problems are more impulsive on measures of response initiation and response inhibition. Drug and Alcohol Dependence. 2011a;117:198–203. doi: 10.1016/j.drugalcdep.2011.02.001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Acheson A, Vincent AS, Sorocco KH, Lovallo WR. Greater discounting of delayed rewards in young adults with family histories of alcohol and drug use disorders: studies from the Oklahoma family health patterns project. Alcoholism: Clinical and Experimental Research. 2011b;35:1607–1613. doi: 10.1111/j.1530-0277.2011.01507.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Aklin WM, Lejuez CW, Zvolensky MJ, Kahler CW, Gwadz M. Evaluation of behavioral measures of risk taking propensity with inner city adolescents. Behavioral Research and Therapy. 2005;43:215–228. doi: 10.1016/j.brat.2003.12.007. [DOI] [PubMed] [Google Scholar]
- Bjork JM, Pardini DA. Who are those “risk-taking adolescents”? Individual differences in developmental neuroimaging research. Developmental cognitive neuroscience. 2015;11:56–64. doi: 10.1016/j.dcn.2014.07.008. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bryk AS, Raudenbush SW. Application of hierarchical linear models to assessing change. Psychological Bulletin. 1987;101:147–158. [Google Scholar]
- Bryk AS, Raudenbush SW. Hierarchical linear models. Sage; Newbury Park, CA: 1992. [Google Scholar]
- Burdick JD, Roy AL, Raver CC. Evaluating the Iowa Gambling Task as a direct assessment of impulsivity with low-income children. Personality and Individual Differences. 2013;55:771–776. doi: 10.1016/j.paid.2013.06.009. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Chapman K, Tarter RE, Kirisci L, Cornelius MD. Childhood neurobehavior disinhibition amplifies the risk of substance use disorder: interaction of parental history and prenatal alcohol exposure. J Dev Behav Pediatr. 2007;28:219–224. doi: 10.1097/DBP.0b013e3180327907. [DOI] [PubMed] [Google Scholar]
- Chassin L, Fora DB, King KM. Trajectories of alcohol and drug use and dependence from adolescence to adulthood: the effects of familial alcoholism and personality. J Abnorm Psychol. 2004;113:483–498. doi: 10.1037/0021-843X.113.4.483. [DOI] [PubMed] [Google Scholar]
- Clark DB, Cornelius JR, Kirisci L, Tarter RE. Childhood risk categories for adolescent substance involvement: a general liability typology. Drug and Alcohol Dependence. 2005;77:13–21. doi: 10.1016/j.drugalcdep.2004.06.008. [DOI] [PubMed] [Google Scholar]
- Cotton NS. The familial incidence of alcoholism: a review. Journal of Studies on Alcohol. 1979;40:89–116. doi: 10.15288/jsa.1979.40.89. [DOI] [PubMed] [Google Scholar]
- Dawson DA. The link between family history and early onset alcoholism: earlier initiation of drinking or more rapid development of dependence? Journal of Studies on Alcohol. 2000;61:637–646. doi: 10.15288/jsa.2000.61.637. [DOI] [PubMed] [Google Scholar]
- de Wit H. Impulsivity as a determinant and consequence of drug use: a review of underlying processes. Addiction Biology. 2009;14:22–31. doi: 10.1111/j.1369-1600.2008.00129.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Dick DM, Smith G, Olausson P, Mitchell SH, Leeman RF, O’Malley SS, Sher K. Understanding the construct of impulsivity and its relationship to alcohol use disorders. Addiction Biology. 2010;15:217–226. doi: 10.1111/j.1369-1600.2009.00190.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Donohew RL, Hoyle RH, Clayton RR, Skinner WF, Colon SE, Rice RE. Sensation seeking and drug use by adolescents and their friends: models for marijuana and alcohol. Journal of Studies on Alcohol. 1999;60:622–631. doi: 10.15288/jsa.1999.60.622. [DOI] [PubMed] [Google Scholar]
- Dougherty DM, Charles NE, Mathias CW, Ryan SR, Olvera RL, Liang Y, Acheson A. Delay discounting differentiates pre-adolescents at high and low risk for substance use disorders based on family history. Drug and Alcohol Dependence. 2014;143:105–111. doi: 10.1016/j.drugalcdep.2014.07.012. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Dougherty DM, Mathias CW, Dawes MA, Furr RM, Charles NE, Liguori A, Shannon EE, Acheson A. Impulsivity, attention, memory, and decision-making among adolescent marijuana users. Psychopharmacology (Berl) 2013;226:307–319. doi: 10.1007/s00213-012-2908-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ernst M, Pine DS, Hardin M. Triadic model of the neurobiology of motivated behavior in adolescence. Psychological Medicine. 2006;36:299–312. doi: 10.1017/S0033291705005891. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Finn PR, Earleywine M, Pihl RO. Sensation seeking, stress reactivity, and alcohol dampening discriminate the density of a family history of alcoholism. Alcoholism: Clinical and Experimental Research. 1992;16:585–590. doi: 10.1111/j.1530-0277.1992.tb01421.x. [DOI] [PubMed] [Google Scholar]
- Gierski F, Hubsch B, Stefaniak N, Benzerouk F, Cuervo-Lombard C, Bera-Potelle C, Cohen R, Kahn JP, Limosin F. Executive functions in adult offspring of alcohol-dependent probands: toward a cognitive endophenotype? Alcoholism: Clinical and Experimental Research. 2013;37(Suppl 1):E356–363. doi: 10.1111/j.1530-0277.2012.01903.x. [DOI] [PubMed] [Google Scholar]
- Gilbert KE, Kalmar JH, Womer FY, Markovich PJ, Pittman B, Nolen-Hoeksema S, Blumberg HP. Impulsivity in Adolescent Bipolar Disorder. Acta Neuropsychiatr. 2011;23:57–61. doi: 10.1111/j.1601-5215.2011.00522.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Grant BF, Dawson DA. Age at onset of alcohol use and its association with DSM-IV alcohol abuse and dependence: Results from the national longitudinal alcohol epidemiologic survey. Journal of substance abuse. 1997;9:103–110. doi: 10.1016/s0899-3289(97)90009-2. [DOI] [PubMed] [Google Scholar]
- Handley ED, Chassin L, Haller MM, Bountress KE, Dandreaux D, Beltran I. Do executive and reactive disinhibition mediate the effects of familial substance use disorders on adolescent externalizing outcomes? Journal of Abnormal Psychology. 2011;120:528–542. doi: 10.1037/a0024162. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Harden KP, Tucker-Drob EM. Individual differences in the development of sensation seeking and impulsivity during adolescence: further evidence for a dual systems model. Developmental Psychology. 2011;47:739–746. doi: 10.1037/a0023279. [DOI] [PubMed] [Google Scholar]
- Hollingshead AB. Four Factor Index of Social Status. Department of Sociology, Yale University; New Haven, CT: 1975. [Google Scholar]
- Iacono WG, Malone SM, McGue M. Behavioral disinhibition and the development of early-onset addiction: common and specific influences. Annual Review of Clinical Psychology. 2008;4:325–348. doi: 10.1146/annurev.clinpsy.4.022007.141157. [DOI] [PubMed] [Google Scholar]
- Janca A, Bucholz K, Janca I. Family History Assessment Module. Washington University School of Medicine; St. Louis, MO: 1992. [Google Scholar]
- Kaufman J, Birmaher B, Brent D, Rao U, Flynn C, Moreci P, Williamson D, Ryan N. Schedule for Affective Disorders and Schizophrenia for School-Age Children-Present and Lifetime Version (K-SADS-PL): initial reliability and validity data. Journal of the American Academy of Child and Adolescent Psychiatry. 1997;36:980–988. doi: 10.1097/00004583-199707000-00021. [DOI] [PubMed] [Google Scholar]
- King KM, Chassin L. Mediating and moderated effects of adolescent behavioral undercontrol and parenting in the prediction of drug use disorders in emerging adulthood. Psychology of Addictive Behaviors. 2004;18:239–249. doi: 10.1037/0893-164X.18.3.239. [DOI] [PubMed] [Google Scholar]
- Kramer TL, Han X, Leukefeld C, Booth BM, Edlund C. Childhood conduct problems and other early risk factors in rural adult stimulant users. Journal of Rural Health. 2009;25:50–57. doi: 10.1111/j.1748-0361.2009.00198.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Li CS, Luo X, Yan P, Bergquist K, Sinha R. Altered impulse control in alcohol dependence: neural measures of stop signal performance. Alcohol Clin Exp Res. 2009;33:740–750. doi: 10.1111/j.1530-0277.2008.00891.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Li X, Stanton B, Cottrell L, Burns J, Pack R, Kaljee L. Patterns of initiation of sex and drug-related activities among urban low-income African-American adolescents. Journal of Adolescent Health. 2001;28:46–54. doi: 10.1016/s1054-139x(00)00173-7. [DOI] [PubMed] [Google Scholar]
- Lieb R, Isensee B, Hofler M, Pfister H, Wittchen HU. Parental major depression and the risk of depression and other mental disorders in offspring: a prospective-longitudinal community study. Archives of General Psychiatry. 2002;59:365–374. doi: 10.1001/archpsyc.59.4.365. [DOI] [PubMed] [Google Scholar]
- Littlefield AK, Sher KJ, Steinley D. Developmental trajectories of impulsivity and their association with alcohol use and related outcomes during emerging and young adulthood I. Alcoholism: Clinical and Experimental Research. 2010;34:1409–1416. doi: 10.1111/j.1530-0277.2010.01224.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Littlefield AK, Sher KJ, Wood PK. Is “maturing out” of problematic alcohol involvement related to personality change? Journal of Abnormal Psychology. 2009;118:360–374. doi: 10.1037/a0015125. [DOI] [PMC free article] [PubMed] [Google Scholar]
- MacKillop J. Integrating behavioral economics and behavioral genetics: delayed reward discounting as an endophenotype for addictive disorders. Journal of the Experimental Analysis of Behavior. 2013;99:14–31. doi: 10.1002/jeab.4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Martel MM, Pierce L, Nigg JT, Jester JM, Adams K, Puttler LI, Buu A, Fitzgerald H, Zucker RA. Temperament pathways to childhood disruptive behavior and adolescent substance abuse: testing a cascade model. J Abnorm Child Psychol. 2009;37:363–373. doi: 10.1007/s10802-008-9269-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Merikangas KR. The genetic epidemiology of alcoholism. Psychological Medicine. 1990;20:11–22. doi: 10.1017/s0033291700013192. [DOI] [PubMed] [Google Scholar]
- Moeller FG, Barratt ES, Dougherty DM, Schmitz JM, Swann AC. Psychiatric aspects of impulsivity. The American Journal of Psychiatry. 2001;158:1783–1793. doi: 10.1176/appi.ajp.158.11.1783. [DOI] [PubMed] [Google Scholar]
- Nandagopal JJ, Fleck DE, Adler CM, Mills NP, Strakowski SM, DelBello MP. Impulsivity in adolescents with bipolar disorder and/or attention-deficit/hyperactivity disorder and healthy controls as measured by the Barratt Impulsiveness Scale. Journal of Child and Adolescent Psychopharmacology. 2011;21:465–468. doi: 10.1089/cap.2010.0096. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Nigg JT, Glass JM, Wong MM, Poon E, Jester JM, Fitzgerald HE, Puttler LI, Adams KM, Zucker RA. Neuropsychological executive functioning in children at elevated risk for alcoholism: findings in early adolescence. J Abnorm Psychol. 2004;113:302–314. doi: 10.1037/0021-843X.113.2.302. [DOI] [PubMed] [Google Scholar]
- Patton JH, Stanford MS, Barratt ES. Factor structure of the Barratt impulsiveness scale. Journal of Clinical Psychology. 1995;51:768–774. doi: 10.1002/1097-4679(199511)51:6<768::aid-jclp2270510607>3.0.co;2-1. [DOI] [PubMed] [Google Scholar]
- Pedersen SL, Molina BS, Belendiuk KA, Donovan JE. Racial differences in the development of impulsivity and sensation seeking from childhood into adolescence and their relation to alcohol use. Alcoholism: Clinical and Experimental Research. 2012;36:1794–1802. doi: 10.1111/j.1530-0277.2012.01797.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Quinn PD, Harden KP. Differential changes in impulsivity and sensation seeking and the escalation of substance use from adolescence to early adulthood. Development and psychopathology. 2013;25:223–239. doi: 10.1017/S0954579412000284. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Rice JP, Reich T, Bucholz KK, Neuman RJ, Fishman R, Rochberg N, Hesselbrock VM, Nurnberger JI, Jr, Schuckit MA, Begleiter H. Comparison of direct interview and family history diagnoses of alcohol dependence. Alcoholism: Clinical and Experimental Research. 1995;19:1018–1023. doi: 10.1111/j.1530-0277.1995.tb00983.x. [DOI] [PubMed] [Google Scholar]
- Russo M, Stokes G, Lahey B, Christ M, McBurnett K, Loeber R, Stouthamer-Loeber M, Green S. A sensation seeking scale for children: Further refinement and psychometric development. Journal of Psychopathology and Behavioral Assessment. 1993;15:69–86. [Google Scholar]
- Ryan SR, Acheson A, Charles NE, Lake SL, Hernandez DL, Mathias CW, Dougherty DM. Clinical and Social/Environmental Characteristics in a Community Sample of Children With and Without Family Histories of Substance Use Disorder in the San Antonio Area: A Descriptive Study. Journal of Child & Adolescent Substance Abuse. 2016;25:327–339. doi: 10.1080/1067828X.2014.999202. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Sanches M, Scott-Gurnell K, Patel A, Caetano SC, Zunta-Soares GB, Hatch JP, Olvera R, Swann AC, Soares JC. Impulsivity in children and adolescents with mood disorders and unaffected offspring of bipolar parents. Comprehensive Psychiatry. 2014;55:1337–1341. doi: 10.1016/j.comppsych.2014.04.018. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Saunders B, Farag N, Vincent AS, Collins FL, Jr, Sorocco KH, Lovallo WR. Impulsive errors on a Go-NoGo reaction time task: disinhibitory traits in relation to a family history of alcoholism. Alcohol Clin Exp Res. 2008;32:888–894. doi: 10.1111/j.1530-0277.2008.00648.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Shulman EP, Harden KP, Chein JM, Steinberg L. The development of impulse control and sensation-seeking in adolescence: independent or interdependent processes? Journal of Research on Adolescence. 2014:1–8. [Google Scholar]
- Soloff PH, Lynch KG, Moss HB. Serotonin, impulsivity, and alcohol use disorders in the older adolescent: A psychobiological study. Alcoholism: Clinical and Experimental Research. 2000;24:1609–1619. [PubMed] [Google Scholar]
- Somerville LH, Casey BJ. Developmental neurobiology of cognitive control and motivational systems. Current Opinion in Neurobiology. 2010;20:236–241. doi: 10.1016/j.conb.2010.01.006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Steinberg L, Albert D, Cauffman E, Banich M, Graham S, Woolard J. Age differences in sensation seeking and impulsivity as indexed by behavior and self-report: evidence for a dual systems model. Developmental Psychology. 2008;44:1764–1778. doi: 10.1037/a0012955. [DOI] [PubMed] [Google Scholar]
- Tarter RE. Etiology of adolescent substance abuse: a developmental perspective. Am J Addict. 2002;11:171–191. doi: 10.1080/10550490290087965. [DOI] [PubMed] [Google Scholar]
- Vanyukov M, Kirisci L, Moss L, Tarter R, Reynolds M, Maher B, Kirillova G, Ridenour T, Clark D. Measurement of the Risk for Substance Use Disorders: Phenotypic and Genetic Analysis of an Index of Common Liability. Behav Genet. 2009;39:233–244. doi: 10.1007/s10519-009-9269-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Verdejo-Garcia A, Perez-Garcia M. Profile of executive deficits in cocaine and heroin polysubstance users: common and differential effects on separate executive components. Psychopharmacology (Berl) 2007;190:517–530. doi: 10.1007/s00213-006-0632-8. [DOI] [PubMed] [Google Scholar]
- Warner LA, White HR, Johnson V. Alcohol initiation experiences and family history of alcoholism as predictors of problem-drinking trajectories. Journal of Studies on Alcohol and Drugs. 2007;68:56–65. doi: 10.15288/jsad.2007.68.56. [DOI] [PubMed] [Google Scholar]
- Webb JA, Baer PE, McLaughlin RJ, McKelvey RS, Caid CD. Risk factors and their relation to initiation of alcohol use among early adolescents. Journal of the American Academy of Child and Adolescent Psychiatry. 1991;30:563–568. doi: 10.1097/00004583-199107000-00006. [DOI] [PubMed] [Google Scholar]
- Wechsler . Wechsler Abbreviated Scale of Intelligence (WASI) Manual. Psychological Corporation; San Antonio, TX: 1999. [Google Scholar]
- Zuckerman M, Link K. Construct validity for the sensation-seeking scale. Journal of Consulting and Clinical Psychology. 1968;32:420–426. doi: 10.1037/h0026047. [DOI] [PubMed] [Google Scholar]