Abstract
Background
The use of Nasolabial flap (NLF) to reconstruct orofacial soft tissue defects is one of the oldest methods for reconstruction in the medical literature. Despite widespread use of this invaluable flap, there are still controversies over the terms used for the description of this flap.
Materials and methods
A search was run in PubMed for articles in English language on nasolabial flap in oral cavity/facial reconstruction, between 1960 and 2016. Inclusion criteria was case series that focused on the anatomy, flap design, blood supply, composition, flap motion, and the reconstructed area and donor site complications.
Results
560 articles were found in PubMed search for nasolabial flap (between 1960 and 2016). 84 articles with case series structure and available full text were included. The results of the search in this topic for anatomy, flap design, blood supply,NLF composition, flap motion, reconstructed area and donor site morbidity are presented.
Conclusion
Nasolabial flap is an old flap for reconstructive purposes. Over time different modifications have been introduced to expand its usage. Clear definition of the terms used with this flap is given.
Keywords: Facial reconstruction, Oral cavity reconstruction, Nasolabial flap
Highlights
-
•
Majority of nasolabial flaps have random pattern blood supply.
-
•
Nasolabial flap can have different thicknesses from full thickness cheek to thin dermis and epidermis variants.
-
•
Nasolabial flap for facial reconstruction can transfer in three ways including; advancement, rotation and transposition.
1. Introduction
Replacement of the soft tissue loss after traumatic injuries or surgical excision requires soft tissue flaps. Nasolabial flap (NLF) cover is one of the oldest techniques to replace orofacial soft tissue defects [1]. Sushruta, an Indian surgeon in 600 BC described a soft tissue flap very similar to what we know today as “Nasolabial flap” [2]. The skin reservoir lateral the nasolabial fold can be used for oral cavity or facial reconstructions. NLF and melolabial flap can be used interchangeably but the latter term is used commonly by the dermatologists.
The ease of surgery, probability of carrying out the procedure under local anesthesia in co-morbid patients and inconspicuous scar are the advantages of this flap [3]. Despite widespread use of this invaluable flap, there are still controversies about the terms used for describing this flap and there is not any comprehensive review about nasolabial flap [4]. In this article, all terms related to nasolabial flap are explained with cases from author's personal experience to clarify this topic.
2. Materials and methods
A search was run in PubMed for articles in English language on nasolabial flap in oral cavity/facial reconstruction, between 1960 and 2016. Inclusion criteria was case series that focused on the anatomy, flap design, blood supply, composition, flap motion, and the reconstructed area and donor site complications.
3. Results
560 articles were found in PubMed search for nasolabial flap (between 1960 and 2016). 84 articles with case series structure and available full text were included.
3.1. Anatomy
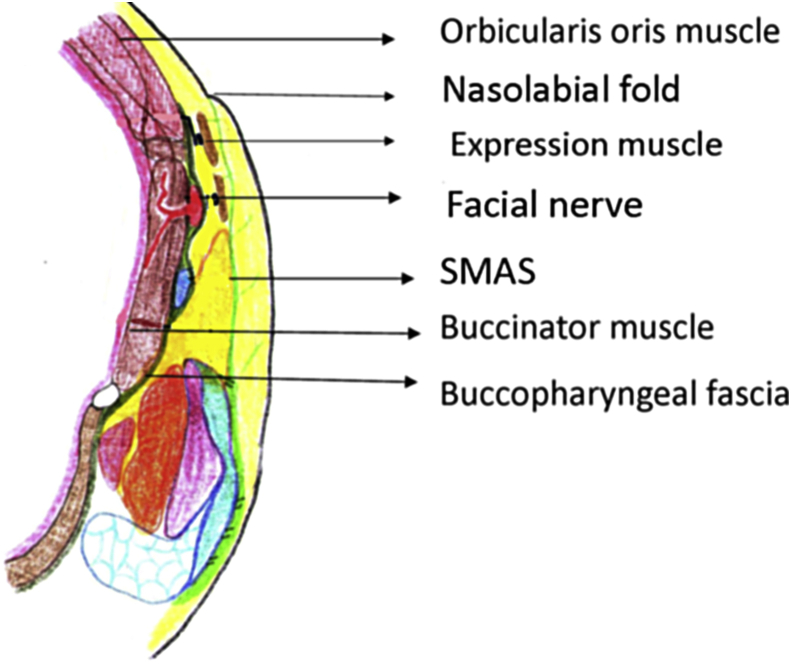
The Anatomy of the nasolabial region is complex. Nasolabial crease run obliquely from approximately 1 Cm superior to the lateral alar rim to approximately 1 Cm lateral to the corner of the mouth. Four expression muscles present in this region including part of levator labi superioris,levator labi superioris alaque nasi,zygomatic major and minor muscles (Tan et al., 2013).Facial artery passes deep to the risorius and zygomatic major muscles but superficial to the buccinator muscle. It also gave off a superficial branch to the zygomaticus major muscle and other small perforating branches to the overlying skin [5]. Extensive subdermal vascular plexus in this region supplies from four arteries; facial, angular, infraorbital and transverse facial [6]. The Buccal and zygomatic branches of the facial nerve innervate the expression muscles of the face from bellow (Fig. 1) [7].
Fig. 1.
Schematic picture: Anatomy of the nasolabial region. Incisions deep to the expression muscles will cut the end branches of the facial nerve without clinical significance.
3.2. Flap design
This flap can be used unilaterally or bilaterally in the form of superiorly, inferiorly or centrally based pedicle flap (Fig. 2) [8]. The terms upper pedicled and cranially based have also been used for description of superiorly based NLF [9], [10].
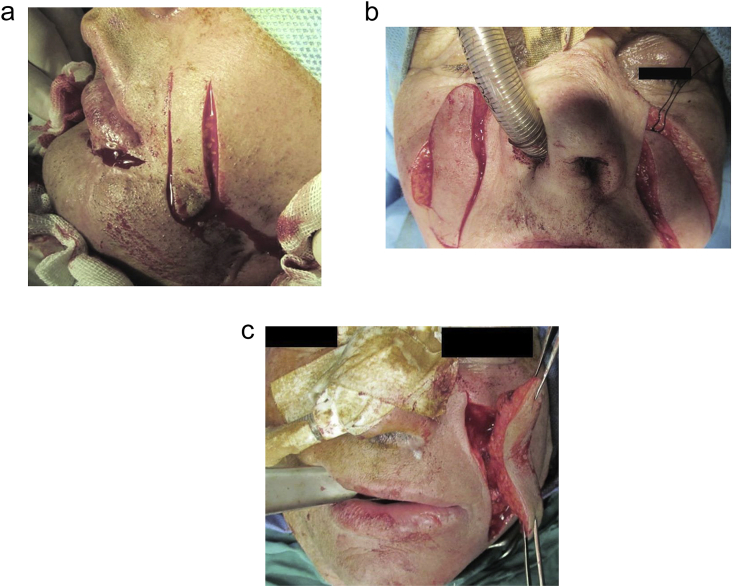
Fig. 2.
Nasolabial flaps based on the location of the pedicle. a, superiorly based. b, Inferiorly based.centrally based.
The flap is commonly designed lateral to the nasolabial fold with the medial limit of the flap 2–3 mm lateral to this fold [11].
In the superiorly based NLF, the base of the flap is near the ala and the apex is in line with the oral commissure [12]. Sometimes when an extra length (10–12 cm) is needed, it can be extended to the skin over the mandibular border. This variant of the superiorly based NLF is called extended NLF (Fig. 3) [13]. In the inferiorly based nasolabial flap the apex of the flap is 5–7 mm lateral to the medial canthus [14].
Fig. 3.

Extended nasolabial flap.
Occasionally NLF is designed medial to the nasolabial fold. This has two indications,first:When the nasolabial flap is used for reconstruction of the upper lip (lateral subunit) and lateral limit of the resected skin falls medial to the nasolabial fold [15] and second: When it is used for nasal floor reconstruction in cleft patients [16].
3.3. Blood supply
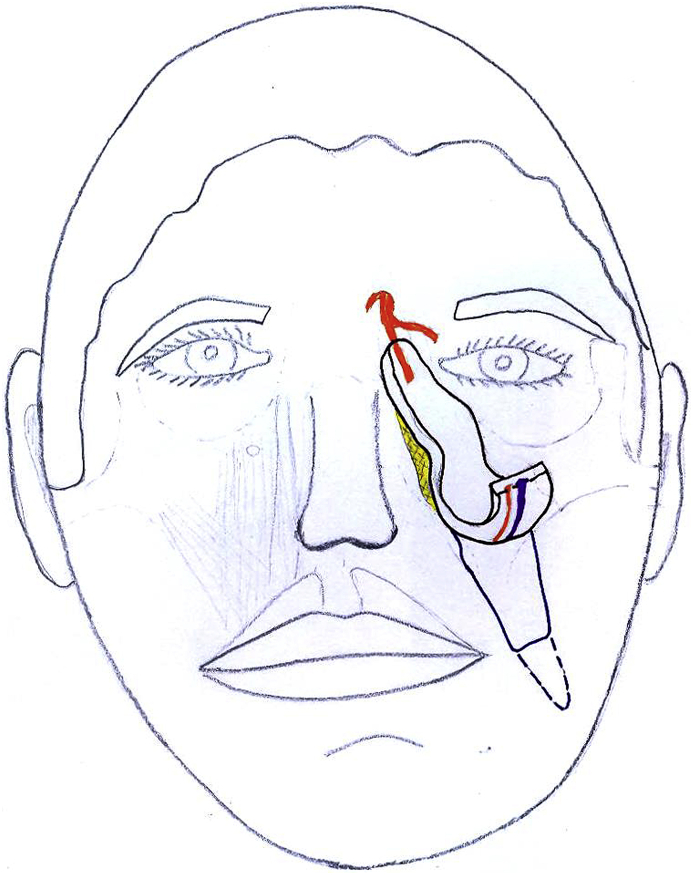
The majority of the NLFs are random pattern [17]. Some NLFs can be designed to have an axial pattern blood supply. These include: Inferiorly based axial nasolabial flap that is nourished by facial artery [18]. Superiorly based reverse flow NLF containing angular artery [19]. The other name for this axial pattern flap is retroangular flap [20]. The orbitonasolabial flap falls in this category (Fig. 4) [21].
Fig. 4.
Schematic picture: Orbitonasolabial flap. It is superiorly based, reverse flow flap based on the angular artery. Boundaries of this flap crosses the skin overlying the nasolabial region up to the medial canthus.
Another arterialized NLF is medially based horizontal NLF that is nourished by the lateral nasal branch of the facial artery [22]. The last axial pattern NLF mentioned in the articles is based on the infraorbital vessels (Fig. 5) [23].This flap is nourished by infraorbital artery that is a branch of maxillary artery and has orthograde blood supply despite its superiorly based pedicle.
Fig. 5.
Axial pattern nasolabial flaps. a, Orthograde flow. b, Reverse flow. c, Based on infraorbital vessels.
The facial artery crosses the face below the expression muscle of the face and above the buccinator muscle [24], so the axial-pattern NLFs are thicker than random-pattern NLFs.The facial artery perforator-based NLF is a versatile flap that has the benefit of axial pattern blood supply through including a perforator branch from the facial artery and is thin because it is not necessary to include the facial artery and the expression muscle in the flap [25].
3.4. Flap composition
Table 1 summarizes the information obtained from the articles in this topic [26], [27], [28], [29], [30].
Table 1.
Different types of the nasolabial flap based on flap composition.
| Type of NLF | Flap composition | Flap thickness |
|---|---|---|
| Buried | Skinless |  |
| Defatted | D + E | |
| Ordinary | D + E + SQ fat | |
| Musculocutanous or Myocutaneous | Skin + Em | |
| Full-thickness | Skin + Em + buccal mucosa |
D: Dermis; E: Epidermis; SQ: Subcutaneous; Em: Expression muscles.
The composite nasolabial flap is the other variant that was not incorporated into the table. This is ordinary NLF that is lined with the skin and is supported by cartilage [31]. Applications for this variant of NLF is exclusively limited to the nasal reconstruction. Nasolabial gate flap is special inferiorly based musculocutaneous transposition NLF that can be used for functional reconstruction of the lower lip [32].
3.5. The flap motion
NLF can be transferred in three directions: Advancement flap: NLF moves in the direction of the long axis of the flap, mainly in cephalic direction. This kind of flap is called nasolabial V-Y advancement flap and is mostly used for infraorbital, medial canthus and lateral nasal reconstruction (Fig. 6) [33]. Rotation flap: The pivot point is the base of the NLF and the lateral limit of the defect coincides with the medial margin of the flap. This flap has a sole indication: reconstruction of the upper lip lateral segment [34], [35]. Transposition flap: This type of NLF is a variant of rotation flaps. NLF is lifted and rotated to reach the defect [30], [36]. If the distance between the nasolabial region and the recipient site is undermined to reach the flap from the donor to the recipient site by this route, this is called tunnelized NLF and if the NLF is passed over the intervening segment of intact skin, then the term interpolated NLF is used [37], [38]. Reconstructed area should fall inside the rotation radius of NLF.
Fig. 6.

Nasolabial V-Y advancement flap.
3.6. Reconstructed area and indications
NLF has been reported for the facial skin reconstruction of the ipsilateral infraorbital, cheek and lower eyelid (advancement flap), upper lip (rotation flap), philtrum (tunnelized flap), commissure, lower lip, and chin (transposition flap) [39], [40], [41], [42], [43], [44].
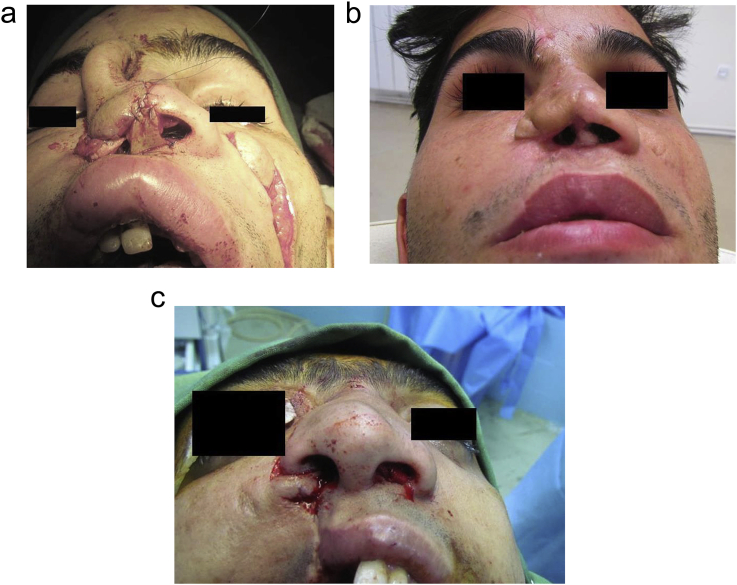
Contralateral NLF could be considered for midline defects when ipsilateral flap is not available for reconstruction [45]. Search of Pubmed for “Nasolabial flap and nasal reconstruction” was half the results of “Nasolabial flap” for all applications. This flap is mainly used in face for the reconstruction of the nose (columella, tip, ala, lateral wall), for skin coverage and as nasal lining for nasal vestibule and septum or in the form of a turn-over flap in combination with the forehead flap (Fig. 7) [46], [47], [48], [49], [50], [51], [52], [53].
Fig. 7.
a, Nasolabial flap for columella reconstruction. b, One year follow up.c,Nasolabial flap for constricted nasal floor reconstruction.
Nasolabial flap perse can be used for nasal lining, and skin coverage when the defect involves the alar rim. Especially named superiorly based NLFs are used exclusively in nasal reconstruction. These flaps included, folded NLF or bipaddled variant that is used for full-thickness alar defect reconstruction, when the alar rim is intact [54], [55]. Bifid NLF is vertically split nasolabial flap that uses in nasal reconstruction when nasal tip and columella are designed to be reconstructed with the same NLF [56]. Spear twisted NLF is medially based nasolabial turn over flap for lining with a distal extension providing the cover with 90° twist of the NLF in between these two parts for full thickness alar defects involving the loss of the lateral alar grove.
For small to moderate intraoral lesions, it is used for buccal, palatal, floor of the mouth, tongue, and maxillary/mandibular alveolar region [57], [58], [59], [60], [61].
3.7. Donor site complications
Donor site often is closed with direct closure. The width of the flap is determined by the laxity of the tissues in the nasolabial region so it is more useful flap in the elderly patients.
The superiorly based flaps can be longer with extension of the apex of the flap to mandibular inferior border, while inferiorly based NLFs are more limited in length [62], [63].
Hypertrophic scars in susceptible individuals and wound dehiscence are two possible complications, when donor site is closed under tension [64].
Subcutaneous plane undermining in the cheek and M plasty are two suggested techniques for reducing the tension during donor site closure [65]. If the simple closure of the donor site is impossible, a cheek rotation flap is mandatory for donor site management. Whenever NLF is used for intraoral reconstruction, the risk of the orocutaneous fistula and iatrogenic dermoid (inclusion) cyst should be considered.
4. Discussion
Clinicians should know that the majority of the nasolabial flaps have random-pattern blood supply. Despite this fact, NLF is highly versatile because blood vessels in subdermal layer travel in axial direction, so the length/width ratio can reach near that of the true axial-pattern flaps [66]. This is true that it is not necessary to include facial artery in flap design for flap survival but facial artery preservation at the same side with nasolabial flap will increase the flap reliability.
Axial-pattern nasolabial flaps are thick flaps. They are more reliable and have more pedicle length [67]. They can be orthograde or reverse flow based on the facial and angular artery, respectively. In cases that facial artery is ligated, these flaps are not indicated but infraorbital-based nasolabial flap that is nourished by infraorbital artery (a branch of the maxillary artery) can be used.
Nasolabial flaps can have different thickness based on the reconstructive requirements. It can be thinned at the level of the dermis and epidermis when a thin pliable flap is needed for alar reconstruction or as thick as possible (full-thickness NLF) when it is used for reconstruction of through-and-through lip defects.
For facial skin replacement, NLF can be used in the form of the advancement, rotation or transposition flaps while for oral cavity reconstruction; only available form is the transposition flap.
The skin island variant of the NLF for facial reconstruction is mandatory when advancement or tunnelized NLFs are used for facial skin reconstruction [68]. This strategy in the advancement or V-Y NLF is necessary to allow movement in the direction of the flap long axis and in the tunnelized variant to avoid the second stage surgery for pedicle division.
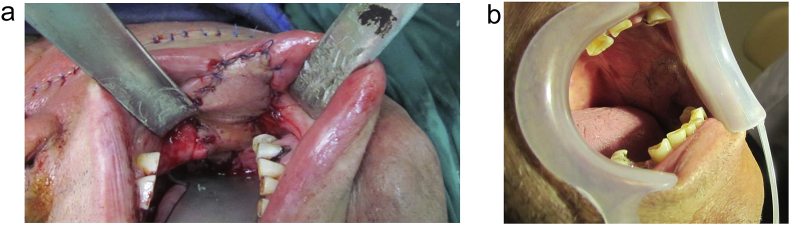
The skin island nasolabial flap or other synonym term “subcutaneous pedicled NLF” is the only variant of the NLF available for intraoral reconstruction. 1–1.5 Cm de-epithelialization of the skin flap near the base is necessary to prevent iatrogenic dermoid cyst formation when this flap is passed through the trans-buccal tunnel to reach the oral cavity (Fig. 8) [69]. The rate of implantation dermoid cysts with this flap is low and is limited to case reports. We have an experience with this unusual complication that occurred three years after usage of tunnelized NLF for philtrum reconstruction in a cleft patient.
Fig. 8.
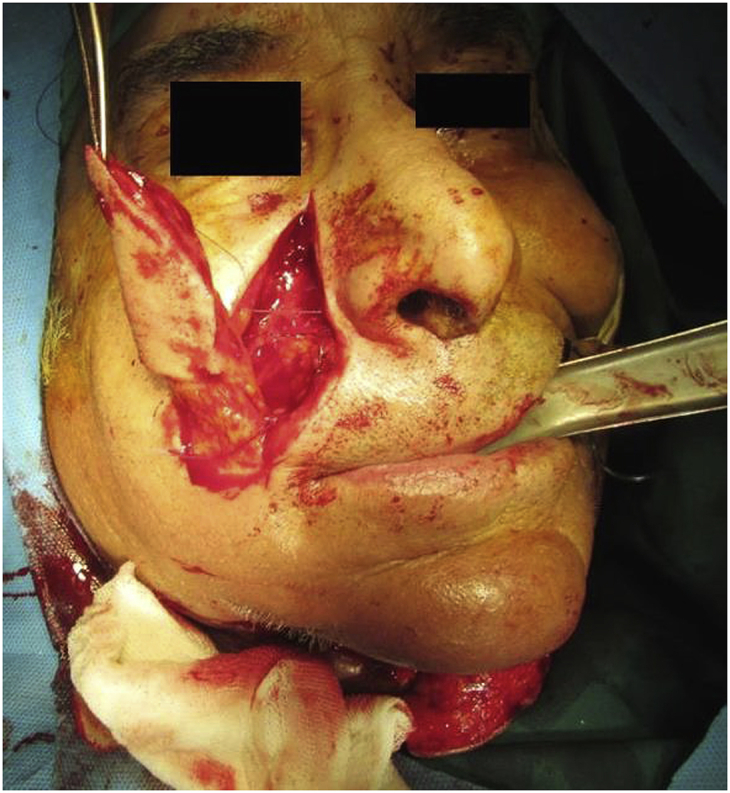
Nasolabial skin island flap. Deepithelialized part of the flap near the pedicle is necessary for transfer of the flap through transbuccal tunnel.
It is important that the readers distinguish the vascular island NLF from the nasolabial island flap. The former is axial-pattern NLF that contains a named artery in the pedicle while the latter is a skin flap that is islanded to the subcutaneous pedicle [70], [71]. Dermal pedicled NLF is more appropriate description for thin defatted NLFs [72].
The patient's dentition is an important factor for selecting the nasolabial flap for intraoral reconstruction. For soft tissue structures inside the dental arch such as the palate, tongue, and mouth floor, the presence of the teeth blocks the NLF to reach these regions and even in edentulous patients need to the second stage surgery for pedicle division.
Today for reconstruction of the tongue and palate, even in edentulous patients, there are better options other than the NLF. In the best conditions it replaces the lost mucosa with the skin and if used for mucosal reconstruction inside the edentulous arches, then a second surgery for vestibuloplasty and pedicle division is needed if the patient desires to wear dentures.
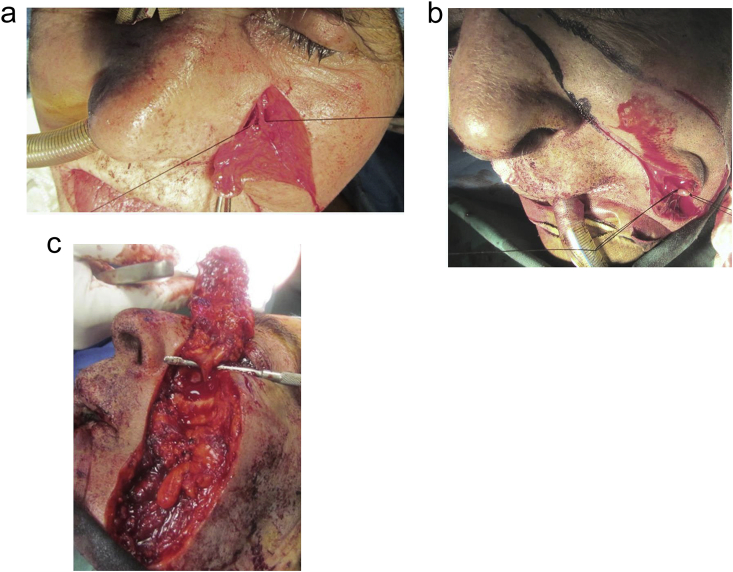
The nasolabial flap has been used for small to moderate sized intraoral defects. However, bilateral NLFs for soft tissue reconstruction of large mandibular anterior region (up to 5 × 5 cm) in edentulous patients is encouraged (Fig. 9) [73].
Fig. 9.
Bilateral nasolabial flap is used for reconstruction of the mandibular alveolar ridge and anterior floor of the mouth after squamous cell carcinoma resection.
Bilateral NLFs produce less asymmetry in the face while slight iatrogenic nasolabial asymmetry is seen in patients receiving unilateral NLF for intraoral reconstruction.
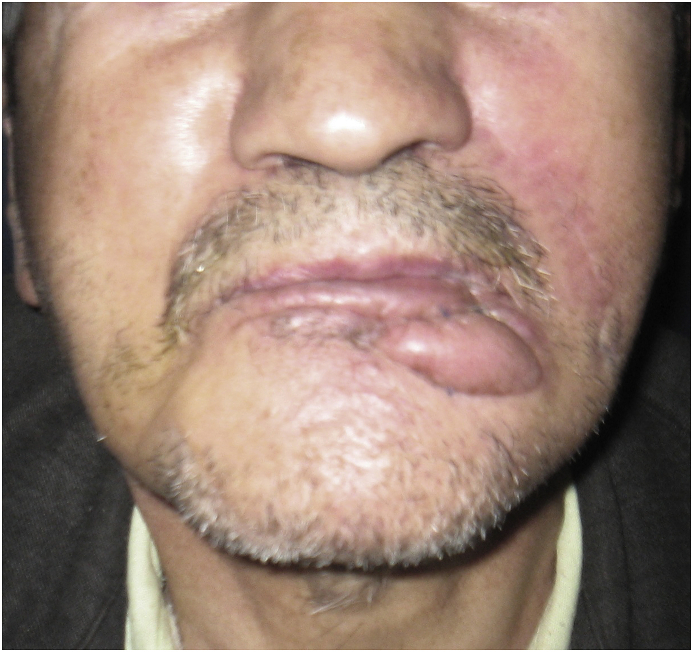
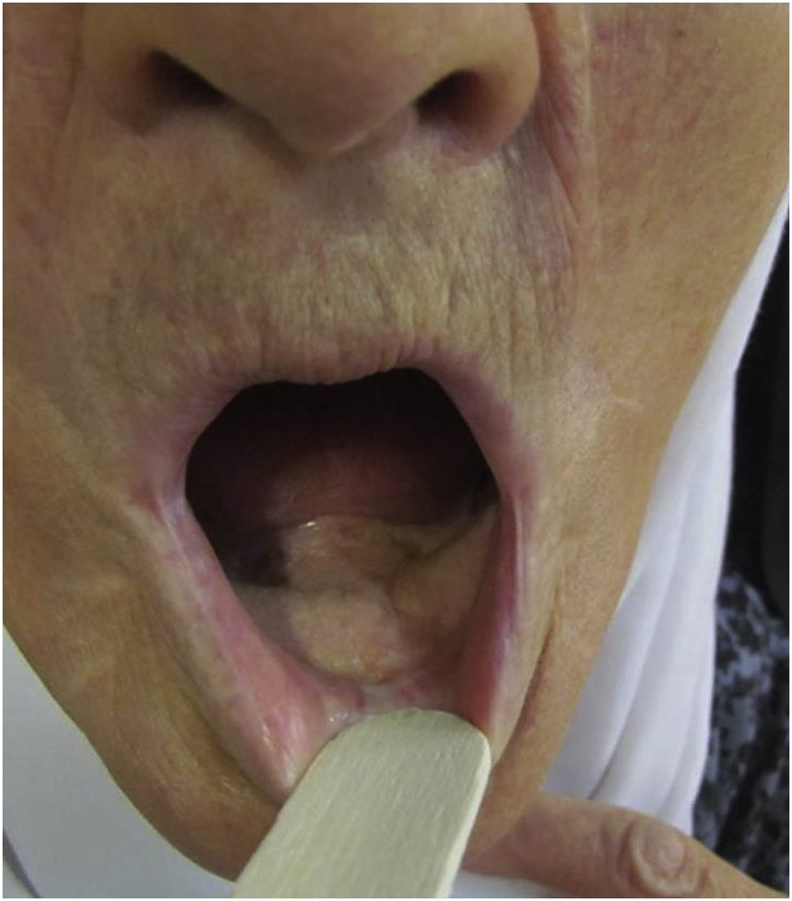
Buccal mucosal reconstruction with NLF in one stage is possible, both in edentulous and dentate patients (Fig. 10). This flap has become popular in the treatment of limitations in mouth opening of patients with oral submucosal fibrosis with vertical mucosal bands in the cheek concomitant with coronoidectomy [74], [75], [76], [77].
Fig. 10.
a, Buccal mucosal reconstruction by nasolabial flap. b, Problem of hairs in intraoral reconstruction in a male patient.
If the rules present in the anatomic section of this article are strictly adhered, the donor site complications will low.
Eliminating nasolabial fold is common if this fold is incorporated into the flap. Periosteal suspension sutures and minimal eversion of the skin during closure of donor site is advised to prevent flat cheek formation [78]. In the medial canthal region, if the distance between the apex of the flap and medial canthus is not followed, medial lower eyelid ectropion is the result. Nasolabial rhomboid flap is a NLF with rhomboid design to prevent dog ear formation during closure of donor site.
Delay procedure is a strategy to increase flap survival, that mostly is used with deltopectoral flap but can be applied with the NLF for reducing complications related to the flap blood supply [79]. This variant is suggested when reutilizing NLF or its blood supply is compromised such as in deep burned face or when extra-long NLF is needed [80].
There is a false concept in NLF: The musculomucosal nasolabial island flap is a misnomer and should not be applied for myomucosal flap in buccal region.NLF contains skin and a better term for this flap is FAMM (facial artery myomucosal) flap [81], [82].
Reverse vascular or reverse blood flow NLF are acceptable terms but reverse NLF that means thin, turn over superiorly based NLF with random pattern blood supply is not suitable.
Composite NLF means prelaminated flap with skin graft and cartilage. Applying this term to the any NLF containing expression muscles or buccal mucosa is not justified.
Inherent limitations of NLF other than limited size of the flap pedicle are:
The problem of the hair in intraoral reconstruction with NLF is seen in extended NLF in male patients [83].
Trapdoor effect in the NLF is possible complication of this flap when it is used for facial skin reconstruction. It is an elevated and bulging deformity of tissue within the semicircular confines of a U-, C-, or V-shaped scar. This can occur in both superiorly or inferiorly based NLFs (Fig. 11). The trapdoor deformity may be prevented or minimized by peripheral undermining about the recipient site of the flap equal to or greater in area than the recipient site [84]. Management of this deformity is via multiple z-plasty.
Fig. 11.
Trapdoor (pincushioning) effect in the inferiorly based nasolabial flap used for lower lip reconstruction.
Limitation of this review is that all articles with nasolabial flap used for orofacial reconstruction are not included but comprehensive review of this flap with limited number of references is done. However this study is not a meta-Analysis or systematic review.
5. Conclusion
Nasolabial flap is an old flap for reconstructive purposes. Over time, different modifications have been introduced to expand its usage. The clear definitions of the terms that used with this flap are presented.
Ethical approval
None.
Sources of funding
This study was supported by a grant from the Vice Chancellor of Research of Mashhad University of Medical Sciences.
Author contribution
Study design:Rahpeyma.
Data collections:khajehahmadi.
Data analysis:
Writing: Rahpeyma.
Conflicts of interest
There are no interests.
Guarantor
This study was supported by a grant from the Vice Chancellor of Research of Mashhad University of Medical Sciences.
Consent
Written patient consent has been obtained to publish clinical photographs.
Registration of research studies
Research registry 1339.
Contributor Information
Amin Rahpeyma, Email: rahpeymaa@mums.ac.ir.
Saeedeh Khajehahmadi, Email: khajehahmadis@mums.ac.ir.
References
- 1.Gewirtz H.S., Eilber F.R., Zarem H.A. Use of the nasolabial flap for reconstruction of the floor of the mouth. Am. J. Surg. 1978;136:508–511. doi: 10.1016/0002-9610(78)90271-4. [DOI] [PubMed] [Google Scholar]
- 2.Ellabban M.A., Van Niekerk W.J., Shoaib T. Sutures to mark the exact site of division of the two-stage nasolabial flap for floor-of-mouth reconstruction. J. Plast. Reconstr. Aesthet. Surg. JPRAS. 2008;61:217–218. doi: 10.1016/j.bjps.2007.09.025. [DOI] [PubMed] [Google Scholar]
- 3.Navarro Cuellar C., Caicoya S.J., Acero Sanz J.J., Navarro Cuellar I., Muela C.M., Navarro Vila C. Mandibular reconstruction with iliac crest free flap, nasolabial flap, and osseointegrated implants. J. Oral Maxillofac. Surg. Off. J. Am. Assoc. Oral Maxillofac. Surg. 2014;72 doi: 10.1016/j.joms.2014.02.031. 1226.e1-15. [DOI] [PubMed] [Google Scholar]
- 4.Matsuda H., Takahashi Y., Ichinose A., Miyazaki H., Kakizaki H. Combination of nasolabial v-y advancement flap and glabellar subcutaneous pedicled flap for reconstruction of medial canthal defect. Case Rep. Ophthalmol. 2014;5:50–53. doi: 10.1159/000360130. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Pinar Y.A., Bilge O., Govsa F. Anatomic study of the blood supply of perioral region. Clin. Anat. (New York, NY) 2005;18:330–339. doi: 10.1002/ca.20108. [DOI] [PubMed] [Google Scholar]
- 6.Whetzel T.P., Mathes S.J. Arterial anatomy of the face: an analysis of vascular territories and perforating cutaneous vessels. Plast. Reconstr. Surg. 1992;89:591–603. discussion 4–5. [PubMed] [Google Scholar]
- 7.Hwang K. Surgical anatomy of the facial nerve relating to facial rejuvenation surgery. J. Craniofacial Surg. 2014;25:1476–1481. doi: 10.1097/SCS.0000000000000577. [DOI] [PubMed] [Google Scholar]
- 8.Weathers W.M., Wolfswinkel E.M., Nguyen H., Thornton J.F. Expanded uses for the nasolabial flap. Semin. Plast. Surg. 2013;27:104–109. doi: 10.1055/s-0033-1351234. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Thiery G., Coulet O., Guyot L. Reconstruction of a transfixing partial loss of substance from the wing of nose with the upper pedicled nasolabial flap. Rev. Laryngol. Otol. Rhinol. 2008;129:49–51. [PubMed] [Google Scholar]
- 10.Kerem H., Bali U., Sonmez E., Manavbasi Y.I., Yoleri L. The cranially based contralateral nasolabial flap for reconstruction of paranasal and periorbital surgical defects. J. Plast. Reconstr. Aesthet. Surg. JPRAS. 2014;67:655–661. doi: 10.1016/j.bjps.2014.01.027. [DOI] [PubMed] [Google Scholar]
- 11.Bi H., Xing X., Li J. Nasolabial-alar crease: a natural line to facilitate transposition of the nasolabial flap for lower nasal reconstruction. Ann. Plastic Surg. 2014;73:520–524. doi: 10.1097/SAP.0b013e31827f547e. [DOI] [PubMed] [Google Scholar]
- 12.Field L.M. Design concepts for the nasolabial flap. Plast. Reconstr. Surg. 1983;71:283–285. doi: 10.1097/00006534-198302000-00044. [DOI] [PubMed] [Google Scholar]
- 13.Borle R.M., Nimonkar P.V., Rajan R. Extended nasolabial flaps in the management of oral submucous fibrosis. Br. J. oral Maxillofac. Surg. 2009;47:382–385. doi: 10.1016/j.bjoms.2008.08.019. [DOI] [PubMed] [Google Scholar]
- 14.Ducic Y., Burye M. Nasolabial flap reconstruction of oral cavity defects: a report of 18 cases. J. Oral Maxillofac. Surg. Off. J. Am. Assoc. Oral Maxillofac. Surg. 2000;58:1104–1108. doi: 10.1053/joms.2000.9564. discussion 8–9. [DOI] [PubMed] [Google Scholar]
- 15.Bento M., Carmo L., Trigo M., Rebelo N., Garcia P. The island nasolabial flap in philtrum reconstruction after bite avulsion: a case report. J. Plast. Reconstr. Aesthet. Surg. JPRAS. 2009;62 doi: 10.1016/j.bjps.2008.08.069. e487–9. [DOI] [PubMed] [Google Scholar]
- 16.Rahpeyma A., Khajehahmadi S. The last resort for reconstruction of nasal floor in difficult-to-repair alveolar cleft cases: a retrospective study. J. Cranio Maxillo Facial Surg. off. Publ. Eur. Assoc. Cranio Maxillo-Facial Surg. 2014;42:995–999. doi: 10.1016/j.jcms.2014.01.022. [DOI] [PubMed] [Google Scholar]
- 17.Hynes B., Boyd J.B. The nasolabial flap. Axial or random? Arch. Otolaryngol. Head Neck Surg. 1988;114:1389–1391. doi: 10.1001/archotol.1988.01860240039019. [DOI] [PubMed] [Google Scholar]
- 18.Rose E.H. One-stage arterialized nasolabial island flap for floor of mouth reconstruction. Ann. Plastic Surg. 1981;6:71–75. doi: 10.1097/00000637-198101000-00012. [DOI] [PubMed] [Google Scholar]
- 19.Le-Quang C. Reversed vascular full-thickness nasolabial flap. Ann. de Chir. Plast. Esthet. 1994;38:273–278. [PubMed] [Google Scholar]
- 20.Iida N., Ohsumi N., Tsutsumi Y., Tonegawa M. The full-thickness retroangular flap. Ann. Plastic Surg. 2000;45:544–549. doi: 10.1097/00000637-200045050-00015. [DOI] [PubMed] [Google Scholar]
- 21.Dagregorio G., Baraer F., Darsonval V. Seven reconstructions of the orbital and periorbital region with a contralateral orbitonasolabial flap. Br. J. Plast. Surg. 2005;58:940–943. doi: 10.1016/j.bjps.2005.04.020. [DOI] [PubMed] [Google Scholar]
- 22.Pincus R.L., Bukachevsky R.P. Medially based horizontal nasolabial flaps for reconstruction of columellar defects. Arch. Otolaryngol. Head Neck Surg. 1990;116:973–974. doi: 10.1001/archotol.1990.01870080095025. [DOI] [PubMed] [Google Scholar]
- 23.He B., Song J., Fan X. Clinical application of nasolabial subcutaneous pedicle skin flap with infraorbital artery. Zhonghua zheng xing shao shang wai ke za zhi = Zhonghua zheng xing shao shang waikf [ie waike] zazhi = Chin. J. plastic Surg. burns/[Chung-hua cheng hsing shao shang wai k'o tsa chih pien. 1994;10:423–425. [PubMed] [Google Scholar]
- 24.Funt D., Pavicic T. Dermal fillers in aesthetics: an overview of adverse events and treatment approaches. Clin. Cosmet. Investig. Dermatol. 2013;6:295–316. doi: 10.2147/CCID.S50546. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Yoon T.H., Yun I.S., Rha D.K., Lee W.J. Reconstruction of various perinasal defects using facial artery perforator-based nasolabial island flaps. Arch. Plast. Surg. 2013;40:754–760. doi: 10.5999/aps.2013.40.6.754. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Steenfos H., Tarnow P., Blomqvist G. Experience with the modified defatted nasolabial transposition flap in nasal reconstruction. Scand. J. Plast. Reconstr. Surg. Hand Surg./Nordisk plastikkirurgisk forening Nordisk klubb handkirurgi. 1995;29:51–52. doi: 10.3109/02844319509048423. [DOI] [PubMed] [Google Scholar]
- 27.Campus G., Standoli N., Alfano C. Reconstruction of the lower lip with a full thickness nasolabial island flap. Scand. J. Plast. Reconstr. Surg. Hand Surg./Nordisk plastikkirurgisk forening Nordisk klubb handkirurgi. 1994;28:285–288. doi: 10.3109/02844319409022013. [DOI] [PubMed] [Google Scholar]
- 28.Hagan W.E. Nasolabial musculocutaneous flap in reconstruction of oral defects. Laryngoscope. 1986;96:840–845. doi: 10.1002/lary.1986.96.8.840. [DOI] [PubMed] [Google Scholar]
- 29.Vecchione T.R. Use of a buried nasolabial flap to fill a depression over the lower jaw. Case report. Plast. Reconstr. Surg. 1976;58:375–376. doi: 10.1097/00006534-197609000-00029. [DOI] [PubMed] [Google Scholar]
- 30.Soh K.B., Soo K.C. Reconstruction of moderate sized intra-oral defects using the nasolabial flap. Ann. Acad. Med. Singapore. 1994;23:891–895. [PubMed] [Google Scholar]
- 31.Goldman G.D., Kakinuma A composite nasolabial flap for an entire ala reconstruction. Dermatol. Surg. 2002;28:870–871. doi: 10.1046/j.1524-4725.2002.02046.x. official publication for American Society for Dermatologic Surgery [et al] [DOI] [PubMed] [Google Scholar]
- 32.Fujimori R. Gate flap“ for the total reconstruction of the lower lip. Bri. J. Plast. Surg. 1980;33:340–345. doi: 10.1016/s0007-1226(80)90079-x. [DOI] [PubMed] [Google Scholar]
- 33.Ayeni O., Ayeni O., Carey W., Muhn C. Combined advancement and single-lobed nasolabial transposition flaps for a nasal sidewall defect. Dermatol. Surg. 2012;38:1386–1389. doi: 10.1111/j.1524-4725.2012.02426.x. official publication for American Society for Dermatologic Surgery [et al] [DOI] [PubMed] [Google Scholar]
- 34.Simons G., Greco J.M., Darsonval V. The naso-cheek or nasolabial rotation flap with subcutaneous pedicle in the repair of tissue loss above the lip. Ann. de Chir. Plast. Esthet. 1984;29:74–77. [PubMed] [Google Scholar]
- 35.Rahpeyma A., Khajehahmadi S. Unilateral one stage nasolabial flap for reconstruction of the lips. J. Maxillofac. Oral Surg. 2015;14:234–239. doi: 10.1007/s12663-013-0615-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Barlow J.O. The bifurcated nasolabial transposition flap. Dermatol. Surg. 2011;37:695–699. doi: 10.1111/j.1524-4725.2011.01948.x. official publication for American Society for Dermatologic Surgery [et al] [DOI] [PubMed] [Google Scholar]
- 37.Georgiade N.G., Mladick R.A., Thorne F.L. The nasolabial tunnel flap. Plast. Reconstr. Surg. 1969;43:463–466. doi: 10.1097/00006534-196905000-00002. [DOI] [PubMed] [Google Scholar]
- 38.Pharis D.B., Papadopoulos D.J. Superiorly based nasolabial interpolation flap for repair of complex nasal tip defects. Dermatol. Surg. 2000;26:19–24. doi: 10.1046/j.1524-4725.2000.99057.x. official publication for American Society for Dermatologic Surgery [et al] [DOI] [PubMed] [Google Scholar]
- 39.Yeo J.F., Egyedi P. Reconstruction of soft tissues of the chin and lower lip region following excision of a basal cell carcinoma. J. Cranio Maxillo Facial Surg. Off. Publ. Eur. Assoc. Cranio Maxillo Facial Surg. 1988;16:337–339. doi: 10.1016/s1010-5182(88)80074-x. [DOI] [PubMed] [Google Scholar]
- 40.Yildirim S., Akoz T., Akan M., Cakir B. The use of combined nasolabial V-Y advancement and glabellar flaps for large medial canthal defects. Dermatol. Surg. 2001;27:215–218. doi: 10.1046/j.1524-4725.2001.00301.x. official publication for American Society for Dermatologic Surgery [et al] [DOI] [PubMed] [Google Scholar]
- 41.Shipkov C.D., Anastassov Y.K., Simov R.I. Unilateral superiorly-based nasolabial island flap for the reconstruction of the philtrum. Scand. J. Plast. Reconstr. Surg. Hand Surg./Nordisk plastikkirurgisk forening [and] Nordisk klubb for handkirurgi. 2002;36:177–179. doi: 10.1080/028443102753718078. [DOI] [PubMed] [Google Scholar]
- 42.Aslan A., Ozkan A.C., Aydin H., Koldas T., Tuncer S. Orocutaneous fistula arising secondary to irritation of an external dental prosthesis and its reconstruction using a nasolabial island flap. Ann. Plast. Surg. 2001;47:95–96. doi: 10.1097/00000637-200107000-00022. [DOI] [PubMed] [Google Scholar]
- 43.Vannieuwenhuyse J.B., Duflos M. Nasolabial flaps for repair of defects on the upper lip and lateral aspects of the nose. J. Dermatol. Surg. oncol. 1982;8:351–355. doi: 10.1111/j.1524-4725.1982.tb00299.x. [DOI] [PubMed] [Google Scholar]
- 44.Walker A.W., Schewe J.E., Jr. Nasolabial flap reconstruction for carcinoma of the lower lip. An eleven year follow-up study. Am. J. Surg. 1967;113:783–786. doi: 10.1016/0002-9610(67)90347-9. [DOI] [PubMed] [Google Scholar]
- 45.Ponte P., Goulao J., de Almeida J.R. Contralateral nasolabial flap for a large nasal defect. Dermatol. Surg. 2009;35:675–678. doi: 10.1111/j.1524-4725.2009.01119.x. official publication for American Society for Dermatologic Surgery [et al] [DOI] [PubMed] [Google Scholar]
- 46.Santos O.A., Pappas J.C. Repair of nostril defect with a contralateral nasolabial flap. Plast. Reconstr. Surg. 1976;57:704–706. doi: 10.1097/00006534-197606000-00004. [DOI] [PubMed] [Google Scholar]
- 47.Wesser D.R., Burt G.B., Jr. Nasolabial flap for losses of the nasal ala and columella. Case report. Plast. Reconstr. Surg. 1969;44:300–302. doi: 10.1097/00006534-196909000-00021. [DOI] [PubMed] [Google Scholar]
- 48.Kroll S.S. Nasal alar reconstruction using the nasolabial turnover flap. Laryngoscope. 1991;101:1127–1131. doi: 10.1288/00005537-199110000-00016. [DOI] [PubMed] [Google Scholar]
- 49.Uchinuma E., Matsui K., Shimakura Y., Murashita K., Shioya N. Evaluation of the median forehead flap and the nasolabial flap in nasal reconstruction. Aesthet. Plast. Surg. 1997;21:86–89. doi: 10.1007/s002669900089. [DOI] [PubMed] [Google Scholar]
- 50.Edgerton M.T., Marsh J.L. Uses of the nasolabial flap in the correction of cleft lip nasal deformities. Plast. Reconstr. Surg. 1977;60:56–67. doi: 10.1097/00006534-197707000-00008. [DOI] [PubMed] [Google Scholar]
- 51.Burnam J.A. The nasolabial flap in reconstruction of the nose. J. Fla. Med. Assoc. 1972;59:32–34. [PubMed] [Google Scholar]
- 52.McLaren L.R. Nasolabial flap repair for alar margin defects. Br. J. Plast. Surg. 1963;16:234–238. doi: 10.1016/s0007-1226(63)80115-0. [DOI] [PubMed] [Google Scholar]
- 53.Haas E. Reconstruction of the ala nasi and the lateral wall of the nose. Rhinology. 1976;14:83–90. [PubMed] [Google Scholar]
- 54.Rohrich R.J., Conrad M.H. The superiorly based nasolabial flap for simultaneous alar and cheek reconstruction. Plast. Reconstr. Surg. 2001;108:1727–1730. doi: 10.1097/00006534-200111000-00046. quiz 31. [DOI] [PubMed] [Google Scholar]
- 55.Jovanovic M., Colic M., Rasulic L., Stojicic M., Malis M. Reconstruction of the alae nasi by folded nasolabial flap. Acta Chirur. Iugosl. 2007;54:29–32. doi: 10.2298/aci0702029j. [DOI] [PubMed] [Google Scholar]
- 56.Ozkus I., Cek D.I., Ozkus K. The use of bifid nasolabial flaps in the reconstruction of the nose and columella. Ann. Plast. Surg. 1992;29:461–463. [PubMed] [Google Scholar]
- 57.Ananian S.G., Bezrukov V.M. Use of a nasolabial flap for correcting defects of the hard palate. Vestnik khirurgii imeni I I Grekova. 1989;142:91–92. [PubMed] [Google Scholar]
- 58.Mutimer K.L., Poole M.D. A review of nasolabial flaps for intra-oral defects. Br. J. Plast. Surg. 1987;40:472–477. doi: 10.1016/s0007-1226(87)90075-0. [DOI] [PubMed] [Google Scholar]
- 59.Birt B.D., Gruss J.S. Intra-oral reconstruction using the nasolabial flap. J. otolaryngol. 1985;14:233–236. [PubMed] [Google Scholar]
- 60.Morgan R.F., Chambers R.G., Jaques D.A., Hoopes J.E. Nasolabial flap in intraoral reconstruction. Review of 55 cases. Am. J. Surg. 1981;142:448–450. doi: 10.1016/0002-9610(81)90372-x. [DOI] [PubMed] [Google Scholar]
- 61.Cohen I.K., Theogaraj S.D. Nasolabial flap reconstruction of the floor of the mouth after extirpation of oral cancer. Am. J. Surg. 1975;130:479–480. doi: 10.1016/0002-9610(75)90488-2. [DOI] [PubMed] [Google Scholar]
- 62.El-Marakby H.H. The versatile naso-labial flaps in facial reconstruction. J. Egypt. Natl. Cancer Inst. 2005;17:245–250. [PubMed] [Google Scholar]
- 63.Mebeed A.H., Hussein H.A., Saber T. Critical appraisal of nasolabial flap for reconstruction of oral cavity defects in cancer patients. J. Egypt. Natl. Cancer Inst. 2009;21:33–42. [PubMed] [Google Scholar]
- 64.Chitlangia P., Kumuran E., Sabitha K.S. Use of nasolabial flap in intra and extraoral reconstruction: our experience with 40 cases. J. of Maxillofac. Oral Surg. 2012;11:451–454. doi: 10.1007/s12663-012-0336-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 65.Braasch D.C., Lam D., Oh E.S. Maxillofacial reconstruction with nasolabial and facial artery musculomucosal flaps. Oral and Maxillofac. Surg. Clin. N. Am. 2014;26:327–333. doi: 10.1016/j.coms.2014.05.003. [DOI] [PubMed] [Google Scholar]
- 66.Herbert D.C., DeGeus J. Nasolabial subcutaneous pedicle flaps. Br. J. Plast. Surg. 1975;28:90–96. doi: 10.1016/s0007-1226(75)90164-2. [DOI] [PubMed] [Google Scholar]
- 67.Thaller S.R., Kim S., Wildman M., Patterson H. Microdissection of the nasolabial axial myocutaneous flap. Ear nose Throat J. 1991;70:93–96. [PubMed] [Google Scholar]
- 68.Rahpeyma A., Khajehahmadi S. Treatment of a unilateral Tessier number 4 facial cleft in an adult: role of nasolabial V-Y advancement flap. Br. J. Oral Maxillofac. Surg. 2015;53:99–101. doi: 10.1016/j.bjoms.2014.09.019. [DOI] [PubMed] [Google Scholar]
- 69.Elliott R.A., Jr. Use of nasolabial skin flap to cover intraoral defects. Plast. Reconstr. Surg. 1976;58:201–205. doi: 10.1097/00006534-197608000-00011. [DOI] [PubMed] [Google Scholar]
- 70.Lazaridis N., Tilaveridis I., Karakasis D. Superiorly or inferiorly based “islanded” nasolabial flap for buccal mucosa defects reconstruction. J. Oral Maxillofac. Surg. 2008;66:7–15. doi: 10.1016/j.joms.2006.06.285. official journal of the American Association of Oral and Maxillofacial Surgeons. [DOI] [PubMed] [Google Scholar]
- 71.Braun M., Jr., Cook J. The island pedicle flap. Dermatol. Surg. 2005;31:995–1005. doi: 10.1111/j.1524-4725.2005.31824. official publication for American Society for Dermatologic Surgery [et al] [DOI] [PubMed] [Google Scholar]
- 72.Chen Y. Dermal pedicled nasolabial flap with subdermal vascular network for repairing nasolabial skin defects. Chin. J. Repar. Reconstr. Surg. 2011;25:1459–1461. Zhongguo xiu fu chong jian wai ke za zhi = Zhongguo xiufu chongjian waike zazhi. [PubMed] [Google Scholar]
- 73.Deora S.S., Nanjappa M., Kumaraswamy S.V. Bilateral pedicled nasolabial flaps for the anterior alveolus mandibular defect: a review. J. Maxillofac. Oral Surg. 2010;9:385–388. doi: 10.1007/s12663-010-0135-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 74.Patel S.G., Deshmukh S., Savant D.N. Squamous cell carcinoma arising in a nasolabial flap used in treatment of oral submucous fibrosis. Br. J. Plast. Surg. 1994;47:388–389. doi: 10.1016/0007-1226(94)90104-x. [DOI] [PubMed] [Google Scholar]
- 75.Eckardt A.M., Kokemuller H., Tavassol F., Gellrich N.C. Reconstruction of oral mucosal defects using the nasolabial flap: clinical experience with 22 patients. Head neck oncol. 2011;3:28. doi: 10.1186/1758-3284-3-28. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 76.Agarwal M., Gupta D.K., Tiwari A.D. Extended nasolabial flaps in the management of oral submucous fibrosis. J. Maxillofac. Oral Surg. 2011;10:216–219. doi: 10.1007/s12663-011-0236-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 77.Kshirsagar R., Chugh Modi A., Rai A. Bilateral inferiorly based nasolabial flaps for the management of advanced oral submucous fibrosis. J. Maxillofac. Oral Surg. 2010;9:22–26. doi: 10.1007/s12663-010-0008-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 78.Zitelli J.A. The nasolabial flap as a single-stage procedure. Arch. Dermatol. 1990;126:1445–1448. [PubMed] [Google Scholar]
- 79.Zilinsky I., Alcalay J., Jacobs D., Tamir J., Winkler E., Haik J. The versatility of the nasolabial flap enhanced by the delay procedure. Dermatol. Surg. 2001;27:161–164. doi: 10.1046/j.1524-4725.2001.99162.x. official publication for American Society for Dermatologic Surgery [et al] [DOI] [PubMed] [Google Scholar]
- 80.Haack S., Fischer H., Gubisch W. Lining in nasal reconstruction. Fac. Plast. Surg. FPS. 2014;30:287–299. doi: 10.1055/s-0034-1376874. [DOI] [PubMed] [Google Scholar]
- 81.Uglesic V., Virag M. Musculomucosal nasolabial island flaps for floor of mouth reconstruction. Br. J. Plast. Surg. 1995;48:8–10. doi: 10.1016/0007-1226(95)90022-5. [DOI] [PubMed] [Google Scholar]
- 82.Pribaz J., Stephens W., Crespo L., Gifford G. A new intraoral flap: facial artery musculomucosal (FAMM) flap. Plast. Reconstr. Surg. 1992;90:421–429. doi: 10.1097/00006534-199209000-00009. [DOI] [PubMed] [Google Scholar]
- 83.Bande C.R., Datarkar A., Khare N. Extended nasolabial flap compared with the platysma myocutaneous muscle flap for reconstruction of intraoral defects after release of oral submucous fibrosis: a comparative study. Br. J. oral Maxillofac. Surg. 2013;51:37–40. doi: 10.1016/j.bjoms.2012.02.015. [DOI] [PubMed] [Google Scholar]
- 84.Koranda F.C., Webster R.C. Trapdoor effect in nasolabial flaps. Causes and corrections. Arch. Otolaryngol. (Chicago, Ill 1960) 1985;111:421–424. doi: 10.1001/archotol.1985.00800090035002. [DOI] [PubMed] [Google Scholar]