Abstract
Background
The aim of this meta-analysis is to examine the safety and effectiveness of unilateral percutaneous vertebroplasty (PVP) for treatment of osteoporotic vertebral compression fractures (OVCFs) compared with that of bilateral treatment.
Methods
The multiple databases including PubMed, Springer, EMBASE, OVID, and China Journal Full-text Database were adopted to search for relevant studies in English or Chinese, and full-text articles involving comparison of unilateral and bilateral PVP surgery were reviewed. Review Manager 5.0 was adopted to estimate the effects of the results among selected articles. Forest plots, sensitivity analysis, and bias analysis for the articles included were also conducted.
Results
Finally, 1043 patients were included in the 14 studies, which eventually satisfied the eligibility criteria, and unilateral and bilateral surgeries were 550 and 493, respectively. The meta-analysis suggested that there was no significant difference of VAS score, ODI score, and cement leakage rate (MD = 0.12, 95%CI [−0.03, 0.26], P = 0.11; MD = −1.28, 95%CI [−3.59, 1.04], P = 0.28; RR = 0.89, 95%CI [0.61, 1.29], P = 0.52). The surgery time of unilateral PVP is much less than that of bilateral PVP (MD = −16.67, 95%CI [−19.22, −14.12], P < 0.00001). Patients with bilateral PVP surgery have been injected more cement than patients with unilateral PVP surgery (MD = −1.55, 95%CI [−1.94, −1.16], P < 0.00001).
Conclusions
Both punctures provide excellent pain relief and improvement of life quality. We still encourage the use of the unipedicular approach as the preferred surgical technique for treatment of OVCFs due to less operation time, limited X-ray exposure, and minimal cement introduction and extravasation.
Keywords: Unilateral percutaneous vertebroplasty, Osteoporotic vertebral compression fractures, Bilateral treatment
Background
Osteoporosis is an important health issue in ageing populations, characterized by low bone mass that leads to fragile bones and higher fracture risks [1, 2]. Osteoporosis and associated fractures are the cause of morbidity in older adults, and osteoporotic vertebral compression fracture (OVCF) is the most common one, which affects more than 200 million individuals worldwide [3]. It occurs more frequently than ankle, wrist, or hip fractures, and it may occur spontaneously just in a simple activity such as picking up something or just rising from a chair [4]. Patients with osteoporotic vertebral fractures (OVFs) suffer severe back pain for weeks to months, and spinal deformities, reduced pulmonary function, restriction of the abdominal and thoracic contents, impaired mobility, and clinical depression caused by OVCFs produce effects on patient quality of life [5–8]. OVCFs can affect both the elderly male and female. Studies suggested that OVCFs are developed in 8% of women older than 50 years and 27% of men and women older than 65 years [9, 10].
OVCFs have traditionally been treated with bed rest, analgesic use, physical therapy, and antiresorptive medications. But these treatments are conservative managements which cannot reverse the kyphotic deformities, and also cause comorbidities including deep venous thrombosis, acceleration of osteopenia, respiratory problems, and emotional problems [4, 11]. Besides, because of the poor quality of osteoporotic bone, classical surgery with metal implants often fails and contributes to persistent back pain, neurological symptoms, and functional limitations [8, 12]. Percutaneous vertebroplasty (PVP), which was introduced by Galibert in 1984 for treating osteolytic metastasis, myeloma, and hemangioma [13], is a minimally invasive surgical procedure that has gained popularity as a new treatment of OVCFs. The procedure includes placing spinal needles into fractured vertebral bodies and injecting polymethylmethacrylate (PMMA) or other bone cements into the fractured vertebral body under radiological control to relieve pain and increase bone strength [14]. After the injection of the cement, pain pathways in the surrounding tissue seem to be altered in response to various stimulations. Mechanism stabilization of the fracture, such as thermal injury to the nerve endings, results in immediate pain relief [15]. It has been reported that PVP can produce immediate pain relief compared to conservative treatments [16].
PVP is one of the optimal treatments for OVCFs and provides rapid pain relief and stabilization of fractured vertebral bodies [17, 18], but the matter of surgical approach selection remains controversial. As a minimally invasive technique, the standard technique is typically carried out using the bipedicular approach [19, 20]. Some researchers believe that bilateral PVP is more superior for excellent pain relief, which is associated with symmetrical distribution of bone cement in the vertebral body [15, 21]. But in recent years, unilateral PVP is being increasingly used for the reduction of operation and radiation exposure time and the lower risk of cement leakage and complications [22, 23]. In theory, bilateral PVP shows increased surgery time and injected cement volume, and the risk of bone cement leakage is twice that of the unipedicular approach; on the other hand, unilateral PVP can reduce the operation time, surgery-associated complications, radiation exposure, and cost, and unilateral PVP can also achieve the same clinical results.
The aim of this meta-analysis is to examine the safety and effectiveness of unilateral percutaneous vertebroplasty for treatment of osteoporotic vertebral compression fractures compared with that of bilateral treatment. Owing to the inconsistent results of studies about shear bond strength, it is necessary to perform a systematic review and meta-analysis to study the difference of curative effects and complication rates of surgery between unilateral and bilateral PVP, which will undoubtedly increase surgeon confidence of both medical staffs and patients.
Methods
Search strategy
Related citations about unilateral and bilateral PVP surgery were systematically searched, and a systematic review was undertaken with articles published from January 2000 to January 2016 among multiple electronic databases. To assemble all of the relevant published citations, PubMed, Springer, EMBASE, OVID, and China Journal Full-text Database were searched. All publication statuses (published, unpublished, in press, and in progress) were included. We searched the literature independently, and studies were initially reviewed by titles and abstracts. No restrictions about the publication language were made.
The following keywords were used to maximize the search specificity and sensitivity in our search work: (1) osteoporotic vertebral compression fractures OR OVCF OR VCF, (2) percutaneous vertebroplasty OR vertebroplasty OR PVP OR VP, and (3) unilateral OR bilateral OR unipedicular OR bipedicular. MeSH terms and Boolean operators were selected for each database search. All the citations searched out were screened for further selection.
Citation selection
Both my companion and I selected the citations in this process, independently and attentively. They screened the titles and abstracts of the articles identified by the electronic search criteria presented above. Subsequently, the full text of the studies that potentially met the criteria were obtained and reviewed to check whether the study was likely to be relevant.
These relevant studies included in this study must meet the following inclusion criteria:
Adult patients with osteoporotic vertebral fractures
Sample size of more than 20
A randomized control trial or controlled clinical trial study
Comparison between unilateral and bilateral PVP
Available exclusion criteria
Exclusion criteria:
Non-randomized studies
Studies on other diseases rather than OVCFs
Studies lacking outcome measures or comparable results
After the primary selection, these two researchers met and reviewed their selections for agreement. Disagreements were resolved by reaching a consensus through discussion.
Data extraction
Two of the reviewers independently read the full text of the articles and extracted the characteristics from each study using a standard data extraction form in Excel 2010. The data extracted from these studies included the first author’s name, year of publication, year of onset, mean age of patients, sample size (unilateral/bilateral), sex distribution (male/female), outcome measurements, and follow-up time. Outcome measurements, including visual analog scale (VAS), Oswestry Disability Index (ODI), surgery time, injected cement volume, and cement leakage outcome were collected to estimate the difference between unilateral and bilateral PVP.
Statistical analysis
We performed all of the meta-analyses with Review Manager 5.0 (The Cochrane Collaboration, 2011) to estimate the safety and effectiveness of unilateral PVP compared with that of bilateral treatment among selected articles. Following the Review Manager 5.3 Tutorial, the risk-of-bias table of the included studies was independently assessed by two authors. The assessment included the following criterions: (1) random sequence generation, (2) allocation concealment, (3) blinding of participants and personnel, (4) blinding of outcome assessment, (5) incomplete outcome data, (6) selective reporting, and (7) other biases. Any disagreements were resolved by discussion. If any problems of poor agreement occurred or no consensus could be achieved, a third investigator was the adjudicator.
For continuous outcomes, including VAS, ODI, surgery time, and injected cement volume, standard mean difference (SMD) with 95% confidence intervals (CIs) was calculated by the mean and standard deviation. Related risk (RR) with 95%CIs was calculated to estimate the cement leakage outcome. A P value <0.05 was considered to be statistically significant.
Heterogeneity was assessed using Q statistics in this study. The value of I 2 statistic reflects the levels of heterogeneity. A random-effect model was adopted when moderate or high heterogeneity was obtained, which means the heterogeneity I 2 statistic is >50%; otherwise, a fixed-effect model was chosen.
In addition, sensitivity analysis and bias analysis of the studies were conducted to examine the quality of articles. To estimate possible publication bias, a funnel plot was used.
Results
Search results
A total of 1223 titles and abstracts were preliminarily reviewed in these electronic databases after the primary selection, of which 14 studies [22, 24–36] eventually satisfied the eligibility criteria. The other 1207 articles were excluded for duplication, irrelevant studies, inappropriate data, inappropriate comparison, reviews, without a control group, other diseases, other surgeries, or not a full text. A flow diagram that reflects the search process can be seen in Fig. 1 including the reasons for exclusion. Among these 14 articles, 9 report on VAS score for analgesic efficacy evaluation, 4 on ODI for functional assessment, 9 on surgery time, 11 on injected cement volume, and 9 on cement leakage.
Fig. 1.

Flow diagram of the study selection showing the number of citations identified, excluded, and included in final analysis
Characteristics of included studies
Detailed characteristics of the included studies are provided in Table 1. The first author’s name, year of publication, year of onset, mean age of patients, sample size (unilateral/bilateral), sex distribution (male/female), outcome measurements, and follow-up time are presented in the table. All these articles were published from 2013 to 2015. In total, 1043 patients were included in the 14 studies, and unilateral and bilateral surgeries were 550 and 493, respectively. The sample size ranges from 39 to 153. All patients in these studies were adults.
Table 1.
Characteristic of the included studies
| Author | Year of publication | Year of onset | Mean age | Sample size (unilateral/bilateral) | Sex distribution (male/female) | Outcome measurements | Follow-up time |
|---|---|---|---|---|---|---|---|
| Chen CM [25] | 2014 | – | Unilateral group, 69.43 ± 6.25; bilateral group, 68.66 ± 8.76 | 39 (20/19) | –/– | VAS, ODI, surgery time, Cement leakage, injected cement volume | 2 years |
| Feng Y [26] | 2014 | February 2010 to February 2012 | Unilateral group, 72.5; bilateral group, 69.4 | 117 (61/56) | 30/87 | VAS, ODI, injected cement volume | 2 years |
| Guo ZP [27] | 2015 | March 2008 to March 2014 | Unilateral group, 67.32 ± 11.24; bilateral group, 69.35 ± 12.46 | 153 (91/62) | 29/124 | VAS, ODI, surgery time, Injected cement volume, cement leakage | – |
| Li J [28] | 2015 | April 2007 to February 2014 | Unilateral group, 67.9; bilateral group, 65.7 | 65 (36/29) | 30/35 | VAS, surgery time, injected cement volume, cement leakage | 6 to 18 months |
| Ren HL [29] | 2014 | January 2009 to January 2012 | Unilateral group, 69.4 ± 10.4; bilateral group, 69.7±9.7 | 101 (45/56) | 17/84 | Surgery time, injected cement volume, cement leakage | More than 1 year |
| Wang W [30] | 2013 | February 2009 to February 2011 | Unilateral group, 66.9; bilateral group, 68.7 | 47 (25/22) | 18/29 | VAS, cement leakage | 1 year |
| Xiao L [31] | 2015 | September 2012 to December 2014 | Unilateral group, 70.9 ± 9.3; bilateral group, 68.5±7.3 | 71 (40/31) | –/– | VAS, injected cement volume, cement leakage | 3 days |
| Yuan WQ [32] | 2014 | June 2013 to June 2014 | 70.36 ± 0.35 | 72 (36/36) | 33/39 | Surgery time, injected cement volume | 2 days |
| Zhai HL [33] |
2013 | January 2010 to February 2012 | Unilateral group, 70.5; bilateral group, 74.3 | 48 (27/21) | 6/42 | VAS, surgery time, injected cement volume | 1 day |
| Zhang L [34] | 2015 | November 2010 to October 2012 | Unilateral group, 71.7 ± 7.5; bilateral group, 72.1 ± 6.0 | 50 (24/26) | 13/37 | VAS, ODI, PCS, MCS, surgery time, cement leakage, injected cement volume | 2 years |
| Zhang LG [35] | 2015 | January 2008 to December 2011 | Unilateral group, 70.0 ± 2.9; bilateral group, 70.7 ± 2.5 | 68 (36/32) | 0/68 | VAS, QUALEFFO, cement, cement leakage | 1 year |
| Zhang X [36] | 2014 | March 2012 to August 2013 | 70 ± 0.27 | 53 (28/25) | 25/28 | Surgery time, injected cement volume | – |
| Zhao XQ [37] | 2014 | May 2011 to February 2013 | Unilateral group, 74; bilateral group, 73 | 80 (40/40) | 48/32 | Curative effect, surgery time, injected cement volume | 2 days |
| Zhou R [38] | 2015 | February 2011 to January 2013 | Unilateral group, 68.8 ± 5.1; bilateral group, 70.6 ± 4.8 | 79 (41/38) | 46/33 | VAS, surgery time, injected cement volume, cement leakage | 1 year |
Quality assessment
All of the non-randomized control trials had insufficient information on the randomization methods. All 14 included studies were grouped randomly, but the methods of randomization were not mentioned. So we classified these articles as controlled clinical trial studies. The risk-of-bias table was used to evaluate the risk of each study. The risk-of-bias table in this meta-analysis is shown in Table 2. High risk of blinding of participants and personnel existed for the particularity of the operation.
Table 2.
The risk-of-bias table in this meta-analysis
| Chen CM [25] | Feng Y [26] | Guo ZP [27] | Li J [28] | Ren HL [29] | Wang W [30] | Xiao L [31] | Yuan WQ [32] | Zhai HL [33] | Zhang L [34] | Zhang LG [35] | Zhang X [36] | Zhao XQ [37] | Zhou R [38] | |
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Random sequence generation | Low | Low | Low | Low | Low | Low | Low | Low | Low | Low | Low | Low | Low | Low |
| Allocation concealment | Not | Not | Not | Not | Not | Not | Not | Not | Not | Not | Not | Not | Not | Not |
| Blinding of participants and personnel | High | High | High | High | High | High | High | High | High | High | High | High | High | High |
| Blinding of outcome assessment | Low | Low | Low | Not | Low | High | Low | High | Low | Low | Low | Low | High | High |
| Incomplete outcome data | Low | Low | Low | Low | Low | Low | Low | Low | Low | Low | Low | Low | Low | Low |
| Selective reporting | Not | Low | Not | High | Not | High | Low | Low | Low | Low | Low | High | Low | Low |
| Other biases | Low | Low | Low | Not | Not | Low | Not | Not | Not | Low | Low | High | Not | Low |
Note: In this table, “Low” stands for low risk, “High” stands for high risk, and “Not” stands for not clear
Results of meta-analysis
Meta-analysis about VAS score
Nine of the 14 included studies report on VAS score for analgesic efficacy evaluation. The forest plot for the VAS score in unilateral and bilateral PVP groups is shown in Fig. 2. Among these 9 articles, only Zhang LG’s study showed the statistical difference between unilateral and bilateral PVP (MD = 0.41, 95%CI [0.09, 0.73]). The other studies showed no statistical significance. The meta-analysis suggested that there was no significant difference of the VAS score in the unilateral group and bilateral group (MD = 0.12, 95%CI [−0.03, 0.26], P = 0.11; P for heterogeneity = 0.33, I 2 = 12%).
Fig. 2.
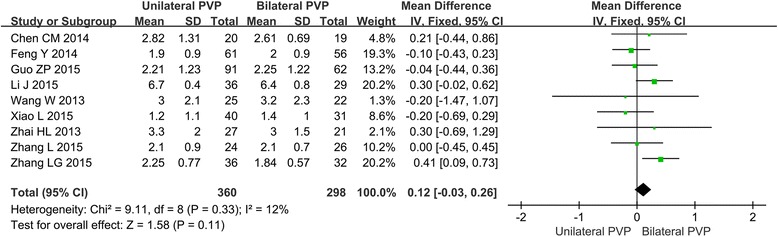
Forest plot for the VAS score in unilateral and bilateral PVP groups
Meta-analysis about ODI score
Four included studies report on the ODI score between unilateral and bilateral PVP groups. As shown in the forest plot (Fig. 3), Chen CM reported the statistical difference between unilateral and bilateral PVP (MD = −3.94, 95%CI [−5.61, −2.27]). The result of the meta-analysis showed that the difference of ODI score between unilateral and bilateral PVP was not significant (MD = −1.28, 95%CI [−3.59, 1.04], P = 0.28; P for heterogeneity = 0.002, I 2 = 80%).
Fig. 3.
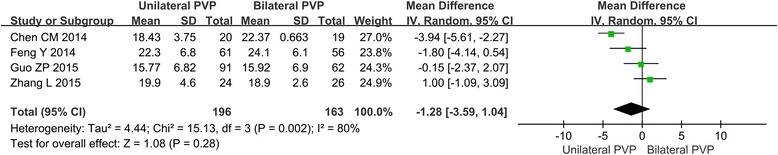
Forest plot for the ODI score in unilateral and bilateral PVP groups
Meta-analysis about the surgery time
Among the 14 articles, there are 9 studies which are about the comparison of surgery time. The forest plot for the surgery time is shown in Fig. 4. All these 9 studies showed the significant differences of surgery time between unilateral and bilateral PVP, and the meta-analysis indicated that the surgery time of unilateral PVP is much less than that of bilateral PVP (MD = −16.67, 95%CI [−19.22, −14.12], P < 0.00001; P for heterogeneity < 0.00001, I 2 = 87%).
Fig. 4.
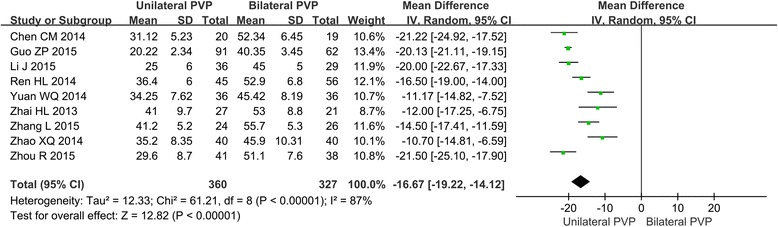
Forest plot for the surgery time in unilateral and bilateral PVP groups
Meta-analysis about the injected cement volume
All the 11 studies on the cement volume injected in PVP have showed the statistically significant difference between unilateral and bilateral PVP. The result of the meta-analysis indicated that in bilateral PVP surgery, patients with OVCFs have been injected more cement than patients in a unilateral surgery (MD = −1.55, 95%CI [−1.94, −1.16], P < 0.00001; P for heterogeneity < 0.00001, I 2 = 92 %). The forest plot for the injected cement volume is shown in Fig. 5.
Fig. 5.
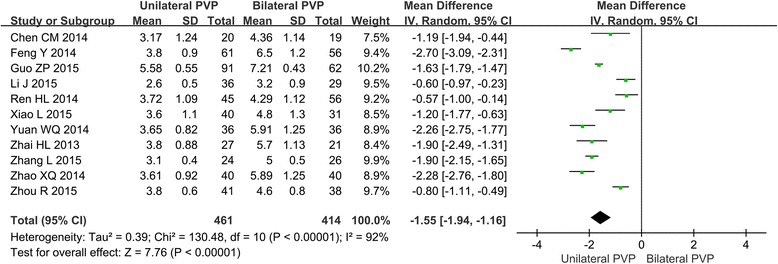
Forest plot for the injected cement volume in unilateral and bilateral PVP groups
Meta-analysis about the cement leakage rate
Among the 14 included studies, 11 are about the cement leakage outcome in unilateral and bilateral PVP groups. The forest plot (Fig. 6) showed that only Chen CM has reported the statistical difference of cement leakage rate between unilateral and bilateral PVP (RR = 0.57, 95%CI [0.33, 0.98]). The result of the meta-analysis showed that the difference of cement leakage rate between unilateral and bilateral PVP was not significant (RR = 0.89, 95%CI [0.61, 1.29], P = 0.52; P for heterogeneity = 0.02, I 2 = 55%).
Fig. 6.
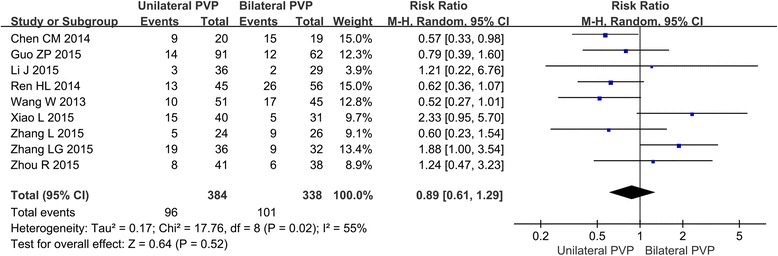
Forest plot for the cement leakage outcome in unilateral and bilateral PVP groups
Bias analysis
According to the results above, high heterogeneities of the ODI score, surgery time, injected cement volume, and cement leakage rate were observed (I 2 = 80, 87, 92, and 55%, respectively).
A funnel plot for the studies about VAS score in unilateral and bilateral PVP groups was performed (Fig. 7). Egger's tests of different parameters are presented in Table 3, which showed that no publication bias was observed in these meta-analyses (P > 0.05).
Fig. 7.
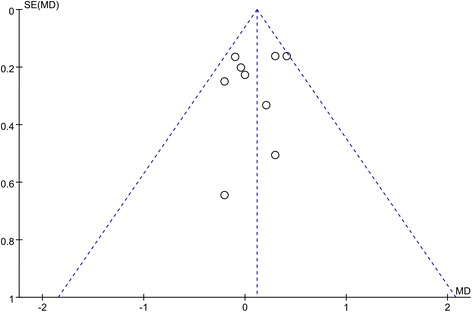
Funnel plot for the studies about VAS score in unilateral and bilateral PVP groups
Table 3.
Egger’s tests of different parameters
| Coefficient | Standard error | t | P > |t| | [95% confidence interval] | |
|---|---|---|---|---|---|
| VAS score | −0.612 | 1.017 | −0.600 | 0.566 | [−3.016648, 1.792176] |
| ODI score | 10.550 | 7.103 | 1.490 | 0.276 | [−20.01237, 41.11181] |
| Surgery time | 3.177 | 1.427 | 2.230 | 0.061 | [−0.1973189, 6.552231] |
| Injected cement volume | 0.445 | 2.572 | 0.170 | 0.867 | [−5.372733, 6.262107] |
| Cement leakage rate | 0.206 | 0.181 | 1.140 | 0.293 | [−0.2219323, 0.6332165] |
Discussion
Excellent strategies for OVCFs are treatments with effective management of pain, short time of recovery, and no requirement of an extended nursing and rehabilitation care [37]. Longo et al. [38] had reported the evidence available on the conservative care for patients with OVCFs and focused on the role of the most commonly used spinal orthoses. But conservative management has not been standardized. Since percutaneous vertebroplasty was introduced more than 30 years ago, researchers extended to vertebral fractures. In the past decades, it has been proved that PVP is a safe and effective surgery. In these studies [17–20], both unipedicular and bipedicular surgeries achieved satisfactory results and patients’ clinical outcome parameters were significantly improved and consistent compared to pre-surgical condition. Some have proved that compared with bilateral PVP, unilateral PVP surgery provides comparable restoration of vertebral body stiffness and therapeutic effects [39, 40]. In this meta-analysis, we compared the effectiveness between unilateral and bilateral PVP through VAS, ODI, surgery time, injected cement volume, and cement leakage outcome.
Owing to the cytotoxic effect of polymethylmethacrylate (PMMA), which is injected into the bones and causes damage to terminal nerve endings, and the immobility and inhibition of micro movement in the fractured fragment [41, 42], significant pain reduction was achieved in the PVP groups who suffered from thoracolumbar compression fractures [43]. VAS is a psychometric response scale used in questionnaires, which measures the subjective characteristics or attitudes that cannot be directly measured. Studies use VAS to estimate pain relief after PVP surgery compared with pre-operation. The meta-analysis suggested that there was no significant difference of the VAS score in the unilateral group and bilateral group, which means that the pain relief of the unilateral group is as much as that of the bilateral group. ODI is an index used by clinicians and researchers to quantify disability for low back pain. A score of 0 is equated with no disability and 100 is the maximum disability possible. The results showed that the ODI score of unilateral PVP was similar to that of bilateral PVP. Also, as we had expected, the bilateral surgery costs more time and more material than the unilateral surgery.
Although relatively safe and effective, PVP may cause complications including cement leakage, soft tissue damage, pedicle fracture, nerve injury, and spinal epidural hematoma [44]. Cement leakage is one of the most frequent complications of vertebroplasty. Symptoms of nerve irritation through compression of nerve roots may be caused by the leakage. It has been reported that pulmonary cement embolism (PCE) following vertebroplasty existed. Cement leakages of both unilateral and bilateral PVP are reported to be as high as 73% [9], but most leakages remain clinically asymptomatic, and even small quantities of leakage may have a significant clinical impact, which is often recognized by their clinical signs and symptoms such as chest pain, dyspnea, tachypnea, coughing, and sweating [45]. In this study, the total cement leakage rates of both groups were 25% (96/384) and 29.88% (101/338), respectively, but no statistically significant difference was observed. The results suggested that increased bone cement injection did not result in increased bone cement leakage rate, and it may be attributed to the nature of the high-viscosity bone cement itself.
Our results support the point that the unipedicular technique is a faster, lower risk alternative that provides a comparable spinal deformity correction than the bipedicular approach. It also increased the cost-effectiveness of the procedure for injecting less cement and cost less surgery time, which lowers the risk of surgery and morbidity.
However, this study has some limitations. In this study, we chose the random-effect model for high heterogeneities of the meta-analyses (I 2 > 50%). The reasons for high heterogeneities were complex, including different surgical technologies used, varying types of fractures, pre-surgical medical status, and different follow-up times. Also non-RCT studies cause greater bias risks than RCT studies. Besides, the poor quality of some studies indicates that further well-designed and prospective studies are needed to determine the clinical outcomes, which this study did not cover.
Conclusions
Both unipedicular and bipedicular surgery are safe and effective treatments for OVCF. Although both punctures provide excellent pain relief and improvement of life quality, we encourage the use of the unipedicular approach as the preferred surgical technique for treatment of OVCFs due to less operation time, limited X-ray exposure, and minimal cement introduction and extravasation.
Acknowledgements
Not applicable.
Funding
This research was funded by the Scientific Research Foundation for the Returned Overseas Chinese Scholar, Ministry of Education of China [(2015) 311].
Availability of data and materials
All data are available, and there is no supporting material in this study.
Authors’ contributions
HS and CL wrote the paper, collected the data, analyzed the data, and reviewed the paper prior to submission. CL took control of the whole work. Both authors read and approved the final manuscript.
Competing interests
The authors declare that they have no competing interests.
Consent for publication
Not applicable.
Ethics approval and consent to participate
Not applicable.
Abbreviations
- OVCFs
Osteoporotic vertebral compression fractures
- OVFs
Osteoporotic vertebral fractures
- PVP
Percutaneous vertebroplasty
- RR
Related risk
- SMD
Standard mean difference
- VAS
Visual analog scale
References
- 1.Litwic A, Cooper C, Dennison E. Osteoporosis therapies in 2014. Panminerva Med. 2014;56(4):273–83. [PubMed] [Google Scholar]
- 2.European Prospective Osteoporosis Study G. Felsenberg D, Silman AJ, Lunt M, Armbrecht G, Ismail AA, et al. Incidence of vertebral fracture in Europe: results from the European Prospective Osteoporosis Study (EPOS) J Bone Miner Res. 2002;17(4):716–24. doi: 10.1359/jbmr.2002.17.4.716. [DOI] [PubMed] [Google Scholar]
- 3.Johnell O, Kanis JA. An estimate of the worldwide prevalence and disability associated with osteoporotic fractures. Osteoporis Int. 2006;17(12):1726–33. doi: 10.1007/s00198-006-0172-4. [DOI] [PubMed] [Google Scholar]
- 4.Ma XL, Xing D, Ma JX, Xu WG, Wang J, Chen Y. Balloon kyphoplasty versus percutaneous vertebroplasty in treating osteoporotic vertebral compression fracture: grading the evidence through a systematic review and meta-analysis. Eur Spine J. 2012;21(9):1844–59. doi: 10.1007/s00586-012-2441-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Bergland A, Thorsen H, Karesen R. Association between generic and disease-specific quality of life questionnaires and mobility and balance among women with osteoporosis and vertebral fractures. Aging Clin Exp Res. 2011;23(4):296–303. doi: 10.1007/BF03324967. [DOI] [PubMed] [Google Scholar]
- 6.Frankel BM, Monroe T, Wang C. Percutaneous vertebral augmentation: an elevation in adjacent-level fracture risk in kyphoplasty as compared with vertebroplasty. Spine J. 2007;7(5):575–82. doi: 10.1016/j.spinee.2006.10.020. [DOI] [PubMed] [Google Scholar]
- 7.Leech JA, Dulberg C, Kellie S, Pattee L, Gay J. Relationship of lung function to severity of osteoporosis in women. Am Rev Respir Dis. 1990;141(1):68–71. doi: 10.1164/ajrccm/141.1.68. [DOI] [PubMed] [Google Scholar]
- 8.Phillips FM. Minimally invasive treatments of osteoporotic vertebral compression fractures. Spine. 2003;28(15 Suppl):S45–53. doi: 10.1097/01.BRS.0000076898.37566.32. [DOI] [PubMed] [Google Scholar]
- 9.Bonnick SL. Osteoporosis in men and women. Clin Cornerstone. 2006;8(1):28–39. doi: 10.1016/S1098-3597(06)80063-3. [DOI] [PubMed] [Google Scholar]
- 10.Kumar K, Verma AK, Wilson J, LaFontaine A. Vertebroplasty in osteoporotic spine fractures: a quality of life assessment. Can J Neurol Sci. 2005;32(4):487–95. doi: 10.1017/S0317167100004492. [DOI] [PubMed] [Google Scholar]
- 11.Kim KW, Cho KJ, Kim SW, Lee SH, An MH, Im JH. A nation-wide, outpatient-based survey on the pain, disability, and satisfaction of patients with osteoporotic vertebral compression fractures. Asian Spine J. 2013;7(4):301–7. doi: 10.4184/asj.2013.7.4.301. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Dickman CA, Fessler RG, MacMillan M, Haid RW. Transpedicular screw-rod fixation of the lumbar spine: operative technique and outcome in 104 cases. J Neurosurg. 1992;77(6):860–70. doi: 10.3171/jns.1992.77.6.0860. [DOI] [PubMed] [Google Scholar]
- 13.Galibert P, Deramond H, Rosat P, Le Gars D. Preliminary note on the treatment of vertebral angioma by percutaneous acrylic vertebroplasty. Neuro-Chirurgie. 1987;33(2):166–8. [PubMed] [Google Scholar]
- 14.Barr JD, Barr MS, Lemley TJ, McCann RM. Percutaneous vertebroplasty for pain relief and spinal stabilization. Spine. 2000;25(8):923–8. doi: 10.1097/00007632-200004150-00005. [DOI] [PubMed] [Google Scholar]
- 15.Cotten A, Dewatre F, Cortet B, Assaker R, Leblond D, Duquesnoy B, et al. Percutaneous vertebroplasty for osteolytic metastases and myeloma: effects of the percentage of lesion filling and the leakage of methyl methacrylate at clinical follow-up. Radiology. 1996;200(2):525–30. doi: 10.1148/radiology.200.2.8685351. [DOI] [PubMed] [Google Scholar]
- 16.Klazen CA, Lohle PN, de Vries J, Jansen FH, Tielbeek AV, Blonk MC, et al. Vertebroplasty versus conservative treatment in acute osteoporotic vertebral compression fractures (Vertos II): an open-label randomised trial. Lancet. 2010;376(9746):1085–92. doi: 10.1016/S0140-6736(10)60954-3. [DOI] [PubMed] [Google Scholar]
- 17.Voormolen MH, Mali WP, Lohle PN, Fransen H, Lampmann LE, van der Graaf Y, et al. Percutaneous vertebroplasty compared with optimal pain medication treatment: short-term clinical outcome of patients with subacute or chronic painful osteoporotic vertebral compression fractures. The VERTOS study. Am J Neuroradiol. 2007;28(3):555–60. [PMC free article] [PubMed] [Google Scholar]
- 18.Stevenson M, Gomersall T, Lloyd Jones M, Rawdin A, Hernandez M, Dias S, et al. Percutaneous vertebroplasty and percutaneous balloon kyphoplasty for the treatment of osteoporotic vertebral fractures: a systematic review and cost-effectiveness analysis. Health Technol Assess. 2014;18(17):1–290. doi: 10.3310/hta18170. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Georgy BA. Clinical experience with high-viscosity cements for percutaneous vertebral body augmentation: occurrence, degree, and location of cement leakage compared with kyphoplasty. AJNR Am J Neuroradiol. 2010;31(3):504–8. doi: 10.3174/ajnr.A1861. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Nieuwenhuijse MJ, Muijs SP, van Erkel AR, Dijkstra SP. A clinical comparative study on low versus medium viscosity polymethylmetacrylate bone cement in percutaneous vertebroplasty: viscosity associated with cement leakage. Spine. 2010;35(20):E1037–44. doi: 10.1097/BRS.0b013e3181ddd262. [DOI] [PubMed] [Google Scholar]
- 21.Liebschner MA, Rosenberg WS, Keaveny TM. Effects of bone cement volume and distribution on vertebral stiffness after vertebroplasty. Spine. 2001;26(14):1547–54. doi: 10.1097/00007632-200107150-00009. [DOI] [PubMed] [Google Scholar]
- 22.Chen C, Bian J, Zhang W, Zhang W, Zhao C, Wei H. Unilateral versus bilateral vertebroplasty for severe osteoporotic vertebral compression fractures. J Spinal Disord Tech. 2014;27(8):E301–4. doi: 10.1097/BSD.0000000000000118. [DOI] [PubMed] [Google Scholar]
- 23.Gao W, Mi S, Gao J. [Percutaneous vertebroplasty to treat osteoporotic vertebral compression fractures combined with intravertebral clefts by unilateral approach]. Zhongguo xiu fu chong jian wai ke za zhi = Zhongguo xiufu chongjian waike zazhi = Chinese Journal of Reparative and Reconstructive Surgery. 2012;26(11):1330–5. [PubMed]
- 24.Guo ZPWG, Li XQ. The effect comparison of the percutaneous vertebroplasty for osteoporotic vertebral compression fractures via the unilateral and bilateral transpedicular approach. Chin J Modern Operative Surgery. 2015;19:439–42. [Google Scholar]
- 25.Feng YWH, Chen B. Comparison of unilateral and bilateral percutaneous vertebroplasty for treating aged osteoporotic vertebral compression fractures with local anesthesia. J Clin Exp Med. 2014;13:911–4. [Google Scholar]
- 26.Li JSW, Chang XH. Comparison of clinical effects between unilateral and bilateral percutaneous vertebroplasty for osteoporotic vertebral compression fractures. J Dalian Med Uni. 2015;37:145–7. [Google Scholar]
- 27.Ren HLWJ, Chen JT. Comparison of unipedicular versus bipedicular percutaneous vertebroplasty for osteoporotic vertebral compression fractures. Chin J Orthop Trauma. 2014;16:684–9. [Google Scholar]
- 28.Wang WWC, Zhu SH. Outcomes of unilateral or bilateral percutaneous vertebroplasty for osteoporotic vertebral compression fractures. J Pract Orthop. 2013;19:690–2. [Google Scholar]
- 29.Xiao LXH, Liu P. Comparison of the clinical effects by unilateral or bilateral percutaneous vertebroplasty for osteoporotic vertebral compression fracture. J Wannan Med College. 2015;34:533–6. [Google Scholar]
- 30.Yuan WQ ZL. Comparison of unilateral and bilateral PVP for treating aged OVCF with local anesthesia. Journal of Bethune Medical Science. 2014;12:582
- 31.Zhai KLZF. The clinical effects of unilateral or bilateral percutaneous vertebroplasty for osteoporotic vertebral compression fracture. Inner Mongolia Med J. 2013;12:1501–2. [Google Scholar]
- 32.Zhang L, Liu Z, Wang J, Feng X, Yang J, Tao Y, et al. Unipedicular versus bipedicular percutaneous vertebroplasty for osteoporotic vertebral compression fractures: a prospective randomized study. BMC Musculoskelet Disord. 2015;16:145. doi: 10.1186/s12891-015-0590-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Zhang LG, Gu X, Zhang HL, Zhang QG, Cai XB, Tao K. Unilateral or bilateral percutaneous vertebroplasty for acute osteoporotic vertebral fracture: a prospective study. J Spinal Disord Tech. 2015;28(2):E85–8. doi: 10.1097/BSD.0000000000000147. [DOI] [PubMed] [Google Scholar]
- 34.Zhang XGA, Hou SZ. Investigation of the superiority of unilateral or bilateral percutaneous vertebroplasty for osteoporotic vertebral compression fractures. Medical Innovation China. 2014;11:17–9. [Google Scholar]
- 35.Zhao XQRY, Sun QL. Comparison of the effects by unilateral and bilateral percutaneous vertebroplasty for osteoporotic vertebral compression fracture. Contemporary Medicine Forum. 2014;12:209. [Google Scholar]
- 36.Zhou RFH, Zhou YH. Unilateral or bilateral percutaneous vertebroplasty for osteoporotic vertebral fracture. J Clin Orthopaedics. 2015;18:667–8. [Google Scholar]
- 37.Longo UG, Loppini M, Denaro L, Brandi ML, Maffulli N, Denaro V. The effectiveness and safety of vertebroplasty for osteoporotic vertebral compression fractures. A double blind, prospective, randomized, controlled study. Clin Cases Miner Bone Metab. 2010;7:109–13. [PMC free article] [PubMed] [Google Scholar]
- 38.Longo UG, Loppini M, Denaro L, Maffulli N, Denaro V. Conservative management of patients with an osteoporotic vertebral fracture: a review of the literature. J Bone Joint Surg (Br) 2012;94:152–7. doi: 10.1302/0301-620X.94B2.26894. [DOI] [PubMed] [Google Scholar]
- 39.Steinmann J, Tingey CT, Cruz G, Dai Q. Biomechanical comparison of unipedicular versus bipedicular kyphoplasty. Spine. 2005;30(2):201–5. doi: 10.1097/01.brs.0000150831.46856.87. [DOI] [PubMed] [Google Scholar]
- 40.Tohmeh AG, Mathis JM, Fenton DC, Levine AM, Belkoff SM. Biomechanical efficacy of unipedicular versus bipedicular vertebroplasty for the management of osteoporotic compression fractures. Spine. 1999;24(17):1772–6. doi: 10.1097/00007632-199909010-00004. [DOI] [PubMed] [Google Scholar]
- 41.Belkoff SM, Mathis JM, Jasper LE, Deramond H. The biomechanics of vertebroplasty. The effect of cement volume on mechanical behavior. Spine. 2001;26(14):1537–41. doi: 10.1097/00007632-200107150-00007. [DOI] [PubMed] [Google Scholar]
- 42.Heini PF, Walchli B, Berlemann U. Percutaneous transpedicular vertebroplasty with PMMA: operative technique and early results. A prospective study for the treatment of osteoporotic compression fractures. Eur Spine J. 2000;9(5):445–50. doi: 10.1007/s005860000182. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Schofer MD, Efe T, Timmesfeld N, Kortmann HR, Quante M. Comparison of kyphoplasty and vertebroplasty in the treatment of fresh vertebral compression fractures. Arch Orthop Trauma Surg. 2009;129(10):1391–9. doi: 10.1007/s00402-009-0901-1. [DOI] [PubMed] [Google Scholar]
- 44.Nieuwenhuijse MJ, Van Erkel AR, Dijkstra PD. Cement leakage in percutaneous vertebroplasty for osteoporotic vertebral compression fractures: identification of risk factors. Spine J. 2011;11(9):839–48. doi: 10.1016/j.spinee.2011.07.027. [DOI] [PubMed] [Google Scholar]
- 45.Martin DJ, Rad AE, Kallmes DF. Prevalence of extravertebral cement leakage after vertebroplasty: procedural documentation versus CT detection. Acta Radiol. 2012;53(5):569–72. doi: 10.1258/ar.2012.120222. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Data Availability Statement
All data are available, and there is no supporting material in this study.


