Abstract
To understand the persistence of latently HIV-1 infected cells in virally suppressed infected patients, a number of in vitro models of HIV latency have been developed. In an attempt to mimic the in vivo situation as closely as possible, several models use primary cells and replication-competent viruses in combination with antiretroviral compounds to prevent ongoing replication. Latency is subsequently measured by HIV RNA and/or protein production after cellular activation. To discriminate between pre- and post-integration latency, integrase inhibitors are routinely used, preventing novel integrations upon cellular activation. Here, we show that this choice of antiretrovirals may still cause a bias of pre-integration latency in these models, as unintegrated HIV DNA can form and directly contribute to the levels of HIV RNA and protein production. We further show that the addition of reverse transcriptase inhibitors effectively suppresses the levels of episomal HIV DNA (as measured by 2-LTR circles) and decreases the levels of HIV transcription. Consequently, we show that latency levels described in models that only use integrase inhibitors may be overestimated. The inclusion of additional control conditions, such as 2-LTR quantification and the addition of reverse transcriptase inhibitors, is crucial to fully elucidate the actual levels of post-integration latency.
In HIV-1 infected individuals, combination antiretroviral therapy (ART) is able to suppress HIV replication but it fails to clear the virus. This is due to a reservoir of latently infected cells that evade the host immune response and persist throughout the lifetime of infected patients. HIV-1 latency is a dynamic state defined by infected cells containing integrated provirus that does not produce progeny viral particles, but remains capable to do so1. Latent HIV reservoirs are intensively studied as they are considered as the last step on the road to full HIV cure2.
It is estimated that for every million resting CD4+ T cells only one latently infected cell can be found in patients on long term ART3. This extremely low frequency of cells combined with the lack of methods capable to specifically target or isolate these cells underscores the need for in vitro models of HIV latency4. HIV latency models are used to study the molecular aspects of HIV latency formation and maintenance, but also to screen for candidate latency reversing agents (LRA) that could reactivate latent HIV in a so-called “shock and kill” strategy to clear HIV reservoirs. Initially, most research was performed on latently infected cell lines with integrated silent proviruses. However, these cell lines may not form a good mimic of the in vivo situation. Clonal cells are highly homogeneous and do not reflect the diversity of CD4+ T cell populations in vivo2. Additional limitations of latent cell lines include the cell cycle status (resting or dividing cells), the inability to change the proliferation status (active or quiescent cells) as well as the clonal HIV integration sites5. Recently, a number of latency models have been developed with primary CD4+ T cells and with infectious virus to mimic the in vivo situation as closely as possible6,7,8. These models better represent the diversity of CD4 T cells in vivo and multiple distinct infections lead to a number of different integrated proviruses in multiple genomic sites. To prevent ongoing replication in primary HIV latency models with infectious virus, ART treatment is routinely performed5,7,8,9,10,11,12.
HIV latency can be broadly classified into two forms, i.e. pre- and post-integration latency. Pre-integration latency refers to cells that are infected by HIV but in which the HIV DNA did not yet integrate. This includes viral particles that recently entered the host cell and have not completed reverse transcription, or HIV DNA that has not yet integrated into the genome of the host cell. Post-integration latency refers to cells that harbour integrated HIV DNA that is transcriptionally silent, yet fully competent to produce new viruses upon reactivation. In HIV infected patients, post-integration latency is believed to be the major contributor of the long lived HIV reservoir1. However, in cell cultures with primary infected cells, both forms of latency are prevalent.
In addition to pre- and post-integration latency, episomal dead end HIV DNA may also persist as 1- or 2-LTR circles. These circles are formed when reverse transcribed HIV DNA fails to integrate. It was initially assumed that 1- or 2-LTR circles are not stable and eventually disappear13, but this hypothesis is now under debate as accumulating data indicate that in vitro, this form of episomal HIV DNA appears to be rather stable14. Interestingly, RNA transcription from unintegrated HIV DNA circles has been reported15,16,17,18,19. It has been shown that episomal HIV DNA can lead to the production of HIV proteins and may even generate fully replication competent viruses20,21,22. However, the implications of transcription from 2-LTR circles, especially in the context of HIV latency, have remained underestimated and incompletely understood19,23.
Integrase inhibitors are commonly used in HIV in vitro research. Several latency models include integrase inhibitors treatment to inhibit the step of viral integration before cellular reactivation, assumed to prevent a bias from pre-integration latency. However, this is based on the assumption that unintegrated HIV DNA forms do not contribute to the production of viral transcription and protein production. It is already well known that 2-LTRs accumulate in the presence of INSTI in active infection as well as in treatment intensifications studies in vivo17,20,21,24,25.
The observations of HIV DNA transcription from unintegrated HIV DNA imply that the use of integrase inhibitors may not effectively discern pre- and post-integration latency18,19. To date, this has not been investigated in any of the latency models. Using a recent model of HIV latency, we here show that latency models may indeed be biased by the contribution of pre-integration latency and this bias may lead to an overestimation of latency levels.
Results
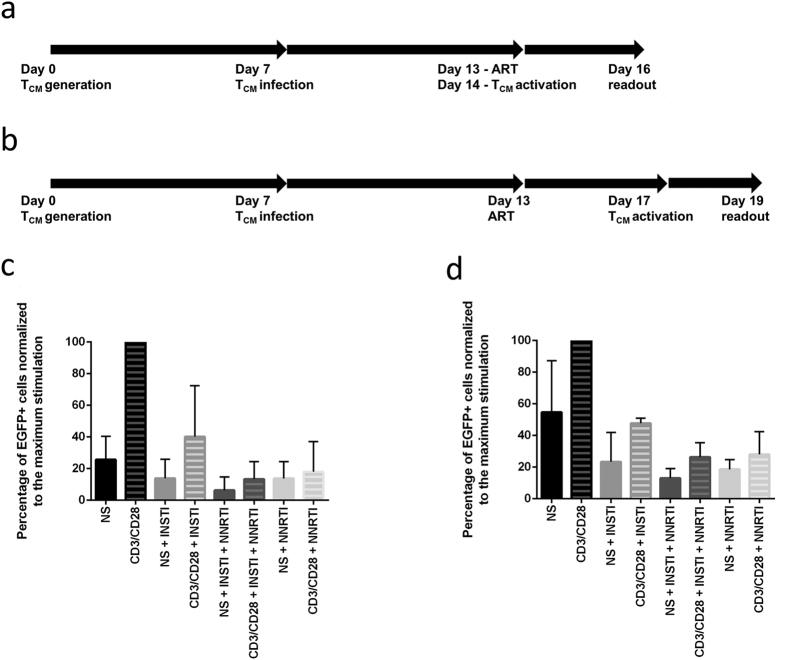
Decreased HIV DNA transcription is observed upon activation in the presence of NNRTIs
We followed two alternative workflows for the generation of HIV latently infected TCM cells, based on the TCM model described earlier6. In this study, we used a modified short protocol (Fig. 1a) and the original described long protocol (Fig. 1b)6. Statistical analysis of the results obtained from the short model performed on cells from seven independent donors (Supplementary Table S1) indicates that the observed difference in EGFP expression between INSTI-treated non-activated and activated cells is significant (p = 0.029). However, the difference between activated and non-activated cells treated with an NNRTI alone (p = 0.33), or INSTI and an NNRTI (p = 0.23) were not significantly different, indicating that the addition of NNRTI removed the effect observed in the condition with INSTI alone. Among the activated cells, the cells treated with INSTI alone expressed EGFP at a significantly higher level compared to activated cells treated with NNRTI alone (p = 0.006) or the combination of INSTI and an NNRTI (p = 0.019). Of note, NNRTIs efavirenz and nevirapine were both used throughout the study, leading to very similar results.
Figure 1.
Schematic representation of the modified short (a) and original long (b) model workflows and corresponding average EGFP expression in the short (c) model depicted in 1a and in the long (d) model depicted in (b). (a and b) legend: TCM–central memory T cells. (c and d) legend: NS–cells not stimulated (full bars). CD3/CD28–cells activated with αCD3/CD28 microbeads (striped bars), INSTI–integrase strand transfer inhibitors treatment. NNRTI–non-nucleoside reverse transcriptase inhibitor treatment. (c) Error bars represent the standard deviation (SD) of 7 replicate experiments performed on cells from 7 independent donors. (d) Error bars represent the standard deviation of 3 replicate experiments performed on cells from 3 independent donors. The data was normalized to maximum stimulation by CD3/CD28 per experiment.
Although the half-life of 2-LTR circles in vitro is an ongoing debate14,22, the time between ART treatment initiation and readout might have an important impact on the outcomes of the model. To show that the observed effects were not due to our modified short latency model, we followed the original long protocol6 in three replicates with independent donor cells. This original model involves a longer period of ART treatment before cellular reactivation (Fig. 1b), possibly decreasing the bias introduced by unstable forms of unintegrated HIV DNA. However, the outcome of this model (Fig. 1d) was similar to the short model as outlined in Fig. 1a and c. It is worth mentioning that the donor cells used for the experiments presented in Fig. 1d were infected at a higher rate than some of the donor cells shown in Fig. 1c. This natural variation between primary cells led to slightly higher EGFP expression across the test conditions in Fig. 1d.
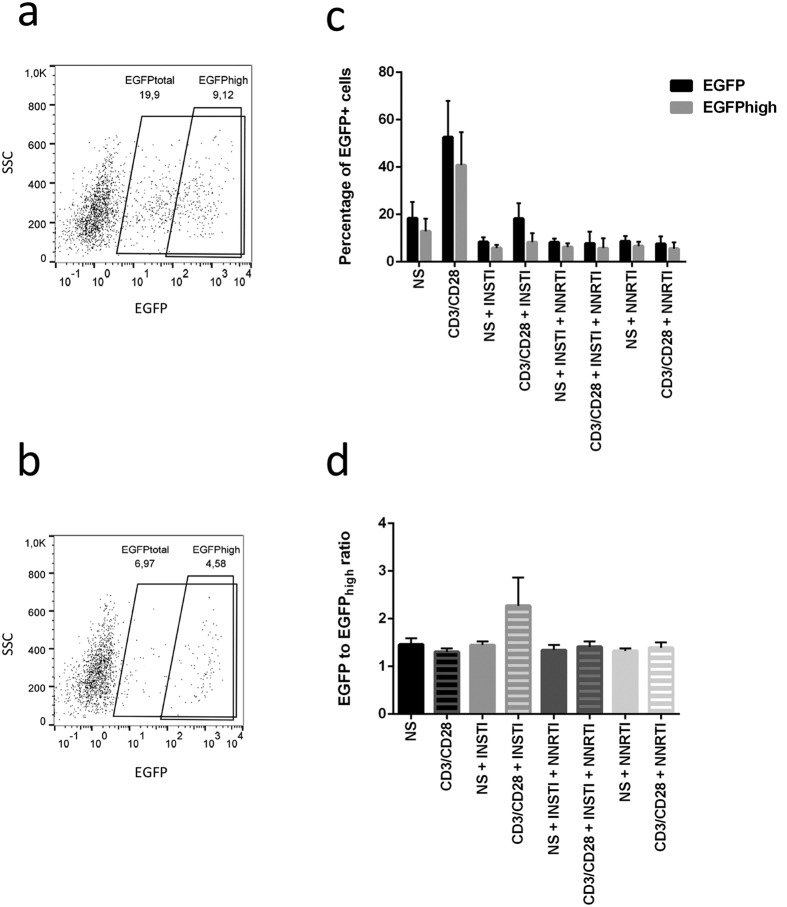
The presence of distinct EGFPhigh and EGFPdim populations in activated T cells
The EGFP + cells appeared as 2 distinct populations (Fig. 2a–c, Supplementary Fig. S2) differing by the intensity of the signal (MFI). This phenomenon was previously observed by Trinité et al. who showed that unintegrated HIV DNA may cause protein production, but at lower levels compared to integrated HIV DNA19. The ratios between total EGFPtotal and EGFPhigh were calculated (Fig. 2d). For samples representing most test conditions of the latency model, the ratio approximates 1.5; however, the cells activated in the presence of INSTI show a higher proportion of EGFPdim with the ratios approximating 2. Kruskal-Wallis test performed on these ratios indicates that the differences in EGFP ratios observed are significant (p = 0.020). Interestingly, treatment with reverse-transcriptase inhibitors decreased the levels of EGFPdim in activated cells, indicating that the blockage of reverse transcription suppressed the generation of EGFPdim cells.
Figure 2. The levels of total EGFP and EGFPhigh in the short latency model.
(a and b) Flow cytometry readout showing distinct EGFP+ fractions, i.e. the total EGFP (larger gate) and EGFPhigh (smaller gate). The percentages indicate cells expressing EGFP. (c and d) legend: NS–cells not stimulated with aCD3/CD28 activator microbeads (full bars). CD3/CD28–cells activated with aCD3/CD28 microbeads (shaded bars). INSTI–integrase strand transfer inhibitors treatment. NNRTI–non-nucleoside reverse transcriptase inhibitor treatment. (a) Cells treated with INSTI and activated with anti-CD3/CD28 show high levels of EGFPdim. (b) Levels of EGFPdim are considerably lower in cells treated with RT inhibitors before activation. (c) Levels of total EGFP (black) and EGFPhigh (grey) across experimental conditions in the model. (d) Ratios between EGFP total and EGFPhigh. Error bars represent the SD of 4 replicate experiments performed on cells from 4 independent donors.
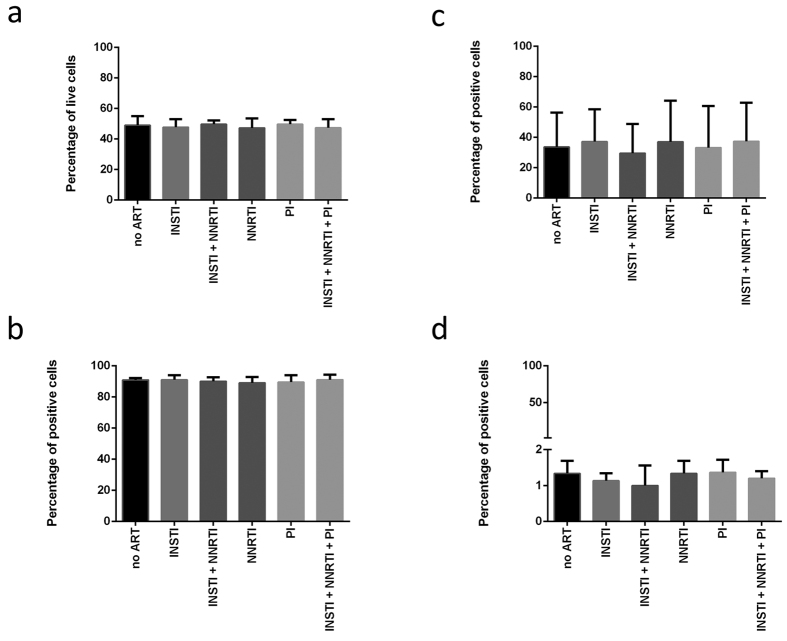
NNRTI treatment largely decreases the levels of 2-LTR circles in activated T cells
To confirm that INSTI treatment induces higher levels of unintegrated HIV DNA, we quantified the levels of episomal 2-LTR circles across the test conditions (Fig. 3). The EGFP expression across the test conditions in the cells from individual donors used for the quantification of 2-LTR circles is represented in Supplementary Fig. S3. The highest levels of 2-LTRs were found in activated cells treated with INSTI, whereas activation in the presence of NNRTIs did not result in high levels of 2-LTRs. This indicates that excess episomal HIV DNA was formed due to the ongoing reverse transcription and the blockage of HIV integration. Interestingly, activation by CD3/CD28 in the presence of NNRTI alone decreased the levels of 2-LTR circles compared to the conditions with INSTI or INSTI and NNRTI, but also compared to the non-activated condition with NNRTI alone (Fig. 3).
Figure 3. Levels of 2-LTR circles across test conditions as quantified by ddPCR.
These levels correspond with the levels of EGFP signal measured by flow cytometry. Error bars represent the standard error of the mean (SEM) of 2 replicate experiments performed on cells from 2 independent donors. Figure legend: NS–cells not stimulated with aCD3/CD28 activator microbeads (full bars). CD3/CD28–cells activated with aCD3/CD28 microbeads (shaded bars). INSTI–integrase strand transfer inhibitors treatment. NNRTI–non-nucleoside reverse transcriptase inhibitor treatment.
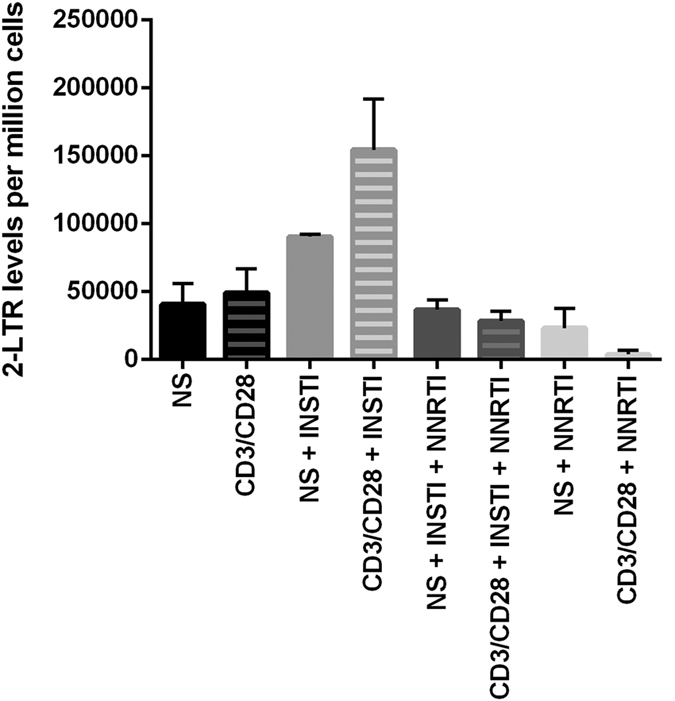
NNRTI treatment does not influence the expression of activation markers or cell viability and has no effect on cellular reactivation
To rule out the possibility that NNRTI treatment alone would affect reactivation, we assessed the cell survival and the expression of activation markers CD69, CD25 and CD38 in cells treated with INSTI, NNRTI and PI (protease inhibitor), alone or in combinations (Fig. 4). To obtain data relevant in the context of the latency model, ART was added to the non-infected cells at day 13 of the workflow and the influence of the drugs on cell viability and activation status was assessed 72 h later. The cell survival as determined by negative propidium iodide staining and expression of activation markers throughout experimental conditions were plotted for three independent donors. We observed different levels of activation and cell viability between donors, but within particular donors the differences between experimental conditions were negligible. Additionally, the same treatment was applied to target cells at day 7 of the workflow and its effect was analysed 72 h later. Similarly, high consistency between experimental conditions was observed (data not shown). This indicates that cell treatment with the tested classes of antiretroviral drugs does not influence their activation status or survival.
Figure 4. Cell viability and expression of activation markers in the short model.
The charts represent cell viability determined by PI staining (a) and the expression of activation markers CD38 (b), CD25 (c) and CD69 (d) across test conditions. The experiment was performed on cells from 3 independent donors. Figure legend: no ART–cells not treated with antiretroviral drugs. INSTI–integrase strand transfer inhibitors treatment. NNRTI–non-nucleoside reverse transcriptase inhibitor treatment. PI–protease inhibitor treatment.
Finally, to ascertain that ART treatment does not interfere with HIV reactivation, we treated latently infected J-Lat 6.3 cells with individual ARTs as well as their combinations before the reactivation was performed. No difference in the levels of EGFP was observed across test conditions at 24 h and 48 h post-activation (Supplementary Fig. S4), indicating that the ART treatment does not have an influence on the cellular reactivation and HIV transcription.
Discussion
The present report shows that expression of viral proteins from unintegrated HIV DNA may bias HIV latency models using integrase inhibitors only. Recent studies of HIV infection have shown that unintegrated HIV DNA may indeed produce viral proteins, but its contribution in HIV latency models has not been assessed so far.
In vitro models of HIV latency can harbour various forms of pre-integration latency which are either in the process of reverse transcription or still present as viral RNA. Experimental reactivation induces the formation of new HIV DNA which can integrate and start producing new viruses. Integrase inhibitors effectively suppress the integration of these new HIV DNA forms, but cannot prevent the production of viral proteins derived from the episomal HIV DNA forms which accumulate due to the blockage of viral integration. Our data are supported by recent reports that also suggest a contribution of unintegrated DNA to viral gene expression in resting CD4+ T cells19,23.
Although protease inhibitors and reverse transcriptase inhibitors are used in the course of some of the latency models described to date, most studies only use INSTI treatment upon reactivation to distinguish between already integrated HIV DNA (post-integration latency) and HIV DNA that would integrate as a result of the activation itself (pre-integration latency). Several primary in vitro models of HIV latency implemented such treatment5,6,7,9,10,12, however, the possible bias introduced by the inclusion of INSTI has been overlooked. Our results show that treatment of HIV-infected T cells with INSTI before cellular reactivation leads to an increase in EGFP signal normally attributed to reversed latency, but NNRTI acting upstream of EGFP production blocks the formation of this signal. This strongly indicates that it is not, at least in part, the reversed latency that contributes to the increase in EGFP upon activation, but that unintegrated HIV DNA which can be formed in the presence of INSTI and is not formed in the presence of NNRTI is an important contributor to the increase in EGFP protein levels. Interestingly, there is little difference in the levels of EGFP expression upon cellular reactivation between the cells treated with NNRTI alone versus NNRTI and INSTI, indicating that it is the newly formed episomal HIV DNA that is the major source of pre-integration latency and bias in this experimental system.
This observation corresponds with an increased proportion of cells expressing moderate levels of EGFP (EGFPdim) formed in the presence of INSTI, a population that is less abundant in the environment with NNRTI. Additionally, the assessment of 2-LTR levels across the test conditions links the increased ratio of EGFP with higher proportions of episomal, HIV 2-LTR circles in the presence of INSTI, further indicating that the EGFP signal does not originate from the reversed post-integration latency. Conversely, the treatment with NNRTI decreases the levels of unintegrated HIV DNA, consistent with the lower levels of EGFP upon activation in these culture conditions. Similar to what we observed in respect to EGFP levels, activation in the presence of NNRTI leads to a lower number of 2-LTR circles compared to treatment with NNRTI/INSTI or INSTI alone.
In conclusion, treatment with NNRTI acts upstream of INSTI and prevents the formation of any HIV DNA from the viral particles that are still present in the system or from viral RNA that is still in the process of reverse transcription to viral DNA. This indicates that in the condition of INSTI treatment alone, most of the 2-LTRs originate from viral particles or incompletely reverse transcribed viral RNA and not from full pre-integration complexes (PIC) as the latter would not be blocked by NNRTIs and would hence also induce an increase in the levels of 2-LTR circles. Our study shows that the addition of NNRTI shortly before reactivation is crucial to minimize the impact of pre-integration latency in this experimental system and we believe that the combination with INSTI gives the most reliable estimation of post-integration latency levels.
Experiments aimed at excluding the influence of ART on the process of cellular reactivation and downstream EGFP production as well as ascertaining that ART treatment does not influence cellular activation status or survival, confirm the notion that these are not off-target effects of antiretroviral drugs used that lead to the observed phenomena, but rather the desired mode of action of these compounds.
It is also worth mentioning that ART treatment is performed shortly before the reactivation and EGFP readout. If the observed effect of EGFP production from episomal HIV DNA was due to the accumulation of unintegrated HIV DNA in the period between the infection and the ART treatment and activation, there would be no differences between experimental conditions. However, these differences occur with the consistently highest EGFP expression originating from cells treated with INSTI, indicating that it is the increased formation of 2-LTR circles stimulated by CD3/CD28 activation in the presence of integrase inhibitors that leads to the increase in the EGFP levels.
The results of this study are mainly based on EGFP expression from the laboratory strain of HIV containing an egfp reading frame upstream of nef. This fact may lead to an overestimation of virus-derived EGFP protein since the expression of Nef protein from 2-LTR circles has already been reported earlier17,26. However, other primary latency models do use the same viral construct harbouring the egfp gene in the reading frame of nef. Hence, considering the build-up of 2-LTR circles in the presence of INSTI only, we would strongly recommend that these conditions should be very carefully tested and the results validated in other latency models to estimate whether, and to what extent these 2-LTR circles bias the read-out.
At this point, the possible contribution of unintegrated HIV DNA to HIV protein production in HIV latency models has been largely overlooked. Our findings emphasize that other HIV latency models should be validated rigorously by monitoring the levels of 2-LTRs and by evaluating the effect of different classes of ART compounds. We therefore urge researchers performing in vitro HIV latency models to include relevant control steps (2-LTR quantification) and conditions (use of NNRTIs) to investigate whether, and to what extent, the contribution of episomal HIV DNA biases the levels of latency in their models.
We would like to emphasize that our findings indicate that the percentage of latently infected cells may be smaller than previously assumed in this and similar latency models. Since these findings may apply for any in vitro HIV-1 latency model employing replication-competent strains of HIV and treatment with INSTI, the latency levels described and processed in downstream applications may be largely overestimated. As a result, findings believed to broaden our understanding of HIV latency may originate from a phenomenon other than in vitro post-integration HIV latency.
Methods
Plasmids and viruses
HIV-1 NLENG1-IRES was a kind gift from Dr. David Levy18. The replication-competent virus stocks were prepared by calcium phosphate transfection of 293 T cells (DZSM, Braunschweig, Germany) according to manufacturer’s instructions (Life Technologies).
Cell isolation and culture
Peripheral blood mononuclear cells (PBMCs) were isolated from the blood of healthy donors following density gradient centrifugation. Donor samples were obtained from Rode Kruis-Vlaanderen, Gent, after informed consent. Blood was diluted in PBS (Lonza, Verviers, Belgium) at 1:1 ratio and 25 ml of diluted blood were slowly added on 12 ml LymphoprepTM (Axis-Shield, Oslo, Norway). This was followed by centrifugation at 770 g for 20 min at RT. Isolated PBMCs were washed twice in PBS and naïve CD4+ T cells were isolated using the Naive CD4+ T Cell Isolation Kit II, human (Miltenyi Biotec, Bergisch Gladbach, Germany) routinely yielding purity exceeding 95% as analysed by flow cytometry (data not shown).
In vitro cultured central memory T cells (TCM) were generated from naïve CD4+ T cells cultured for 3 days in non-polarising conditions, i.e. RPMI supplemented with 1 μg/ml anti-IL-4, 2 μg/ml anti-IL-12, 10 ng/ml TGF-β (Peprotech) and anti-CD3/CD28 microbeads (Invitrogen). After three days, magnetic beads were removed with DynaMag™ Spin Magnet (Life Technologies), cells were collected, counted and resuspended in fresh RPMI with 30 IU/ml IL-2 at 1 million cells in 1 ml of RPMI medium before seeding in 96 well plates. Daily medium change was performed for 4 additional days.
Both naïve CD4 T cells and in vitro cultured central memory T cells were characterized for the expression of CD45RA and CD45RO (Supplementary Fig. S5). The expression of CD45RA and CD45RO was determined by staining with respective antibodies (Miltenyi Biotech). 1 × 105 cells were transferred to a V-bottom 96 well plate and centrifuged for 5 min, 380 g, at room temperature to remove the medium. Next, anti-CD45RO-APC or anti-CD45RA-VioBlue antibody was added to the cells at a concentration of 10 μl/1 ml PBS, mixed and incubated for 30 min at 4 °C. After 30 min of staining, the unbound antibody was washed away and the cells were analysed by flow cytometry using MACSQuant.
The central memory T cells were infected at day 7 post-isolation by spinoculation in 96-well flat bottom plates. The cells were distributed at 2 × 105 cells/well and viral supernatants were added at 2 × 105 cells/well as quantified by the RT assay. After spinoculation for 90 min, 710 g, 32 °C, the supernatant containing HIV was replaced with fresh RPMI. Cells were transferred to U-bottom 96-well plates for further culture.
J-Lat 6.3 cells (Cat. No 9846, obtained through the NIH AIDS Reagent Program, Division of AIDS, NIAID, NIH) were cultured in IMDM medium (Invitrogen) at a density of 5 × 105–106 cells per 1 ml medium27. Medium change was performed twice a week to maintain the desired density of cells. For the experiment investigating the influence of ART treatment on latency reversal, 105 cells were plated in a 96-well plate, treated with the single ART or combinations of drugs and treated with 16 nM PMA for 24 h or 48 h. This was followed by flow cytometric readout.
General latency model workflow
The study followed two alternative workflows to generate latently infected cells.
Briefly, the modified short workflow involves the isolation of naïve CD4+ T cells at day 0, culturing in non-polarising conditions for 72 h, daily medium change for additional 4 days and viral infection at day 7. The cells are treated with antiretroviral drugs at day 13, and activated at day 14. The flow cytometric readout follows at day 1612 (Fig. 1a).
The original long workflow involves the isolation of naïve CD4+ T cells at day 0, culturing in non-polarising conditions for 72 h, daily medium change for additional 4 days and viral infection at day 7 followed by a longer period of antiretroviral treatment, from day 13, cellular activation at day 17 and the readout at day 196 (Fig. 1b).
Antiretroviral treatment and activation
1 day before activation, cells were distributed at 2 × 105 cells per well in 200 μl medium. To differentiate between pre- and post-integration latency, a fraction of the wells was treated with INSTI (integrase strand transfer inhibitor, raltegravir) at 1 μM (Cat. No 11680 from Merck & Company, Inc.), or 2 μM NNRTI (non-nucleoside reverse-transcriptase inhibitor, efavirenz [Cat. No 4624] or nevirapine [Cat. No 4666] obtained through the NIH AIDS Reagent Program, Division of AIDS, NIAID, NIH). For the assessment of the influence of ART on cell toxicity and activation status, cells were treated with PI (protease inhibitor, ritonavir) at 1 μM (Cat. No 4622). Cells were then stimulated with anti-CD3/CD28 microbeads (Dynabeads® Human T-Activator CD3/CD28, Invitrogen) for 48 h before the readout by flow cytometry.
Quantification of infected cells and activation markers
The amount of HIV productive cells was quantified by the EGFP reporter protein produced by the HIV lab strain. Briefly, 1 × 105 cells were transferred to a V-bottom 96 well plate and centrifuged for 5 min, 380 g, at room temperature to remove the medium. Next, 100 μl of PBS was added and the cells were analysed by flow cytometry using MACSQuant (Miltenyi Biotech).
The expression of activation markers was determined by staining of CD25, CD69 and CD38 with respective antibodies (BD Biosciences). 1 × 105 cells were transferred to a V-bottom 96 well plate and centrifuged for 5 min, 380 g, at room temperature to remove the medium. Next, 1 μl of anti-CD25-PE, anti-CD38-PE or anti-CD69-FITC (BD Biosciences) antibody in 100 μl of PBS was added to the cells, mixed and incubated for 30 min at 4 °C. After 30 min of staining, the unbound antibody was washed away and the cells were analysed by flow cytometry using MACSQuant.
Flow cytometric readout was performed to identify the levels of expression of activation markers CD25, CD38, CD69 or EGFP. The cells were routinely stained with propidium iodide to exclude dead cells. By gating out all propidium iodide positive cells, only the live cells were included in the analysis. The results of a longitudinal analysis of the expression of activation markers CD25, CD38 and CD69 are presented in Supplementary Fig. S6.
2-LTR level quantification
Episomal HIV-1 2-LTR circles were quantified from genomic DNA isolated from TCM using ddPCR as previously described28. Episomal DNA was isolated using the QIAprep Spin Miniprep kit (Qiagen). The measurement was performed in duplicate reactions using ddPCR with the QX100™ Droplet Digital™ PCR platform (Bio-Rad, Hercules, California). The ddPCR reaction mix consisted of 2 μl of genomic DNA, 10 μl of 2x ddPCR™ Supermix for probes (Bio-Rad), 500 nM primers (forward primer -5′-CTAACTAGGGAACCCACTGCT-3, reverse primer -5′-GTAGTTCTGCCAATCAGGGAAG-3′) and 250 nM probe (5′-/56-FAM/AGC CTC AAT/ZEN/AAA GCT TGC CTT GAG TGC/3IABkFQ/-3′) in 20 μl final volume. The cycling conditions were as follows: initial denaturation at 95 °C for 5 min, 40 cycles of 95 °C for 30 sec denaturation and elongation 60 sec with a ramp rate of 2.5 °C/sec. Droplets were read by the QX200™ droplet reader (Bio-Rad) and the data was analyzed using a data driven method for threshold determination with the ddpcRquant software in R as previously performed29.
Statistical analysis
Assessment of the statistical significance of the differences in EGFP levels between test conditions was performed using paired t-test (package ‘stats’, version: 3.0.2) and Kruskal–Wallis one-way analysis of variance (package ‘stats’, version: 3.0.2) with RStudio (version 0.99.902).
Additional Information
How to cite this article: Bonczkowski, P. et al. Protein expression from unintegrated HIV-1 DNA introduces bias in primary in vitro post-integration latency models. Sci. Rep. 6, 38329; doi: 10.1038/srep38329 (2016).
Publisher’s note: Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Material
Acknowledgments
Pawel Bonczkowski and Eva Malatinkova are supported by the Agency for Innovation by Science and Technology in Flanders (IWT; Grant number: 111393 & 111286). Ward De Spiegelaere is a post-doctoral fellow at the Research Foundation-Flanders (FWO), Grant number 12G9716N. Linos Vandekerckhove is a Senior Clinical Investigator at the FWO, Grant number 1802014N. Additionally, this work was supported by the King Baudouin Foundation (Grant nr: 2010-R20640-003), HIV-ERA (130442 SBO, EURECA) and HIVERA:EURECA, ERANET 01KI1307A (to Renate Koenig).
Footnotes
Author Contributions P.B., M.A.D.S., W.D.S. and L.V. conceived and designed experiments. P.B., M.A.D.S., E.M. and A.B. performed the experiments. P.B., M.A.D.S., Z.M., R.K., W.D.S. and L.V. analysed the data. Z.M., R.K., W.D.S. and L.V. provided technical expertise throughout the study. P.B., W.D.S. and L.V. wrote the manuscript. All authors read and approved the final manuscript.
References
- Ruelas D. S. & Greene W. C. An Integrated Overview of HIV-1 Latency. Cell 155, 519–529 (2013). [DOI] [PMC free article] [PubMed] [Google Scholar]
- Van Lint C., Bouchat S. & Marcello A. HIV-1 transcription and latency: an update. Retrovirology 10, 67 (2013). [DOI] [PMC free article] [PubMed] [Google Scholar]
- Finzi D. et al. Identification of a reservoir for HIV-1 in patients on highly active antiretroviral therapy. Science 278, 1295–1300 (1997). [DOI] [PubMed] [Google Scholar]
- Eisele E. & Siliciano R. F. Redefining the Viral Reservoirs that Prevent HIV-1 Eradication. Immunity 37, 377–388, doi: 10.1016/j.immuni.2012.08.010 (2012). [DOI] [PMC free article] [PubMed] [Google Scholar]
- Spina C. A. et al. An In-Depth Comparison of Latent HIV-1 Reactivation in Multiple Cell Model Systems and Resting CD4+ T Cells from Aviremic Patients. PLoS pathogens 9, e1003834, doi: 10.1371/journal.ppat.1003834 (2013). [DOI] [PMC free article] [PubMed] [Google Scholar]
- Martins L. J. et al. Modeling HIV-1 Latency in Primary T Cells Using a Replication-Competent Virus. AIDS Research and Human Retroviruses 32, 187–193, doi: 10.1089/aid.2015.0106 (2016). [DOI] [PMC free article] [PubMed] [Google Scholar]
- Evans V. A. et al. Myeloid Dendritic Cells Induce HIV-1 Latency in Non-proliferating CD4+ T Cells. PLoS pathogens 9, e1003799, doi: 10.1371/journal.ppat.1003799 (2013). [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lassen K. G., Hebbeler A. M., Bhattacharyya D., Lobritz M. A. & Greene W. C. A flexible model of HIV-1 latency permitting evaluation of many primary CD4 T-cell reservoirs. PloS one 7, e30176, doi: 10.1371/journal.pone.0030176 (2012). [DOI] [PMC free article] [PubMed] [Google Scholar]
- Saleh S. et al. CCR7 ligands CCL19 and CCL21 increase permissiveness of resting memory CD4(+) T cells to HIV-1 infection: a novel model of HIV-1 latency. Blood 110, 4161–4164, doi: 10.1182/blood-2007-06-097907 (2007). [DOI] [PubMed] [Google Scholar]
- Swiggard W. J. et al. Human immunodeficiency virus type 1 can establish latent infection in resting CD4+ T cells in the absence of activating stimuli. Journal of virology 79, 14179–14188, doi: 10.1128/jvi.79.22.14179-14188.2005 (2005). [DOI] [PMC free article] [PubMed] [Google Scholar]
- Chavez L., Calvanese V. & Verdin E. HIV Latency Is Established Directly and Early in Both Resting and Activated Primary CD4 T Cells. PLoS pathogens 11, e1004955, doi: 10.1371/journal.ppat.1004955 (2015). [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bosque A. & Planelles V. Induction of HIV-1 latency and reactivation in primary memory CD4(+) T cells. Blood 113, 58–65, doi: 10.1182/blood-2008-07-168393 (2009). [DOI] [PMC free article] [PubMed] [Google Scholar]
- Zhu W. et al. Rapid turnover of 2-LTR HIV-1 DNA during early stage of highly active antiretroviral therapy. PloS one 6, e21081, doi: 10.1371/journal.pone.0021081 (2011). [DOI] [PMC free article] [PubMed] [Google Scholar]
- Pace M. J., Graf E. H. & O’Doherty U. HIV 2-Long Terminal Repeat Circular DNA is Stable in Primary CD4+ T Cells. Virology 441, 18–21, doi: 10.1016/j.virol.2013.02.028 (2013). [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wu Y. T. & Marsh J. W. Selective transcription and modulation of resting T cell activity by preintegrated HIV DNA. Science 293, 1503–1506, doi: 10.1126/science.1061548 (2001). [DOI] [PubMed] [Google Scholar]
- Cara A., Cereseto A., Lori F. & Reitz M. S. Jr. HIV-1 protein expression from synthetic circles of DNA mimicking the extrachromosomal forms of viral DNA. The Journal of biological chemistry 271, 5393–5397 (1996). [DOI] [PubMed] [Google Scholar]
- Sloan R. D. & Wainberg M. A. The role of unintegrated DNA in HIV infection. Retrovirology 8, 52, doi: 10.1186/1742-4690-8-52 (2011). [DOI] [PMC free article] [PubMed] [Google Scholar]
- Trinité B. et al. Suppression of Foxo1 Activity and Down-Modulation of CD62L (L-Selectin) in HIV-1 Infected Resting CD4 T Cells. PloS one 9, e110719, doi: 10.1371/journal.pone.0110719 (2014). [DOI] [PMC free article] [PubMed] [Google Scholar]
- Trinité B. et al. An HIV-1 replication pathway utilizing reverse transcription products that fail to integrate. Journal of virology 87, 12701–12720, doi: 10.1128/jvi.01939-13 (2013). [DOI] [PMC free article] [PubMed] [Google Scholar]
- Thierry S. et al. Integrase inhibitor reversal dynamics indicate unintegrated HIV-1 dna initiate de novo integration. Retrovirology 12, 015–0153 (2015). [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hazuda D., Iwamoto M. & Wenning L. Emerging pharmacology: inhibitors of human immunodeficiency virus integration. Annual review of pharmacology and toxicology 49, 377–394, doi: 10.1146/annurev.pharmtox.011008.145553 (2009). [DOI] [PubMed] [Google Scholar]
- Sharkey M. Tracking episomal HIV DNA: implications for viral persistence and eradication of HIV. Current opinion in HIV and AIDS 8, 93–99, doi: 10.1097/COH.0b013e32835d08c2 (2013). [DOI] [PubMed] [Google Scholar]
- Chan C. N. et al. HIV-1 latency and virus production from unintegrated genomes following direct infection of resting CD4 T cells. Retrovirology 13, 1, doi: 10.1186/s12977-015-0234-9 (2016). [DOI] [PMC free article] [PubMed] [Google Scholar]
- Buzon M. J. et al. Long-term antiretroviral treatment initiated in primary HIV-1 infection affects the size, composition and decay kinetics of the reservoir of HIV-1 infected CD4 T cells. Journal of virology 88, 10056–10065, doi: 10.1128/JVI.01046-14 (2014). [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hatano H. et al. Increase in 2-LTR Circles and Decrease in D-dimer After Raltegravir Intensification in Treated HIV-Infected Patients: A Randomized, Placebo-Controlled Trial. Journal of infectious diseases 9, 1436–42, doi: 10.1093/infdis/jit453 (2013). [DOI] [PMC free article] [PubMed] [Google Scholar]
- Sloan R. D., Donahue D. A., Kuhl B. D., Bar-Magen T. & Wainberg M. A. Expression of Nef from unintegrated HIV-1 DNA downregulates cell surface CXCR4 and CCR5 on T-lymphocytes. Retrovirology 7, 44, doi: 10.1186/1742-4690-7-44 (2010). [DOI] [PMC free article] [PubMed] [Google Scholar]
- Jordan A., Bisgrove D. & Verdin E. HIV reproducibly establishes a latent infection after acute infection of T cells in vitro. Embo Journal 22, 1868–1877 (2003). [DOI] [PMC free article] [PubMed] [Google Scholar]
- Malatinkova E. et al. Accurate quantification of episomal HIV-1 two-long terminal repeat circles by use of optimized DNA isolation and droplet digital PCR. Journal of clinical microbiology 53, 699–701, doi: 10.1128/jcm.03087-14 (2015). [DOI] [PMC free article] [PubMed] [Google Scholar]
- Trypsteen W. et al. ddpcRquant: threshold determination for single channel droplet digital PCR experiments. Analytical and bioanalytical chemistry 407, 5827–5834, doi: 10.1007/s00216-015-8773-4 (2015). [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.