Key Clinical Message
Inflammatory myofibroblastic tumor (IMT) histologically characterized by fibroblastic and myofibroblastic proliferation with inflammatory infiltrate. The therapy adopted was Whipple's pancreaticoduodenectomy with a histological diagnosis of the inflammatory myofibroblastic tumor. The disease that should be considered as the differential diagnosis is pancreatic cancer. The diagnosis and treatment of IMT is surgical resection.
Keywords: Inflammatory tumor, pancreatic mass, surgical resection, Whipple procedure
Introduction
Inflammatory myofibroblastic tumor (IMT), also known as inflammatory pseudotumor, is a generic term applied to a heterogeneous group of lesions occurring in various organs, which is histologically characterized by fibroblastic and myofibroblastic proliferation with inflammatory infiltrate 1. Inflammatory myofibroblastic tumor was first described in the lung, where it was considered a postinflammatory condition rather than a malignancy process 2, 3. Recent data suggest that IMT can be detected in various anatomic regions, and organs including liver, gastrointestinal tract, abdominal soft tissue, lymph node, spleen, and extremely rare in the pancreas. In this study, we reported a patient who admitted to the emergency department with signs of acute abdomen. Further investigations diagnosed as IMT caused from pancreatic head mass.
Case Report
A 46‐year‐old male, without any known health problems, admitted to our hospital with signs and symptoms of acute abdomen. There were no any biliary or gastrointestinal obstruction symptoms. On physical examination, there was diffuse abdominal pain and tenderness. Laboratory analyses have shown that it was acute pancreatitis. The amylase level was 224 U/L, pancreatic amylase level was 597 U/L, GGT was 904 U/L, and WBC was 11.5, respectively. CA19‐9 level was 110.80 U/mL, while all the other tumor markers were at normal levels. Abdominal ultrasound revealed a 129 × 70 mm mass in the head of the pancreas. Abdominal magnetic resonance imaging (MRI) was performed. MRI findings showed that there was a 92 × 84 mm mass with solid and cystic components in the pancreas uncinate process. Multiple lymph nodes, the largest of which was 16 × 10 mm in size, were detected around the pancreatic mass (Fig. 1).
Figure 1.
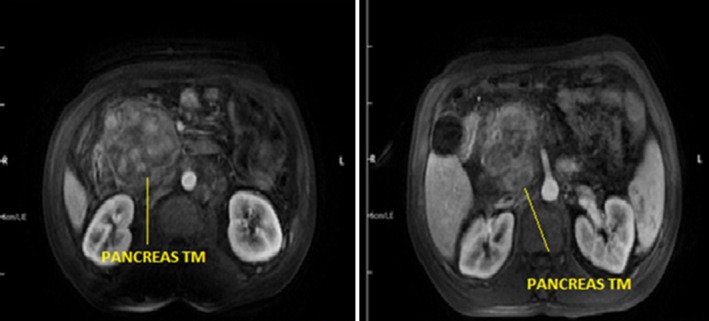
Magnetic resonance imaging sections revealed a heterogeneous pancreatic mass measuring 92 × 84 mm mass with solid and cystic components in the pancreas uncinate process.
The patient's oral intake was stopped, and intravenous fluid therapy was started. During the medical follow‐up, the abdominal pain decreased and laboratory findings fell to normal levels. After 4 weeks of acute pancreatitis episode, patient was operated. During laparotomy, the mass, which was associated with multiple fibrous adhesions to the surrounding tissue, was resected by pancreaticoduodenectomy (Whipple procedure). Eight days after the surgery, the patient was discharged in good health with no complication.
Macroscopically, the tumor was 8 × 6 × 5 cm mass, poorly demarcated from the normal pancreatic parenchyma. The pancreatic duct was intact, and the tumor was as an elastic, hard, solid mass with a yellowish and whitish cut surface (Fig. 2).
Figure 2.
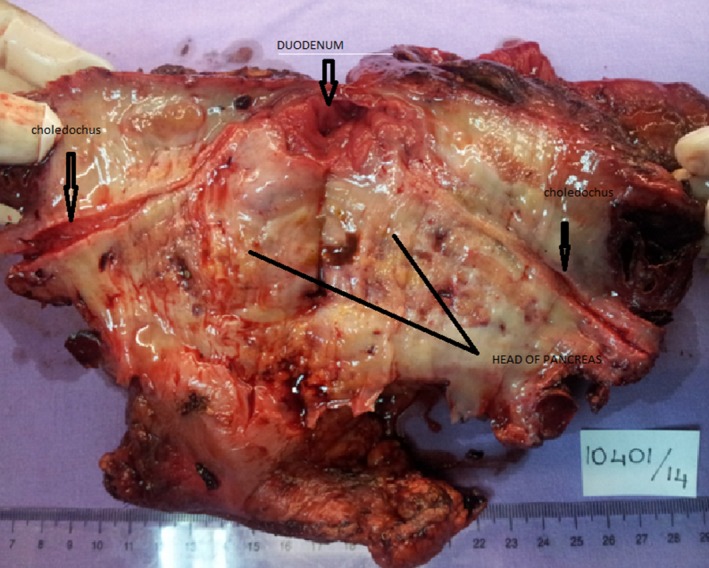
Macroscopic view of the resected material.
Histologically, there was chronic inflammation and edema around the ampulla of Vater. In some sections of the specimen, fibrous spindle cells were observed in myxoid stroma of the pancreas. The immunohistochemical studies showed a nonspecific staining with S100, SMA, Desmin, and C‐kit, while staining with smooth muscle actin was focally positive. Ki‐67 proliferation index was 2% (Fig. 3).
Figure 3.
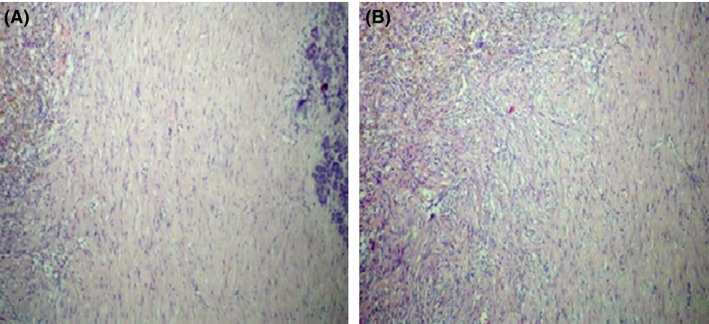
(A) Bland spindle‐shaped cells admixed with lymphocyte predominant inflammatory infiltrate on the left side and uniform pancreatic tissue on the right. H&E, X200, (B) Bland spindle‐shaped cells admixed with lymphocyte predominant inflammatory infiltrate. H&E, X400.
The lesion was composed of bland spindle‐shaped cells arranged in a storiform pattern. Lymphohistiocytic infiltrate was associated with the lesion in scant foci. Atypical mitotic figures, hyperchromasia, and cytological atypia were not present.
Discussion
Various names have been used to describe IMT, such as plasma cell granuloma, plasma cell pseudotumor, inflammatory pseudotumor, inflammatory fibroxanthoma, and histiocytoma 4. IMTs are classified as tumors of intermediate biological potential by the most recent World Health Organization classification, due to a tendency for local recurrence and a small risk of distant metastasis 5.
Although IMT has been seen in various organs, it is extremely rare to be seen in the pancreas. We find only 29 patients with IMT arising from the pancreas reported in the English language scientific literature 6, 7, 8, 9. While the youngest patient in the literature was 6 months old, the oldest patient was 64 years of age (mean age: 36 years). Our patient was 46 years old, and this was consistent with the medical literature.
In the other IMT cases, the patients were usually asymptomatic and diagnosed incidentally. According to our search in the medical literature, our case is the second IMT case that reported who has been diagnosed after signs and symptoms of acute pancreatitis 10. Laboratory findings of IMT were variable and nonspecific to the disease 11. The most common symptom of IMT is a mass discovered incidentally by radiographic investigations for other reasons. Therefore, IMT can be easily diagnosed as pancreatic cancer. Other symptoms could be abdominal pain (45%), jaundice (45%), weight loss (24%), and palpable abdominal mass (21%) 8, 12.
Inflammatory myofibroblastic tumor is most commonly mistaken for a pancreatic cancer clinically and radiologically. Definitive diagnosis was made only by extensive histological examination 13. Therefore, complete surgical resection and pathologic evaluation of the tumor are necessary to confirm the diagnosis 10.
In the management of IMT, surgical excision should be the primary choice to obtain a definitive diagnosis and to relieve symptoms. Careful follow‐up after surgery is also necessary. According to the review of Coffin, the recurrence rate was approximately 25% after the surgery 14, 15.
Conclusion
In this study, we aimed to explain a rare case, who presented to the emergency department with the findings of acute pancreatitis, and the further examinations revealed IMT.
Inflammatory myofibroblastic tumor of the pancreas is a rare, benign tumor of the hepatobiliary system. The first disease, which should be considered in the differential diagnosis, is pancreatic cancer. According to the current medical literature, the primary choice in the diagnosis, and treatment of IMT, as well, is surgical resection.
Conflict of Interest
None of the authors has a conflict of interest with any institution or organization.
References
- 1. Yamamoto, H. , Yamaguchi H., Aishima S., Oda Y., Kohashi K., Oshiro Y., et al. 2009. Inflammatory myofibroblastic tumor versus IgG4‐related sclerosing disease and inflammatory pseudotumor: a comparative clinicopathologic study. Am. J. Surg. Pathol. 33:1330–1340. [DOI] [PubMed] [Google Scholar]
- 2. Brunn, H. 1939. Two interesting benign lung tumors of contradictory histopathology. J. Thorac. Surg. 9:119–131. [Google Scholar]
- 3. Umiker, W. O. , and Iverson L.. 1954. Postinflammatory tumors of the lung; report of four cases simulating xanthoma, fibroma, or plasma cell tumor. J. Thorac. Surg. 28:55–63. [PubMed] [Google Scholar]
- 4. Yamamoto, H. , Watanabe K., Nagata M., Tasaki K., Honda I., and Watanabe S.. 2002. Inflammatory myofibroblastic tumor (IMT) of the pancreas. J. Hepatobiliary Pancreat. Surg. 9:116–119. [DOI] [PubMed] [Google Scholar]
- 5. Gleason, B. C. , and Hornick J. L.. 2008. Inflammatory myofibroblastic tumours: where are we now? J. Clin. Pathol. 61:428–437. [DOI] [PubMed] [Google Scholar]
- 6. Pungpapong, S. , Geiger X. J., and Raimondo M.. 2004. Inflammatory myofibroblastic tumor presenting as a pancreatic mass: a case report and review of the literature. JOP 5:360–367. [PubMed] [Google Scholar]
- 7. Wreesmann, V. , van Eijik C. H. J., Naus D. C. W. H., Velthuysen M.‐L. F., Jeekel J., and Mooi W. J.. 2001. Inflammatory pseudotumour (inflammatory myofibroblastic tumour) of the pancreas: a report of six cases associated with obliterative phlebitis. Histopathology 38:105–110. [DOI] [PubMed] [Google Scholar]
- 8. Walsh, S. V. , Evangelista F., and Khettry U.. 1998. Inflammatory myofibroblastic tumor of the pancreaticobiliary region. Am. J. Surg. Pathol. 22:412–418. [DOI] [PubMed] [Google Scholar]
- 9. Tomazic, A. , Gvardijancic D., Maucec J., and Homan M.. 2015. Inflammatory myofibroblastic tumor of the pancreatic head ‐ a case report of a 6 months old child and review of the literature. Radiol. Oncol. 49:265–270. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10. Panda, D. , Mukhopadhyay D., and Datta C.. 2015. Inflammatory myofibroblastic tumor arising in the pancreatic head: a rare case report. Indian J. Surg. 77:538–540. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11. Dulundu, E. , Sugawara Y., and Makuuchi M.. 2007. Inflammatory myofibroblastic tumor of the pancreas–a case report. Biosci. Trends 1:167–169. [PubMed] [Google Scholar]
- 12. Qanadli, S. D. , d'Anthouard F., Cugnec J.‐P., and Frija G.. 1997. Plasma cell granuloma of the pancreas CT findings. J. Comput. Assist. Tomogr. 21:735–736. [DOI] [PubMed] [Google Scholar]
- 13. Sim, A. , Lee M. W., and Nguyen G. K.. 2008. Inflammatory myofibroblastic tumour of the pancreas. Can. J. Surg. 51:E23. [PMC free article] [PubMed] [Google Scholar]
- 14. Coffin, C. M. , Watterson J., Priest J. R., and Dehner L. P.. 1995. Extrapulmonary inflammatory myofibroblastic tumor (inflammatory pseudotumor). Am. J. Surg. Pathol. 19:859–872. [DOI] [PubMed] [Google Scholar]
- 15. Kim, J. Y. , Song J. S., Park H., and Byun J. H.. 2014. Primary mesenchymal tumors of the pancreas: single‐center experience over 16 years. Pancreas 43:959–968. [DOI] [PubMed] [Google Scholar]


